Professional Documents
Culture Documents
Clean CV
Uploaded by
assssadfOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clean CV
Uploaded by
assssadfCopyright:
Available Formats
Cervical smear management.
I have updated and expanded this document to incorporate the information in CPM16. If there are
any bits you think might be wrong or are difficult to understand, please let me know. I find it very
difficult to edit stuff I have written.
Abbreviations.
ALOs: actinomyces-like organisms
ART: antiretroviral therapy
ASCUS: atypical squamous cells of undetermined significance.
BCE: borderline change in endocervical cells
BCC: borderline change in squamous cells
BSCCP British Society for Colposcopy and Cervical Pathology
cART: combination antiretroviral therapy, now preferred to the term “HAART”.
CPG: DOH: Clinical Practice Guidance for young women with abnormal vaginal bleeding. 2010
CPM10: NHS Cervical Screening Programme’s: “Colposcopy and Programme Management”.
2nd. Edition. May 2010.
CPM16: NHS Cervical Screening Programme’s: “Colposcopy and Programme Management”.
3rd. Edition. March 2016.
CIN: cervical intraepithelial abnormality
CGIN: cervical glandular intraepithelial abnormality
FSRH: Faculty of Sexual and Reproductive Health
?GNE: ? glandular neoplasia of endocervical type
?GNNC: ? glandular neoplasia (non-cervical)
GUM clinic: genito-urinary medicine clinic
HAART: highly active antiretroviral therapy
HGD: high-grade dyskaryosis (? invasive squamous carcinoma)
HGD?I: high-grade dyskaryosis (? invasive squamous carcinoma)
HGDM: high-grade dyskaryosis (moderate)
HGDS: high-grade dyskaryosis (severe)
HPV: human papilloma virus
HPVT: HPV triage
HRHPV: high-risk HPV
Kyrgiou: Kyrgio
LBC: liquid-based cytology
LGD: low-grade dyskaryosis
LLETZ: large loop excision of the transformation zone
MDT: multi-disciplinary team
NEC: normal endometrial cell
POP: progesterone-only Pill
SCJ: squamo-columnar junction
SIL: squamous intraepithelial lesion
SIP: RCOG’s Scientific Impact Paper 7: “Progress in Cervical Screening in the UK”. RCOG
March 2016.
STRATEGIC: Strategies to Increase Cervical Screening Uptake at First Invitation
TA69: NICE’s Technology Appraisal Guidance 69. “Guidance on the use of liquid-based cytology
for cervical screening.”
TOGAF TOG article by Mehrnoosh Aref-Adib & Theresa Freeman-Wang “Cervical cancer
prevention and screening: The role of HPV”. June 2016. DOI: 10.1111/tog.12279.
TZ: transformation zone
VaIN: vaginal intraepithelial neoplasia
Introduction.
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlane Page 1 of 25.
The information for this answer is mostly derived from CPM16.
The introduction of HPV testing has greatly simplified things.
If you are not familiar with colposcopy you may find it helpful to read MCQ paper 2, answer 24 in
which I have tried to explain the SCJ, TZ etc. You need a grasp of these basics to make sense of some
of what follows.
Terminology.
This is usually yawn-inducing, but is important as the category determines the action to be taken.
Some smears will be reported as “inadequate” or “inflammatory”. These have to be repeated as they
don’t allow cytological changes to be assessed and reported.
We then have 4 main categories for smears where the cytological changes can be assessed and
reported:
borderline changes: these can be glandular or squamous and go into triage based on HPV
testing
low-grade dyskaryosis: these go into triage based on HPV testing
high-grade dyskaryosis: these go for colposcopy
? glandular neoplasia: these go for colposcopy if cervical or to gynaecology if thought to be of
endometrial origin
There are sub-categories:
abnormal cervical cells can be squamous or endocervical (glandular).
low and high grade dyskaryosis refers to squames and is graded moderate, severe or ? invasive.
?glandular neoplasia is sub-divided by whether it originates in the cervix or elsewhere.
New terminology Previous terminology
Borderline change in squamous cells Borderline change
Borderline change in endocervical cells
Low-grade dyskaryosis Mild dyskaryosis
Borderline change with koilocytosis
High-grade dyskaryosis (moderate) Moderate dyskaryosis
High-grade dyskaryosis (severe) Severe dyskaryosis
High-grade dyskaryosis ?Invasive squamous carcinoma Severe dyskaryosis? Invasive
?Glandular neoplasia of endocervical type ?Glandular neoplasia
?Glandular neoplasia (non-cervical)
If you have forgotten what koilocytes are, there is a picture + explanation in MCQ paper 10, answer
20, which you can access on Dropbox.
Triage.
Women having routine smears will automatically have a test for high-risk HPV if the smear shows
minor abnormalities: borderline changes or low-grade dyskaryosis.
If the HPV test is –ve, the smear will be treated as normal and the woman returns to routine follow-
up.
The experience of the “sentinel sites”, which were used to evaluate HPV triage, was that about one
third of women with minor changes were HPV –ve and could return to routine follow-up, meaning
that a huge number of women could have the reassurance of being treated as normal and avoid the
unpleasantness and anxiety of unnecessary tests. It also means a substantial reduction in workload
for cytology services. There was an increase in referrals for colposcopy, but it was short-lived.
If the HPV test is +ve, she will be referred for colposcopy.
If a routine smear shows changes worse than LGD, the woman is referred to colposcopy. HRHPV
testing is not done as the cytological changes are sufficient on their own to merit colposcopy.
It could hardly be simpler!
A crucial question, and possible EMQ or SBA, is which smears are included in triage and which are
excluded.
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlane Page 2 of 25.
Smears that are included are those showing:
borderline squamous cells and those with low-grade dyskaryosis,
borderline glandular cells.
Smears that are excluded are those showing:
changes in squamous cells more significant than borderline changes or mild dyskaryosis,
changes in glandular cells more significant than borderline changes, these all being lumped into
the category ?glandular neoplasia.
Other things to remember:
inadequate smears and inflammatory smears,
smears suggestive of invasive disease,
smears & colposcopy and pregnancy,
vault smears.
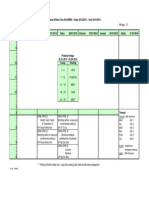
Summary of routine smears & their management.
Smear report What it means Management
Negative No abnormality seen Routine recall
Inadequate Usually insufficient cells or Repeat after 3/12. The first
inadequate preparation, so an smear scraped off the surface
assessment cannot be made. Less cells and you have to allow
likely with LBC. time for the skin to regrow.
Colposcopy if 3 consecutive
inadequate smears
Inflammatory Infection or something causing Treat identified infection and
inflammatory features. repeat.
Borderline changes * Appearances not normal, but not HPV triage.
bad enough for dyskaryosis to be
diagnosed.
Mild dyskaryosis Suggestive of CIN1 HPV triage.
Moderate dyskaryosis Suggestive of CIN 2 Colposcopy no HPV test
Severe dyskaryosis Suggestive of CIN 3 Colposcopy no HPV test
Suspicious of invasive Suggestive of invasive disease Urgent colposcopy no HPV test
disease
Glandular neoplasia Suggestive of endocervical or Colposcopy/ gynaecology
endometrial disease. Rarely tubal referral no HPV test
or ovarian.
* This includes glandular as well as squamous cells. Previously glandular changes were treated
separately and differently.
Test of cure.
You might argue that “cure” should never be used as it is too absolute a word. But let’s not get into
that!
Which treatments are eligible?
Treatment of CIN 1, 2 and 3 and CGIN. Excision margins don’t matter with CIN, but must be clear for
CGIN to be included.
What follow-up is done?
Smear at 6 months.
What is done after the smear is taken?
Exactly the same as in triage. Smears with minor changes: borderline or mildly dyskaryotic,
automatically have a HPV test. Women with –ve HPV tests go back to routine recall, those with +ve
smears go to colposcopy.
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlane Page 3 of 25.
Summary of Test of Cure.
After treatment, all women with CIN 1, 2 or 3 will have a smear at 6 months to determine
management. There are differences between women treated for CIN and women treated for CGIN.
One is the management if the excision margins are not clear. CPM16, section 4.16 says that all
women treated for CIN go back to care in the community with a smear 6 months after treatment
“irrespective of their excision margin status”. What happens with CGIN comes later, but excision
margins must be clear.
Those with minor changes have HPV testing. If –ve, they go to normal recall, if +ve they go to
colposcopy.
Six month smear result Management if HPV +ve Management if HPV –ve
Normal Colposcopy Normal recall
Borderline Colposcopy Normal recall
Mild dyskaryosis Colposcopy Normal recall
If the 6-month smear shows anything worse than mild dyskaryosis, the woman goes to colposcopy
without HPV testing.
Six month smear result Management
Moderate dyskaryosis Colposcopy, no HPV test needed
Severe dyskaryosis Colposcopy, no HPV test needed
What happens after treatment of CGIN?
This is dealt with in CPM16, section 4.17.
Women whose CGIN has been completely excised.
Management of CGIN is a bit more complicated, so you’ll probably need to read it a few times to get
your head round it.
CPM16 says: “Although robust data is lacking the increased sensitivity of HR-HPV testing permits the
introduction of TOC for women with completely excised GCIN”.
The woman attends in the community for a smear at 6 months. If the smear and the HRHPV test are
–ve, she returns 1 year later, i.e. at 18 months to repeat the process. If both tests are again –ve, she
is discharged to recall in 3 years.
Note all women come back at 3 years. They all had the same problem, so need the same follow-up.
Routine smears at 3 or 5 years depending on age reflect the probability of developing abnormality.
Here we are dealing with actual abnormality.
If any of the tests are +ve, colposcopy is needed.
If a woman has a –ve smear but +ve HR-HPV test and no abnormality is detected at colposcopic
examination, she has a second TOC test 12 months later. If both cytology and HRHPV are negative,
she is discharged with recall in three years.
If a +ve cytology report results from the 6 or 18 month TOC samples, the woman must be referred to
colposcopy. If no colposcopic abnormality is present and re-excision is not appropriate, she should
revert to ten years of cytology follow up.
CPM16 says that endocervical cells must be seen for smears to be valid, but that has been a
precondition for a smear to be “adequate” for as long as I can remember. If there are no endocervical
cells, you can’t guarantee that the whole of the SCJ has been sampled. However, the fact this this is
highlighted means that it could feature in the exam database.
Women whose CGIN has not been fully excised.
If a first procedure to excise CGIN comes back with a report that the excision margins are not clear,
repeat excision is usually offered.
Women whose excision margins are not clear and who don’t have re-excision have follow-up in the
colposcopy clinic. Cytology should be performed six months after treatment and if negative repeated
six months later (i.e. 12 months after treatment) and then annually for the subsequent nine years.
Is the HPV test really recommended if the cytology is normal after treatment of CIN or CGIN?
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlane Page 4 of 25.
You might think that if the smear result is normal, no HPV testing would be needed. But a normal
smear and a –ve HPV test is powerful reassurance that all is well.
It will be some time before all the laboratories catch up and we have universal implementation. But
we must assume that the exam committee has caught up and modified its answers.
Answer all questions on the basis that the new changes have been implemented and that HPV Triage
and Test of Cure are in place.
One of the issues that is likely to come up is the follow-up after hysterectomy.
This is summarised in section 10.5 of CPM16.
Uterine histology Type of smear recall Follow-up
No CIN Routine No follow-up
No CIN Not on routine recall VS at 6/12. No FU if VS -ve
Completely excised CIN Any recall VS at 6/12 & 18/12
Incomplete / uncertain excision CIN1 Any recall VS at 6/12, 12/12 & 24/12
Incomplete / uncertain excision CIN 2/ 3 Any recall VS at 6/12 & 12/12 + LTFU*
*LTFU: long-term follow up with 9 annual vault smears to 65 years or until 10 years after surgery
(whichever is later)
Suggested reading.
I have given basic information in MCQ paper 2, question 24.
I hope this document gives you what you need.
CPM16 is the main source of answers.
TOGAF is worth a look.
The FSRH’s “Intrauterine Contraception” of 2007 deals with actinomyces on pages 11 & 12.
Option list.
A. repeat the test
B. repeat the test after 6 months
C. repeat the test at 6 and 12 months
D. repeat the test at 6 and 12 months and then annually until she has had 10 years’ follow-up
followed by repeat tests at the normal intervals for her age
E. repeat the test after 3 or 5 years according to her age as per routine follow-up
F. repeat the test after HPV testing
G. management according to HRHPV triage
H. repeat the test after giving an appropriate antibiotic
I. repeat the test after removing her IUCD.
J. repeat the test after removing the IUCD and giving an appropriate antibiotic
K. repeat the test after treating the TZ with diathermy
L. repeat the test after treating the TZ with cryocautery
M. discharge from follow-up
N. refer for colposcopy
O. refer for colposcopy within 2 weeks
P. refer for colposcopy within 8 weeks
Q. refer for colposcopy within 12 weeks
R. refer for colposcopy only if she has other significant signs or symptoms
S. refer for cone biopsy
T. refer for fractional curettage
U. refer for “see and treat” LLETZ
V. refer to GUM clinic
W. recommend that she go back to America
X. there is insufficient information to formulate a management plan
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlane Page 5 of 25.
Y. false
Z. true
AA. none of the above
BB. age 24 years
CC. age 24.5 years
DD. age 25 years
Question 1.
At what age is the first invitation to have a smear test sent?
Option list.
A 20 years
B 22 years
C 24 years
D 24.5 years
E 25 years
Answer. D. CPM16 says: “A woman’s first invitation … must be sent out six months before her 25th
birthday … This ensures that the woman can be screened by her 25th birthday”.
Question 2.
Which of the following statements is used by the NHSCSP to justify not offering routine screening to
younger women?
Option list.
A most low-grade changes in younger women regress spontaneously
B most high-grade changes in younger women regress spontaneously
C HPV induced changes are common in younger women and screening would cause
large numbers of unnecessary colposcopy referrals and be prohibitively expensive
D colposcopic treatments may cause pre-term labour in subsequent pregnancies
E there is no evidence that screening younger women reduces incidence of cervical
cancer or resulting mortality.
Answer. A + D + E. You might think this an unfair question, but the starting age is frequently
challenged and campaigns conducted to have the age reduced below 25. CPM devotes a whole page
to justifying the starting age, so worth having a look.
There is still debate about the extent to which treatment of CIN causes pre-term delivery hence the
use of “may” in the question. The BMJ of the 28 th. May 2016 had an article with a meta-analysis by
Kyrgiou et al and an editorial which concluded: “This new meta-analysis adds to growing evidence
that cervical treatment for preinvasive disease can lead to preterm birth … outcomes. Women and
their clinicians must navigate the difficult trade-off between oncological safety now and the safety of
future pregnancies”.
Their figures for the risks were:
Feature Risk
≤10-12 mm 7.1% v 3.4%
≥10-12 mm 9.8% v 3.4%
≥15-17 mm 10.1% v 3.4%
≥20 mm 10.2% v 3.4%
> 1 treatment 13.2% v 4.1%
It also included the odd fact that women with untreated CIN have a higher risk of premature delivery
than women without CIN: 5.9% v 5.6%, a relative risk of 1.24.
CPM16 says in section 5.2.3 that a case control study NHSCSP, found no ↑in the risk of premature
labour when the length/depth of the excised specimen was ≤10mm.
Which facts will you use in the exam? Always a dilemma! I’d stick with CPM16 as the exam is so close
and it will probably take longer for the BMJ data to be incorporated.
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlane Page 6 of 25.
Question 3.
How often should women of 30 have routine smear tests?
Option list.
A every year
B every 2 years
C every 3 years
D every 4 years
E every 5 years
Answer. C.
The programme is as follows:
1st. invitation to have a smear age 24.5 with smear taken before 25th. birthday
ages 25-49 3-yearly smears
ages 50-64 5-yearly smears
age ≥ 65 no routine smears: there are exceptions – see later questions
Question 4.
A woman of 30 years is due to have a routine smear. How long after the previous smear should the
invitation be sent?
Option list.
A 34 months
B 36 months
C 58 months
D 60 months
E none of the above
Answer. E. She would be due another smear after 36 months and the invitation should be sent one
and a half months before the smear is due. So the answer is 34.5 months.
Question 5.
How often should women of 50 have routine smear tests?
Option list.
A every year
B every 2 years
C every 3 years
D every 4 years
E every 5 years
Answer. E.
Question 6.
A woman of 50 years is due to have a routine smear. How long after the previous smear should the
invitation be sent?
Option list.
A 34 months
B 36 months
C 58 months
D 60 months
E none of the above
Answer. E. She would be due another smear after 60 months and the invitation should be sent one
and a half months before the smear is due. So the answer is 58.5 months.
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlane Page 7 of 25.
Question 7.
Which, if any, of the following are grounds for continuing smear tests beyond the age of 64?
Option list.
A no adequate screening test after the age of 50
B no adequate screening test after the age of 55
C no adequate screening test after the age of 60
D patient’s request due to family history of fatal cervical cancer
E presence of genital warts
Answer. A. Women may require to continue as they have had previous abnormalities / treatment and
additional smears are part of follow-up. Most cancer in women > 65 occurs in women who have not
been screened. Any woman > 65 who has not been screened can be included. CPM16, section 2.1.1
says: “Invitation as required for women who have had recent abnormal tests. Women who have not
had an adequate screening test reported since age 50 may be screened on request … The pre-
existing recommendation to offer a test to previously unscreened women over the age of 65 is still
appropriate”.
Question 8.
Which, if any, of the following are grounds for smear tests in addition to routine tests?
Option list.
A history of heavy cigarette consumption
B 1st. use of the combined oral contraceptive
C diagnosis of genital warts involving the cervix
D new sexual partner
E multiple sexual partners
Answer. None. CPM16 refers to this as “unscheduled screening” and states very firmly that it should
not be done: “.Unscheduled cervical screening does not form part of the NHSCSP. Provided a woman
has undergone screening within the recommended interval (depending on her age), she should not
be re-screened”.
Question 9.
Which, if any, of the following are grounds for smear tests in addition to routine tests in the GUM
clinic?
Option list.
A 1st. attendance at a GUM clinic
B any attendance at a GUM clinic with proven STI
C diagnosis of genital warts involving the cervix
D new sexual partner with history of STI
E multiple sexual partners – simultaneous
F multiple sexual partners – not simultaneous
Answer. None. CPM16 says: “The indications for performing cervical cytology in GUM clinics are no
different to those for the rest of the NHSCSP”. The only exception is women who are HIV+ve and later
questions deal with that.
Question 10.
Which, if any, of the following are true of cervical cytology as a means of diagnosing STIs?
Option list.
A cervical cytology can be used to diagnose chlamydial infections
B cervical cytology can be used to diagnose gonococcal infections
C cervical cytology can be used to diagnose herpes
D cervical cytology can be used to diagnose syphilis
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlane Page 8 of 25.
E cervical cytology can be used to diagnose trichomonal infections
Answer. None of the above. There may be a strong indication that a particular STI is present, but
CPM16 says: “The specificity and sensitivity of cervical cytology for the identification of sexually
transmitted infections … is not high enough to permit this test to be used as a diagnostic tool”. It
should be “are” not “is”, but I’ll let it pass.
Question 11.
Which of the following should be used in the initial investigation of the woman, younger than the age
for inclusion in the NHSCSP programme, who presents with a three month history of intermenstrual
and postcoital bleeding?
Option list.
A inspection of the cervix using a speculum
B inspection of the cervix using a colposcope
C pregnancy test
D screening for chlamydia
E cervical smear
Answer. A + C + D. CPM refers to the existence of “specific algorithms” for managing this problem,
particularly referring to CPG. It is only a few pages long, so worth a look.
It estimates that PCB is the most significant sign of cancer in this age group and is reported by about
1 in 600 women aged 20-24 per year. IMB is more common and it estimates that 0.5-1% of women of
this present with abnormal bleeding each year. Cancer, of course, is very rare – CPM16 says it is
“rare” and that most cases are microinvasive only.
CPG’s advice about management is: “ If the cervix looks abnormal … which will be the case in a very
small proportion … urgent referral to colposcopy under the ‘two week wait’ rule.
If there is a benign lesion, such as cervical polyp, routine gynaecological referral …
If the cervix looks normal … pregnancy test and testing for cervical infection (e.g. Chlamydia, N
Gonorrhoea, Herpes)”. I doubt that most people would test for gonorrhoea and herpes.
Question 12.
Which, if any, of the following statements are true with regard to HRHPV as primary screening.
Option list.
A HRHPV is about 10% more sensitive than LBC in detecting borderline or worse changes
B HRHPV is about 25% more sensitive than LBC in detecting borderline or worse changes
C HRHPV detects > 70% of CIN2, CIN3 and invasive cancer
D HRHPV detects > 90% of CIN2, CIN3 and invasive cancer
E HRHPV is about 6% less specific in detecting borderline or worse changes
Answer. B + D + E. CPM16 says in section 3.3: “primary screening with HR-HPV … detects >90% of all
cases of CIN2, CIN3, and invasive cancer ... HR-HPV is approximately 25% more sensitive than LBC in
detecting borderline changes or worse, though it is about 6% less specific”.
Question 13.
Approximately how much of the NHSCSP was covered by the six sentinel sites used to evaluate
modern approaches to cervical screening?
Option list.
A 1%
B 5%
C 10%
D 15%
E 20%
Answer. C. CPM16 says in section 3.2.1: “In 2007, six sentinel sites (accounting for approximately 10%
of the English NHSCSP) began to carry out HR-HPV tests on all LBC samples showing low-grade
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlane Page 9 of 25.
abnormalities … to assess whether HPV triage and test of cure could be introduced … in a safe and
non-disruptive way”.
Question 14.
Which of the following statements are true in relation to the data obtained from the six sentinel
sites?
Option list.
A 16% of women with low-grade dyskaryosis were HRHPV –ve and returned to routine screening
B 26% of women with low-grade dyskaryosis were HRHPV –ve and returned to routine screening
C 45% of women with borderline changes were HRHPV –ve and returned to routine screening
D 65% of women with borderline changes were HRHPV –ve and returned to routine screening
E colposcopy referral rates increased by > 60%
Answer. A + C + E. CPM16 says in section 3.2.1: “... 16% of samples showing LGD and 45% of samples
showing borderline changes were returned to routine screening, significantly reducing the number of
women invited for repeat cytology”. This was because their HRHPV tests were –ve.
The corollary is that HR-HPV +ve rates were:
Changes on LBC smear tests Percentage +ve for HRHPV
borderline 53.7
low-grade dyskaryosis 83.9
It goes on to say that the percentage of women referred to colposcopy who were found to have high-
grade disease (defined as CIN2 or worse) varied from 9.1 to 30% in the 6 sites.
And that negative colposcopy had high negative predictive value, with only 4.4% having CIN2 or
worse diagnosed in the next 3 years.
The increase in referral to colposcopy was 64%, but was “transient”. Just as well as colposcopy
services would have had an enormous problem with an overall rise of this magnitude if it had been
sustained.
Question 15.
Which, if any, of the following statements are true in relation to the NHSCSP in the year ending 31
March 2015?
Statements.
A 85% of eligible women were screened in the year up to 31 March 2015
B 72% of eligible women aged 25-49 years were screened
C 78% of eligible women aged 50-64 years were screened
D 4.31 million women were invited for screening & 3.12 million women were tested
E 98% of women should receive their smear reports within 2/52, but only 91% did
F 3.2 million samples were examined by the laboratories
G 198,216 referrals were made to colposcopy, a 0.6% ↓ from the previous year
H 2.5% of smears were inadequate
Answer. All except A.
Key facts are given on the NHS website, http://digital.nhs.uk/catalogue/PUB18932, but you don’t
need to look at them.
The key facts highlighted were:
1. the % of women aged 25 to 64 who were recorded as screened adequately was 73.5
Age → 31 March 15 → 31 March 14 → 31 March 11
25-49 71.2% 71.8% 73.7%
50-64 78.4% 79.4% 80.1%
Overall 73.5% 74.2% 75.7%
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlanePage 10 of 25.
2. 4.31 million women were invited for screening 3.12 million were tested, a fall of 3.3% from
2013-14 when 3.23 million were tested.
3. Women should receive their test result within 2/52. 91.0% of women … in this time scale
compared to 93.7% in 2013-14. This is below the Key Performance Indicator of 98.0%.
4. 3.20 million samples were examined … in 2014-15 compared with 3.41 million in 2013-14.
2.5% were inadequate compared with 2.4% in 2013-14.
5. 198,216 referrals were made to colposcopy a 0.6% ↓ from 2013-14.
Question 16.
Which, if any, of the following statements are true in relation to LBC and the traditional
cervical smear?
Statements.
A both involve drying the slide on which the smear is made in air by the person taking the smear
B the sensitivity of LBC is superior
C the specificity of LBC is superior
D inadequate smears ↓ from about 9% with traditional smears to 1-2% with LBC
E LBC is now the NHSCSP standard for cervical screening
F HPV testing cannot be done on routine LBC samples
Answer. B + D + E.
TA69 says: “meta-analysis … the sensitivity of LBC and the Pap smear in the detection of
abnormalities of low-grade squamous intraepithelial lesions or greater demonstrated that sensitivity
may be up to 12% better with LBC … compared with the Pap smear.
CPM16 says in section 3.1: “the standard screening modality within the NHSCSP is LBC … a 2003
review by NICE concluded:
that LBC represented a cost-effective alternative to Papanicolaou smears
offering improved sensitivity without any reduction in specificity
and a reduction in the number of inadequate tests reported”.
Note that the recent figure from the NHSCSP for inadequate smears is about 2.5%
Question 17.
Lead in.
Which, if any, of the following statements are true in relation to inadequate smears?
A inadequate smears are defined as those showing insufficient squamous cells
B inadequate smears are defined as those showing inflammatory changes
C a smear should not be defined as inadequate if there are borderline or dyskaryotic changes
D a repeat LBC sample should be obtained within 1 month of an initial inadequate sample
E a repeat LBC sample should be obtained within 2 months of an initial inadequate sample
F a repeat LBC sample should be obtained after an initial inadequate sample, but not within 3
months
G referral for colposcopy is required after 2 consecutive inadequate cervical smear reports
H referral for colposcopy is required after 3 consecutive inadequate cervical smear reports
I referral for colposcopy is required after 4 consecutive inadequate cervical smear reports
J the appointment for initial colposcopy after inadequate smears should be within 6/52 of
referral
K the appointment for initial colposcopy after inadequate smears should be within 12/52 of
referral
L referral for colposcopy after inadequate smears is to exclude invasive cancer
Answer. C + F + H + J + L. Inadequate samples are dealt with in section 4.4 of CPM16: “Where … LBC
sample is reported as inadequate, cytology should be repeated … not less than three months after
the previous test. … a sample must be reported as inadequate if the sample taker has not completely
visualised the cervix, or if the sample has been taken in an in inappropriate manner, e.g. with a
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlanePage 11 of 25.
sampling device that has not been approved by the NHSCSP. Samples must not be reported as
inadequate if they contain any evidence of borderline change or dyskaryotic cells.
4.4.2 … After three consecutive inadequate samples a woman should be referred to colposcopy. She
should be seen … within six weeks of referral (99%) … Invasive cancers may be associated with
cytology samples which do not contain abnormal cells. Women with persistent inadequate smears
should undergo colposcopy to exclude invasive cancer”.
Question 18.
A woman with no previous abnormal smears has a routine smear showing an inadequate sample .
What management will you suggest?
Answer. a. Repeat the test. If the sample is inadequate, it cannot be analysed so triage cannot apply
and the only thing is to repeat the test. The question that arises is “when do you do more than
repeat the test when the result keeps coming back as inadequate?”.
CAPM says: “Women should be referred for colposcopy after 3 inadequate smears”.
The rationale is that malignancies do not always produce malignant cells on smear tests and
“inadequate results may be associated with lesions that are not exfoliating”.
Other facts. When colposcopy is done as investigation of an abnormal smear result, it is not routine
to take a smear. But this may be done when dealing with a series of inadequate smears. (6.2). In this
situation, if the colposcopy is normal, the woman can go back to routine recall. (9.8.5). The
document also mentions that inadequate smears are more common in GUM clinics as a result of
infection. (2.5)
LBC has been the standard technique for cervical cytology since 2008. A useful fact to remember is
that it reduces the number of inadequate smears (3.1), but does not eliminate them.
Question 19.
A woman with no previous abnormal smears has had a smear showing borderline nuclear changes.
What management will you suggest?
Answer: AA. HPV triage. This should now happen automatically.
If a smear has been shown to have borderline or mildly dyskaryotic cells, including borderline
glandular cells, which is a new recommendation, the laboratory will automatically perform HRHPV
testing. So, the answer will be derived from the HPV result. We would need an entry in the option list
like: “return to normal recall if the HPV test is –ve; arrange colposcopy if +ve”.
A lot of people answer “f. repeat the test after HPV testing”. This is a desperate attempt to find an
answer on the option list that could somehow be interpreted in such a way as to be the correct
answer. There is no way this can be the correct answer and you must have enough self-confidence to
go for “AA. none of the above”. It accentuates the need for good EMQ technique. Don’t read the
option list until you have decided the answer! You have heard it time and again, but lots of people
still do it. You need to decide the correct answer and then look for it on the option list. If it is not
there, the answer is “none of the above”. Reading the lead in and then going on a fishing trip with
the option list is a recipe for disaster. The exam committee will have tried to create a list with one or
two answers that look attractive as well as the correct answer. They will also put in things that you
won’t understand or know about to confuse. Don’t fall into the trap!
Question 20.
A woman with no previous abnormal smears has had a smear showing borderline nuclear changes.
Cervical ectopy is noted. What management will you suggest?
Answer. HPV triage. This is the management of borderline changes as in Question 19. The ectopy is
irrelevant. Indeed, the CPM16 does not even mention it!
Question 21.
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlanePage 12 of 25.
A woman with no previous abnormal smears has had a smear showing borderline cells of
endocervical origin. What management will you suggest?
Answer. HPV triage. This is the same as Question 19. Borderline glandular cells from the endocervix
used to be treated as much more serious than borderline changes in squamous cells and the answer
used to be “refer for colposcopy within 8 weeks”. Borderline cells of both types are now treated the
same and have triage.
Question 22.
A woman with no previous abnormal smears has had a smear showing inflammatory changes. What
management will you suggest?
Answer. AA. None of the above.
CPM16 only mentions “inflammatory” smears in in section 2.5 where it says that inadequate and
inflammatory smears are more common in GUM clinics. It makes the point that smears should not be
used to diagnose infection, even when there is clear evidence of a particular infecting agent such as
Tv or Monilia. The obvious point is that other infections can’t be excluded, so appropriate tests must
be done. Inflammatory changes on their own do not indicate an increased risk of CIN, CGIN or
malignancy; they are about infection or some other inflammatory process.
For us, the management will depend on:
is the cytology normal, abnormal or inadequate?
is there is evidence of specific infection, assuming the smear was not taken in GUM?
The woman should be informed of specific infection and referred to GUM if it indicates a risk of STI,
e.g. Tv or herpes.
Question 23.
A woman with no previous abnormal smears has had a smear showing inflammatory changes and
ALOs. What management will you suggest?
Answer: AA. None of the above.
We can’t answer this question unless we know if the cytology was normal and if she is symptomatic
or not. CPM16 deals with ALOs in section 7.3.1. “ALOs are usually associated with an IUD. If the
woman is symptomless, then neither removal of the device nor antibiotic treatment is indicated. If
the woman has symptoms, the IUD may need to be removed”. It goes on about contraception but
the summary is: “Due to the poor sensitivity and specificity and low positive predictive value of
cervical cytology for the detection of ALOs, the prognostic significance of ALOs detected via this
method is minimal in the absence of concomitant symptoms”.
The FSRH’s advice is similar but briefer: “Intrauterine contraceptive users with ALO detected on a
swab who have no symptoms should be advised there is no reason to remove the intrauterine
method unless signs or symptoms of infection occur. There is no indication for follow-up screening. If
symptoms of pelvic pain occur, women should be advised to seek medical advice. Other causes of
infection (in particular STIs) should be considered and it may be appropriate to remove the
intrauterine method”.
Question 24.
A woman with no previous abnormal smears has had a smear showing inflammatory changes. She
takes the COC for contraception. What management will you suggest?
Answer. AA. None of the above.
You must be getting bored with inflammatory changes! The management of any abnormal smear in a
woman on the COC or POP is based on the nature of the abnormality. The Pill does not alter the
management and should not be stopped.
Section 11.2.1 states: “Women with abnormal cervical screening results should not be advised to
change from the oral contraceptive pill if it is a successful method of contraception for them. An
abnormal result should not influence the choice of contraception”.
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlanePage 13 of 25.
So, the answer to inflammatory changes on the Pill is the same as in the preceding answers. Is there
evidence of atypia? is there evidence of specific infection?
Question 25.
A woman with no previous abnormal smears has had a smear showing inflammatory changes. She
has a copper IUCD. What management will you suggest?
Answer. AA. None of the above.
More damned inflammatory changes!
Ignore the IUCD, once again it is just the management of inflammatory changes.
CPM16 deals with women coming to colposcopy in section 11.2.2. Women need clear advice about
the local policy as to whether an IUD will be removed and alternative contraception. It also says that
local treatment does not mean an IUD has to be removed.
Question 26.
A woman with no previous abnormal smears has had a smear showing inflammatory changes and
ALOs. She has had hysteroscopic sterilisation with ESSURE. What management will you suggest?
Answer. AA. None of the above.
This is managed as an inflammatory smear and the ESSURE is irrelevant. I think I must have been
getting bored when I wrote this! There is nothing in the document about sterilisation, never mind
ESSURE, so we have to go back to first principles. ESSURE is designed to block the tubes, so should
reduce the risk of ascending infection from the ALOs. If you were dealing with a patient, you would
need to mention that we don’t have any facts.
If you are unsure about ESSURE, there is a simple video here that gives a good, basic explanation:
http://essure.co.uk/Home/Resources/tabid/137/Default.aspx.
And this ends inflammatory smears! Sorry for the surfeit of examples, but they have caused a lot of
problems. I hope you are now confident.
Question 27.
A woman with no previous abnormal smears had a smear showing borderline changes. A repeat
smear after 6 months was normal. A repeat smear after 3 years showed mild atypia. A repeat smear
after 6 months was normal. A recent repeat smear, 3 years after the previous one, showed borderline
changes. What management will you suggest?
Answer. g. Management based on HRHPV triage. This sounds difficult, but is exactly the same as the
above questions. She will automatically have had HPV testing with the latest smear and the
management will be dictated by that. The smear history was added to complicate matters and make
it seem more difficult than it is. But, in essence, the previous smear management was correct, so the
issue is really about the recent smear with borderline changes.
Question 28.
A woman with no previous abnormal smears has had a smear showing mild dyskaryosis of squamous
cells. What management will you suggest?
Answer. g. Management based on HRHPV testing. It illustrates how much better things are – the
previous management would have been to refer for colposcopy within 8 weeks”. But HRHPV testing
will have been done and triage will determine the outcome.
Question 29.
A woman with no previous abnormal smears has had a smear showing moderate dyskaryosis of
squamous cells. What management will you suggest?
Answer: O. Colposcopy within 2 weeks. This should have been reported using the new terminology
as “high-grade dyskaryosis (moderate). CPM deals with this in section 3.2.2, but basically any report
showing worse changes than borderline or mildly dyskaryotic cells triggers colposcopy with no need
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlanePage 14 of 25.
for HRHPV testing – she would need colposcopy regardless of the result, so there is no point in the
test.
Waiting times are dealt with in section 4.8.2 of CPM16. Women with HGD are included in the 62-day
standard introduced by the ‘Cancer Reform Strategy’. The time starts with the receipt of the referral
and she must be seen within 2 weeks.
Question 30.
A woman with no previous abnormal smears has had a smear showing severe dyskaryosis of
squamous cells. What management will you suggest?
Answer. N. Colposcopy within 2 weeks. The answer is the same as that for the previous question.
Question 31.
A woman with no previous abnormal smears has had a smear suggestive of invasive disease. What
management will you suggest?
Answer. O. Urgent referral for colposcopy within 2 weeks. This is dealt with in section 4.10.1 and 2 of
CPM16. It says there is a high correlation with cancer, with one series putting it at 56%.
Question 32.
A woman with no previous abnormal smears has had a smear showing borderline nuclear changes in
glandular cells. What management will you suggest?
Answer. g. Management according to HRHPV triage. This is a repeat of question 21. Borderline
glandular cells are now included in triage, so she will have had a HPV test.
Question 33.
A woman with no previous abnormal smears has had a smear showing ? glandular neoplasia. What
management will you suggest?
Answer. AA. None of the above. This is an ‘it depends’ answer. It is covered in section 4.11 of CPM16.
If the cells are thought to come from the cervix, she gets referral for colposcopy and must be seen
within 2 weeks. If it is thought that the cells come from the endometrium or elsewhere, she gets
urgent referral to gynaecology and must be seen within 2 weeks.
Question 34.
A 30-year-old woman with no previous abnormal smears has had a smear showing ? glandular
neoplasia. She is nulliparous and would like to have children. Colposcopic appearances suggest high-
grade CGIN. What management will you suggest?
Answer. AA. None of the above. She needs a cylindrical excisional biopsy that includes the Tz and ≥ 1
cm. of the endocervix proximal to the SCJ”.
CPM16, 9.3.1 says: “Expert opinion supports a primary excisional procedure for initial management
of all cases of high-grade atypical glandular cytology, with further management decisions based on …
histological assessment … women who wish to conserve their fertility who have a visible SCJ, a
cylindrically-shaped cervical excisional biopsy, including the whole Tz and at least 1cm of endocervix
above the SCJ is appropriate”.
Question 35.
A 50-year-old woman with no previous abnormal smears has had a smear showing ? glandular
neoplasia. Colposcopic appearances suggest high-grade CGIN. What management will you suggest?
Answer. AA. None of the above. CPM16, 9.3.1 says: “Expert opinion supports a primary excisional
procedure for initial management of all cases of high-grade atypical glandular cytology, with further
management decisions based on a thorough histological assessment, including margin status… In
older women, or where the SCJ is not visible at colposcopy, a cylindrical biopsy should be taken that
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlanePage 15 of 25.
includes all of the visible TZ and 20mm to 25mm of the endocervical canal. Expert opinion favours
techniques that either avoid thermal artefact to improve assessment of the excision margins”.
Question 36.
A 50-year-old woman with no previous abnormal smears has had a smear showing ? glandular
neoplasia. Colposcopic appearances suggest high-grade CGIN. An appropriate excisional biopsy is
taken which shows no abnormality. What management will you suggest?
Answer. AA. None of the above. CPM16, 9.3.1 says: “where cervical pathology has been excluded, an
endometrial biopsy, +/- pelvic imaging should be considered”. This is the sort of case that would be
discussed by the MDT.
Question 37.
A woman with no previous abnormal smears has had a smear showing normal endometrial cells.
What management will you suggest?
Answer. AA. None of the above. We don’t have enough information. CPM16 says that the significance
of such cells depends on the woman’s age and history, the phase of the menstrual cycle and any
drugs she might be taking.
CPM16 deals with this is section 4.13.
For women under 40, it says the evidence is that normal endometrial cells are not a sign of
significant endometrial pathology. It goes so far as to say that they do not need to be reported.
For women over the age of 40, it says that normal endometrial cells are significantly more likely to be
found up to the 12th day of the cycle and do not need to be reported.
Normal endometrial cells found after the 12 th. day may indicate endometrial pathology, ranging from
benign polyps to cancer. As you would expect, the risk of serious pathology goes up with age and it
cites a risk of up to 13% of endometrial hyperplasia and cancer in women > 60 years.
Normal endometrial cells found after the 12 th. day are less likely to be linked to pathology if the
woman has an IUD or is taking an oral contraceptive, HRT or tamoxifen.
It says that normal endometrial cells should always be reported in women > 40 if the menstrual,
drug, and contraceptive histories are not known. It suggests words be used such as: ‘Endometrial
cells are present but menstrual history not stated. If there is any history of abnormal vaginal
bleeding, referral for a gynaecological opinion should be considered’.
For postmenopausal women, normal endometrial cells should always be reported and it suggest a
form of words to be used: ‘Endometrial cells are present in a woman aged over 40. Such cells may be
associated with endometrial pathology, particularly if out-of-phase or after the menopause. Referral
for a gynaecological opinion should be considered in light of the menstrual, medication, and clinical
history.’ If the day of the menstrual cycle is not known and the sample is otherwise negative, then it
should be reported as negative, with a comment similar to the following:
Question 38.
A woman with no previous abnormal smears has had a smear showing atypical endometrial cells.
What management will you suggest?
Answer. AA. None of the above.
She needs urgent referral to a gynaecologist, i.e. to be seen within 2 weeks. CPM16 deals with this in
section 9.2.5. It says that atypical endometrial cells are clinically significant, with more than one third
of women having significant disease.
Question 39.
A woman with no previous abnormal smears and no symptoms has had a smear with a normal
result. Clinical examination was normal, but contact bleeding was noted when the smear was taken.
The Practice Nurse who took the smear phones you for advice about her management. What advice
will you give?
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlanePage 16 of 25.
Answer: E. No action is needed if she has no other symptoms and she can return to routine follow-
up.
CPM16, section 4.15.1 says: “contact bleeding … may occur and is not an indication for referral to
colposcopy in the absence of other symptoms”.
Question 40.
An American woman with no previous abnormal smears has been used to having annual smears. She
has had a smear with a normal result and requests a repeat in 12 months. What management will
you suggest?
Answer. AA. None of the above.
You will tell her that the NHS recall is for 3-yearly smears between the ages of 25 and 49 and 5-yearly
from 50 – 64. After 65 women only need to be screened if they have not been screened since the age
of 50 or have had recent abnormal smears or treatment and further smears are part of follow-up.
More frequent screening would have to be done on a private basis.
Question 41.
A woman with no previous abnormal smears is on renal dialysis and has had a smear with a normal
result. What management will you suggest?
Answer. AA. None of the above. .
CPM16 section 12.2 says that women on dialysis or needing organ transplantation must have
cytology at or shortly after diagnosis.
Women due to have organ transplant should have had a smear in the previous year.
It says that women who are immunosuppressed are at more risk of getting an HPV infection and less
likely to be able to clear it. It says that more frequent screening may be beneficial but does not give
any specific advice. It also says that cytology is relatively insensitive in this group and that they
should have early referral to colposcopy, but again it gives no details.
Question 42.
Which, if any, of the following statements are true in relation to women who are HIV +ve compared
to those who are HIV -ve?
A there is an increased incidence of false –ve smear reports
B there is an increased incidence of false +ve smear reports
C the prevalence of SILs is 10-20%, 10 times higher than for HIV-ve women
D the prevalence of SILs is 20-40%, 10 times higher than for HIV-ve women
E HIV +ve women taking HAART have higher rates of abnormal cytology than HIV –ve women
F HAART may reduce the prevalence of squamous intraepithelial lesions
G LGD is less likely to regress
H LGD is more likely to regress
I HGD responds less well to standard treatments
J HGD responds better to standard treatments
K Close co-operation between the HIV medical team and colposcopists / smear takers is essential
Answer. A + D + E + F + G + I + K. CPM16, section 12.8 has the following.
Annual cytology should be performed with an initial colposcopy if resources permit.
Evidence: there is evidence … that there is an increased risk of false –ve cytology.
The estimated prevalence of cervical disease … in HIV -ve women is 3%... studies have indicated a
greatly increased prevalence of SILs, between 20% to 40% in HIV +ve women…
regression of low-grade lesions is rare and high-grade lesions may respond poorly to standard
therapies… In one study, the recurrence rate was 87% in women with CD4 counts <200/mm 3,
compared with < 10% in immunocompetent women.
The reason for this high incidence and recurrence … is thought to be the lack of immune activity
against HPV. Even cohorts using HAART are at increased risk of abnormal cytology, although HAART
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlanePage 17 of 25.
may increase the regression of low-grade lesions. Early data from a European study shows a 33%
prevalence of abnormal cytology, ASCUS, or worse … although a large proportion were receiving
HAART”.
Question 43.
A woman recently diagnosed as HIV +ve has had a smear with a normal result. Previous smears have
been normal. Which, if any, of the following statements are true?
A twice yearly smears should be arranged
B annual smears should be arranged
C colposcopy should be arranged if resources permit as part of the initial assessment
D annual colposcopy should be arranged if resources permit
E ablation of low-grade CIN should be offered as such lesions are more likely to progress than in
HIV –ve women
F surgical removal of the cervix should be offered if high-grade CIN is diagnosed
G screening should continue until at least the age of 75
H women with good response to HAART and normal cytology can safely return to routine
screening
Answer. B + C + D. This is dealt with by CPM16 in section 12.8. It says that cervical surveillance should
be done by the HIV medical team or in conjunction with it. Initial colposcopy should be done if
feasible and annual smears. Subsequent colposcopy should be done according to national guidelines
and the age range should be the same as for HIV –ve women.
It says that high-grade CIN should be managed according to national guidelines although there is a
higher failure rate. And that low-grade CIN (< CIN2) should “probably” be left untreated as it is likely
to be due to persistent HPV infection responds poorly and may clear spontaneously. It is expected
that progression will be detected by the proposed surveillance.
HAART reduces HIV viral load, and may do the same to HPV viral load. The rates of cervical atypia
may be reduced, but the evidence in inconclusive and more surveillance than normal is needed to
detect preinvasive lesions.
Close co-operation is advised between colposcopists and HIV physicians to ensure that women are
not over-treated if there is a possibility of enhancing immunocompetence with ART.
Women who are HIV positive can cease cervical screening at age 65 if they fulfil the usual criteria.
Question 44.
A woman with no previous abnormal smears has had a smear with a normal result. She smokes 20
cigarettes daily and has a long history of recurrent genital warts. What management will you
suggest?
Answer. E. Routine follow-up.
Section 2.4 of CPM16 says that unscheduled screening is not part of the NHSCSP. It gives a list of
examples, presumably reasons people have thought indicated more smears, of things that make no
difference. COC, IUD, HRT, pregnancy warts or genital infection, cigarettes and multiple sexual
partners.
Question 45.
A woman of 70 presents with postmenopausal bleeding. She had smears at the recommended
intervals from the age of 22. All were normal. The last was taken at the age of 64. What is your
management in relation to taking a smear?
Answer. AA. None of the above.
She needs referral to a gynaecologist, but does not need a smear if her cervix looks normal.
Section 11.3.2 says that PMB is not grounds for a smear if she has been screened adequately.
Question 46.
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlanePage 18 of 25.
A woman of 55 presents with hot flushes since her periods stopped at the age of 54. She wishes to
go on HRT and there are no contraindications. She had smears at the recommended intervals from
the age of 25. All were normal. The last was taken two years ago. What is your management in
relation to taking a smear?
Answer. E. Routine follow-up.
HRT makes no difference to anything in relation to smears.
As noted above, Section 2.4 of CPM16 says HRT makes no difference to how she should be screened.
In addition, it is not a known risk factor for cervical cancer and pre-cancer.
Question 47.
Which, if any, of the following statements are true about women who have been treated for CIN
compared to women who have not been treated?
A their risk of developing cervical cancer is increased by a factor of 2 – 5 compared to women
who have not been treated
B women should be returned to community-based recall
C women should have a cervical sample taken for cytology at 6 months, but only if the excision
margins were clear. Where the excision margin was, or may have been involved, colposcopy
should be done at 6 months
D if the 6 months cytology is normal, borderline or low-grade and the HRHPV test is –ve, women
should return to routine recall based on their age
E if the 6 months cytology is normal, borderline or low-grade and the HRHPV test is –ve, women
should have repeat cytology at 3 years, regardless of their age
F if the 6 months cytology shows changes worse than low-grade, colposcopy should be done and
HRHPV testing is not required
G if “test of cure” cytology is done in hospital, it should be in a cytology clinic, not the colposcopy
clinic
Answer. A + B + E + F + G. CPM16 is the source of these answers.
A Section 10.1 gives the increased risk of cancer as 2-5 times that of women who have not been
treated.
B. Section 4.1.6 says that women should be returned to community-based recall and that follow-up
should take place 6 months after treatment.
C. This is wrong as the excision margins are irrelevant. 4.1.6 says: “Women who have been treated
for CIN should be returned to community-based recall, irrespective of their excision margin status.
A cervical cytology sample should be taken six months after treatment”. There is scope for
confusion as 8.6.1 dealing with CIN3 extending to the margins of excision or uncertainty about the
margins says that there is a bigger risk of recurrence but that “routine” repeat excision is not
justified so long as there is no evidence of glandular abnormality or invasive disease and the
woman is under 50 years of age. 8.6.2 says that women > 50 years with CIN3 at the margins and
“in whom satisfactory cytology, HRHPV typing and colposcopy cannot be guaranteed” should
have repeat excision to try to get clear margins. My understanding of this is that cytology / HRHPV
typing / colposcopy would not be done until the 6 month follow up, so the initial management is
the same as for younger women: community-based cytology 6 months after treatment.
D. This is correct except for the bit about age. All women will be recalled after 3 years. This makes
sense. The risk of having HPV is greater at young ages, hence the advice about 3 year smears. But
here we are dealing with women who have had the same problem, CIN that needed to be treated,
so their recall timings should be the same.
G. This is stated in 4.1.6 and makes sense as it a cytology clinic would be simpler than a colposcopy
clinic and probably involve fewer staff. It would not need a permanent colposcopy set-up, so could
be used for other things.
Question 48.
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlanePage 19 of 25.
More than 50% of women who develop cervical cancer have been lost to follow-up. True or false?
Answer. True.
Section 10.1 says: “Much of this increased risk may result from poor compliance with long-term
follow up; several case series demonstrate that > 50% of cancers develop in women who are lost to
follow up.”.
Question 49.
Which of the following statements are true and which false in relation to treatment of CIN?
a. cone biopsy is linked to ↓risk of recurrence compared to LLETZ.
b. the Tz must be seen in its entirety if ablative techniques are to be used
c. excision margins that are not CIN-free ↑ the risk of recurrence, with endocervical margins that
are not CIN-free posing a greater risk that similar ectocervical margins.
d. age > 35 years increases the risk of recurrent disease.
e. the “see and treat” policy should no longer be used.
f. excisional treatments should be used in women > 50 years.
d. follow-up after treatment for CIN should start between 3 & 6 months from the time of treatment.
e. the initial follow-up examination after treatment for CIN should be with colposcopy plus cytology.
f. a failure to achieve negative results in the year after treatment means cone biopsy should be
done.
g. a required standard for treatment success is that ≥ 90% of women should have no evidence of
dyskaryosis in the year after treatment.
h. a required standard for treatment success is that there should be ≤ 5% of histologically-confirmed
treatment failures by 1 year after treatment.
Answers. These answers come from Section 8.
a. False. 8.1 says that there is no “obviously superior” conservative technique.
b. True. 8.1 lists 4 criteria: the Tz must be fully seen, there must be no glandular anomalies, no
evidence of invasive disease and no discrepancy between cytology and histology.
Section 8.6 Repeat excision.
c. “Evidence: CIN extending to the resection margins of a LLETZ has been shown to be a risk factor
for recurrent CIN in both the short and the long term. This risk appears predominantly due to the
presence of CIN at the endocervical margin. Despite the increased incidence of recurrence, the
majority of women in the above studies had no evidence of residual disease, and the
recommendation is that these women have colposcopy and cytology at first follow up”.
c. False. Section 8.6.2. See “b”. The increased risk is identified from the age of 50.
d. False. Follow up-should start at 6 months after treatment and not later than 8 months.
e. False. “Cytology alone is recommended for follow up and samples should be taken by
appropriately trained staff”. The next bit states that follow-up can be done in the community,
which could easily be a question: “Initial follow up cytology … may be performed in the
colposcopy or gynaecology clinic. Alternatively, it may be performed in the community”.
f. True: “All women who do not have negative test results after treatment should be re-colposcoped
at least once within 12 months”. This is not entirely clear. I take it to mean that if you had an
initial result showing borderline cells or reported as “inadequate” you should have a subsequent
negative result or you should have colposcopy. Not that women with positive reports can be
colposcoped any time up to 12 months later.
g. False. This standard is a measure of the quality of the treatment but is for the first 6 months. “The
proportion of treated women with no dyskaryosis six months following treatment should exceed
90%”.
h. True. “The proportion of confirmed histological treatment failures should not exceed 5% within
12 months of treatment”.
Question 50
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlanePage 20 of 25.
Women who have had normal follow-up results for 2 years after treatment of CIN 1 can revert to the
routine recall.
Answer. This was true. See the answer to Question 31. But now we are back to “test of cure”.
They will have had a smear at 6 months. If normal or showing borderline or dyskaryotic cells, they
will have had an automatic HPV test. If –ve, they go back to routine recall. If +ve, they go for
colposcopy.
Question 51.
Follow-up should continue with increased frequency for 5 years after treatment of CIN 2 & 3, after
which recall at routine intervals is OK if all the follow-up has been normal. True or false?
Answer. False. See the answer to Question 31.
Question 52.
A woman with LLETZ for CIN3 twelve months ago had a normal smear 6 months later. A smear taken
12 months after treatment is also normal. What management will you suggest?
Answer. AA. None of the above. The management will depend on the HPV test which should have
been done automatically. Routine recall is appropriate for those with –ve tests; colposcopy for those
with +ve tests.
Question 53.
A woman with LLETZ for CIN3 twelve months ago had a normal smear 6 months later. A smear taken
12 months after treatment shows mild dyskaryosis. What management will you suggest?
Answer. Same as for Question 31.
Question 54.
A woman on normal recall has hysterectomy for menorrhagia. There is no evidence of CIN on
histology. What follow-up would you recommend?
Answer. M. Discharge from follow-up.
CPM16 deals with hysterectomy in section 10.5.
It says that expert consensus is that the woman on routine recall with no CIN on histology of the
uterus does not require vault cytology. It makes the point that vault smears are not part of triage or
test of cure.
The full list of recommendations is here.
Uterine histology Type of smear recall Follow-up
No CIN Routine No follow-up
No CIN Not on routine recall VS at 6/12. No FU if VS -ve
Completely excised CIN Any recall VS at 6/12 & 18/12
Incomplete / uncertain excision CIN1 Any recall VS at 6/12, 12/12 & 24/12
Incomplete / uncertain excision CIN 2/ 3 Any recall VS at 6/12 & 12/12 + LTFU*
*LTFU: long-term follow up with 9 annual vault smears to 65 years or until 10 years after surgery
(whichever is later)
Question 55.
A woman who was not on normal recall has hysterectomy for menorrhagia. There is no evidence of
CIN on histology. What follow-up would you recommend?
Answer. B. CPM16 says repeat the smear after 6 months. If that is OK she can be discharged from
follow-up. This is the only situation in which the type of recall is important. If she was not having
regular smears before the hysterectomy, it makes sense to have some kind of follow-up to make sure
that there was no CIN brewing.
Question 56.
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlanePage 21 of 25.
Women who have had hysterectomy and require follow-up with vault smears cannot be managed
within the NHSCSP. True or False?
Answer. True.
It seems daft that the programme does not continue to care for them, but section 9.6 states: “as
women who have undergone hysterectomy have no cervix, and so are no longer eligible for recall
within the NHSCSP, their vault cytology following treatment of CIN must be managed outside the
programme”.
This is messy and ripe with potential for cock-up and seems particularly daft as women who have had
sub-total hysterectomy remain within the programme! As the NHSCSP has well-proven, fail-safe
mechanisms for recall, you would have thought that common sense would have ignored semantics
and kept these women in the programme. How can highly intelligent people come up with such daft
and deficient ideas?
9.6 goes on to say that:
there must be locally-agreed policies for dealing with these women,
responsibility … will rest with the gynaecologist and will be informed by the local lead
colposcopist
any gynaecologist discharging a patient … should ensure that the GP receives specific written
guidance for follow up
the clinician in charge (gynaecologist or GP) will be responsible for failsafe mechanisms …
… cases of incomplete excision, a high risk group … will be dealt with by the colposcopy clinic
follow up arrangements
… will be agreed locally, along with any failsafe arrangements.
there is no national guidance on how this should be achieved.
… will be based on consultation with the local screening service, local screening leads, the
lead colposcopist and local GPs.
What an imbroglio, when all of this could have been dealt with easily by the well- established and
well-oiled machinery of the NHSCSP!
I have rather laboured the point, but I bet there are marks in the system for this point and I’m sure
you will now remember it forever and probably curse me when it comes to mind in the middle of the
night.
Question 57.
A woman who was not on normal recall has hysterectomy for menorrhagia. There is evidence of
completely excised CIN3 on histology. What follow-up would you recommend?
Answer. AA. None of the above. The type of recall is irrelevant. She should have vault smears at 6 and
18 months and then be discharged.
CPM16 section 10.5 says: “women who … have completely excised CIN should have vaginal vault
cytology at six and 18 months following their hysterectomy”.
Question 58.
A woman who was not on normal recall has hysterectomy for menorrhagia. There is evidence of
incompletely excised CIN3 on histology. What follow-up would you recommend?
Answer. AA. The type of recall is irrelevant. She needs vault smears at 6 and 12 months then
annually until she has had 10 years’ follow-up or reaches the age of 65, whichever is later. As noted
above, once the cervix has been removed, the woman is outside the NHSCSP and will not be sent
appointments. Local arrangements must be made to provide the follow-up.
Question 59.
A woman is referred with severe dyskaryosis, but colposcopy is normal. What follow-up should be
recommended?
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlanePage 22 of 25.
Answer. AA. CPM16 section 10.6.1 says: “women with high-grade dyskaryosis who have a
colposcopically low grade lesion … and who are not treated should have multiple biopsies. If CIN 1 or
less is confirmed, colposcopic and cytological follow up at six months is advised. Cases with
unexplained high-grade dyskaryosis should be discussed at multidisciplinary meetings”.
Question 60.
A woman has FIGO stage 1a1 cervical cancer. She wishes to retain her fertility. Which of the following
treatments should be offered?
A brachytherapy
B cone biopsy
C cryocautery
D laser ablation
E LLETZ
F radical trachelectomy
G simple trachelectomy
Answer. B + F + G. CPM16 has the following about FIGO stage1a1 in section 8.7.1: “FIGO stage Ia1 can
be managed by local excisional techniques if:
the excision margins are free of CIN and invasive disease
the gynaecological cancer centre pathologist and MDT have reviewed the histology”.
Brachytherapy, cryocautery and laser ablation preclude histological examination. Cone biopsy would
carry the least risk to her potential fertility as trachelectomy has a higher risk of causing premature
delivery. The risks are discussed in a BMJ editorial by Ioannis Biliatis. BMJ 2016;354:i4027. It is open
access and draws on an open access meta-analysis by Kyrgiou et al. BMJ 2016;354:i3633. The main
conclusions were that women with CIN have an increased risk for premature labour even without
treatment. The risk increases with treatment, with excision having more risk than ablation. Adverse
outcomes increase with increasing depth of cone biopsy and more than one treatment.
Relative risks of delivery at < 37 weeks.
Treatment Relative risk
cold knife conisation 2.70
laser conisation 2.11
excision method not specified 2.02
LLETZ 1.56
> 1 treatment compared with no treatment 13.2
cone depth ≤10-12 mm 7.1% v 3.4%
cone depth ≥10-12 mm 9.8% v 3.4%
cone depth ≥15-17 mm 10.1% v 3.4%
cone depth ≥20 mm 10.2% v 3.4%
I don’t think you will be asked the details of these figures, but remember the watershed figure of
cone depth ≥10-12 mm.
Question 61.
A woman has local excision for early cervical cancer. What follow-up should be arranged by the
NHSCSP?
A colposcopy and smears six monthly for 1 year, then annually for 9 years
B colposcopy and smears six monthly for 2 years, then annually for 8 years
C smears six monthly for 1 year, then annually for 9 years
D smears six monthly for 2 years, then annually for 8 years
E smears six monthly for 5 years, then annually for 5 years
F none of the above
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlanePage 23 of 25.
Answer. AA. None of the above. Trick question. It depends on whether or not the cervix was excised.
CPM16 says that the NHSCSP does not deal with a woman whose cervix has been removed – she
remains the responsibility of the gynaecological oncologist who arranges follow up.
CPM16 says in section 9.6 includes: “women who have trachelectomy … should remain under the
care … their treating gynaecologist or . Follow up is recommended with colposcopy and cytology;
owing to the limited information on outcome, however, all cases should be subject to local audit. As
these women have cancer they are under the individual care of a gynaecologist and are no longer
within the NHSCSP”.
Question 62.
A woman has conservative treatment for early stage cancer of the cervix. What follow-up should be
recommended?
Answer. AA. None of the above. We don’t have enough information. Crucially, was the cervix
removed? What about the histology: was it squamous or adenocarcinoma? What was the stage of
the disease or the treatment done?
CPM16 has the following about FIGO stage1a1 in section 8.7.1: “FIGO stage Ia1 can be managed by
local excisional techniques if:
the excision margins are free of both CIN and invasive disease
the gynaecological cancer centre pathologist and MDT have reviewed the histology”.
If CIN extends to the excision margin, a repeat excision should be performed to confirm complete
excision and to exclude invasive disease. This should be performed even if hysterectomy is planned …
CPM also says: “Variation in histological diagnosis of microinvasive disease is well recognised and all
cases should be reviewed by an independent pathologist”
For stages Ia2/Ib it says the following. “If conservative management for Ia2/Ib1 disease was by simple
or radical trachelectomy, cytological follow up is determined by the management policy of the
gynaecological oncologist”. Section 9.6 includes: “women who have radical trachelectomy, as part of
conservative management of cervical cancer, should remain under the care and guidance of their
treating gynaecologist or gynaecological oncologist. Follow up is recommended with colposcopy and
cytology; owing to the limited information on outcome, however, all cases should be subject to local
audit. As these women have cancer they are under the individual care of a gynaecologist and are no
longer within the NHSCSP”.
Question 63.
Which, if any, of the following statements are true in relation to pregnancy?
A routine smear tests should be deferred until after delivery
B colposcopy requires more expertise than in the non-pregnant
C all smears suggesting CIN should have initial colposcopic assessment in
late 1st. or early 2nd. trimester
D women with low-grade changes who have been referred to colposcopy
because of a +ve HPV test can had colposcopy delayed until after delivery
E if CIN1 is diagnosed, follow-up can be delayed until after delivery
F “test of cure” appointments after treatment of CIN 2 or 3 can be deferred
until after delivery
G follow-up assessment after treatment of CGIN can be left until after the
delivery if the excision margins were disease-free.
H the risk of haemorrhage after LLETZ is about 25%
Answer. A + B + C + D + H are true. F + G are false.
dCPM16. Section 11.1.1
• if a woman has been called for routine screening … the test should be deferred
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlanePage 24 of 25.
• a woman with abnormal cytology should undergo colposcopy in late 1 st. or early 2nd. trimester …
for low-grade changes triaged on the basis of a +ve HPV test, the assessment may be delayed
until after delivery
• if a previous colposcopy was abnormal and … the woman becomes pregnant, colposcopy should
not be delayed
• if a pregnant woman requires colposcopy or cytology after treatment (or follow-up of untreated
CIN1), her assessment may be delayed until after delivery… assessment should not be delayed if
the first follow-up cytology or colposcopy is due following treatment for CGIN. The ‘test of cure’
appointment should not be delayed after treatment for CIN2 or CIN3 with involved or uncertain
margin …
11.1.4 Colposcopic evaluation of the pregnant woman requires a high degree of skill:
• if CIN1 or less is suspected, repeat the examination three months following delivery
• if CIN2 or CIN3 is suspected, repeat colposcopy at the end of the 2 nd trimester. If the pregnancy
has already advanced beyond that point, repeat three months following delivery
• if invasive disease is suspected clinically or colposcopically, a biopsy … is essential. Cone, wedge,
and diathermy loop biopsies are all associated with a risk of haemorrhage and … biopsies should
be taken only where appropriate facilities to deal with haemorrhage are available. Punch biopsy
suggesting CIN only cannot reliably exclude invasion
Evidence: case series of biopsies taken by diathermy loop in pregnancy have shown risk of
haemorrhage is in the order of 25%. Case series of women with low-grade disease confirm the safety
of deferring further follow-up until postpartum period.
Manchester MRCOG Tutorial Group www.drcog-mrcog.info Tom McFarlanePage 25 of 25.
You might also like
- CIN SeminarDocument53 pagesCIN SeminarA PoudelNo ratings yet
- Pre Mal Dis of CervixDocument44 pagesPre Mal Dis of CervixnoreenfatimamaanNo ratings yet
- Cervical CancerDocument38 pagesCervical Cancerreema.saleh123No ratings yet
- Management of Cervical Smears GoldenDocument47 pagesManagement of Cervical Smears GoldenFelixNo ratings yet
- Belle Cervical DiseaseDocument7 pagesBelle Cervical DiseaseRashed ShatnawiNo ratings yet
- 1 CervixDocument12 pages1 Cervixzianab aliNo ratings yet
- Cervical DysplasiaDocument4 pagesCervical DysplasiaCarleta StanNo ratings yet
- Cervical Cancer ScreeningDocument25 pagesCervical Cancer ScreeningDr VermaNo ratings yet
- CACXDocument34 pagesCACXMax ZealNo ratings yet
- Milla Kviatkovsky, OMS-III, April 2013Document23 pagesMilla Kviatkovsky, OMS-III, April 2013api-210786702No ratings yet
- Colposcopy, Cervical Screening, and HPV, An Issue of Obstetrics and Gynecology Clinics (The Clinics - Internal Medicine)Document155 pagesColposcopy, Cervical Screening, and HPV, An Issue of Obstetrics and Gynecology Clinics (The Clinics - Internal Medicine)Annca RoXanna100% (1)
- Benign and Premalignant Disease of The CervixDocument23 pagesBenign and Premalignant Disease of The CervixJ.V. Siritt ChangNo ratings yet
- CERVICAL CANCER SeminarDocument15 pagesCERVICAL CANCER SeminarAkinsoun MotunrayoNo ratings yet
- Cervical Cancer Prevention & Management of Pre-Malignant LesionsDocument41 pagesCervical Cancer Prevention & Management of Pre-Malignant LesionsMichaelNo ratings yet
- Cervical Screening EssentialsDocument7 pagesCervical Screening Essentialsdoc moNo ratings yet
- Cervical Cancer Church PresentationDocument48 pagesCervical Cancer Church Presentationbande_adegboyegaNo ratings yet
- 1 Cervical and Vaginal CytologyDocument63 pages1 Cervical and Vaginal Cytologynanxtoyah100% (1)
- Group Health EducationDocument20 pagesGroup Health EducationBrijesh Yadav100% (1)
- Praktikum Reproduksi 2Document46 pagesPraktikum Reproduksi 2Andika Tatag100% (1)
- Adnexal Masses in Pregnancy: An Updated Review: Key Words: Adnexa, Management, Mass, Pregnancy, SurgeryDocument7 pagesAdnexal Masses in Pregnancy: An Updated Review: Key Words: Adnexa, Management, Mass, Pregnancy, SurgeryPamela laquindanumNo ratings yet
- Fast Facts: Advanced Cutaneous Squamous Cell Carcinoma for Patients and their Supporters: Information + Taking Control = Best OutcomeFrom EverandFast Facts: Advanced Cutaneous Squamous Cell Carcinoma for Patients and their Supporters: Information + Taking Control = Best OutcomeNo ratings yet
- 8-Cervical CancerDocument45 pages8-Cervical CancerBekeNo ratings yet
- Role of Primary Care Physician in OncologyDocument73 pagesRole of Primary Care Physician in OncologyTushar PatilNo ratings yet
- Cervical OncologyDocument17 pagesCervical OncologyNalin AbeysingheNo ratings yet
- 1 - Cervical CancerDocument87 pages1 - Cervical Cancerzuzuyasi65No ratings yet
- Pap TestDocument24 pagesPap TestAmirah MuhammadNo ratings yet
- Cervix Uteri1Document5 pagesCervix Uteri1twiggy484No ratings yet
- gtg62 021211 OvarianmassesDocument14 pagesgtg62 021211 OvarianmassesMaryamNo ratings yet
- C. Nodal Status: A. Mitotic Number B. GradeDocument46 pagesC. Nodal Status: A. Mitotic Number B. GradeOstazNo ratings yet
- Colposcopy: Prof. M. AddarDocument58 pagesColposcopy: Prof. M. AddarAvnish KumarNo ratings yet
- Pre Malignant and Malignant Lesions of Cervix: Gynaec Unit 5Document147 pagesPre Malignant and Malignant Lesions of Cervix: Gynaec Unit 5FarazNo ratings yet
- Bab Ii Tinjauan PustakaDocument7 pagesBab Ii Tinjauan PustakaDMdewiNo ratings yet
- PNP NCM 103Document6 pagesPNP NCM 103Mark Joseph Mabazza LappayNo ratings yet
- Ovarian Cancer Notes - G7 3BSN1Document52 pagesOvarian Cancer Notes - G7 3BSN1Shyne HazyNo ratings yet
- Application of Exfoliative Cytology in Obstetrics & GynaecologyDocument20 pagesApplication of Exfoliative Cytology in Obstetrics & Gynaecologyapi-3705046100% (3)
- OvaryDocument4 pagesOvaryCarolina MartinezNo ratings yet
- Endometrial CarcinomaDocument6 pagesEndometrial CarcinomaĶHwola ƏľsHokryNo ratings yet
- Tumor PayudaraDocument53 pagesTumor PayudaraBeivyNo ratings yet
- Correlation of PAP Smear Findings With Clinical Findings and Cervical BiopsyDocument7 pagesCorrelation of PAP Smear Findings With Clinical Findings and Cervical BiopsyKavita Saxena KhareNo ratings yet
- Intraepithelial Neoplasia of The Lower Genital TractDocument54 pagesIntraepithelial Neoplasia of The Lower Genital TractDee SarajanNo ratings yet
- Cervical CancerDocument7 pagesCervical CancerLarisse de LeonNo ratings yet
- Ca Cervix: Shabana R Anchu Mariam CharlyDocument53 pagesCa Cervix: Shabana R Anchu Mariam CharlySuci Rahayu EvashaNo ratings yet
- Pap SmearsDocument28 pagesPap Smearskhadzx100% (2)
- Management of AISDocument10 pagesManagement of AISMaría Reynel TarazonaNo ratings yet
- Lesson Plan On TumorsDocument19 pagesLesson Plan On TumorsPuneetNo ratings yet
- The Bethesda and EvaluationDocument5 pagesThe Bethesda and Evaluationvyvie89No ratings yet
- 10 Cervical NeoplasiaDocument33 pages10 Cervical NeoplasiaDawit g/kidanNo ratings yet
- Cervical Cancer: Predominately Squamous Cell CancerDocument1 pageCervical Cancer: Predominately Squamous Cell CancerAila CamachoNo ratings yet
- ONCOLOGICAL GYNECOLOGY - Malignant Tumors of The Vagina and Modalities of TreatmentDocument9 pagesONCOLOGICAL GYNECOLOGY - Malignant Tumors of The Vagina and Modalities of TreatmentVesna AntovskaNo ratings yet
- Cervical CancerDocument6 pagesCervical CancerJohndave CazarNo ratings yet
- Cervical CancerDocument28 pagesCervical CancerAmlan jyoti thanapatiNo ratings yet
- Carcinoma BreastDocument8 pagesCarcinoma BreastYeshvi s100% (1)
- Care For Women: With Ovarian, Cerviacl, Vulvar and Endometrial CancerDocument26 pagesCare For Women: With Ovarian, Cerviacl, Vulvar and Endometrial CancerAhmad JradeenNo ratings yet
- Cytology FinalDocument68 pagesCytology FinalamyNo ratings yet
- Endometrial CancerDocument16 pagesEndometrial CancerSusan Powell-ProctorNo ratings yet
- Breast Cancer: Dr. Armando V. Tan AnatomyDocument9 pagesBreast Cancer: Dr. Armando V. Tan AnatomyJennifer Dumaluan AtaNo ratings yet
- Committee 3: Diagnostic Terminology: BackgroundDocument36 pagesCommittee 3: Diagnostic Terminology: BackgroundDaniel KurtyczNo ratings yet
- Review Adnexal Masses Pregnancy Rcog PDFDocument6 pagesReview Adnexal Masses Pregnancy Rcog PDFRosália Coutada100% (1)
- An Are PortDocument18 pagesAn Are PortKirsten NVNo ratings yet
- Soul Voice Oldies Watz Xiao Yu Zhong BianDocument1 pageSoul Voice Oldies Watz Xiao Yu Zhong BianassssadfNo ratings yet
- Breast+endocrine Surg-EMQ-18Document18 pagesBreast+endocrine Surg-EMQ-18assssadfNo ratings yet
- TX Sba-10Document10 pagesTX Sba-10assssadfNo ratings yet
- Vascular Surgery EMQ 28Document28 pagesVascular Surgery EMQ 28assssadfNo ratings yet
- 222Document19 pages222assssadfNo ratings yet
- Emergency traumaEMQ34Document34 pagesEmergency traumaEMQ34assssadfNo ratings yet
- CPG Medical StudentsDocument33 pagesCPG Medical StudentsKalichandren ArumugamNo ratings yet
- Pic RollDocument8 pagesPic RollsocnewNo ratings yet
- Clean CVDocument1 pageClean CVnaveenbala100% (1)
- Final Year Medicine CS TayDocument5 pagesFinal Year Medicine CS TayassssadfNo ratings yet
- VJ Bible 2Document199 pagesVJ Bible 2Michael Liu89% (19)
- Phase 3A 14-15 (Week 21-53)Document27 pagesPhase 3A 14-15 (Week 21-53)assssadfNo ratings yet
- SettingsDocument2 pagesSettingsPhinwegNo ratings yet
- Breast LumpDocument1 pageBreast LumpassssadfNo ratings yet
- Definition: Stoma Means 'Mouth' or 'Opening'. in Medicine, It Indicates That There Is AnDocument3 pagesDefinition: Stoma Means 'Mouth' or 'Opening'. in Medicine, It Indicates That There Is AnassssadfNo ratings yet
- Ultrasound Showing Uterus and Tubal PregnancyDocument58 pagesUltrasound Showing Uterus and Tubal PregnancyassssadfNo ratings yet
- Greetings: Ní Hâo Zâo Än Wû Än Wân Än Wân Än Wô Néng Gën Nî Jiâng Huã Mä Jïn Tiän Hâo Diân Lè Méi YôuDocument29 pagesGreetings: Ní Hâo Zâo Än Wû Än Wân Än Wân Än Wô Néng Gën Nî Jiâng Huã Mä Jïn Tiän Hâo Diân Lè Méi YôuassssadfNo ratings yet
- OSCES MarkingDocument125 pagesOSCES Markinghy7tn100% (5)
- OSCE GynecologyDocument55 pagesOSCE GynecologySyahmi Yahya88% (8)
- CTGDocument3 pagesCTGassssadfNo ratings yet
- Full Report A-1Document35 pagesFull Report A-1assssadfNo ratings yet
- Paediatric Blood TransfusionDocument4 pagesPaediatric Blood TransfusionassssadfNo ratings yet
- Obgyn Advice DocumentDocument6 pagesObgyn Advice DocumentthatshipcreighNo ratings yet
- Tutorial On Basic ObstetricDocument1 pageTutorial On Basic ObstetricassssadfNo ratings yet
- Guide For Physical ExaminationsDocument18 pagesGuide For Physical ExaminationsassssadfNo ratings yet
- Authentication Slip Printing ServicesDocument5 pagesAuthentication Slip Printing ServicesassssadfNo ratings yet
- CPCils With AnswersDocument87 pagesCPCils With AnswersassssadfNo ratings yet
- The Use of Blood Products EditDocument39 pagesThe Use of Blood Products EditassssadfNo ratings yet
- Introduction To ABO Blood GroupsDocument39 pagesIntroduction To ABO Blood GroupsassssadfNo ratings yet
- INTRODUCTION TO PROGRAMMING Exam QuestionsDocument30 pagesINTRODUCTION TO PROGRAMMING Exam Questionshorrett100% (4)
- Course Outline Math 221C Advanced AlgebraDocument1 pageCourse Outline Math 221C Advanced Algebraherbertjohn2450% (2)
- Suitcase Lady Christie Mclaren ThesisDocument7 pagesSuitcase Lady Christie Mclaren ThesisWriteMyPaperForMeCheapNewHaven100% (2)
- Notes On The "Historical Turn" and The Uses of Theory in Film Studies - ARTDocument7 pagesNotes On The "Historical Turn" and The Uses of Theory in Film Studies - ARTaarmherNo ratings yet
- Chapter 2: Demand, Supply & Market EquilibriumDocument15 pagesChapter 2: Demand, Supply & Market EquilibriumRaja AfiqahNo ratings yet
- Spiderman EvolutionDocument14 pagesSpiderman EvolutionLuis IvanNo ratings yet
- Test Bank For Essentials of Human Development A Life Span View 2nd Edition by KailDocument24 pagesTest Bank For Essentials of Human Development A Life Span View 2nd Edition by Kailmichaelwatson05082003xns100% (47)
- Brochure 1st RMLNLU Kochhar Co. Arbitration Moot Court Competition 2023Document21 pagesBrochure 1st RMLNLU Kochhar Co. Arbitration Moot Court Competition 2023Rishi Raj MukherjeeNo ratings yet
- Thesis Project Management SoftwareDocument7 pagesThesis Project Management Softwarehollyschulzgilbert100% (2)
- Lesson Plan (Kinder1)Document3 pagesLesson Plan (Kinder1)MadelNo ratings yet
- Certified Quality Director - CQD SYLLABUSDocument3 pagesCertified Quality Director - CQD SYLLABUSAnthony Charles ANo ratings yet
- Education Is The Foundation For Women Empowerment in IndiaDocument111 pagesEducation Is The Foundation For Women Empowerment in IndiaAmit Kumar ChoudharyNo ratings yet
- HRA Strategic PlanDocument40 pagesHRA Strategic PlanjughomNo ratings yet
- The Meaning of LifeDocument1 pageThe Meaning of LifeJayas SharmaNo ratings yet
- Presentation Management Trainee Batch VII - Mohammad Arian RahmatullahDocument8 pagesPresentation Management Trainee Batch VII - Mohammad Arian RahmatullahMohammad Arian RahmatullahNo ratings yet
- CASE ANALYSIS PretDocument4 pagesCASE ANALYSIS PretNate Dela CruzNo ratings yet
- 03 9609 12 MS Prov Rma 08022023111718Document18 pages03 9609 12 MS Prov Rma 08022023111718Kalsoom SoniNo ratings yet
- Manila Jocky Club Vs CADocument20 pagesManila Jocky Club Vs CAryusuki takahashiNo ratings yet
- Wdnsakn KDniend w5564Document8 pagesWdnsakn KDniend w5564Jo BloNo ratings yet
- Tugas Pak Hendro PoemDocument24 pagesTugas Pak Hendro PoemLaila LalaNo ratings yet
- Quarter 4 Week 4 Parallel Lines Cut by A TransversalDocument26 pagesQuarter 4 Week 4 Parallel Lines Cut by A TransversalZaldy Roman MendozaNo ratings yet
- Estimation of Barium From Barium Sulphate GravimetricallyDocument4 pagesEstimation of Barium From Barium Sulphate GravimetricallyMg H67% (15)
- Elliot Kamilla - Literary Film Adaptation Form-Content DilemmaDocument14 pagesElliot Kamilla - Literary Film Adaptation Form-Content DilemmaDavid SalazarNo ratings yet
- Sword Art Online - Unital Ring IV, Vol. 25Document178 pagesSword Art Online - Unital Ring IV, Vol. 257022211485aNo ratings yet
- Delhi Public School, Agra: The HolocaustDocument3 pagesDelhi Public School, Agra: The Holocaustkrish kanteNo ratings yet
- Incremental and TwiceDocument12 pagesIncremental and TwiceAgung KaryawinaraNo ratings yet
- Fornilda vs. Br. 164, RTC Ivth Judicial Region, PasigDocument11 pagesFornilda vs. Br. 164, RTC Ivth Judicial Region, PasigJenny ButacanNo ratings yet
- Dark Enemies by Effie CampbellDocument250 pagesDark Enemies by Effie Campbellsheenuyadav06080No ratings yet
- River: A Boon or A BaneDocument3 pagesRiver: A Boon or A BaneIJELS Research JournalNo ratings yet
- Basic English: Unit 14 Guidelines Leisure ActivitiesDocument5 pagesBasic English: Unit 14 Guidelines Leisure ActivitiesDeyan BrenesNo ratings yet