Professional Documents
Culture Documents
Bone and Parathyroid Metabolism
Uploaded by
Cyner Cruz0 ratings0% found this document useful (0 votes)
37 views6 pagesBone and Parathyroid Metabolism handouts
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentBone and Parathyroid Metabolism handouts
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
37 views6 pagesBone and Parathyroid Metabolism
Uploaded by
Cyner CruzBone and Parathyroid Metabolism handouts
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 6
that they begin to discharge spontaneously,
BONE AND PARATHYROID METABOLISM
CALCIUM
Dr. Labrador
Normal Values: 9.4 mg/dl or 2.4 mmol/L initiating trains of nerve impulses that pass
Hypercalcemia - CNS DEPRESSION to the peripheral skeletal muscles
Hypocalcemia -CNS STIMULATION 9.4 mg/dL to 6 mg/dL - lethal at 4 mg/dL
Seizures
Total Body Calcium Increasing excitability in the brain
ECF - 0.1% Laboratory animals
Cells - 1% Marked dilatation of the heart
Bones - 98.9% (largest reservoir of calcium) Changes in cellular enzyme activities
Increased membrane permeability in some
Complexed - 10% cells
Protein-bound - 40% Impaired blood clotting
Ionized - 50%
Carpopedal spasm
CALCIUM in Plasma Tetany in the hand
Usually occurs before tetany develops in
With anions Nondiffusible most other parts of the body
(41%) thru
membrane
HYPERCALCEMIA
Protein-bou Diffusible Unionized
Abnormal neurologic function that involves
nd (9%)
muscle weakness, depression, confusion, coma
Ionized Diffusible Ionized Gastrointestinal disturbances
(50%) Functional EKG abnormalities (shortening of QT interval)
Normal levels: 1.2 mmol/L or 2.4 mEq/L Kidney abnormalities: kidney stones
One half of total plasma Ca concentration Cause CNS depression
PHOSPHATE Sluggish reflexes
Lack of appetites, constipation-depressed
contractility of GIT muscles
Forms Concent Acidic Basic Symptoms at 12 mg/dL-15 mg/dL
ration Calcium crystals at 17 mg/dL
HPO4 1.05 Increased decreased
mmol/L INTESTIAL ABSORPTION AND FECAL EXCRETION OF CA
H2PO4 0.26 Decreased Increased
mmol/L Normal intake: 1000 mg/day each for calcium
and phosphorus = approx. 1 liter of milk
Divalent cations such as calcium ions are poorly
absorbed from the intestines
HYPOCALCEMIA Vitamin D promotes calcium absorption by the
Difficulty in determining levels of each intestines
NV: 3-4 mg/dL (adults): 4-5 mg/dL (children) About 35% (350 mg/day) of the ingested calcium
usually is absorbed
Nervous system excitement and tetany Ca remaining in the intestine excreted in the
Increased neuronal membrane permeability to feces
sodium ions, allowing easy initiation of action Additional 250 mg/day of calcium enters the
potentials. intestines via secreted gastrointestinal juices and
Tetany sloughed mucosal cells
50% below normal level About 90% (900 mg/day) of the daily intake of
Peripheral nerve fibers become so excitable Ca excreted in the feces
Intestinal absorption occurs very easily
A small portion excreted in the feces in 5-10% (ground substance)-controls Ca
combination with nonabsorbed Ca deposition
Almost all the dietary phosphate absorbed into 90-95%-(collagen)-strength
the blood fro the gut and alter excreted in the Collagen
urine Provides tensile and compressional strength
RENAL EXCRETION OF Ca Ground substance
About 10% (100mg/dL) of the ingested Ca Composed of extracellular fluid plus
excreted in the urine proteoglycan, especially chondroitin sulfate
About 41% of the plasma Ca is bound to plasma and hyaluronic acid
proteins and is therefor not filtered by the The precise function of each of these are not
glomerular capillaries known, although they do help control the
The rest is combined with anions such as deposition of Ca salts.
phosphate (9%) or ionized (50%) and is filtered
through the glomeruli into the renal tubules. Bone salts
Mainly Ca and phosphate
RENAL EXCRETION OF PHOSPHATE Hydroxyapatite-major crystals
Controlled by an overflow mechanism
When phosphate concentration in the plasma Magnesium, sodium, potassium and carbonate
is belwo the critical value of about 1 mmol/L, Believed to be conjugated to the
all the phosphate in the glomerular filtrate is hydorxyapatite crystals rather than organized
reabsorbed and no phosphate is lost int the into distinct crystals of their own
urine
But above this critical concentration, the rate Contain a type of exchangeable Ca that is always
of phosphate loss is directly proportional to in equilibrium with Ca ions in ECF
the additional increase. Osteoblasts-bone deposition
Thus, the kidneys regulate the phosphate Osteoclasts-bone reabsorption
concentration in the extracellular fluid by
altering the rate of phosphate excretion in TENSILE AND COMPRESSIONAL STRENGHT OF BONE
accordance with the plasma phosphate
concentration and the rate of phosphate These combined properties plus the degree of
filtration by the kidneys bondage between the collagen fibers and the
PTH can greatly increase phosphate crystals provide a bony structure that has both
excretion by the kidneys extreme tensile strength and extreme
PTH plays an important role in the control of compressional strength.
plasma phosphate concentration as well as Collagen fibers of bone
Ca concentration Have great tensile strength
Ca salts
BONE Have great compressional strength
Composed of a tough organic matrix greatly Hydroxyapatite
strengthened by deposits of Ca salts Does not precipitate in extracellular fluid
Average compact bone by weight is approx. 30% despite supersaturation of Ca and phosphate
matrix, 70% salts ion
Newly formed bone - higher percentage of Pyrophosphate-prevent precipitation
matrix in relation to salts Fail to precipitate in normal tissues except in
Functions: bone despite the state of supersaturation of
Structural the ions
Major role in Ca, Phosphorus, Magnesium
homeostasis (reservoir)
Source of numerous growth factors, BONE REMODELING
cytokines, prostaglandins involved in bone Occurs through coordinated coupling of bone
formation and resorption resorption and bone formation in bone
remodeling units (osteons) osteoblastic deposition and calcification of bone
3-8 months Bone stress also determines the shape of bones
10% total bone mass/year under certain circumstances
Bone ordinarily adjusts its strength in proportion If a long bone of the leg breaks in it center and
to the degree of bone stress (bone thicken when then heals at an angle, the compression stress on
subjected to heavy loads) the inside of the angle causes increased
Even the shape of the bone can be rearranged for deposition of bone, and increased absorption
proper support of mechanical forces by occurs on the outer side of the angle where the
deposition and absorption of bone in accordance bone is not compressed
with stress patterns.
Old bone becomes relatively brittle and weak, REPAIR OF FRACTURE ACTIVATES OSTEOBLASTS
new organic matrix is needed as the organic
matrix degenerates so the normal toughness of
Osteoprogenitor cells
bone is maintained
Bones stem cells in the surface tissue lining
Bones of children-rapid rates of deposition and
bone
absorption
Callus-new organic matrix followed shortly
Bones of the elderly - rates of deposition and
by the deposition of Ca salts
absorption are slow
Many bone surgeons use the phenomenon of
Ca PRECIPITATION IN NONOSSEOUS TISSUES UNDER
bone stress to accelerate the rate of fracture
ABNORMAL CONDITIONS
healing
Ca salts almost never
Use of special mechanical fixation
precipitate in normal tissues besides except in
apparatuses for holding the ends of the
abnormal conditions
broken bone together so that the patient can
Precipitate in arterial walls-arteriosclerosis
continue to use the bone immediately
(arteries become bonelike tubes)
Calcium salts deposits in degenerating tissues or
in old blood cells VITAMIN D
Increase Ca absorption from the GIT
EXCHANGEABLE CALCIUM Effects on bone deposition and absorption
Present in bones Not an active substance, has to be converted to
Always in equilibrium with the Ca ions in the active form 1,25(OH)2D3.
extracellular fluids 7-dehydrocholesterol
Within 30 minutes - 1 hour or more, Ca ion Occurs primarily in keratinocytes
concentration returns to normal 7-DHC most abundant
Provides a rapid buffering mechanism to keep Pre vitamin D3
the calcium ion concentration in the extracellular Cleavage of carbon bonds between carbons 9
and 10
fluids from rising to excessive levels or falling to
Thermally labile previtamin D3
very low levels under transient conditions of Undergoes temp dependent rearrangement into
excess or decreased availability of Ca. vitamin D3
UV light also converts previtamin D3 to inert products
(lumisterol and tachysterol)
RATE OF BONE DEPRESSION BY BONE "STRESS" > Prolonged sun exposure does not cause vitamin D
Bone is deposited in proportion to the intoxication
compressional load that the bone must carry. SYNTHESIS OF CALCITROL
Bone of athletes-heavier than those of
nonathletes Not tightly regulated
One leg in a cast-the bone of the leg in the cast Reflects increases in vitamin D3 or ingestion of Vitamin
becomes thin, as much as 30% decalcified within D or vitamin D deficiency
Biologically inert
a fe weeks; the opposite bone remains thick and
normally calcified.\
Therefore, continual physical stress stimulates
Vitamin D concentrations for hydroxyapatite deposition into
Steps matrix
1. Cholecalciferol (vitamin D3) is formed in the skin
2. Vit D3 converted to 25(OH) cholecalciferol in the liver Actions of Vitamin D
First step in activation of cholecalciferol Increase serum calcium
Limited by negative feedback Increase serum phosphate
Feedback Control Normal bone mineralization
a) precisely regulates 25-hydroxycholecalciferol VITAMIN D DISORDERS
b) Conserved vit D stored in the liver for future use incr - increase
decr – decrease
3. Formation of 1,15(OH)2D3 in the kidneys and its Ca PO PTH
control by PTH Excess incr incr decr
Proximal renal tubules Vitamin D
Absence of kidneys cancels effects of vitamin D
Vitamin D decr decr incr
4. Ca ion concentration controls formation of deficiency
1,25(OH)2D3
Inversely affected by plasma Ca concentration PARATHYROID HORMONE
Reasons
4 in humans
a) Ca ions has slight effect in prevention conversion of
Located immediately behind the thyroid gland
25-dehydrocolecalciferol ----- 1,25(OH)2D3
(one behind each of the upper and lower poles)
b) At low Ca levels, PTH promotes conversion of
25-hydroxycholecalciferol ------ 1,25(OH)2D3 6 mm long, 3mm wide, 2 mm think
Grossly dark brown fat
Actions
Histology
Promote intestinal Ca absorption
Epithelial cells
Promotes phosphate absorption by the GIT
- Chief
Decreases renal Ca and phosphate excretion
- Oxyphil
Effects on bone and ratio to PTH Stromal cells
Actions of Vitamin D on the Gut Parathyroid Hormone
Increases intestinal absorption f Calcium and - Contains mainly chief cells that secrete PTH
Phosphorus - Oxyphil cells absent in humans and many animals
Increases synthesis of calbindin(calcium binding - MW 9,500
protein
Decreases renal Can ad Phosphate excretion Effects
- Weak effect - Increases Ca and PO absorption from the bone
- Decreases Ca excretion and increase phosphate
Vitamin D effects on bone and relation to PTH excretion by the kidneys
Extreme amounts of Vit D causes absorption of - Increases intestinal absorption of Ca and PO
bone - Decreases Ca excretion and increases PO
In the absence of Vit D PTH effects greatly excretion by the kidneys
reduced or prevented o Diminished proximal tubular reabsorption
Effect of 1,25(OH)2D3 to increase Ca transport of phosphates
thru membranes o Increase renal tubular reabsorption of Ca
Small amounts of vitamin D promotes bone
calcification PTH ACTIONS ON KIDNEYS CALCIUM AND
Increase ca and phosphate absorption from GIT PHOSPHATE
Effect of 1,25(OH)2D3 to increase Ca transport 1. Increases calcium reabsorption in ascending loop and
thru membranes (opposite effect) distal tubule
- BUT due to increase in filtered load
Direct effect: stimulates bone resorption hypercalciuria kidney stones
Synergistic with PTH 2. Decreases reabsorption of phosphate in proximal tubule
activates osteoclast via osteoblast phosphaturia decreases serum phosphate
Indirect effect: maintains normal ECF Ca and PO4 - Calcium phosphate ion product
Days to weeks – increase proliferation of PTH
Effects
Increases intestinal absorptoion of CA and PO REGULATION OF PTH: PHOSPHATE
- Increased formation of 1,25(OH)2D3 in the Increase phosphate
kidneys Decrease in ionized calcium
- Mediated by cAMP 2nd messenger mechanism Increase in PTH secretion
PTH actions in the kidneys Effects of Calcitrol
1. Increased synthesis of 1,25(OH)2D (cacitrol) via o Decrease in PTH gene transcription
activation of 1a hydroxylase indirectly stimulates o Decrease in PTH secretion
intestinal absorption of Calcium o Decrease in PT cell proliferation
2. Decreases renal bicarbonate reabsorption non-gap
metabolic acidosis PARATHYRIOD HORMONE RELATED PROTEIN (PTHrP)
o Homologous to PTH and binds to PTH receptor
- Ca ion concentration controls PTH secretion with equivalent affinities
- Conditions causing hypertrophy of PT glands o Normal circulating level PTHrP ---- PTH
o Rickets o Vital functions in developmental (intrauterine,
o Pregnancy infancy) and at cell and tissue level (paracrine)
o Lactation o Major cause of hypercalcemia associated with
- Ca ion concentration controls PTH secretion malignancies (tumor production of PTHrP)
- Conditions causing diminished size of parathyroid
glands CALCITONIN
o Excess Ca in the diet
o Increased vit D in the diet\ o Peptide hormone secreted by the thyroid gland
o Bone absorption caused by factors other that o Decrease plasma Ca concentration
PTH o Has effects opposite to PTH
o Synthesis and secretion occur in the parafollicular
- Powerful mechanism for controlling ECF Ca and cells or C cells
phosphate concentrations by regulating: o Composed 0.1% of human thyroid gland
o Intestinal absorption o Remnants of ultimo brachial glands of lower
o Renal excretion animals
o Exchange between ECF and bones of these o 32-AA peptide
ions o MW 3,400
Intact PTH o Increased plasma Ca concentration stimulates
- 84 amino acids\ calcitonin secretion
- half life 2- 4 minutes o Decreases plasma Ca concentration
- cleared by liver and kidneys o Weal effect on plasma Ca concentration on adult
human
Actions of PTH o Secreted by parafollicular © cells of thyroid
o Increase serum calcium (neural crest) – 0.1 % of thyoid mass
o Decrease serum phosphate o Polypeptide 32 amino acids
o Increase 1,25(OH)2D
Increased plasma Ca concentration stimulates calcitonin
Regulation of PTH secretion secretion
- Plasma calcium level o 2nd hormonal feedback mechanism for Ca level
- Phosphate control
- Calcitrol o Relatively weak
- Magnesium o Works opposite that of PTH
TEMPORAL HIERARCHY OF PTH RESPONSE TO
HYPOCALCEMIA Decreases plasma Ca concentration
Sec – few min release of PTH o Decrease absorptive activities of osteoclasts
o Decreases formation of new osteoclast
Min – 1 hour – intracellular PTH degradation
Weak effect on plasma Ca concentration in adult human
Hours to few days – increase PTH gene expression o Any initial reduction of Ca ion concentration
caused by calcitonin leads within hours to a
powerful stimulation of PTH secretion ---
overrides the calcitonin effect
Action os Calcitonin
o Decrease serum calcium
o Decrease serum phosphate
Major effect – antagonizes effects of PTH on bone
- Decrease osteoclastic differentiation and activity
- Osteoclast receptors for calcitonin
1. Buffer function of exchangeable Ca in bones
- CaHPO4 (5-10 gm)
- 5% of all blood flows through the bones
- 50% of excess Ca in the ECF removed in 70 mins
- Mitochondria helps in maintaining Ca
concentrations
2. Hormonal control of Ca ion concentration
- Parathyroid and calcitonin hormonal systems
- Long term control resides in the PTH and vitamin
CLINICAL PRESENTATION OF PRIMARY
HYPO/HYPERPARATHYROIDISM
Ca PO Calcitrol
Hyperpara incr decr incr
Hypopara decr incr decr
Secondary Hyperparathyroidism
Rickets
- Vitamin D deficiency
- Occurs mainly in children who remain indoors
throughout winter
- Common in spring months
- Vit D Deficiency: Rickets
- Defective mineralization leads to profusion of
disorganize non mineralized cartilage, bonuy
abnormalities
You might also like
- OB Dystocia Part II and IIIDocument6 pagesOB Dystocia Part II and IIICyner CruzNo ratings yet
- Acls Manual PDFDocument30 pagesAcls Manual PDFCyner Cruz100% (2)
- Community Health NursingDocument28 pagesCommunity Health NursingCyner CruzNo ratings yet
- Gynecoid Anthropoid Android Sonogram Acceleration Deceleration Tocolytic Agent RicketsDocument137 pagesGynecoid Anthropoid Android Sonogram Acceleration Deceleration Tocolytic Agent RicketsCyner Cruz100% (1)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Chapter 2 ProblemsDocument6 pagesChapter 2 ProblemsYour MaterialsNo ratings yet
- Chapter 3 - Organization Structure & CultureDocument63 pagesChapter 3 - Organization Structure & CultureDr. Shuva GhoshNo ratings yet
- FMC Derive Price Action GuideDocument50 pagesFMC Derive Price Action GuideTafara MichaelNo ratings yet
- Excon2019 ShowPreview02122019 PDFDocument492 pagesExcon2019 ShowPreview02122019 PDFSanjay KherNo ratings yet
- A Case Study of Coustomer Satisfaction in Demat Account At: A Summer Training ReportDocument110 pagesA Case Study of Coustomer Satisfaction in Demat Account At: A Summer Training ReportDeepak SinghalNo ratings yet
- DC 7 BrochureDocument4 pagesDC 7 Brochures_a_r_r_yNo ratings yet
- Test Your Knowledge - Study Session 1Document4 pagesTest Your Knowledge - Study Session 1My KhanhNo ratings yet
- 13 Adsorption of Congo Red A Basic Dye by ZnFe-CO3Document10 pages13 Adsorption of Congo Red A Basic Dye by ZnFe-CO3Jorellie PetalverNo ratings yet
- Turning PointsDocument2 pagesTurning Pointsapi-223780825No ratings yet
- Principals' Leadership Styles and Student Academic Performance in Secondary Schools in Ekiti State, NigeriaDocument12 pagesPrincipals' Leadership Styles and Student Academic Performance in Secondary Schools in Ekiti State, NigeriaiqraNo ratings yet
- SMR 13 Math 201 SyllabusDocument2 pagesSMR 13 Math 201 SyllabusFurkan ErisNo ratings yet
- PR KehumasanDocument14 pagesPR KehumasanImamNo ratings yet
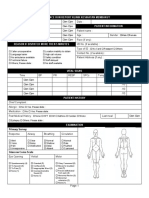
- Borang Ambulans CallDocument2 pagesBorang Ambulans Callleo89azman100% (1)
- Chemistry Test 1Document2 pagesChemistry Test 1shashankNo ratings yet
- Lecture 4 ENGR 243 DynamicsDocument45 pagesLecture 4 ENGR 243 DynamicsRobby RebolledoNo ratings yet
- Mastertop 1230 Plus PDFDocument3 pagesMastertop 1230 Plus PDFFrancois-No ratings yet
- MGMT Audit Report WritingDocument28 pagesMGMT Audit Report WritingAndrei IulianNo ratings yet
- Ob NotesDocument8 pagesOb NotesRahul RajputNo ratings yet
- Lesson PlanDocument2 pagesLesson Plannicole rigonNo ratings yet
- Unit 7: Anthropology: Q2e Listening & Speaking 4: Audio ScriptDocument6 pagesUnit 7: Anthropology: Q2e Listening & Speaking 4: Audio ScriptĐại học Bạc Liêu Truyền thông100% (1)
- Carriage RequirementsDocument63 pagesCarriage RequirementsFred GrosfilerNo ratings yet
- Environmental Economics Pollution Control: Mrinal Kanti DuttaDocument253 pagesEnvironmental Economics Pollution Control: Mrinal Kanti DuttashubhamNo ratings yet
- Business Analytics Emphasis Course GuideDocument3 pagesBusiness Analytics Emphasis Course Guidea30000496No ratings yet
- Lec 33 - Householder MethodDocument11 pagesLec 33 - Householder MethodMudit SinhaNo ratings yet
- Turn Around Coordinator Job DescriptionDocument2 pagesTurn Around Coordinator Job DescriptionMikeNo ratings yet
- 2009 2011 DS Manual - Club Car (001-061)Document61 pages2009 2011 DS Manual - Club Car (001-061)misaNo ratings yet
- Stearns 87700 Series Parts ListDocument4 pagesStearns 87700 Series Parts ListYorkistNo ratings yet
- Equivalent Fractions Activity PlanDocument6 pagesEquivalent Fractions Activity Planapi-439333272No ratings yet
- Proceeding of Rasce 2015Document245 pagesProceeding of Rasce 2015Alex ChristopherNo ratings yet
- Study 107 - The Doctrine of Salvation - Part 8Document2 pagesStudy 107 - The Doctrine of Salvation - Part 8Jason MyersNo ratings yet