Professional Documents
Culture Documents
Amen Ta 2012
Uploaded by
Alberto BrasoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Amen Ta 2012
Uploaded by
Alberto BrasoCopyright:
Available Formats
RESEARCH—HUMAN—CLINICAL STUDIES
TOPIC RESEARCH—HUMAN—CLINICAL STUDIES
Analysis of Nonmodifiable Risk Factors for
Intracranial Aneurysm Rupture in a Large,
Retrospective Cohort
BACKGROUND: The risk factors predictive of intracranial aneurysm rupture remain
Peter S. Amenta, MD* incompletely defined.
Sanjay Yadla, MD* OBJECTIVE: To examine the association between various nonmodifiable risk factors
Peter G. Campbell, MD* and aneurysm rupture in a large cohort of patients evaluated at a single institution.
Mitchell G. Maltenfort, PhD* METHODS: A retrospective analysis of patients admitted to a cerebrovascular facility
between January 2006 and 2010 with a primary diagnosis of cerebral aneurysm.
Saugat Dey, MBBS‡
Aneurysms were divided into 2 groups: unruptured or ruptured. The dome diameter,
Sayantani Ghosh, MBBS‡
aspect ratio (AR), location, sidedness, neck morphology, and multiplicity were entered
Muhammad S. Ali, MD* into a central database. A full model was constructed, and a systematic removal of the
Jack I. Jallo, MD, PhD* least significant variables was performed in a sequential fashion until only those vari-
Stavropoula I. Tjoumakaris, ables reaching significance remained.
MD* RESULTS: We identified 2347 patients harboring 5134 individual aneurysms, of which
L. Fernando Gonzalez, MD* 34.90% were ruptured and 65.09% were unruptured. On admission, 25.89% of aneur-
ysms with a dome diameter ,10 mm and 58.33% of aneurysms with a dome .10 mm
Aaron S. Dumont, MD*
were ruptured (P , .001). Of aneurysms with an AR .1.6, 52.44% presented following
Robert H. Rosenwasser, MD*
a rupture (P , .001). The highest incidence of rupture (69.21%) was observed in
Pascal M. Jabbour, MD* aneurysms with an AR .1.6, dome diameter ,10 mm, and a deviated neck. Deviated
neck-type aneurysms had a significantly greater incidence of rupture than classical neck-
*Department of Neurological Surgery,
Thomas Jefferson University, Philadel- type aneurysms (P , .001).
phia, Pennsylvania; ‡Bankura Sammilani CONCLUSION: An AR .1.6, dome diameter .10 mm, a deviated neck, and right-sid-
Medical College, University of Calcutta,
edness are independently associated with aneurysm rupture.
Bankura, West Bengal, India
KEY WORDS: Aneurysm location, Aneurysm morphology, Aneurysm size, Aspect ratio, Neck-type, Subarachnoid
Correspondence: hemorrhage
Pascal Jabbour, MD,
Department of Neurological Surgery, Neurosurgery 70:693–701, 2012 DOI: 10.1227/NEU.0b013e3182354d68 www.neurosurgery-online.com
Thomas Jefferson University,
909 Walnut St, 2nd Floor,
A
Philadelphia, PA 19107.
E-mail: pascal.jabbour@jefferson.edu neurysmal subarachnoid hemorrhage imaging quality and availability, family screening,
(SAH) incidence remains stable in the and broader surveillance the prevalence of unrup-
Received, January 18, 2011. United States, affecting approximately tured aneurysms has increased.4,5 Treatment of
Accepted, August 9, 2011. 30000 individuals each year.1 However, it con- unruptured aneurysms by coiling or clipping
Published Online, September 1, 2011.
tinues to have a devastating impact on affected carries an associated risk that must be weighed
Copyright ª 2011 by the patients with a 50% to 60% 30-day mortality against the risk of future rupture.6-8 Therefore,
Congress of Neurological Surgeons rate, and less than 60% of survivors progressed to accurate predictions of the natural history of
functional independence.1-3 With improved unruptured cerebral aneurysms are a key factor in
counseling patients for elective treatment.9,10
ABBREVIATIONS: AR, aspect ratio; CI, confidence Large collaborative studies have been conducted
interval; CTA, computed tomographic angiogra- to clarify the natural history of unruptured ane-
phy; ICA, internal carotid artery; ISUIA, Interna- urysms, including the International Study of
tional Study of Unruptured Intracranial Aneurysms; Unruptured Intracranial Aneurysms (ISUIA).
JHN, Jefferson Hospital for Neurosciences; MRA, Although aneurysm size and location were inves-
magnetic resonance angiography; PCA, posterior
tigated in the original ISUIA data and its follow-up
cerebral artery; PCOM, posterior communicating
artery; SAH, subarachnoid hemorrhage publication, other aspects of morphology were not
reported.11 Aneurysm size and location have since
NEUROSURGERY VOLUME 70 | NUMBER 3 | MARCH 2012 | 693
Copyright © Congress of Neurological Surgeons. Unauthorized reproduction of this article is prohibited.
Copyright © Congress of Neurological Surgeons. Unauthorized reproduction of this article is prohibited.
AMENTA ET AL
been substantiated as reliable predictors of rupture risk.5,7,8 size, and morphologic characteristics felt to increase the risk of rupture (ie,
Other investigators have studied morphological parameters such presence of excrescence). Statistical analysis was performed by using
as aspect ratio,12,13 height-width ratio,14 neck type,14,15 and inflow individual aneurysm risk.
angle.15,16 However, few studies have analyzed these factors
Statistical Analysis
together in a single cohort.
The goal of the present article was to highlight nonmodifiable A full model, including all study variables, was constructed from the
risk factors related to the risk of aneurysmal rupture in a large information in the database. Backward stepwise regression, with system-
atic removal of the least significant variables, was performed in a sequential
cohort of patients who presented to a single institution. We aimed
fashion until only those variables reaching significance remained.
to determine whether these commonly cited variables were Univariate analysis was conducted to assess statistical differences in
associated with rupture on presentation when applied to a large individual nonmodifiable risk factors (size, AR, location, neck type, and
sample size. We do not intend this study to serve as a guideline for multiplicity) between patients with ruptured and unruptured aneurysms
clinical decision making, nor did we attempt to construct by the use of the Student t test. Parameters that had statistically significant
a treatment algorithm based on our findings. associations with rupture status by univariate analysis were then included
in multivariate regression to further assess interdependence. Smoking
status and age were also included in multivariate regression because they
PATIENTS AND METHODS have demonstrated strongly independent associations with risk of
aneurysm rupture in previous studies.17,18 A P value of less than .05
Patients
was considered statistically significant. Data were analyzed with the use
A retrospective analysis was done of patients admitted to Jefferson of JMP 7.0.2 statistical software (SAS Institute, Cary, North Carolina).
Hospital for Neurosciences (JHN), a high-volume tertiary cerebrovascular Nonmodifiable variables of aneurysm size, AR, location, and multiplicity
facility, between January 2006 and January 2010 with a primary diagnosis were evaluated with CTA, MRA, angiography, or a combination of
of cerebral aneurysm. The study protocol was approved by the modalities. Only saccular aneurysms with a discrete dome and neck were
Institutional Review Board of Thomas Jefferson University prior to included in the analysis. Aneurysms were included in the study regardless of
commencement. Aneurysms were divided into 2 groups based on their whether or not they were associated with an arteriovenous malformation. (1)
rupture status: unruptured or ruptured aneurysm. Patients with an Aneurysm size was analyzed as a dichotomous variable of greater than or less
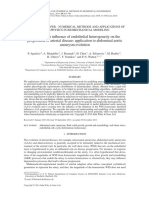
unruptured aneurysm were admitted for one or more of the following than 10 mm. (2) AR was calculated as the maximum perpendicular height in
reasons: aneurysm diagnosed on workup of headache, transient ischemic millimeters divided by the neck width in millimeters (Figure 1). AR was
attack, stroke, or seizure, incidental aneurysm found on imaging study analyzed as a dichotomous variable of greater or less than 1.6 based on the
performed for separate pathology (head trauma, etc), signs and symptoms contemporary literature that suggests that an AR of 1.6 is signifi-
of cranial nerve compression (ie, third nerve palsy), and sentinel headache cant.12,13,15 (3) Neck type was evaluated by CTA, MRA, or angiography
(worst headache of life without evidence of SAH on CT or lumbar and aneurysms were classified as either having a classical (apical) or
puncture). Because JHN is a large tertiary care cerebrovascular center, deviated neck type (Figure 1). (4) Location was analyzed as a dichotomous
a significant number of patients with incidental aneurysms were directly variable based on the parent vessel. Aneurysms of the anterior
admitted from outpatient neurology, internal medicine, and family communicating artery, anterior cerebral artery, posterior communicating
medicine practitioners. Patients with ruptured aneurysms were admitted artery (PCOM), middle cerebral artery, cavernous or carotid-ophthalmic
to JHN through the Jefferson emergency department or from outside segments of the internal carotid artery (ICA), and distal ICA or ICA
institutions without cerebrovascular capabilities. bifurcation were considered anterior circulation. Aneurysms of the basilar
Data of interest were collected by retrospective review of electronic artery, posterior cerebral artery (PCA), vertebral artery, and superior
medical records, outpatient charts, and radiographic reports. Information cerebellar artery were considered posterior circulation. To address the
on age, sex, history of tobacco use, aneurysm dome diameter, aspect ratio ISUIA inclusion of PCOM aneurysms in the posterior circulation, we
(AR), location, aneurysm sidedness (left vs right), neck morphology performed 2 separate analyses of ruptured and unruptured aneurysms in
(classical or deviated neck types), and multiplicity (the presence of more which PCOM aneurysms were included in either the anterior or posterior
than 1 aneurysm) was entered into a central database. A history of previous circulation. (5) Multiplicity was analyzed as a dichotomous variable of 1
SAH was not included in the analysis, because it had already been shown aneurysm or more than 1 aneurysm at any site.
to be associated with an increased risk of rupture of additional aneurysms.
Thus, to more effectively evaluate the contributions of the variables listed RESULTS
above, patients with a history of SAH were excluded from the study.
Family history was not used in the analysis because the data were not The database contained 2347 patients harboring 5139 in-
recorded for a significant number of patients. dividual aneurysms, for which complete information was available
Only patients with a radiographically confirmed diagnosis of cerebral for 5134 aneurysms. Of these aneurysms, 1792 (34.90%) were
aneurysm by computed tomographic angiography (CTA), magnetic
ruptured and 3342 (65.09%) were unruptured. The distribution
resonance angiography (MRA), or digital subtraction angiography were
of individual aneurysms and the number of ruptured and
included. Aneurysms were not grouped based on the imaging modality by
which they were identified. As per our protocol, all patients admitted with unruptured aneurysms within each group are listed in the Table.
an aneurysmal SAH underwent digital subtraction angiography on the day Of the aneurysms, 3587 (69.87%) arose from the left side of the
of or day after admission. circulation, 1183 (32.98%) of which ruptured. There were 1547
In patients with multiple aneurysms, selection of the aneurysm for (30.00%) right-sided aneurysms, 609 (39.37%) of which
treatment was based on the blood pattern on CT, evaluation of aneurysm ruptured. Six hundred twelve (28.43%) aneurysms demonstrated
694 | VOLUME 70 | NUMBER 3 | MARCH 2012 www.neurosurgery-online.com
Copyright © Congress of Neurological Surgeons. Unauthorized reproduction of this article is prohibited.
Copyright © Congress of Neurological Surgeons. Unauthorized reproduction of this article is prohibited.
ANEURYSMAL RUPTURE RISK FACTOR ANALYSIS
FIGURE 1. Calculation of AR and depiction of aneurysm neck types. A, the AR is calculated using the following equation: AR =
dome height (mm)/neck diameter (mm). B, aneurysms were classified as having either a classical or deviated neck type. AR, aspect
ratio.
a classical neck type, 174 (28.43%) of which were ruptured; 4526 The combination of AR, dome size, and neck type within an
(88.16%) aneurysms had a deviated neck, 1619 (35.77%) of individual aneurysm was also investigated (Figure 2). One
which were ruptured. thousand two hundred seventy aneurysms were found to have
The size of the aneurysm dome was also evaluated in both the an AR .1.6, a dome diameter .10 mm, and a deviated neck
ruptured and unruptured groups: 3056, 580 (25.89%) of which type; 879 (69.21%) of these aneurysms were ruptured on
were ruptured, were found to have domes measuring , 10 mm; admission. Two hundred thirty aneurysms had an AR .1.6,
2078 aneurysms possessed domes .10 mm, and of these, 1212 a dome diameter .10 mm, and a classical neck type, of which
(58.33%) were ruptured on admission (P , .001). Aneurysm AR 128 (55.65%) ruptured. 224 (30.43%) of 736 aneurysms had an
was analyzed as a dichotomous variable of greater or less than 1.6. AR .1.6, dome diameter ,10 mm, and a deviated neck type.
Of the aneurysms, 2374 (46.24%) were calculated to have an AR One hundred thirty-eight aneurysms had an AR .1.6, dome
,1.6, whereas 2760 (53.76%) of the aneurysms had an AR diameter ,10 mm, and a classical neck type, of which 14
.1.6. Of aneurysms with an AR ,1.6, 19.82% were ruptured, (10.14%) ruptured. Five hundred two aneurysms had an AR
and 52.44% of aneurysms with an AR .1.6 presented following ,1.6, dome diameter .10 mm, and a deviated neck type; 192
a rupture (P , .001). Six hundred twelve aneurysms were (38.25%) of these aneurysms were ruptured. Seventy-six
classified as having a classical neck type and 174 (28.43%) of aneurysms demonstrated an AR ,1.6, dome diameter .10
these were ruptured, and 4526 aneurysms had a deviated neck mm, and a classical neck type, of which 13 (17.11%) ruptured.
type and 1619 (35.77%) of these were ruptured (P , .001). Two thousand fifteen aneurysms had an AR ,1.6, dome
NEUROSURGERY VOLUME 70 | NUMBER 3 | MARCH 2012 | 695
Copyright © Congress of Neurological Surgeons. Unauthorized reproduction of this article is prohibited.
Copyright © Congress of Neurological Surgeons. Unauthorized reproduction of this article is prohibited.
AMENTA ET AL
posterior circulation aneurysms. When PCOM aneurysms were
TABLE. 5138 Aneurysms by Location and Rupture Status on classified as arising from the anterior circulation, 4737 (92.19%)
Admissiona of the total number of aneurysms arose within the anterior
Aneurysm circulation, 35.28% of which were ruptured. Four hundred one
Location Ruptured Unruptured Total % Ruptured SE (7.80%) aneurysms were found in the posterior circulation, and
Cavernous 159 407 566 28.09 1.89%
30.42% of these aneurysms were ruptured. If PCOM aneurysms
ICA/CO were considered along with posterior circulation aneurysms, 3684
ICA 114 297 411 27.74 2.21% (71.70%) aneurysms arose from the anterior circulation, 1247
ACOM/ACA 485 969 1454 33.36 1.24% (33.85%) of which were ruptured; 1454 posterior circulation
MCA 489 764 1253 39.03 1.38% aneurysms were found with 546 (37.55%) ruptured.
Basilar 94 207 301 31.23 2.67% Dome diameter .10 mm, AR .1.6, and right sidedness had
PCOM 424 629 1053 40.27 1.51%
statistically significant associations with rupture status in
PCA/SCA 28 72 100 28.00 4.49%
Total 1793 3345 5138
univariate analysis. Aneurysm size of .10 mm had an odds
ratio (OR) of 5.97 for rupture (95% confidence interval [CI],
a
ACA, anterior cerebral artery; ACOM, anterior communicating artery; CO, carotid- 5.27-6.77; P , .001). AR .1.6 had an OR of 4.46 for rupture
ophthalmic; ICA, internal carotid artery; MCA, middle cerebral artery; PCA, (95% CI, 3.94-5.05; P , .001). Presence of a deviated neck type
posterior cerebral artery; PCOM, posterior communicating artery; SCA, superior
cerebellar artery; SE, standard error.
had an OR of 1.40 for rupture (95% CI, 1.17-1.69; P = .001),
and aneurysms of the anterior circulation had an OR of 0.85 for
rupture (95% CI, 0.75-0.97; P = .012).
diameter ,10 mm, and a deviated neck type; 323 (16.03%) of In multivariate analysis, dome diameter .10 mm and an AR
these aneurysms were ruptured on admission. Finally, 167 .1.6 remained statistically significant. The presence of a deviated
aneurysms had an AR ,1.6, dome diameter , \10 mm, and neck type became statistically significant in multivariate analysis,
a classical neck-type; 19 (11.38%) of these aneurysms ruptured. whereas right sidedness was no longer significant. Dome diameter
Two separate analyses of the incidence of ruptured and .10 mm had an OR of 4.35 for rupture (95% CI, 3.79-4.99;
unruptured aneurysms within the study population were per- P , .001). AR .1.6 had an OR of 2.81 for rupture (95% CI,
formed with PCOM aneurysms included as either anterior or 2.45-3.22; P , .001). Presence of a deviated neck had an OR of
2.11 for rupture (95% CI, 1.72-2.59; P , .001) and aneurysms
of the anterior circulation had an OR of 0.77 for rupture (95%
CI, 0.67-0.89; P = .001). Right sidedness had an OR of 1.32 for
rupture (95% CI, 1.15-1.52; P = .001). PCOM aneurysms were
considered anterior circulation aneurysms for the multivariate
analyses.
DISCUSSION
Intracranial aneurysms, which are found in approximately 2%
to 5% of the population, represent a class of relatively common
vascular lesions. Despite their prevalence, only 1% to 2% of
aneurysms will rupture, resulting in SAH.19-21 Through retro-
spective review, the present study evaluates associations between
several morphological risk factors and the occurrence of
aneurysmal rupture.
Aneurysm Size
The present study was not designed in a manner conducive to
FIGURE 2. Number of ruptured and unruptured aneurysms based on the si-
multaneous evaluation of AR, dome diameter, and neck type in an individual
establishing a threshold value or "critical size" predictive of
aneurysm. AR was analyzed as a dichotomous variable of greater or less than 1.6. rupture. We did find that aneurysms with a dome diameter .10
Dome diameter was analyzed as a dichotomous variable of greater than or less than mm are significantly more likely to present following a rupture in
10 mm. Neck type was analyzed as a dichotomous variable: classical vs deviated comparison with aneurysms measuring ,10 mm. Of those
neck type. The highest incidence of rupture was found in aneurysms with an AR aneurysms ,10 mm in diameter, 25.89% were ruptured,
.1.6, dome diameter .10 mm, and a deviated neck type. Small aneurysms (AR whereas 58.33% of aneurysms .10 mm had ruptured before
,1.6, dome diameter ,10) were the most frequently encountered aneurysms
admission. Thus, our results are similar to the data presented in
within the series. Small aneurysms with a classical neck type had the lowest
incidence of rupture. AR, aspect ratio. the original ISUIA report, in which aneurysms with a dome
diameter $10 mm were at a higher risk of rupture.22 Perhaps,
696 | VOLUME 70 | NUMBER 3 | MARCH 2012 www.neurosurgery-online.com
Copyright © Congress of Neurological Surgeons. Unauthorized reproduction of this article is prohibited.
Copyright © Congress of Neurological Surgeons. Unauthorized reproduction of this article is prohibited.
ANEURYSMAL RUPTURE RISK FACTOR ANALYSIS
more importantly, within our series, over one quarter of aneurysms with an AR ,1.6, dome diameter .10 mm, and
aneurysms ,10 mm were ruptured on admission, thereby a deviated neck type. The predictive value of the AR combined
supporting the existing literature that demonstrates that smaller with dome diameter and neck type held true for small aneurysms,
aneurysms rupture frequently. Juvela et al19 provided some of the as well. In aneurysms with a dome diameter ,10 mm and
most convincing data in their experience with 142 patients a deviated neck, the incidence of rupture was 30.43% for
harboring unruptured aneurysms over 2575 person-years in aneurysms with an AR .1.6 and 16.03% when the AR was
a patient population not offered surgical intervention. The key ,1.6. In classical neck-type aneurysms, an AR .1.6 was also
data was that an aneurysmal dome ,6 mm in diameter was found associated with a significantly greater incidence of rupture in
in 23 (70%) of 33 ruptured aneurysms that had been initially aneurysms with a dome diameter .10 mm. Aneurysms with
followed in the wake of a previous diagnosis. Perhaps, of even a dome diameter ,10 mm and a classical neck showed no
greater importance, is the observation that, in 3 patients with significant difference in rupture rate regardless of the AR.
aneurysms ,5 mm, aneurysmal diameter increased significantly Furthermore, the combination of AR, aneurysm dome di-
before rupture. A thorough review of the literature will reveal ameter, and neck type held a significantly stronger predictive value
multiple studies reporting a significant rupture rate in aneurysms than any variable considered alone. Thus, these data draw
,5 mm in diameter.23,24 attention to the need for further prospective analysis to further
Our results do not clarify the debate over the aneurysm size at define the AR threshold value and to investigate the significance of
which the risk of rupture is the greatest. If nothing else, however, AR within the context of other morphologic variables.
they do reinforce what is commonly encountered in practice.
Larger aneurysms appear to rupture with a significantly greater Aneurysm Location
frequency than smaller aneurysms. Importantly, smaller aneur- Anterior circulation aneurysms were found to be ruptured with
ysms continue to pose a significant challenge in the management incidences ranging from 27.74% to 40.27%. PCOM aneurysms
algorithm, because they were also found to be ruptured in demonstrated the highest incidence of rupture (40.27%). Poste-
a significant percentage of cases.25-27 rior circulation aneurysms, basilar artery and PCA or superior
cerebellar artery, had incidences of rupture of 31.23% and
Aspect Ratio 28.00%, respectively, which fell within the range of anterior
Using animal models of aneurysmal blood flow, Ujiie et al28 circulation aneurysms. As a result, our findings do not agree with
published the morphometric and hemodynamic data pertaining the existing literature, in which posterior circulation aneurysms
to the use of the AR as a clinically relevant variable. Intra- exhibit a greater risk of rupture.22,25
aneurysmal flow correlates with the AR and decreases as the The findings of the ISUIA retrospective review have been
aneurysmal neck narrows and dome volume (dome height) criticized for the inclusion of PCOM aneurysms within the
increases. In clinical retrospective analyses, the AR threshold posterior circulation. The data showed basilar tip, PCOM,
value was established as 1.6, because nearly 80% of ruptured vertebrobasilar, and PCA aneurysms to display a higher risk of
aneurysms demonstrated an AR .1.6. Conversely, approxi- rupture in group 1 patients, while the basilar tip was the only
mately 90% of unruptured aneurysms displayed an AR ,1.6.13 location predictive of rupture in group 2.22 To address the
The AR was analyzed as a dichotomous variable of greater or less importance of the inclusion of PCOM aneurysms within the
than 1.6 based on these findings.12,13,15 We found that 46.24% of anterior or posterior circulation, we performed 2 separate
aneurysms within our series had an AR ,1.6, whereas 53.76% of analyses. When PCOM aneurysms were included in the anterior
aneurysms had an AR .1.6. The rates of rupture were somewhat circulation, 4737 (92.19%) of the total number of aneurysms
different than those published by Ujiie et al,28 with 19.82% of arose within the anterior circulation, 35.28% of which were
aneurysms with an AR ,1.6 rupturing and 52.44% of aneurysms ruptured; 401 (7.80%) aneurysms were found in the posterior
with an AR .1.6 presenting after a rupture. Of unruptured circulation, and 30.42% of these aneurysms were ruptured.
aneurysms, 66.22% had an AR ,1.6, whereas 33.78% of If PCOM aneurysms were considered along with posterior
unruptured aneurysms had an AR .1.6. Thus, our data support circulation aneurysms, 3684 (71.70%) aneurysms arose from the
the association between higher ARs and an increased incidence of anterior circulation, 1247 (33.85%) of which were ruptured. One
rupture. Importantly, our data demonstrate that aneurysms with thousand four hundred fifty-four posterior circulation aneurysms
an AR ,1.6 rupture frequently, and suggest that this value is not were found with a 37.55% incidence of rupture. Thus, the
a clinically useful threshold.5,29,30 inclusion of PCOM aneurysms in the posterior circulation group
To clarify the importance of the AR, we performed a multivariate significantly influenced our results. Because PCOM aneurysms
analysis in which the incidence of aneurysm rupture was determined demonstrated the highest incidence of rupture among all
for individual aneurysms with a specific combination of AR, dome locations, their inclusion in the anterior circulation resulted in
diameter, and neck type. We found that 1270 aneurysms had an AR a significantly greater incidence of rupture for these aneurysms
.1.6, dome diameter .10 mm, and a deviated neck type. Of compared with the posterior circulation. Furthermore, when
these aneurysms, 879 (69.21%) were ruptured on presentation. considered as part of the posterior circulation, the incidence of
This value was significantly higher than the 38.25% of ruptured rupture for this group was significantly greater compared with
NEUROSURGERY VOLUME 70 | NUMBER 3 | MARCH 2012 | 697
Copyright © Congress of Neurological Surgeons. Unauthorized reproduction of this article is prohibited.
Copyright © Congress of Neurological Surgeons. Unauthorized reproduction of this article is prohibited.
AMENTA ET AL
anterior circulation aneurysms. Also, the incidence of posterior a result, the data pertaining to unruptured aneurysms may not
circulation rupture was significantly higher between analyses reflect the lifetime risk of rupture to this population.
when PCOM aneurysms were classified as arising from the The article would have gained significant strength if the
posterior circulation. As a result, our data support the criticism variables had been evaluated in a continuous manner. This
that has befallen the ISUIA data for inclusion of PCOM approach would have allowed for the identification of ideal
aneurysms within the posterior circulation cohort. The present threshold values for dome diameter and AR beyond which the
study suggests that the choice to include PCOM aneurysms in the incidence of rupture was significantly increased. The data had been
posterior circulation cohort potentially falsely elevates the in- entered in a dichotomous fashion from the initiation of the study,
cidence of rupture for posterior circulation aneurysms. Regardless and specific characteristics beyond what is presented are not
of the classification of PCOM aneurysms, the anterior circulation available.
incidence of rupture did not differ significantly, perhaps because Unruptured aneurysms were admitted for a variety of reasons,
of the significantly greater number of aneurysms present in the ranging from incidental findings to sentinel headache, thereby
anterior circulation. introducing a significant selection bias. Furthermore, patients
Although aneurysm sidedness represents a variable that is far less presented with a varying number of medical comorbidities that
examined, we found a significant difference in the incidence of influenced the decision-making process in a significant number of
rupture between sides. Six hundred nine of the 1547 (39.37%) patients. The study reflects the practice patterns of multiple
right-sided aneurysms were ruptured, whereas 1183 of the 3587 physicians, each with unique training, comfort level, and man-
(32.98%) left-sided aneurysms ruptured. The significantly greater agement style. Additionally, because JHN is a high-volume tertiary
incidence of rupture in right-sided aneurysms is not consistent care cerebrovascular facility, a large number of patients are directly
with other reports within the literature.31 Because we do not have admitted with the preconceived notion that their aneurysm
a pathophysiologic explanation for the increased number of requires immediate treatment. Despite counseling and the offer
ruptured right-sided aneurysms, we have to acknowledge the to observe a percentage of aneurysms, patients often demand
potential existence of a chance finding or a process that has yet to treatment. As a result, the decision to treat a particular unruptured
be adequately described. Regardless of the underlying cause, aneurysm was influenced by multiple factors not included in our
aneurysm sidedness is a variable in obvious need of further analysis.
investigation. Finally, although the size of the series gives the study its greatest
strength, certain important characteristics, such as family history
Neck Type of SAH, were not available for a percentage of patients. Future
When evaluating the morphology of the aneurysmal neck, prospective investigations should attempt to include all of these
a distinction is made between aneurysms that arise from the parent variables in their analyses.
artery midline (classical neck type) and those whose neck is
deviated (deviated neck type) in the direction of one of the CONCLUSION
daughter arteries.29 We must point out that the accurate analysis
of neck type in a large retrospective series such as this is difficult To our knowledge, we have presented data from one of the
and open to significant inter- and intraobserver variability. Neck largest retrospective reviews of ruptured and unruptured aneur-
type was assigned by the attending physician managing each ysms. Dome diameter .10 mm and an AR .1.6 were associated
individual patient and the determination was not blinded. The with the highest incidence of rupture. Furthermore, simultaneous
assignation of neck type to a particular aneurysm was not consideration of both variables along with neck type held
discussed among physicians, nor was there a consensus in the a considerably higher predictive value than the use of any
morphologic criteria needed to classify an aneurysm as having variable in isolation. The inclusion of PCOM aneurysms within
a classical or deviated neck type. Nevertheless, a significantly the anterior or posterior circulation significantly influenced the
greater percentage of aneurysms with a deviated neck type, incidences of rupture for each group. Right-sided aneurysms
35.77%, were ruptured compared with the 28.43% of ruptured ruptured more frequently than left-sided aneurysms, while
classical neck-type aneurysms. This finding is consistent with a significantly higher incidence of ruptured deviated neck-type
data from studies within the literature.32-34 Future computational aneurysms was found compared with classical neck-type
and clinical analyses are needed to better define the risk of rupture aneurysms.
in relation to neck type. The methodology used imposes significant restrictions on the
interpretation of the results, because selection bias and practice
Limitations of the Present Study patterns affect the final outcomes. As a result, this study cannot be
The present study is limited by its retrospective design and the used as a basis on which to guide clinical decision making.
relatively short follow-up period of 4 years. A longer period of Nevertheless, the evaluation of commonly cited risk factors in such
observation of unruptured aneurysms is necessary to estimate the a large patient population was able to lend additional insight into
lifetime risk of rupture, and there is no way to know if treated the characteristics of ruptured and unruptured aneurysms upon
unruptured aneurysms would have ever ruptured in the future. As initial presentation. Additional prospective analysis of these
698 | VOLUME 70 | NUMBER 3 | MARCH 2012 www.neurosurgery-online.com
Copyright © Congress of Neurological Surgeons. Unauthorized reproduction of this article is prohibited.
Copyright © Congress of Neurological Surgeons. Unauthorized reproduction of this article is prohibited.
ANEURYSMAL RUPTURE RISK FACTOR ANALYSIS
morphologic variables combined with extended follow-up of 20. Tsutsumi K, Ueki K, Morita A, Kirino T. Risk of rupture from incidental cerebral
aneurysms. J Neurosurg. 2000;93(4):550-553.
unruptured aneurysms is needed to better define the characteristics 21. Rinkel GJ, Djibuti M, Algra A, van Gijn J. Prevalence and risk of rupture of
predictive of rupture. intracranial aneurysms: a systematic review. Stroke. 1998;29(1):251-256.
Disclosure 22. Unruptured intracranial aneurysms—risk of rupture and risks of surgical
intervention. International Study of Unruptured Intracranial Aneurysms Inves-
The authors report no disclosures of funding, personal conflicts of interest, or tigators. N Engl J Med. 1998;339(24):1725-1733.
financial interests pertaining to this article. 23. Forget TR, Benitez R, Veznedaroglu E, et al. A review of size and location of
ruptured intracranial aneurysms. Neurosurgery. 2001;49(6):1322-1325; discussion
REFERENCES 1325-1326.
24. Nakagawa T, Hushi K. The incidence and treatment of asymptomatic, unruptured
1. Zacharia BE, Hickman ZL, Grobelny BT, et al. Epidemiology of aneurysmal cerebral aneurysms. J Neurosurg. 1994;80(2):217-223.
subarachnoid hemorrhage. Neurosurg Clin N Am. 2010;21(2):221-233. 25. Clarke G, Mendelow AD, Mitchell P. Predicting the risk of rupture of intracranial
2. le Roux AA, Wallace MC. Outcome and cost of aneurysmal subarachnoid aneurysms based on anatomical location. Acta Neurochir (Wien). 2005;147(3):
hemorrhage. Neurosurg Clin N Am. 2010;21(2):235-246. 259-263; discussion 263.
3. Wilby MJ, Sharp M, Whitfield PC, Hutchinson PJ, Menon DK, Kirkpatrick PJ. 26. Kailasnath P, Dickey P. ISUIA-II: the need to share more data. Surg Neurol. 2004;
Cost-effective outcome for treating poor-grade subarachnoid hemorrhage. Stroke. 62(2):95.
2003;34(10):2508-2511. 27. Mira JM, Costa FA, Horta BL, Fabião OM. Risk of rupture in unruptured anterior
4. Vernooij MW, Ikram MA, Tanghe HL, et al. Incidental findings on brain MRI in communicating artery aneurysms: meta-analysis of natural history studies. Surg
the general population. N Engl J Med. 2007;357(18):1821-1828. Neurol. 2006;66(suppl 3):S12-S19; discussion S19.
5. Lall RR, Eddleman CS, Bendok BR, Batjer HH. Unruptured intracranial 28. Ujiie H, Tachibana H, Hiramatsu O, et al. Effects of size and shape (aspect ratio)
aneurysms and the assessment of rupture risk based on anatomical and on the hemodynamics of saccular aneurysms: a possible index for surgical
morphological factors: sifting through the sands of data. Neurosurg Focus. 2009; treatment of intracranial aneurysms. Neurosurgery. 1999;45(1):119-129; discus-
26(5):E2. sion 129-130.
6. Horowitz M. Guidelines for the surgical treatment of unruptured intracranial 29. Sadatomo T, Yuki K, Migita K, Taniguchi E, Kodama Y, Kurisu K. Evaluation of
aneurysms: the first annual J. Lawrence Pool Memorial Research Symposium— relation among aneurysmal neck, parent artery, and daughter arteries in middle
controversies in the management of cerebral aneurysms. Neurosurgery. 2009;64(3): cerebral artery aneurysms, by three-dimensional digital subtraction angiography.
E577. author reply E577. Neurosurg Rev. 2005;28(3):196-200.
7. Komotar RJ, Mocco J, Solomon RA. Guidelines for the surgical treatment of 30. Weir B, Amidei C, Kongable G, et al. The aspect ratio (dome/neck) of ruptured
unruptured intracranial aneurysms: the first annual J. Lawrence Pool Memorial and unruptured aneurysms. J Neurosurg. 2003;99(3):447-451.
Research Symposium—controversies in the management of cerebral aneurysms. 31. Aarhus M, Helland CA, Wester K. Differences in anatomical distribution, gender,
Neurosurgery. 2008;62(1):183-193; discussion 193-184. and sidedness between ruptured and unruptured intracranial aneurysms in
8. Lee T, Baytion M, Sciacca R, Mohr JP, Pile-Spellman J. Aggregate analysis of the a defined patient population. Acta Neurochir (Wien). 2009;151(12):1569-1574.
literature for unruptured intracranial aneurysm treatment. AJNR Am J Neuroradiol. 32. Ohshima T, Miyachi S, Hattori K, et al. Risk of aneurysmal rupture: the
2005;26(8):1902-1908. importance of neck orifice positioning-assessment using computational flow
9. Chang HS. Simulation of the natural history of cerebral aneurysms based on data simulation. Neurosurgery. 2008;62(4):767-773; discussion 773-775.
from the International Study of Unruptured Intracranial Aneurysms. J Neurosurg. 33. Strother CM, Graves VB, Rappe A. Aneurysm hemodynamics: an experimental
2006;104(2):188-194. study. AJNR Am J Neuroradiol. 1992;13(4):1089-1095.
10. Raymond J, Guillemin F, Proust F, et al. Unruptured intracranial aneurysms. A 34. Suzuki J, Ohara H. Clinicopathological study of cerebral aneurysms. Origin,
critical review of the International Study of Unruptured Intracranial Aneurysms rupture, repair, and growth. J Neurosurg. 1978;48(4):505-514.
(ISUIA) and of appropriate methods to address the clinical problem. Interv
Neuroradiol. 2008;14(1):85-96.
11. Wiebers DO, Whisnant JP, Huston J III, et al. Unruptured intracranial COMMENTS
A
aneurysms: natural history, clinical outcome, and risks of surgical and endovascular
treatment. Lancet. 2003;362(9378):103-110.
uthors examined the associations between various nonmodifiable
12. Nader-Sepahi A, Casimiro M, Sen J, Kitchen ND. Is aspect ratio a reliable risk factors and admissions at Jefferson Hospital for Neurosciences
predictor of intracranial aneurysm rupture? Neurosurgery. 2004;54(6):1343-1347; for ruptured (RAs) or unruptured intracranial aneurysms (UAs).
discussion 1347-1348. There are multiple difficulties in interpreting the results of this type of
13. Ujiie H, Tamano Y, Sasaki K, Hori T. Is the aspect ratio a reliable index for study. Sources of biases are so numerous and complex that exploring and
predicting the rupture of a saccular aneurysm? Neurosurgery. 2001;48(3):495-502; discussing them all would be longer than the original article.
discussion 502-503.
14. Hoh BL, Sistrom CL, Firment CS, et al. Bottleneck factor and height-width ratio:
To start, 1 set of problems is related to the multiplicity of lesions: Surely
association with ruptured aneurysms in patients with multiple cerebral aneurysms. among the 1792 patients with RAs, some patients with nonlocalizing
Neurosurgery. 2007;61(4):716-722; discussion 722-723. subarachnoid hemorrhages and 2 or more aneurysms were treated by
15. Baharoglu MI, Schirmer CM, Hoit DA, Gao BL, Malek AM. Aneurysm inflow- coiling. The treating team would commonly assume that the larger
angle as a discriminant for rupture in sidewall cerebral aneurysms: morphometric aneurysm was responsible for the bleed. This unproven assumption would
and computational fluid dynamic analysis. Stroke. 2010;41(7):1423-1430. then be encrypted into the database. It would be no wonder if, at the end,
16. Cebral JR, Castro MA, Burgess JE, Pergolizzi RS, Sheridan MJ, Putman CM.
Characterization of cerebral aneurysms for assessing risk of rupture by using
the results of the study would point at ruptures being more common in
patient-specific computational hemodynamics models. AJNR Am J Neuroradiol. larger than smaller lesions. This, of course, is begging the question.
2005;26(10):2550-2559. Another set of problems is related to the comparison that is being made.
17. Clarke M. Systematic review of reviews of risk factors for intracranial aneurysms. Admission for RAs is taken as a surrogate for UAs that have now shown
Neuroradiology. 2008;50(8):653-664. their propensity to rupture. On the other hand, some UAs are presumably
18. Nahed BV, DiLuna ML, Morgan T, et al. Hypertension, age, and location predict unruptured only for the time of diagnosis; for all we know, UAs could be
rupture of small intracranial aneurysms. Neurosurgery. 2005;57(4):676-683;
discussion 676-683.
a mixture of some nonrisky, some “yet-to-rupture” lesions sharing all
19. Juvela S, Porras M, Poussa K. Natural history of unruptured intracranial “nonmodifiable risk factors” with RAs. But how long should UAs be
aneurysms: probability of and risk factors for aneurysm rupture. J Neurosurg. observed to qualify as low-risk lesions, to be distinguished from high-risk
2000;93(3):379-387. lesions, according to their characteristics? Status on admission cannot
NEUROSURGERY VOLUME 70 | NUMBER 3 | MARCH 2012 | 699
Copyright © Congress of Neurological Surgeons. Unauthorized reproduction of this article is prohibited.
Copyright © Congress of Neurological Surgeons. Unauthorized reproduction of this article is prohibited.
AMENTA ET AL
represent a meaningful observation period. This only shows that a natural a right-sided craniotomy (right sidedness being in this article a risk
history of aneurysms cannot come out of a comparison between factor), that some people may use results of this study to justify treatment
admissions for RAs and UAs. decisions is a serious matter.
A thought experiment may help illustrate another, most important Epidemiological methods are not appropriate for clinicians hoping to
problem with this type of material: selection bias. Let us imagine that justify their clinical decisions.5 Patients are not exposed to medical
during the period of data collection (2006-2010), clinicians followed the interventions the way populations are exposed to mercury. Can clinicians
implicit advice from the ISUIA study published in 19991: the natural act first and ask questions, do the research, later? By then it is too late to
history of unruptured aneurysms smaller than 10 mm is so benign that protect patients from unjustified decisions and unproved interventions,
nothing should be offered, and no patient should be admitted for and it is too late for sound and ethical research; patients have not
asymptomatic aneurysms 10 mm or less. In this work, 1212 of 1792 consented to research, but to care that was supposedly informed and
ruptured aneurysms (68%, already a high proportion, perhaps reflecting based on reliable knowledge. The appropriate way for clinicians to deal
referral bias) are larger than 10 mm, but 100% of patients admitted for with clinical dilemmas is not to pretend we know and to act, to later
unruptured aneurysms now have lesions larger than 10 mm. The admit the uncertain, and do the biased research without the consent of
methodology used in this article would show that the smaller the participants. The only way to justify decisions that involve risky
aneurysm, the larger the risks of rupture. This implausible thought preventive treatments in asymptomatic individuals is to show, using
experiment only shows that even if the data are prospectively collected, randomized allocation of treatment options, that treatments are safe and
this methodology can never disentangle true risk factors from effective, and above all, that they do more good than harm, in the same
confounders such as referral and selection biases, since we are not patients. We cannot expect scientific methods to realize their normative,
looking at UAs, we are looking at UAs admitted to Jefferson. truth-seeking potential role in regulating medical actions, or to protect
One general, insurmountable problem is the hope to find a “natural patients from error, bias, and abuse, when the science is only introduced
history” of an incidental imaging finding, nearly a contradiction in terms, after the fact. In the mean time, waiting for the results of trials, statistical
since the finding is by definition irrelevant to the disease. The data that methods applied to past admissions for an imaging finding cannot justify
are being collected are only a reflection of the availability and use of past actions and cannot guide future clinical decisions, without grave
imaging equipment, of comorbidities that led to diagnostic testing. We dangers. Clinicians must get their acts together and propose inter-
can imagine UAs having a much different “natural history,” according to ventions that have yet to be shown beneficial only within the context of
this research methodology, in places where imaging is not so widely appropriate trials.
available. We only have to remember the times when noninvasive
imaging did not exist, when less than 20% of aneurysms were Jean Raymond
unruptured on admission, to realize that the natural history of an Marc Kotowski
imaging finding is nothing but the history of medical imaging, of its use Tim E. Darsaut
and abuse.2 Montreal, Quebec, Canada
Prospective longitudinal cohort studies would be needed to avoid some
of the aforementioned problems, but many would remain. Cohort studies
1. The International Study of Unruptured Intracranial Aneurysms Investigators.
such as ISUIA end up comparing risks of treatment in patients we feel Unruptured Intracranial Aneurysms? Risk of Rupture and Risks of Surgical
must be treated with the supposed natural history of patients we do not Intervention. N Engl J Med. 1998;339:1725-1733.
want to treat, surely an invalid procedure, no matter how much we toil 2. Raymond J. Incidental intracranial aneurysms: rationale for treatment. Curr Opin
with statistical adjustments.2 Neurol. 2009;22(1):96-102; Review.
How then, have we become convinced that a “natural history of UAs” 3. Greving JP, Rinkel GJ, Buskens E, Algra A. Cost-effectiveness of preventive
would be needed, and that statistical methods could distinguish what is treatment of intracranial aneurysms: new data and uncertainties. Neurology. 2009;73
(4):258-265.
natural, what is man made in this story? The fatal logical fallacy 4. Raymond J, Molyneux AJ, Takao H, Nojo T, Ohtomo K. Unruptured intracranial
underlying all observational studies is the, at first sight, plausible but, on aneurysms: evidence and speculations. Radiology. 2008;247(1):294. author reply
further reflection, false premise that an “accurate prediction of the 294.
natural history of UAs” is needed to be “weighted against risks of 5. Byar DP. Problems with using observational databases to compare treatments. Stat
treatments,” as the authors pretend. How are we supposed to do that? Med. 1991;10:663-666.
The only way to make sense of comparing immediate risks of treatments 6. Raymond J, Darsaut TE, Molyneux AJ. A trial on unruptured intracranial
aneurysms (the TEAM trial): results, lessons from a failure and the necessity for
with long-term risks of a disease is through Markov modeling, in fact, clinical care trials. Trials. 2011;12(1):64.
computerized speculations that assume the facts that need to be
proved.3,4 The so-called natural history of UAs more often serves to
instill fear to justify risky preventive interventions than to provide a “key
factor in counseling patients for elective treatment,” as the authors claim
in the introduction.
T he authors provide an analysis of nonmodifiable risk factors for rupture
of intracranial aneurysms in a large, retrospective cohort. As the authors
point out, an understanding of these risk factors is critical in understanding
It seems to us that we have replaced self-promoting case series with the natural history of unruptured intracranial aneurysms and will ultimately
pseudo-scientific retrospective studies that now use sophisticated statis- aid in decision making, as an increasing number of incidental aneurysms are
tical methodologies. The problem is that, inserted between the in- being discovered. The authors confirm a number of nonmodifiable risk
troduction and the results sections, “Methods” have become like black factors, namely an aspect ratio of greater than 1.6, dome size greater than 10
boxes that readers, reviewers, and, we suspect, sometimes authors mm, and a deviated neck as being independently associated with aneurysm
themselves, understand barely enough to identify intrinsic pitfalls and rupture. Although not terribly novel, the study does confirm these pre-
biases. While we can pause a minute to muse about a science-fiction story viously noted morphometric characteristics in a large patient cohort. Ulti-
in which you could guess someone’s hometown by the presence of mately, however, the retrospective study design does not allow for detailed
700 | VOLUME 70 | NUMBER 3 | MARCH 2012 www.neurosurgery-online.com
Copyright © Congress of Neurological Surgeons. Unauthorized reproduction of this article is prohibited.
Copyright © Congress of Neurological Surgeons. Unauthorized reproduction of this article is prohibited.
ANEURYSMAL RUPTURE RISK FACTOR ANALYSIS
analysis of the natural history of unruptured aneurysms, a point which it does provide evidence that further supports the notion that morphological
significantly weakens the conclusions of the article. The quality of these characteristics of intracranial aneurysms are associated with risk of rupture.
studies relies on comprehensive and adjudicated data collection, and this Additional longitudinal, prospective patient studies that include advanced
study lacks critical information regarding the reason for admission in neuroimaging and analytic software will be needed to provide a deeper
patients with an unruptured aneurysm, as well as data regarding treatment understanding of if and when an unruptured aneurysm may rupture.
decisions. This paves the way for substantial selection bias, which is com-
mon in this type of study. Although this study does not ultimately help in Brad Zacharia
decision making regarding treatment of unruptured intracranial aneurysms, New York, New York
NEUROSURGERY VOLUME 70 | NUMBER 3 | MARCH 2012 | 701
Copyright © Congress of Neurological Surgeons. Unauthorized reproduction of this article is prohibited.
Copyright © Congress of Neurological Surgeons. Unauthorized reproduction of this article is prohibited.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- MathematicsNumericsDerivationsAndOpenFOAM PDFDocument166 pagesMathematicsNumericsDerivationsAndOpenFOAM PDFAlberto BrasoNo ratings yet
- O-Ring UKDocument12 pagesO-Ring UKAan Sarkasi AmdNo ratings yet
- Past Question Papers Theory Solved Jan 12 To Jan 15 Capt. Saujanya SinhaDocument282 pagesPast Question Papers Theory Solved Jan 12 To Jan 15 Capt. Saujanya Sinhabasheer shaik100% (2)
- 1113 FullDocument6 pages1113 FullAlberto BrasoNo ratings yet
- Multiscale Modeling of Intracranial Aneurysms: Cell Signaling, Hemodynamics, and RemodelingDocument4 pagesMultiscale Modeling of Intracranial Aneurysms: Cell Signaling, Hemodynamics, and RemodelingAlberto BrasoNo ratings yet
- A Theoretical Model of Enlarging Intracranial Fusiform AneurysmsDocument8 pagesA Theoretical Model of Enlarging Intracranial Fusiform AneurysmsAlberto BrasoNo ratings yet
- Medical Engineering & PhysicsDocument9 pagesMedical Engineering & PhysicsAlberto BrasoNo ratings yet
- Gry Tsan 2015Document11 pagesGry Tsan 2015Alberto BrasoNo ratings yet
- Promedio de Un Plano.: Postprocess - Func 'Patchaverage (Name Wall1, Nusseltnumber) 'Document1 pagePromedio de Un Plano.: Postprocess - Func 'Patchaverage (Name Wall1, Nusseltnumber) 'Alberto BrasoNo ratings yet
- Aparcio 2014Document24 pagesAparcio 2014Alberto BrasoNo ratings yet
- OFLecFSI 1 PDFDocument37 pagesOFLecFSI 1 PDFAlberto BrasoNo ratings yet
- Post Purchase Cognitive DissonanceDocument18 pagesPost Purchase Cognitive DissonancePawan DihiyeNo ratings yet
- Anwar Ali Khan ProposalDocument65 pagesAnwar Ali Khan ProposalAnwar Ali TanhaNo ratings yet
- Alter NadorDocument10 pagesAlter NadorJOSE0% (2)
- Collaboration Rubric PowellDocument1 pageCollaboration Rubric PowellFrancis A. BuenaventuraNo ratings yet
- Roddy Lawsuit DismissedDocument66 pagesRoddy Lawsuit DismissedThe Huntsville TimesNo ratings yet
- TestingDocument116 pagesTestingAkarsh LNo ratings yet
- Gs Reported Speech - ExercisesDocument6 pagesGs Reported Speech - ExercisesRamona FloreaNo ratings yet
- Big Breakfasts Help Us Burn Double The CaloriesDocument4 pagesBig Breakfasts Help Us Burn Double The CaloriesBastian IgnacioNo ratings yet
- Diagnosis Dan Tatalaksana Pasien Dengan Insufisiensi Akomodasi - Sri Hudaya WidihasthaDocument13 pagesDiagnosis Dan Tatalaksana Pasien Dengan Insufisiensi Akomodasi - Sri Hudaya WidihasthamalaNo ratings yet
- Behavior Intervention PlanDocument22 pagesBehavior Intervention Planapi-343163369100% (1)
- OverlandersDocument17 pagesOverlandersJoe FloodNo ratings yet
- 6 5 Nerves Hormones and HomeostasisDocument19 pages6 5 Nerves Hormones and Homeostasisapi-235355872No ratings yet
- 20 - Offshore Construction - Part 1Document27 pages20 - Offshore Construction - Part 1Edytha SimamoraNo ratings yet
- Cimt in Children WTH CP: Sample Measures/ FindingsDocument6 pagesCimt in Children WTH CP: Sample Measures/ Findingsapi-253994356No ratings yet
- Micro Hydro BrochureDocument4 pagesMicro Hydro BrochureErlangga SatyawanNo ratings yet
- Gastric Feeding TubesDocument10 pagesGastric Feeding Tubesapi-254470605No ratings yet
- Wap-3101 Um V1.0 PDFDocument34 pagesWap-3101 Um V1.0 PDFhtweakNo ratings yet
- Iron Ore Value-In-Use: Benchmarking and Application: Peter Hannah AnalystDocument19 pagesIron Ore Value-In-Use: Benchmarking and Application: Peter Hannah AnalystAnkit BansalNo ratings yet
- Human Genetics: Ms MB KekanaDocument31 pagesHuman Genetics: Ms MB Kekanavulkaan van huisNo ratings yet
- Internet BillDocument2 pagesInternet Billshiva ramNo ratings yet
- Geometri Unsur StrukturDocument10 pagesGeometri Unsur StrukturNirmaya WulandariNo ratings yet
- Seed Health Testing in Field Crops Seeds........... AaaaaaaDocument37 pagesSeed Health Testing in Field Crops Seeds........... AaaaaaaJagadish GowdaNo ratings yet
- ToolsDocument1 pageToolsJolangNo ratings yet
- 20 Leverage of E Marketing A CaseStudy of Reliance Jio PDFDocument5 pages20 Leverage of E Marketing A CaseStudy of Reliance Jio PDFankush birlaNo ratings yet
- Revenge, Hypnotism, and Oedipus in OldboyDocument13 pagesRevenge, Hypnotism, and Oedipus in OldboyAdrián PiqueroNo ratings yet
- CMC Business PlanDocument32 pagesCMC Business PlanRobert ShisokaNo ratings yet
- "Some of Us May Never Die," by Kathleen SteinDocument5 pages"Some of Us May Never Die," by Kathleen SteinMark PlusNo ratings yet
- RET541 543ParlistENaDocument145 pagesRET541 543ParlistENaMatthew Mason100% (1)