Professional Documents
Culture Documents
The Practice and Science of Wound Healing History and Physiology of Wound Healing
Uploaded by
screwdriverOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Practice and Science of Wound Healing History and Physiology of Wound Healing
Uploaded by
screwdriverCopyright:
Available Formats
Wound Care: The practice and science of wound healing: history and physiology of wound healing
The practice and science of wound healing: history and
physiology of wound healing
Naude L, BCur, MCur (UP), Certificate in Wound Care (UFS), Certificate in Wound Care (Hertfordshire)
Correspondence to: Liezl Naude, e-mail: liezl@eloquent.co.za
www.eloquent.co.za
Abstract
This is the first in a series of articles focusing on wound management. In this article, I will discuss the history and physiology of
wound healing, utilising a comparison of wound healing to a building site.
Introduction Looking at wound healing like a builder
Wound healing is a complex process influenced by various The process of wound healing is explained by Kane as being
factors such as the host (the patient), the environment, and similar to that of rebuilding a house after it has been damaged
the multi-disciplinary team.1 Wound care practitioners can no for some reason.1
longer make use of a single modality for the progressive care
of a wound. They must critically select wound healing therapy According to this model, the major cells responsible for wound
according to the phase of healing of each wound. healing are like the builders who have been hired to repair the
house. The initial phase is characterised by the formation of
The first documentation of wound care can be found in the a temporary platelet plug to stop the bleeding (haemostasis),
ancient Egyptian Edwin Smith Papyrus of 1600 BC, with a which is like the contractors capping the conduits to prevent
description of the removal of devitalised skin and pus following further loss. Within the inflammatory phase, the neutrophils
war injuries.2 The Hippocratic Collection of 400 BC provides us responsible for phagocytosis are represented by the labourers
with some insight into the Greek practice of using drains to who have to clean up the landfill. The proliferation phase
evacuate pus from abscesses. depends on the macrophage in the same way as the rebuilding
process depends on the building supervisor on site.
Joseph Lister introduced the modern “germ theory” by
demonstrating the beneficial effects of carbolic acid in the The macrophage is the key mediator in signalling other
dressings of infected wounds at the turn of the century.3 “subcontractors” such as the lymphocytes (specific
Debridement, skin cleansing and the use of antiseptics became site preparers or cleaners), angiocytes (plumbers) and
common practice thereafter. During the same period gloves, neurocytes (electricians). The fibroblasts can be seen as
gowns, and masks were introduced by William Halsted, and the frame workers or builders of reinforcement structures,
silver foil was revived as an antiseptic in dressings.3 Modern the basic building blocks ensuring a solid appearance. The
wound care really took off when, in 1908, Elie Metchnikoff keratinocytes are the roofers providing the waterproofing
identified and characterised phagocytosis as it applied to and an external barrier. Remodelling of scar tissue occurs
inflammation and wound debridement.4 over the next two years in the same way we would do
interior decorating of our houses.
DP Kane describes the wound environment as part of a
larger human ecosystem, 1 and I couldn’t agree more. No Matrix metalloproteinases (MMPs), and their effect on the
wound should be treated as an isolated phenomenon. If extracellular matrix (ECM), are missing from this model.5
each wound is treated as part of a macroenvironment, According to Gibson and Schultz, MMPs form part of the key
this will result in sustainable wound repair. Comorbidities proteins that regulate the actions of the wound cells and they
and other factors that can potentially affect healing are essential to remove the denatured ECM and to digest
should always be considered. These factors to be “holes” in the basement membrane surrounding capillaries
considered include arterial insufficiency, chronic illness, to enable vascular endothelial cells to migrate and form new
diabetes mellitus, cancer, surgery, trauma and venous capillaries. The ECM can also be compared to the blueprint
insufficiency. prepared by the structural engineer or architect, which
Professional Nursing Today 17 2010;14(3)
Wound Care: The practice and science of wound healing: history and physiology of wound healing
provides the plan for the rebuilding project.7 The ECM is key Figure 2: Schematic representation of haemostasis with vaso-
to ensuring that the final product is delivered according to the constriction and platelet releasing growth factors. (Graphics used
building plan. with permission from Dr G Schultz.) It is important to note that fibrin
clot forms a provisional wound matrix that promotes coagulation
and migration of fibroblasts and vascular endothelial cells, and that
Wound healing from a physiological perspective
platelets release growth factors that initiate healing by stimulating
chemotaxis, proliferation, and matrix synthesis.
For wound healing to take place, both the macro- and
microvascular structures must be intact, with adequate
cardiac output and flow to perfuse the wound environment.
Adequate nutrition and a well-balanced and functioning
immune system are also important. Without these, white cell
debridement, bio-burden control and wound repair cannot
take place, resulting in a non-healing wound.
The stages of the wound healing process
Figure 1: The stages of the wound healing process
Injury PDGF
EGF
VEGF
Haemostasis
Aggregated Platelets
Eary Inflammatory
Inflammation Phase TGFß
Late
FGF
Inflammation
Angiogenesis Fibrin net RBC
Proliferation
Phase
Granulation
Inflammation
As soon as the clot stops the bleeding, neutrophils are attracted
Epithelialisation by the inflammatory messengers within the coagulum.
Maturation
Phase The released endothelial prostaglandins, kinins, and hista-
Remodelling
mines promote vasodilatation and neutrophil leakage into
the ECM, along with inflammatory proteins, causing oedema.
These non-specific white cells produce MMPs and reactive
oxygen species (ROS) in order to combat invading microbes
Injury and begin the phagocytic removal of debris and micro-
Tissue injury is followed by the different phases of wound organisms. The cell signalling attracts monocytes, which will
healing. morph into activated macrophages (“Pac-Man cells”). The
macrophages synthesise nitric oxide, creating more toxic
Haemostasis free radicals, vasodilatation and phagocytosis. The activated
The predominant cells active duriadothelium stimulates macrophages are essential and central to the progress
platelets to release factors essential for vasoconstriction towards the proliferative stage.1
and endothelial and other platelet activation,resulting
in the initiation of the coagulation cascade.1 Thrombin, Proliferation
followed by a temporary fibrin clot, causes the initial matrix The predominant cells during this phase are lymphocytes and
to stop bleeding. Complement prostaglandin, vascular fibroblasts. The activated macrophages release several chemical
endothelial transforming growth factors, nitric oxide and activators and messengers to promote healing. Several released
other cytokines are released at the site of injury, resulting growth factors (see Table I) stimulate vessel development and
in the production and migration and attraction of a host of angiogenesis. Connective tissue formation or fibrogenesis of the
inflammatory cells at the wound site. ECM is generated from some of these growth factors.
Professional Nursing Today 18 2010;14(3)
Wound Care: The practice and science of wound healing: history and physiology of wound healing
Figure 3: The inflammatory phase. The proteases and reactive oxygen MMPs continue to break down the debris, creating a
species act like cleaners. The neutrophils and the macrophages act granular foundation for the wound. Angiogenesis provides
like debris removers the “conduits” for further cell migration towards the centre
of the wound. Peripheral keratinocytes migrate there, and
then the “scaffolding” provided by the connective tissue and
fibroblasts for cover and closure of the wound. Fibroblasts
and endothelial cells are the primary cells in the proliferation
phase, which is under T-cell control.
Figure 4: Schematic representation of controlled inflammation.
(Graphics used with permission from Dr G Schultz.) Inflammatory
cells kill micro-organisms by phagocytosis and with free radicals
(O2-, H2O2, HOCl), and release proteases (MMPs, elastase) that remove
denatured ECM components and permit wound healing to proceed
through the inflammatory phase.
Table I: Growth factors involved in wound healing Maturation and remodelling
The fibroblasts are essential for
Growth Factor Abbreviation Source Activity scar remodelling. The remodelling
of the ECM is a very complex
Transforming TGF platelets angiogenesis process, since it contains collagen,
growth factor macrophages fibroblast proliferation proteoglycans, fibronectin and
lymphocytes collagen synthesis elastin. Fibroblasts produce
fibroblasts cell division proteoglycans, and fibronectin
keratinocytes
consists of protein connections
Platelet-derived PDGF platelets macrophage, fibroblast necessary for wound healing.
growth factor macrophages and smooth muscle cell
keratinocytes migration The average wound contracts
endothelial cells collagen synthesis by 0.6-0.75 mm/day towards its
fibroblasts
centre, with this process beginning
Fibroblast FGF macrophages angiogenesis four to five days post-injury.
growth factor fibroblasts fibroblast proliferation Myofibroblasts are responsible for
keratinocyte proliferation wound contraction. Keratinocytes
Epidermal EGF platelets collagen synthesis are responsible for the re-
growth factor macrophages epithelialisation epithelialisation from the wound
keratinocytes edges. Wound tensile strength
is dramatically increased by the
Hepatocyte HGF macrophages angiogenesis
growth factor fibroblasts fibroblast proliferation
process of scar remodelling.
keratinocyte proliferation This process of scar remodelling
continues for 6-24 months,
Vascular endothelial VEGF endothelium angiogenesis depending on the duration of
growth factor
wound healing.
Professional Nursing Today 19 2010;14(3)
Wound Care: The practice and science of wound healing: history and physiology of wound healing
Figure 5: The proliferation phase
Proliferation
Figure 6: The maturation or remodelling phase
Maturation
Professional Nursing Today 20 2010;14(3)
Wound Care: The practice and science of wound healing: history and physiology of wound healing
Figure 7: Sequence of molecular and cellular events in skin wound healing. (Graphics used with permission from Dr G Schultz.)
Conclusion 5. Gibson DJ, Schultz G. Chronic wound diagnostic for matrix
metalloproteinase. Wound Heal Southern Afr. 2002;2(2):58-70.
6. Aronow WS. Management of peripheral arterial disease. Cardiol Rev.
A firm knowledge of the different phases of wound healing 2005;13(2):61-68.
will enable the practitioner to understand advanced wound
management. Multiple factors influence wound healing, and
holistic wound management utilising a multidisciplinary
team is important. Each wound and patient is unique
and should be treated as such. By comparing the wound
healing process to that of building or renovating a house
we are able to form a much better visual understanding
of the complexity of wound healing. Just like a blueprint
is followed for building a house, so the body has a similar
plan for which certain requirements must be met in order
to facilitate wound healing. The concept of matching the
right wound healing phase to the specific wound dressing
will be addressed in future articles in this series.
References
1. Kane DP. Chronic wound healing and chronic wound management. In:
Rodeheaver GT, Sibbald RG, Krasner DL, editors. Chronic wound care: a
clinical source book for healthcare professionals. 4th ed. Wayne: Health
Management Publications Inc, 2007; p. 11-24.
2. Majuno G. The healing hand: man and wound in the ancient world.
Cambridge: Harvard University Press; 1975.
3. Helling T, McNabney WK. The role of amputation in the management
of battlefield casualties: a history of two millennia. J Trauma.
2000;49:930-939.
4. Tauber AI. Metchnikoff and the phagocytosis theory. Nature Rev Mol Cell
Biol. 2003;4:897-901
Professional Nursing Today 21 2010;14(3)
You might also like
- Wound Healing ProcessDocument34 pagesWound Healing ProcessoctyvaniNo ratings yet
- Physiology of Wound Healing PIIS0263931914001343Document6 pagesPhysiology of Wound Healing PIIS0263931914001343Nariska CooperNo ratings yet
- Zombie Brains PDFDocument1 pageZombie Brains PDFLorna GrayNo ratings yet
- Community Outreach ProgramDocument31 pagesCommunity Outreach ProgramAngelo PaulinoNo ratings yet
- Wound Healing 2022Document53 pagesWound Healing 2022John Patrick Daiz100% (1)
- Tissue RepairDocument45 pagesTissue RepairTewodros Teshome100% (1)
- 2.08 Surg - Wound Healing (Dr. Jayme 2020)Document13 pages2.08 Surg - Wound Healing (Dr. Jayme 2020)DETECTIVE CONANNo ratings yet
- Gastrointestinal Drugs: Karen Ruffin RN, MSN EdDocument104 pagesGastrointestinal Drugs: Karen Ruffin RN, MSN EdMarie KrisNo ratings yet
- Wound Healing JurnalDocument10 pagesWound Healing JurnalBrilliantNo ratings yet
- Module 5 Nursing ProcessDocument34 pagesModule 5 Nursing Processscrewdriver100% (5)
- CircCircuit Protection in Health Care Facilitiesuit Protection in Health Care FacilitiesDocument43 pagesCircCircuit Protection in Health Care Facilitiesuit Protection in Health Care FacilitiesMenaNo ratings yet
- Principles of Wound HealingDocument8 pagesPrinciples of Wound HealingTracy100% (6)
- Interval TrainingDocument24 pagesInterval TrainingRukmantaraNo ratings yet
- Healing of OralwoundsDocument38 pagesHealing of OralwoundsPuspa AdhikariNo ratings yet
- Jcad 13 2 33Document11 pagesJcad 13 2 33ntnquynhproNo ratings yet
- Wound Healing )Document14 pagesWound Healing )miftahuldursinaNo ratings yet
- Tissue Engineering and Wound Healing: A Short Case StudyFrom EverandTissue Engineering and Wound Healing: A Short Case StudyRating: 5 out of 5 stars5/5 (2)
- Skin and Soft Tissue Injuries & InfectionsDocument221 pagesSkin and Soft Tissue Injuries & InfectionsMario Espinosa100% (1)
- Guidelines For Contemporary Air-Rotor StrippingDocument6 pagesGuidelines For Contemporary Air-Rotor StrippingGerman Cabrera DiazNo ratings yet
- Cardio CuracionDocument11 pagesCardio Curacionapi-613248156No ratings yet
- Tissue Injury and Healing: Brent Kincaid, DDS, John P. Schmitz, DDS, PHDDocument10 pagesTissue Injury and Healing: Brent Kincaid, DDS, John P. Schmitz, DDS, PHDAmith HadhimaneNo ratings yet
- The Roles of in Ammation in Keloid and Hypertrophic ScarsDocument10 pagesThe Roles of in Ammation in Keloid and Hypertrophic ScarsireneardianiNo ratings yet
- Manejo de HeridasDocument17 pagesManejo de HeridassaortizpNo ratings yet
- A Practical Guide To Wound Healing: Learning ObjectivesDocument15 pagesA Practical Guide To Wound Healing: Learning ObjectivesVanessaGGSNo ratings yet
- Artcol Ccatrici 2019Document6 pagesArtcol Ccatrici 2019Krina MarynaNo ratings yet
- Abd 91 05 0614Document7 pagesAbd 91 05 0614Selvy Anriani GasperszNo ratings yet
- Lecture 10 Wound HealingDocument10 pagesLecture 10 Wound HealingRose Ann RaquizaNo ratings yet
- Wound Healing and Perioperative Care Vol 18 Issue 1 Feb 2006 Omfs PDFDocument7 pagesWound Healing and Perioperative Care Vol 18 Issue 1 Feb 2006 Omfs PDFR KNo ratings yet
- Cellular Human Tissue-Engineered Skin Substitutes Investigated For Deep and Dif Ficult To Heal InjuriesDocument23 pagesCellular Human Tissue-Engineered Skin Substitutes Investigated For Deep and Dif Ficult To Heal InjuriesNovelas, Series y PelículasNo ratings yet
- Bovine Surger y of The Skin: Matt D. MiesnerDocument10 pagesBovine Surger y of The Skin: Matt D. MiesnerGuadalupe Cristina Chuchón CáceresNo ratings yet
- Basic Science of Wound HealingDocument4 pagesBasic Science of Wound HealingMarnia SulfianaNo ratings yet
- Principles of Wound HealingDocument16 pagesPrinciples of Wound HealingApril FloresNo ratings yet
- 10 1 1 473 9492 PDFDocument9 pages10 1 1 473 9492 PDFarseniosilvaNo ratings yet
- Wound RepairDocument24 pagesWound RepairSrishti SrivastavaNo ratings yet
- Review Article: Nanotechnology-Based Therapies For Skin Wound RegenerationDocument12 pagesReview Article: Nanotechnology-Based Therapies For Skin Wound RegenerationDina Arwina DalimuntheNo ratings yet
- Corneal Wound Healing After Laser Vision Correction: Leopoldo Spadea, Daniele Giammaria, Paolo TrabuccoDocument6 pagesCorneal Wound Healing After Laser Vision Correction: Leopoldo Spadea, Daniele Giammaria, Paolo TrabuccoNabita AuliaNo ratings yet
- Management of Ocular Adnexal TraumaDocument21 pagesManagement of Ocular Adnexal TraumamariaNo ratings yet
- Potential Anti-Inflammatory Treatments For Chronic Wounds: Mckelvey K, Xue M, Whitmont K, Shen K, Cooper A & Jackson CDocument4 pagesPotential Anti-Inflammatory Treatments For Chronic Wounds: Mckelvey K, Xue M, Whitmont K, Shen K, Cooper A & Jackson CAnonymous IruFyBNo ratings yet
- Curacion de Heridas y Tratamiento de HeridasDocument17 pagesCuracion de Heridas y Tratamiento de HeridasVar AndaNo ratings yet
- Management of Keloids and Hypertrophic Scars Current Anf Emerging OptionsDocument12 pagesManagement of Keloids and Hypertrophic Scars Current Anf Emerging OptionsCyntia RatnadiNo ratings yet
- Wound Healing and Its Impairment in The Diabetic Foot: ReviewDocument9 pagesWound Healing and Its Impairment in The Diabetic Foot: ReviewJoey TsaiNo ratings yet
- Chronic Inflammation Healing and RepairDocument51 pagesChronic Inflammation Healing and Repairahmed mokhtarNo ratings yet
- Wound Healing1Document8 pagesWound Healing1muralidhar_mettaNo ratings yet
- CicatrizacionDocument19 pagesCicatrizacionAlejandro MejiaNo ratings yet
- Martin Paul PDFDocument8 pagesMartin Paul PDFSteven NoriegaNo ratings yet
- Giles 2007 Wound Healing in Spontaneous Perforation or Myringotomy Middle Ear ReconstructionDocument3 pagesGiles 2007 Wound Healing in Spontaneous Perforation or Myringotomy Middle Ear Reconstructionprashantpatel.jaipurNo ratings yet
- 2020 Wound Healing Cellular Mechanisms and PathologicalDocument14 pages2020 Wound Healing Cellular Mechanisms and PathologicalSOPHIASTIA KUSBIANTI MHS 2017No ratings yet
- International Immunopharmacology: SciencedirectDocument10 pagesInternational Immunopharmacology: SciencedirectRohadatul AisyNo ratings yet
- Anatomy & Phyiology of The SkinDocument32 pagesAnatomy & Phyiology of The SkinDanielle Louise CaingatNo ratings yet
- Leoni 2015Document10 pagesLeoni 2015Yunita SaharawatiNo ratings yet
- GROUP6Document22 pagesGROUP6AYUSHI PATELNo ratings yet
- Biomaterials in Wound Healing PDFDocument11 pagesBiomaterials in Wound Healing PDFshubhamNo ratings yet
- Stem CellDocument14 pagesStem CellsattwikaNo ratings yet
- The Basic Science of Wound Healing: SummaryDocument23 pagesThe Basic Science of Wound Healing: SummaryKevin AdrianNo ratings yet
- Incisions and ClosureDocument14 pagesIncisions and ClosuregabiptenorioNo ratings yet
- Desjardins Park2018Document6 pagesDesjardins Park2018Stella SunurNo ratings yet
- Wounds Biology Pathology and ManagementDocument13 pagesWounds Biology Pathology and ManagementChilo PrimaNo ratings yet
- Wound Healing and Tissue RepairDocument27 pagesWound Healing and Tissue RepairKELVIN MAYOMBONo ratings yet
- Keloids and Hypertrophic Scars: Pathophysiology, Classification, and TreatmentDocument16 pagesKeloids and Hypertrophic Scars: Pathophysiology, Classification, and TreatmentStella SunurNo ratings yet
- Biology of PeriodontalDocument78 pagesBiology of PeriodontalSudip SenNo ratings yet
- Patho FEU PGI BCA Exit Exam May 2020Document34 pagesPatho FEU PGI BCA Exit Exam May 2020Sheryl Layne LaoNo ratings yet
- 2 Wound HealingDocument6 pages2 Wound HealingMohamad AlfarisNo ratings yet
- Principles of Wound HealingDocument28 pagesPrinciples of Wound HealingRafael BagusNo ratings yet
- Wound Healing Bahan 4Document42 pagesWound Healing Bahan 4Deden SiswantoNo ratings yet
- Autologous Cellular Rejuvenation (ACR)Document25 pagesAutologous Cellular Rejuvenation (ACR)4uslimbeauty clinicNo ratings yet
- Stmcls..exosomes 33 7 2158Document12 pagesStmcls..exosomes 33 7 2158Muhammad Javed GabaNo ratings yet
- Wound Healing & Wound Care: Souvik Adhikari Postdoctoral TraineeDocument55 pagesWound Healing & Wound Care: Souvik Adhikari Postdoctoral TraineeClaudio Luis VenturiniNo ratings yet
- Innate Immune Cell-Epithelial Crosstalk During Wound RepairDocument11 pagesInnate Immune Cell-Epithelial Crosstalk During Wound Repairvanessa_werbickyNo ratings yet
- Power and Politics: Virginia W. Adams, PH.D., R.N. Dean UNCW School of Nursing Adamsv@uncw - EduDocument30 pagesPower and Politics: Virginia W. Adams, PH.D., R.N. Dean UNCW School of Nursing Adamsv@uncw - EduscrewdriverNo ratings yet
- GSPC Leaflet MasterDocument2 pagesGSPC Leaflet MasterscrewdriverNo ratings yet
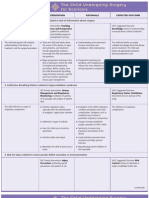
- NURSING CARE PLAN The Child Undergoing Surgery For ScoliosisDocument3 pagesNURSING CARE PLAN The Child Undergoing Surgery For ScoliosisscrewdriverNo ratings yet
- Safety Inspection Checklist Project: Location: Inspector: DateDocument2 pagesSafety Inspection Checklist Project: Location: Inspector: Dateyono DaryonoNo ratings yet
- Physical Fitness Test Individual Score CardDocument12 pagesPhysical Fitness Test Individual Score CardJunessa TadinaNo ratings yet
- UrethralstricturesDocument37 pagesUrethralstricturesNinaNo ratings yet
- HKS CannabisDocument21 pagesHKS CannabisRavioli Boo GaddamNo ratings yet
- Written Assignment Unit 2 - HS 2212Document5 pagesWritten Assignment Unit 2 - HS 2212bnvjNo ratings yet
- Marchand 2012Document20 pagesMarchand 2012Elton MatsushimaNo ratings yet
- Chapter 6 QuestionsDocument2 pagesChapter 6 QuestionsGabo DanteNo ratings yet
- Building Occupational Safety and Health k3 Analysis of The Work Environment and Work DisciplineDocument10 pagesBuilding Occupational Safety and Health k3 Analysis of The Work Environment and Work Disciplineipraul167No ratings yet
- Proforma For College - Information Regarding Fee, Bond - Conditions EtcDocument2 pagesProforma For College - Information Regarding Fee, Bond - Conditions EtcThe Indian DentistNo ratings yet
- ETW-2013 Amma PDFDocument100 pagesETW-2013 Amma PDFRosalete LimaNo ratings yet
- F17 Reflection 383 FN - 15 Nov 17Document7 pagesF17 Reflection 383 FN - 15 Nov 17jigsawNo ratings yet
- Lab 11 AntianginalDocument4 pagesLab 11 AntianginalanaNo ratings yet
- Phys Ther 2012 Macedo 363 77Document18 pagesPhys Ther 2012 Macedo 363 77Anang FajarNo ratings yet
- AH1N1 PPT PresentationDocument28 pagesAH1N1 PPT PresentationIna Isabela CostiboloNo ratings yet
- Brain Tumors - KY Cancer RegistryDocument45 pagesBrain Tumors - KY Cancer RegistryMohammad Galih PratamaNo ratings yet
- Resume - EportfolioDocument3 pagesResume - Eportfolioapi-337162374No ratings yet
- 4th Public Health Conf. Abstract Revised 29-8-2023..... YyDocument1 page4th Public Health Conf. Abstract Revised 29-8-2023..... YyskyremedyhubNo ratings yet
- Reactive Hyperplastic Lesions of The Oral CavityDocument8 pagesReactive Hyperplastic Lesions of The Oral CavityMarïsa CastellonNo ratings yet
- Strengthening Health Emergency Management System Through The ILHZDocument7 pagesStrengthening Health Emergency Management System Through The ILHZCliff GubatNo ratings yet
- Stroke PamphletDocument12 pagesStroke Pamphletapi-232971337No ratings yet
- Chapter 3 Definition - DisabilityDocument12 pagesChapter 3 Definition - DisabilityAnimesh KumarNo ratings yet
- Women Devlopment-Government Policies and ProgrammesDocument19 pagesWomen Devlopment-Government Policies and ProgrammesVishalMishraNo ratings yet
- (ENGLISH) Perbandingan Khasiat Cetirizine Dan LoratadinDocument9 pages(ENGLISH) Perbandingan Khasiat Cetirizine Dan Loratadinintan nabilah pratiwiNo ratings yet