Professional Documents
Culture Documents
Sepsis Algorithm PDF
Uploaded by
Ryaa Nitaa AdyaaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Sepsis Algorithm PDF
Uploaded by
Ryaa Nitaa AdyaaCopyright:
Available Formats
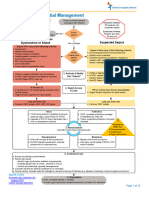
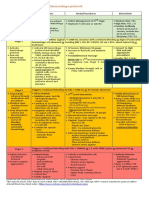
Northwell Health
ED Sepsis/Severe Sepsis Management
Patient with suspected significant
ARRIVAL AND EVALUATION
infection (i.e. possible admission)
POSSIBLE SEPSIS
PLUS Probable Severe Sepsis
Two of the following:
SIRS Criteria: Two of the following: • Temp > 101 F or < 96.8 F OR Recent
• Temp > 101 F or < 96.8 F Fever, OR clinical suspicion of Infection.
• Pulse > 90 bpm • SBP < 90 or ↓ in SBP > 40 mm Hg from
• Resp Rate > 20/min baseline, or MAP < 65
• WBC > 12K, < 4K or Bands > 10% • Pulse > 120 bpm T-0 =
• Resp rate > 24 / min Triage
• New Unexplained Altered Time
Mental Status
Clinician evaluates patient and
suspects early sepsis; orders labs
(must include lactate/ BCs X 2).
Code SEPSIS
T-0 =
Lactate
SEPSIS Order ACTIVATE “Code Sepsis”
1. Activate “Code Sepsis” in ED
2. Two RNs to bedside if possible.
3. Place 18 G IV, Ask MD re: 2nd Line & Foley
1. Document Accurate Blood Culture 4. Draw Labs for Sepsis Panel in < 30 min.
and Lactate draw times 5. Prepare for Fluid Bolus, Alert X-Ray tech
2. Repeat Vital Signs in 30 minutes 6. Source Control as appropriate
3. Source Control as appropriate
Severe Sepsis Resuscitation Elements
Lactate draw < 30 min and result < 90 min
Sepsis Resuscitation Elements •
INTERVENTION
• BCs X 2 ordered and drawn before Antibiotic
(Unless clinically contraindicated) • Antibiotics < 60 min of Code Sepsis
• Lactate ordered and resulted < 90 min • IVF bolus started < 30 min of Code Sepsis
• BCs X 2 ordered and drawn before Abx • Fluids: NS 500 mL boluses q 15 min to total
• Abx < 3 hrs of arrival 30mL/kG of actual body weight
• IV fluids –consider NS 1 - 2 L over 2 hrs • Repeat lactate approximately 30 - 60 min s/p
• Repeat lactate if initial lactate is elevated fluid bolus completion
• Monitor, document VS < q 60 min • Cont. monitoring, document VS q 15 min x 90
minutes, then q 60 minutes
DURING ED COURSE
Severe Sepsis Dx Repeat Lactate > 4 or
Criteria met (Dx SS) if: YES Code
SEPSIS Persistent SBP < 90
• Lactate > 2.0 OR
• SBP < 90, or ↓ in SBP > NO YES
40 mm Hg from NEW End Organ
baseline, OR MAP < 65 Dysfunction Monitor VS, Septic Shock Bundle
• Severe Sepsis VS •PaO2/FiO2 ratio < 300 mental status, • Consider Additional NS
criteria met OR etc boluses and/or
• Increasing O2
• New End Organ • Start Vasopressor
demand to maintain
Dysfunction (SEE BOX) Norepinephrine (0.05
sat > 90% micrograms/kG/min
NO •Cr > 2.0 or > 50% Path • Repeat Lactate level
increase from known Complete approximately 30 - 60
DISPOSITION
Continue monitoring VS, baseline Document min s/p fluid bolus
mental status, etc. •Urine Output < 0.5 Primary Dx: completion
mL/kG/hr for > 2 hrs Severe Sepsis • Clinical volume
•Bilirubin > 2.0 mg/dL Secondary Dx: reassessment within
Suspected 6 hrs
Path Complete •Platelet Count < 100K
Source
Document •INR > 1.5,
Primary Dx: Sepsis, PTT > 60 sec
Secondary Dx: Suspected Path Complete
•New onset altered
Source Document Primary Dx: Septic Shock,
Mental Status
Secondary Dx: Suspected Source
•Lactate > 2.0
Consultation, disposition, and transfer of care can occur at any point in the above care map.
Hand off communication is critical and must include discussion of incomplete and complete elements.
Northwell Health
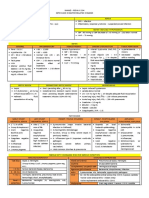
Inpatient Sepsis/Severe Sepsis Management
Sepsis
Patient with known or suspected
ARRIVAL AND EVALUATION
significant infection SEVERE SEPSIS
PLUS
SIRS Criteria: Two of the
following:
• Temp > 101F or < 96.8 F
• Pulse > 90 bpm 1. Two RNs to bedside if possible.
• Resp Rate > 20/min 2. Place 18 G IV, Ask MD re: 2nd Line & Foley
• WBC >12K, <4K or Bands >10% 3. Draw Labs for Sepsis Panel in < 30 min.
4. Prepare for Fluid Bolus, Alert X-Ray tech
5. Source Control as appropriate
Clinician evaluates patient and 6. Consider transfer to a higher level of care
suspects early sepsis; orders labs
(must include lactate/ BCs X 2).
1. Document Accurate Blood Culture
Severe Sepsis Resuscitation Elements
and Lactate draw times
• Lactate draw < 30 min and result < 90 min
2. Repeat Vital Signs in 30 minutes
• BCs X 2 ordered and drawn before Antibiotic if not
3. Source Control as appropriate
already drawn within past 48 hrs
• Initiate or confirm appropriate Antibiotics < 60 min
• IVF bolus started < 30 min of Severe Sepsis
recognition
• Fluids: NS 500 mL boluses q 15 min to total
30mL/kG of actual body weight
Sepsis Resuscitation Elements • Repeat lactate approximately 30 - 60 min s/p fluid
INTERVENTION
(Unless clinically contraindicated) bolus completion
• Lactate ordered and resulted < 90 min • Cont. monitoring, document VS q 15 min x 90
• BCs X 2 ordered and drawn before Abx if minutes, then q 60 minutes
not already drawn within past 48 hrs
• Initiate or confirm Abx < 3 hrs
• IV fluids –consider NS 1 - 2 L over 2 hrs
• Repeat lactate if initial lactate is elevated
Severe Sepsis Dx Repeat Lactate > 4 or
Criteria met (Dx SS) if: Persistent SBP < 90
YES
• SBP < 90, or ↓ in SBP
> 40 mm Hg from NO YES
baseline, OR NEW (otherwise
MAP < 65 unexplained) End
Monitor VS,
• New End Organ Organ Dysfunction mental status,
Septic Shock Bundle
Dysfunction (SEE •PaO2/FiO2 ratio < 300 etc
• Consider Additional NS
BOX) • Increasing O2 demand boluses and/or
• Lactate > 2.0 to maintain sat > 90% • Start Vasopressor
Norepinephrine (0.05
•Cr > 2.0 or > 50%
NO increase from known Path microgram/kG/min)
Complete • Repeat lactate
baseline approximately 30-60
Continue monitoring VS, Document
DISPOSITION
•Urine Output < 0.5 min s/p fluid bolus
mental status, etc. Primary Dx:
mL/kG/hr for > 2 hrs Severe Sepsis completion
•Bilirubin > 2.0 mg/dL Secondary Dx: • Clinical volume re-
•Platelet Count < 100K Suspected assessment within 6 hrs
Path Complete Source
•INR > 1.5, PTT > 60 sec
Document
Primary Dx: Sepsis, •New onset altered
Secondary Dx: Suspected Mental Status
Path Complete
Source •Lactate > 2.0 Document Primary Dx: Septic Shock,
Secondary Dx: Suspected Source
Consultation, disposition, and transfer of care can occur at any point in the above care map.
Hand off communication is critical and must include discussion of incomplete and complete elements.
You might also like
- Recent Advances in The Treatment of ShockDocument52 pagesRecent Advances in The Treatment of ShockasupicuNo ratings yet
- Management Algorithm For Patients With Severe SepsisDocument1 pageManagement Algorithm For Patients With Severe SepsisgilankwibawaNo ratings yet
- SepsisDocument10 pagesSepsisJessa MaeNo ratings yet
- Kegawatdaruratan Bidang Ilmu Penyakit Dalam: I.Penyakit Dalam - MIC/ICU FK - UNPAD - RS DR - Hasan Sadikin BandungDocument47 pagesKegawatdaruratan Bidang Ilmu Penyakit Dalam: I.Penyakit Dalam - MIC/ICU FK - UNPAD - RS DR - Hasan Sadikin BandungEfa FathurohmiNo ratings yet
- NRNP 6566 Week 4 Knowledge CheckDocument7 pagesNRNP 6566 Week 4 Knowledge Checkmary011danielNo ratings yet
- Tumor Lysis Oral Boards CasesDocument15 pagesTumor Lysis Oral Boards Casesczalesky66No ratings yet
- Protocols Checklists Sepsis Alert Wesley HealthcareDocument1 pageProtocols Checklists Sepsis Alert Wesley HealthcareeryxspNo ratings yet
- SepsisDocument1 pageSepsisCharlie LeeNo ratings yet
- (Systemic Inflammatory Response Syndrome) : Norepinephrine Vasopressin or DopamineDocument2 pages(Systemic Inflammatory Response Syndrome) : Norepinephrine Vasopressin or DopaminejamesomooreNo ratings yet
- Dengue: History Physical Examination InvestigationDocument4 pagesDengue: History Physical Examination InvestigationNik Hanisah Zuraidi AfandiNo ratings yet
- Protocols ST Helens Adult Sepsis Management PathwayDocument1 pageProtocols ST Helens Adult Sepsis Management Pathwayputra purnomoNo ratings yet
- Mis C Clinical GuidelineDocument9 pagesMis C Clinical GuidelineasyqarNo ratings yet
- Mis C Clinical GuidelineDocument8 pagesMis C Clinical GuidelineClamargav aNo ratings yet
- SEPSIS Rev 21092020Document46 pagesSEPSIS Rev 21092020rani asfiyaNo ratings yet
- EGDT SepsisDocument8 pagesEGDT Sepsissiti fatmalaNo ratings yet
- The PatientDocument9 pagesThe PatientJan Crizza Dale R. FrancoNo ratings yet
- Lit 2. Sepsis-3 Abdul Hakeem Al Hashim, MD, FRCPCDocument76 pagesLit 2. Sepsis-3 Abdul Hakeem Al Hashim, MD, FRCPCKomang_JananuragaNo ratings yet
- Sepsis: ManagementDocument50 pagesSepsis: Managementer bcmNo ratings yet
- SEPSIS Early DetectionDocument35 pagesSEPSIS Early DetectionKomang_JananuragaNo ratings yet
- SepsisDocument3 pagesSepsisPhilip Poerworahjono100% (3)
- Evaluation and Diagnosis: New York State Department of HealthDocument2 pagesEvaluation and Diagnosis: New York State Department of HealthNisa Annisa ArfiyantiNo ratings yet
- NEONATOLOGYDocument8 pagesNEONATOLOGYmymamym100% (1)
- CURB-65 Score For Pneumonia Score DescriptionDocument14 pagesCURB-65 Score For Pneumonia Score DescriptionMelvin CarewNo ratings yet
- Cookeville Regional Medical Center Severe Sepsis/Septic Shock Clinical PathwayDocument4 pagesCookeville Regional Medical Center Severe Sepsis/Septic Shock Clinical PathwayArnelli HutagalungNo ratings yet
- Morning Report: Physician in ChargeDocument33 pagesMorning Report: Physician in ChargeIka AyuNo ratings yet
- The Intern Pocket Card Surviving GraysDocument2 pagesThe Intern Pocket Card Surviving GraysKathleen Grace ManiagoNo ratings yet
- Ecg PediaDocument2 pagesEcg PediaAdrian Ulu100% (1)
- Case Presentation On Supraventricular TachycardiaDocument64 pagesCase Presentation On Supraventricular TachycardiaHazel AsperaNo ratings yet
- Fluid Resuscitation in SepsisDocument68 pagesFluid Resuscitation in SepsisRonald Ariyanto WiradirnataNo ratings yet
- High Yield Surgery Compatible Version-2Document20 pagesHigh Yield Surgery Compatible Version-2zoozsuhai2No ratings yet
- CODE STROKE Checklist:: NotesDocument1 pageCODE STROKE Checklist:: NotesAdam MochtarNo ratings yet
- Case Scenario:: Is An Eye Finding Occurring Early inDocument5 pagesCase Scenario:: Is An Eye Finding Occurring Early inDenice Tamayo De GuzmanNo ratings yet
- From SIRS To Septic Shock (2022!01!22 00-25-28 UTC)Document1 pageFrom SIRS To Septic Shock (2022!01!22 00-25-28 UTC)Andrea AndradaNo ratings yet
- Shanz - Pedia Ii 2.04Document4 pagesShanz - Pedia Ii 2.04Petrina XuNo ratings yet
- STEMI Thrombolysis Protocol STElevation MIDocument6 pagesSTEMI Thrombolysis Protocol STElevation MISurya AtmajaNo ratings yet
- C. DiffDocument7 pagesC. DiffrNo ratings yet
- Sample Case ScenarioDocument8 pagesSample Case ScenarioJan Crizza Dale R. FrancoNo ratings yet
- High Yield Surgery Compatible Version PDFDocument20 pagesHigh Yield Surgery Compatible Version PDFSurgery CSC1No ratings yet
- Stemi Pathway: Record TimeDocument2 pagesStemi Pathway: Record TimeOlga Jadha CasmiraNo ratings yet
- 13.30 DR Arunraj Navaratnarajah - The Septic PatientDocument49 pages13.30 DR Arunraj Navaratnarajah - The Septic PatientagusNo ratings yet
- Februari, 22 Morning ReportDocument25 pagesFebruari, 22 Morning Reportnadia shabriNo ratings yet
- Post Arrest Hemodynamic OptDocument1 pagePost Arrest Hemodynamic OptMarinaJiménezNo ratings yet
- AKI Pathway (Nottingham University Hospitals April 2015)Document3 pagesAKI Pathway (Nottingham University Hospitals April 2015)Yadi SupriyadiNo ratings yet
- SYOK - Desi Surya IniDocument40 pagesSYOK - Desi Surya IniDesi Suryani DewiNo ratings yet
- Anak - Kasus 7 - Kelompok 7Document48 pagesAnak - Kasus 7 - Kelompok 7mehakNo ratings yet
- AUBF - MidtermsDocument14 pagesAUBF - MidtermsRomie Solacito100% (1)
- Sepsis in The Setting of AspleniaDocument30 pagesSepsis in The Setting of Aspleniaapi-740273867No ratings yet
- Haemorrhage ProtocolDocument1 pageHaemorrhage ProtocolHerwinda GeraldineNo ratings yet
- Resusitasi CairanDocument48 pagesResusitasi Cairanadi tiarmanNo ratings yet
- Sop NBNDocument55 pagesSop NBNSanthosh KumarNo ratings yet
- EGDT - PICU-NICU-Bandung-2016-DadangHDocument63 pagesEGDT - PICU-NICU-Bandung-2016-DadangHvillnachintyaNo ratings yet
- Case Study PDFDocument12 pagesCase Study PDFAngelica AdlawanNo ratings yet
- Post PCI Care When To ReferDocument25 pagesPost PCI Care When To ReferRahmat HidayatullahNo ratings yet
- Severe DengueDocument101 pagesSevere Denguetarakeeshbai1802No ratings yet
- Rhythm QRS Duration Atrial Rate QT Interval Ventricular Rate QRS Axis (Compute)Document10 pagesRhythm QRS Duration Atrial Rate QT Interval Ventricular Rate QRS Axis (Compute)Luis PadillaNo ratings yet
- Group Fdar Hemophilia ADocument2 pagesGroup Fdar Hemophilia AMika SaldañaNo ratings yet
- ECG How To InterpretDocument10 pagesECG How To InterpretMohamad DanialNo ratings yet
- Touch Imprint Cytology: A Rapid and Accurate Method For Diagnosis of Oral Cancer Original ArticleDocument19 pagesTouch Imprint Cytology: A Rapid and Accurate Method For Diagnosis of Oral Cancer Original ArticleNiketa SharmaNo ratings yet
- Strategies For Acute Metabolic DisordersDocument14 pagesStrategies For Acute Metabolic DisordersAhmed AnwarNo ratings yet
- Acute Pancreatitis PresentationDocument24 pagesAcute Pancreatitis PresentationhtmgNo ratings yet
- Lab Report 15438869 20231127064225Document1 pageLab Report 15438869 20231127064225carilloabhe21No ratings yet
- NARPAA E-Class Module 3 - Historical Definitions of AutismDocument19 pagesNARPAA E-Class Module 3 - Historical Definitions of AutismnarpaaNo ratings yet
- Lab Report Activity GlucoseDocument6 pagesLab Report Activity GlucoseTheodore LiwonganNo ratings yet
- Nursing Care Plan 2021-2022Document7 pagesNursing Care Plan 2021-2022AhmedGamalNo ratings yet
- SBAR Communication Form: and Progress NoteDocument3 pagesSBAR Communication Form: and Progress NoteTisa Meriel100% (1)
- Social Change Campaign in IndiaDocument7 pagesSocial Change Campaign in IndiaGauri GargNo ratings yet
- Axis I Clinical Psychiatric Disorders - LMM-1Document11 pagesAxis I Clinical Psychiatric Disorders - LMM-1richhuangNo ratings yet
- Mock Ospe Me211Document15 pagesMock Ospe Me211sahirbuleNo ratings yet
- 3.2 Dr. Taufin SpOT - Operating RoomDocument29 pages3.2 Dr. Taufin SpOT - Operating RoomTaqwatin Ma'rifahNo ratings yet
- Abatacept Hervey2006Document9 pagesAbatacept Hervey2006Calvin Tanuwijaya Stick BolaNo ratings yet
- Swedish Medical Center Patient LetterDocument2 pagesSwedish Medical Center Patient LetterMichael_Lee_RobertsNo ratings yet
- Jin Gui Shen QiDocument2 pagesJin Gui Shen QiJoana ValenteNo ratings yet
- Ap Lang Memoir EssayDocument13 pagesAp Lang Memoir Essayapi-305343417100% (1)
- Aplastic Anemia: Savita HandayaniDocument24 pagesAplastic Anemia: Savita HandayaniAnna Puteri GozaliNo ratings yet
- Cerebral CirculationDocument85 pagesCerebral CirculationCharles Nkurunziza100% (2)
- Teaching-Plan-Health-Education-Plan-Diabetes Mellitus TYPE IIDocument3 pagesTeaching-Plan-Health-Education-Plan-Diabetes Mellitus TYPE IIkasjdkasNo ratings yet
- Principles of Test Taking MTCDocument28 pagesPrinciples of Test Taking MTCMyk MacalintalNo ratings yet
- Introduction History Examination (Prosthodontics)Document37 pagesIntroduction History Examination (Prosthodontics)sarah0% (1)
- Humoral ImmunityDocument86 pagesHumoral ImmunitySinthiya KanesaratnamNo ratings yet
- Telegram@DrbooksDocument493 pagesTelegram@DrbooksDanh Nguyễn100% (3)
- Multi-Frequency and Multi-Component TympanometryDocument8 pagesMulti-Frequency and Multi-Component TympanometryEstudiantede FonoaudiologíaNo ratings yet
- Carevent Dra Rev 8-10-16Document2 pagesCarevent Dra Rev 8-10-16Adrian MorenoNo ratings yet
- Research Paper - Celiac DiseaseDocument5 pagesResearch Paper - Celiac Diseaseapi-316625517100% (1)
- Maternal and Child Health Programmes: MCH ServicesDocument10 pagesMaternal and Child Health Programmes: MCH ServicesRosebel LaguraNo ratings yet
- Dead Space ManagementDocument26 pagesDead Space ManagementIgnasNo ratings yet
- "The Man Who Mistook His Wife For Hat" Is ADocument9 pages"The Man Who Mistook His Wife For Hat" Is AIADT Psy50% (2)
- Rosh Review 11Document6 pagesRosh Review 11Sarwar BaigNo ratings yet