Professional Documents
Culture Documents
Doengoes Bersihan Jalan Nafas Tidak Efektif
Uploaded by
Anonymous ZdqtAqT1W0 ratings0% found this document useful (0 votes)
20 views4 pagesDoenges
Copyright
© © All Rights Reserved
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document0 ratings0% found this document useful (0 votes)
20 views4 pagesDoengoes Bersihan Jalan Nafas Tidak Efektif
Uploaded by
Anonymous ZdqtAqT1WYou are on page 1of 4
NURSING PRIORITY NO.
1 To maintain adequate, patent airway:
• Identify client populations at risk. Persons with impaired ciliary function (e.g., cystic
fibrosis,
status post-heart-lung transplantation); those with excessive or abnormal mucus production
(e.g., asthma, emphysema, pneumonia, dehydration, bronchiectasis, mechanical ventilation);
those with impaired cough function (e.g., neuromuscular diseases, such as muscular
dystrophy;
neuromotor conditions, such as cerebral palsy, spinal cord injury); those with swallowing
abnormalities
(e.g., poststroke, seizures, head/neck cancer, coma/sedation, tracheostomy, facial
burns/trauma/surgery); those who are immobile (e.g., sedated individual, frail elderly,
developmental delay); infant/child (e.g., feeding intolerance, abdominal distention, and
emotional stressors that may compromise airway) are all at risk for problems with
maintenance
of open airways.1,2
• Assess level of consciousness/cognition and ability to protect own airway. Information
essential
for identifying potential for airway problems, providing baseline level of care needed, and
influencing choice of interventions.
• Evaluate respiratory rate/depth and breath sounds. Tachypnea is usually present to some
degree and may be pronounced during respiratory stress. Respirations may be shallow. Some
degree of bronchospasm is present with obstruction in airways and may/may not be
manifested
in adventitious breath sounds, such as scattered moist crackles (bronchitis), faint sounds with
expiratory wheezes (emphysema), or absent breath sounds (severe asthma).2
• Position head appropriate for age and condition/disorder. Repositioning head may, at times,
be all that is needed to open or maintain open airway in at-rest or compromised individual,
such as one with sleep apnea.
• Insert oral airway, using correct size for adult or child, when indicated. Have appropriate
emergency equipment at bedside (such as tracheostomy equipment, ambu-bag, suction
apparatus) to restore or maintain an effective airway.3,4
• Evaluate amount and type of secretions being produced. Excessive and/or sticky mucus can
make it difficult to maintain effective airways, especially if client has impaired cough
function,
is very young or elderly, is developmentally delayed, has restrictive or obstructive lung
disease,
or is mechanically ventilated.5
• Note ability/effectiveness of cough. Cough function may be weak or ineffective in diseases
and conditions such as extremes in age (e.g., premature infant or elderly), cerebral palsy,
muscular dystrophy, spinal cord injury, brain injury, postsurgery, and/or mechanical
ventilation
due to mechanisms affecting muscles of throat, chest, and lungs.5,6
• Suction (nasal/tracheal/oral), when indicated, using correct-size catheter and suction
timing for child or adult to clear airway when secretions are blocking airways, client is
unable to clear airway by coughing, cough is ineffective, infant is unable to take oral
feedings
because of secretions, or ventilated client is showing desaturation of oxygen by oximetry or
ABGs.2,5,7
ineffective AIRWAY CLEARANCE
52
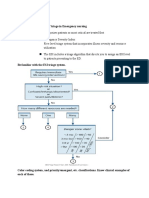
• Assist with/prepare for appropriate testing (e.g., pulmonary function/sleep studies) to
identify
causative/precipitating factors.
• Assist with procedures (e.g., bronchoscopy, tracheostomy) to clear/maintain open airway.
• Keep environment free of smoke, dust, and feather pillows according to individual situation.
Precipitators of allergic type of respiratory reactions that can trigger/exacerbate acute
episode.3
NURSING PRIORITY NO. 2 To mobilize secretions:
• Elevate head of the bed/change position, as needed. Elevation/upright position facilitates
respiratory function by use of gravity; however, the client in severe distress will seek position
of
comfort.3
• Position appropriately (e.g., head of bed elevated, side-to-side) and discourage use of
oilbased
products around nose to prevent vomiting with aspiration into lungs. (Refer to NDs
risk for Aspiration, impaired Swallowing.)
• Encourage/instruct in deep-breathing and directed-coughing exercises; teach (presurgically)
and reinforce (postsurgically) breathing and coughing while splinting incision to maximize
cough effort, lung expansion, and drainage, and to reduce pain impairment.
• Mobilize client as soon as possible. Reduces risk or effects of atelectasis, enhancing lung
expansion and drainage of different lung segments.5
• Administer analgesics, as indicated. Analgesics may be needed to improve cough effort
when
pain is inhibiting. Note: Overmedication, especially with opioids, can depress respirations
and
cough effort.
• Administer medications (e.g., expectorants, anti-inflammatory agents, bronchodilators, and
mucolytic agents), as indicated, to relax smooth respiratory musculature, reduce airway
edema, and mobilize secretions.8
• Increase fluid intake to at least 2000 mL/day within cardiac tolerance (may require IV in
acutely ill, hospitalized client). Encourage/provide warm versus cold liquids, as appropriate.
Warm hydration can help liquefy viscous secretions and improve secretion clearance. Note:
Individuals with compromised cardiac function may develop symptoms of CHF (crackles,
edema, weight gain).4,5
• Provide ultrasonic nebulizer/room humidifier, as needed, to deliver supplemental
humidification,
helping to reduce viscosity of secretions.
• Assist with use of respiratory devices and treatments (e.g., intermittent positive-pressure
breathing [IPPB], incentive spirometer [IS], positive expiratory pressure [PEP] mask,
mechanical ventilation, oscillatory airway device [flutter], assisted and directed cough
techniques, etc.). Various therapies/modalities may be required to maintain adequate
airways,
improve respiratory function and gas exchange. (Refer to NDs ineffective Breathing Pattern,
impaired Gas Exchange, impaired spontaneous Ventilation.)3,11
• Perform/assist client in learning airway clearance techniques, particularly when airway
congestion
is a chronic/long-term condition. Numerous techniques may be used, including (but not
limited
to) postural drainage and percussion (CPT), flutter devices, high-frequency chest
compression
with an inflatable vest, intrapulmonary percussive ventilation administered by a
percussinator, and
active cycle breathing (ACB), as indicated. Many of these techniques are the result of
research in
treatments of cystic fibrosis and muscular dystrophy as well as other chronic lung diseases.9
NURSING PRIORITY NO. 3 To assess changes, note complications:
• Auscultate breath sounds, noting changes in air movement to ascertain current status/effects
of treatments to clear airways.
Cultural Collaborative Community/Home Care Diagnostic Studies
Pediatric/Geriatric/Lifespan Medications
ineffective AIRWAY CLEARANCE
• Monitor vital signs, noting blood pressure/pulse changes. Observe for increased respiratory
rate, restlessness/anxiety, and use of accessory muscles for breathing, suggesting advancing
respiratory distress.
• Monitor/document serial chest radiographs, ABGs, pulse oximetry readings. Identifies
baseline status, influences interventions, and monitors progress of condition and/or treatment
response.
• Evaluate changes in sleep pattern, noting insomnia or daytime somnolence. May be
evidence
of nighttime airway incompetence or sleep apnea. (Refer to ND Insomnia.)
• Document response to drug therapy and/or development of adverse reactions or side
effects with antimicrobial agents, steroids, expectorants, bronchodilators. Pharmacological
therapy is used to prevent and control symptoms, reduce severity of exacerbations, and
improve health status. The choice of medications depends on availability of the medication
and the client’s decision making about medication regimen and response to any given
medication.10
• Observe for signs/symptoms of infection (e.g., increased dyspnea, onset of fever, increase
in sputum volume, change in color or character) to identify infectious process/promote timely
intervention.10
• Obtain sputum specimen, preferably before antimicrobial therapy is initiated, to verify
appropriateness of therapy. Note: The presence of purulent sputum during an exacerbation of
symptoms is a sufficient indication for starting antibiotic therapy, but a sputum culture and
antibiogram (antibiotic sensitivity) may be done if the illness is not responding to the initial
antibiotic.10
NURSING PRIORITY NO. 4 To promote wellness (Teaching/Discharge Considerations):
• Assess client’s/caregiver’s knowledge of contributing causes, treatment plan, specific
medications, and therapeutic procedures to determine educational needs.
• Provide information about the necessity of raising and expectorating secretions versus
swallowing them, to note changes in color and amount.
• Identify signs/symptoms to be reported to primary care provider. Prompt evaluation and
intervention is required to prevent/treat infection.
• Demonstrate/assist client/SO in performing specific airway clearance techniques (e.g.,
forced expiratory breathing [also called “huffing”] or respiratory muscle strength training,
chest percussion), if indicated.11
• Review breathing exercises, effective coughing techniques, and use of adjunct devices (e.g.,
IPPB or incentive spirometry) in preoperative teaching to facilitate postoperative recovery,
reduce risk of pneumonia.
• Instruct client/SO/caregiver in use of inhalers and other respiratory drugs. Include expected
effects and information regarding possible side effects and interactions of respiratory drugs
with other medications/OTC/herbals. Discuss symptoms requiring medical follow-up.
Client is often taking multiple medications that have similar side effects and potential for
interactions.
It is important to understand the difference between nuisance side effects (such as fast
heartbeat after albuterol inhaler) and adverse effects (such as chest pain, hallucinations, or
uncontrolled cardiac arrhythmia).9
• Encourage/provide opportunities for rest; limit activities to level of respiratory tolerance.
Prevents/diminishes fatigue associated with underlying condition or efforts to clear
airways.
• Urge reduction/cessation of smoking. Smoking is known to increase production of mucus
and
to paralyze (or cause loss of) cilia needed to move secretions to clear airway and improve
lung
function.10
Nursing Diagnoses in Alphabetical Order 53
ineffective AIRWAY CLEARANCE
54
• Refer to appropriate support groups (e.g., stop-smoking clinic, COPD exercise group,
weight reduction, American Lung Association, Cystic Fibrosis Foundation, Muscular
Dystrophy Association).
• Instruct in use of nocturnal positive pressure airflow for treatment of sleep apnea. (Refer to
NDs Insomnia, Sleep Deprivation.)
DOCUMENTATION FOCUS
Assessment/Reassessment
• Related factors for individual client.
• Breath sounds, presence/character of secretions, use of accessory muscles for breathing.
• Character of cough/sputum.
Planning
• Plan of care and who is involved in planning.
• Teaching plan.
Implementation/Evaluation
• Client’s response to interventions/teaching and actions performed.
• Attainment/progress toward desired outcome(s).
• Modifications to plan of care.
Discharge Planning
• Long-term needs and who is responsible for actions to be taken.
• Specific referrals made.
You might also like
- Meditation BreakthroughDocument26 pagesMeditation Breakthroughanagard2593100% (3)
- Nursing care process in patients with chronic obstructive pulmonary diseaseFrom EverandNursing care process in patients with chronic obstructive pulmonary diseaseNo ratings yet
- Ashton Manual English PDFDocument58 pagesAshton Manual English PDFMalissa Bowen100% (2)
- DEFENDANT Answer With AttachmentsDocument19 pagesDEFENDANT Answer With AttachmentsMariny Del rosarioNo ratings yet
- Pleural Effusion NCPsDocument7 pagesPleural Effusion NCPsJaja Nagallo100% (2)
- Nursing Diagnosis Impaired Gas ExchangeDocument7 pagesNursing Diagnosis Impaired Gas ExchangeZycon Rodney Ae'zecquel Gachallan50% (2)
- Module 2 - Incentive Spirometry (Student)Document4 pagesModule 2 - Incentive Spirometry (Student)febie pacheco0% (1)
- ABCDE Approach PDFDocument3 pagesABCDE Approach PDFJohn SmithNo ratings yet
- The Impact of Sleep Deprivation On AcademicDocument9 pagesThe Impact of Sleep Deprivation On AcademicJayford Mahognay50% (2)
- Pediatric Advanced Life Support (PALS) - UpToDateDocument49 pagesPediatric Advanced Life Support (PALS) - UpToDateANGIE SIDNEY NARANJO GARCIANo ratings yet
- 1) Nursing Careplan For FeverDocument9 pages1) Nursing Careplan For FeverY. Beatrice AbigailNo ratings yet
- Asthma Nursing Care Plan - NCP - Ineffective Airway ClearanceDocument2 pagesAsthma Nursing Care Plan - NCP - Ineffective Airway ClearanceCyrus De Asis92% (24)
- Nursing Care Plan GoiterDocument3 pagesNursing Care Plan Goiterdee_day_8100% (4)
- Assignment ON Chest PhysiotherapyDocument13 pagesAssignment ON Chest PhysiotherapyGayathri R0% (1)
- Breathing Pattern, IneffectiveDocument8 pagesBreathing Pattern, IneffectiveRudhy SaputraNo ratings yet
- Revised NCP (Baiae)Document9 pagesRevised NCP (Baiae)Jennifer BactatNo ratings yet
- Nsg241 Study Guide Exam 5Document76 pagesNsg241 Study Guide Exam 5NatalieAndersonNo ratings yet
- Copd CaseDocument36 pagesCopd Casejho_No ratings yet
- Incentive Spirometry (Revised)Document4 pagesIncentive Spirometry (Revised)Myangel LoiseNo ratings yet
- Pediatric Advanced Life Support (PALS) - 19-8-19Document36 pagesPediatric Advanced Life Support (PALS) - 19-8-19RimaWulandari50% (2)
- Lung Cancer (Nursing Care)Document5 pagesLung Cancer (Nursing Care)heiyuNo ratings yet
- Drug Study and NCP!Document8 pagesDrug Study and NCP!Abegail Abaygar100% (1)
- Nursing Management For Acute Respiratory FailureDocument7 pagesNursing Management For Acute Respiratory FailureEvolynNo ratings yet
- Assignment ON Chest Physiotherapy: Sri Guru Ram Das Nursing Institute Pandher, AmritsarDocument13 pagesAssignment ON Chest Physiotherapy: Sri Guru Ram Das Nursing Institute Pandher, AmritsarPawan BatthNo ratings yet
- Nursing Diagnosis For AsthmaDocument6 pagesNursing Diagnosis For AsthmaTINAIDA33% (3)
- PneumoniaDocument17 pagesPneumoniajustin_saneNo ratings yet
- 1602126330Document65 pages1602126330AnshulAggarwal100% (1)
- Gaba Tryptophan: Amino Acid Solutions For Anxiety, Sugar CravingsDocument13 pagesGaba Tryptophan: Amino Acid Solutions For Anxiety, Sugar CravingsMirela Olarescu100% (1)
- Concept On Surgery: Postoperative CareDocument44 pagesConcept On Surgery: Postoperative CareMelisa ClaireNo ratings yet
- Ncp-Ineffective Breathing PatternDocument4 pagesNcp-Ineffective Breathing PatternRoxanne Ganayo Claver100% (1)
- Nursing Process of PneumoniaDocument5 pagesNursing Process of Pneumoniatin2x061275% (8)
- NCP BaiaeDocument7 pagesNCP BaiaeJonathan Delos ReyesNo ratings yet
- Cardiac ComplicationDocument12 pagesCardiac ComplicationResa ShotsNo ratings yet
- Chest PhysiotherapyDocument13 pagesChest PhysiotherapyAlma Susan100% (1)
- NCP SDocument8 pagesNCP SMarvie CadenaNo ratings yet
- NANDA DefinitionDocument5 pagesNANDA DefinitionAngel_Liboon_388No ratings yet
- Ward Day Pre-WorkDocument10 pagesWard Day Pre-WorkMannyNo ratings yet
- Nursing DiagnosisDocument7 pagesNursing DiagnosisMariya Mikaela Garcia SoledadNo ratings yet
- Chap 26 To 38 Case Study Answers To QuestionsDocument13 pagesChap 26 To 38 Case Study Answers To QuestionsElaine Jean UayanNo ratings yet
- Comprehensive ExaminationDocument8 pagesComprehensive ExaminationAnonymous dquW2YmO7No ratings yet
- NCPDocument17 pagesNCPShayne Jessemae AlmarioNo ratings yet
- So A PieDocument3 pagesSo A PieHelena EliseNo ratings yet
- AssesmentDocument9 pagesAssesmentmizrypNo ratings yet
- Nursing Care PlanDocument3 pagesNursing Care PlanMarielle SorianoNo ratings yet
- NCP - Pulmonary TuberculosisDocument6 pagesNCP - Pulmonary TuberculosisastrijuNo ratings yet
- PneumoniaDocument3 pagesPneumoniaErwin SmithNo ratings yet
- Breathing ExerciseDocument32 pagesBreathing ExerciseEvan Permana Putra100% (1)
- ABCDE Approach PDFDocument3 pagesABCDE Approach PDFIrsan apatisNo ratings yet
- Pulmonary System 3Document39 pagesPulmonary System 3baraa.2352001No ratings yet
- Funda Lab Mod 5-7Document13 pagesFunda Lab Mod 5-7Liane BartolomeNo ratings yet
- BHTDocument18 pagesBHTNitesh KumawatNo ratings yet
- During ICU StayDocument3 pagesDuring ICU StayKaloy KamaoNo ratings yet
- Neck DissectionDocument24 pagesNeck Dissectionhayat al akoumNo ratings yet
- Nursing Care Plan For Master Shyne With AllDocument17 pagesNursing Care Plan For Master Shyne With AllsreekalaNo ratings yet
- Chest Physiotherapy With Sputum CollectionDocument41 pagesChest Physiotherapy With Sputum CollectionEduardNo ratings yet
- Below Are 8 Pneumonia Nursing Care Plans (NCP)Document16 pagesBelow Are 8 Pneumonia Nursing Care Plans (NCP)Diana CarinoNo ratings yet
- Tugas Pola Nafas Tidak AktifDocument19 pagesTugas Pola Nafas Tidak Aktiffemy lia utamiNo ratings yet
- Breathing BOP I AssignmentDocument23 pagesBreathing BOP I AssignmentSonia guptaNo ratings yet
- Tuberculosis Bacteria.: Risk For InfectionDocument5 pagesTuberculosis Bacteria.: Risk For InfectionLag Lag AlbercaNo ratings yet
- Preoperative ReportDocument33 pagesPreoperative ReportJay VillasotoNo ratings yet
- Bronchial Asthma in Children FdneDocument36 pagesBronchial Asthma in Children FdneRonit ChandNo ratings yet
- Essential Parameters of Airway Evaluation Lecture 6Document27 pagesEssential Parameters of Airway Evaluation Lecture 69yqgmkvyzdNo ratings yet
- Plan of Care For Ineffective Air Way 1Document6 pagesPlan of Care For Ineffective Air Way 1LisaNo ratings yet
- What Is COPD? Chronic Obstructive Pulmonary Disease (COPD) : Signs and SymptomsDocument11 pagesWhat Is COPD? Chronic Obstructive Pulmonary Disease (COPD) : Signs and SymptomsCecil Bhang-i Cacay - PabloNo ratings yet
- Barnes 2019Document7 pagesBarnes 2019José VitorNo ratings yet
- Adelax: Only For The Use of Medical ProfessionalsDocument2 pagesAdelax: Only For The Use of Medical Professionalsparthibanemails5779No ratings yet
- Speech Hobby 2Document30 pagesSpeech Hobby 2Hubert WieczorekNo ratings yet
- Hotel and Travel EnglishDocument121 pagesHotel and Travel EnglishviniciusmdiasNo ratings yet
- Assessment of Nidra As Adharaniya Vega & Its Management With Bhramari PranayamDocument15 pagesAssessment of Nidra As Adharaniya Vega & Its Management With Bhramari PranayamDr Kirti BhatiNo ratings yet
- Task 1. Grammar /12x1 12 Points/ Read The Sentences Below and Choose The Best Answer To Complete Each SentenceDocument6 pagesTask 1. Grammar /12x1 12 Points/ Read The Sentences Below and Choose The Best Answer To Complete Each SentenceUndral UndralNo ratings yet
- ch45 NCP Sleep 1180-1181Document2 pagesch45 NCP Sleep 1180-1181missy23papNo ratings yet
- SH Ankh Push PiDocument10 pagesSH Ankh Push PiRavindra ChobariNo ratings yet
- Sleep: 5 Reasons You Aren'T Sleeping WellDocument4 pagesSleep: 5 Reasons You Aren'T Sleeping WellJen GülerNo ratings yet
- Neurological Disorders With Sleep Alterations: Cristina Panea, MD, PHD Elias Emergency University Hospital BucharestDocument20 pagesNeurological Disorders With Sleep Alterations: Cristina Panea, MD, PHD Elias Emergency University Hospital BucharestGrig GrigNo ratings yet
- Morgan Fisher - Sleep Deprivation Research-3Document11 pagesMorgan Fisher - Sleep Deprivation Research-3api-609519589No ratings yet
- Basic Concepts of Psychiatric Mental Health Nursing 8Th Edition Shives Test Bank Full Chapter PDFDocument29 pagesBasic Concepts of Psychiatric Mental Health Nursing 8Th Edition Shives Test Bank Full Chapter PDFTaylorHarveyawde100% (14)
- Bab Vii Daftar PustakaDocument5 pagesBab Vii Daftar Pustaka19 110 Setya Maharani KadirNo ratings yet
- Insomnia and Depression: Original ArticleDocument7 pagesInsomnia and Depression: Original ArticleFlorina AnichitoaeNo ratings yet
- Environics Paper On Geopathic StresDocument5 pagesEnvironics Paper On Geopathic StresramachariNo ratings yet
- Hortatory ExpositionDocument3 pagesHortatory ExpositionRahardian OkaNo ratings yet
- Circadian Rhythm Sleep Disorders CRSDDocument11 pagesCircadian Rhythm Sleep Disorders CRSDjaime manciaNo ratings yet
- Angenta InsDocument1 pageAngenta InsmksNo ratings yet
- Academic Procrastination and Sleep Impairment of Senior High School Students ManuscriptDocument91 pagesAcademic Procrastination and Sleep Impairment of Senior High School Students ManuscriptDeity Ann ReuterezNo ratings yet
- Prevention and Treatment of Systemic Glucocorticoid Side EffectsDocument10 pagesPrevention and Treatment of Systemic Glucocorticoid Side EffectsMahmoud DiaaNo ratings yet
- Privação Do SonoDocument3 pagesPrivação Do SonoHugo BarbosaNo ratings yet
- Test Bank For Stress Management For Life A Research Based Experiential Approach 5th Edition Michael Olpin Margie HessonDocument36 pagesTest Bank For Stress Management For Life A Research Based Experiential Approach 5th Edition Michael Olpin Margie Hessonjocosevannerh98oj100% (41)
- Paraphrasing N SummarisingDocument5 pagesParaphrasing N SummarisingAnas SheikhNo ratings yet
- Module 16 - Pharmacotherapy For Psychiatric DisordersDocument157 pagesModule 16 - Pharmacotherapy For Psychiatric Disordersgeekay79No ratings yet