Professional Documents
Culture Documents
3.unusual Spontaneous Nasal Septal Abscess PDF
Uploaded by
rahmat aidil fitrahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
3.unusual Spontaneous Nasal Septal Abscess PDF
Uploaded by
rahmat aidil fitrahCopyright:
Available Formats
Journal of Case Reports and Studies
Volume 3 | Issue 3
ISSN: 2348-9820
Case Report Open Access
Unusual Spontaneous Nasal Septal Abscess
Adnane C*, Adouly T, Taali L, Belfaquir L, Rouadi S, Abada R, Roubal M and Mahtar M
Department of ENT; 20 Août hospital. Ibn Rochd University Hospital, Casablanca, Morocco
Corresponding author: Adnane C, Department of ENT, 20 Aout hospital, Ibn Rochd University Hospital,
*
Casablanca, Morocco, E-mail: adnanechoaib@gmail.com
Citation: Adnane C, Adouly T, Taali L, Belfaquir L, Rouadi S, et al. (2015) Unusual Spontaneous Nasal Septal
Abscess. J Case Rep Stud 3(3): 302
Abstract
A nasal septal abscess (NSA) is defined as a collection of pus between the cartilage or bony septum and the mucoperichondrium or
mucoperiostium. It’s an uncommon disease that in the absence of early diagnosis and proper management may lead to lethal complications
and cosmetic deformity. The most common presentation of the nasal septal abscess is nasal obstruction and pain. We present a healthy
patient with idiopathic spontaneous nasal septal abscess who complained of acute complete nasal obstruction and nasal pain.
Keywords: Nasal Septum; Abscess; Emergencies; Nasal deformation
Introduction
The nasal septum is an essential structure maintaining the external shape and function of the nose [1-3]. Nasal septal abscess (NSA)
is defined as a collection of pus between the cartilaginous or bony nasal septum and the mucoperichondrium or mucoperiosteum
[3]. It’s an uncommon condition that most commonly develops in a pre-existing septal hematoma with usually a history of nasal
trauma [4]. NSA is also less frequently associated with nasal furunculosis, sinusitis, influenza, dental infection, and after nasal
septal surgery [3,5-7]. The cerebral spread of infection from NSA could be a lethal complication. Other complications include
saddle nose deformity, septal perforation, and permanent nasal obstruction [3,5,8]. For this reason, early diagnosis and proper
management are necessary to prevent the potentially dangerous complications and the development of severe functional and
structural deformities in the future [5]. This case report presents an uncommon case of spontaneous NSA in an immunocompetent
patient, to alert physicians to be more vigilant about this uncommon disease.
Case report
A 35-year-old male presented to our emergency department with symptoms of nasal and facial pain, and nasal obstruction, which
he had experienced for five days. There was no prior history of nasal surgery, trauma, sinusitis, epistaxis, or dental procedures.
No medical history or immunocompromised states were noted. Physical examination revealed swollen and tender nasal dorsum.
Anterior rhinoscopy found bilateral purple septal swelling with total obliteration of the nasal airway (Figure 1). The nasal septal
swelling did not change in size when topical nasal decongestant was applied. The diagnosis of nasal septal abscess was confirmed
by needle aspiration of pus. The sample was sent for culture and sensitivity testing. The rest of the examination was unremarkable.
Urgent post-contrast computed tomography (CT) scan revealed a 3 cm×1 cm×1.9 cm hypodense bilateral collections at the
anterior nasal septum (Figure 2). Dental examination could not identify any infection. Emergency transnasal drainage of the
abscess under general anesthesia was performed with bilateral septal incision and drainage. A gauze drain was placed in the
abscess cavity and the nasal cavities were packed during 48 hours. Bacteriological culture found a Staphylococcus aureus that was
sensitive to Amoxicillin/clavulanic acid. Patient was treated with Amoxicillin/clavulanic acid , decongestants, anti-inflammatory
and analgesics for 2 weeks. Follow up at 2 weeks and one month showed intact nasal septum without any defects and complete
resolution of the abscess. The abscess had nearly disappeared on CT scan. At 6 months later, there was no nasal deformity.
Discussion
The incidence of nasal septal abscess is rare; major centers reported fewer than 10 cases per year [3,9]. This entity was first reported
in 1810 by Arnal [10]. Ambus et al reported 16 cases occurring over 10 years at the Massachusetts eye and ear infirmary [3]. Canty
and Berkowitz reported 20 cases of nasal septal abscess in a period of 18 months [8]. Naik reported 20 cases over 54 months [11].
NSA most frequently develops in a pre-existing septal hematoma with usually a history of nasal trauma [3,4,12]. It is usually seen
in younger patients and less frequently associated with nasal furunculosis, sinusitis, influenza, dental infection, and after nasal
septal surgery [3,5-7]. A spontaneous idiopathic NSA is far less common. In the literature, there are very few cases of idiopathic
nasal septal abscesses reported previously. According to Chung et al, there are only three idiopathic nasal septal abscesses reported
previously [13,14]. Most of the abscess cavity situated at the anterior cartilaginous nasal septum, posterior localization may be
missed if only anterior rhinoscopy is performed [15].
Annex Publishers | www.annexpublishers.com Volume 3 | Issue 3
Journal of Case Reports and Studies 2
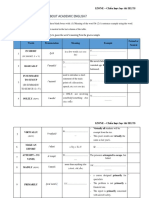
Figure 1: Bilateral purple bulging of the nasal septum
Figure 2: Computer tomographic scan: (A) Axial computed tomography image showing swelling of the nasal septum with hypodense fluid
collection (B) Coronal cut showing showing septal abscess
The most common presentation of the NSA is nasal obstruction and pain [10]. In contrast, septal hematoma usually presents as
painless nasal obstruction after injury. Other signs and symptoms include headache, fever, saddle nose, and swelling of the nasal
septum [3]. On anterior rhinoscopy, this uncommon disease is often mistaken as nasal septal deviation or inferior turbinate
hypertrophy by less experienced physicians [10,15]. Therefore, cautious palpation with fine-needle aspiration as need as possible
may be helpful for diagnosis. CT scan with contrast enhancement is very helpful for the diagnosis, the involved area and cartilage
status.
The accumulation of pus between the cartilage and perichondrium will lead to ischemia and necrosis of the cartilage; this may
result in septal cartilage destruction, saddle nose deformity, functional dysfunction and cosmetic problems [16]. In children in
particular, these consequences may be affect the normal development of the nose and maxilla [16,17]. Life-threatening intracranial
complications; such as brain abscess, meningitis and cavernous sinus thrombosis; especially in the immunocompromised patients
may progress rapidly if the NSA remains untreated [10,13,15,18].
Emergency surgical drainage of nasal septal abscess and intravenous antibiotic administration is required. The abscess can be
drained by a horizontal incision from behind forwards across the swollen area, as low as possible in the septum [4]. Bilateral
drainage is only necessary if the abscess is bilateral with an intact septal cartilage, so that cartilage still exists between the collections
of purulent material on both sides. It is sometimes advantageous to remove a piece of mucoperichondrium to facilitate drainage
[19]. Some authors prefer to use a vertical or L-shaped incision in the mucoperichondrium [20]. A wick is placed in the incision,
and the mucoperichondrium is replaced against the cartilage by supportive intranasal packing [21].
The most common etiological agent is Staphylococcus aureus [22], others less frequently include Streptococcus pneumoniae,
group A beta hemolytic Streptococcus, anaerobes, Hemophilus influenzae [3,23]. Opportunistic fungal agents have been reported
in HIV patients resulting in a high mortality [10,24]. Empirical antibiotic treatment must be started immediately once diagnosis
is made before the organism is isolated.
Annex Publishers | www.annexpublishers.com Volume 3 | Issue 3
3 Journal of Case Reports and Studies
In case of nasal deformity after septal destruction, reconstruction of the nasal septum may be performed immediately after drainage
of the abscess as a primary treatment, or secondary treatment after resolution of the infection [16,18]. Reconstruction of the septal
cartilage may be used by residual septal cartilage or autologous cartilage grafts from tragus, auricle or rib [16,17].
Conclusion
Nasal septal abscess is an uncommon rhinological emergency disease. Because of its non specific symptoms, careful examination
with detailed history is essential especially in the non-traumatic context. Early management would prevent nasal deformity and
intracranial complications.
References
1. Grymer LF, Bosch C (1997) The nasal septum and the development of the midface. A longitudinal study of a pair of monozygotic twins. Rhinology 35: 6-10.
2. Nolst Trenité GJ, Verwoerd CD, Verwoerd-Verhoef HL (1988) Reimplantation of autologous septal cartilage in the growing nasal septum. II. The influence of
reimplantation of rotated or crushed autologous septal cartilage on nasal growth: an experimental study in growing rabbits. Rhinology 26: 25-32.
3. Ambrus PS, Eavey RD, Baker AS, Wilson WR, Kelly JH (1981) Management of nasal septal abscess. Laryngoscope 91(4): 575-82.
4. Fearon B, Mckendry Jb, Parker J (1961) Abscess of the nasal septum in children. A case history of meningitis secondary to a septal abscess. Arch Otolaryngol
74: 408-12.
5. Matsuba HM, Thawley SE (1986) Nasal septal abscess: unusual causes, complications, treatment, and sequelae. Ann Plast Surg 16: 161-6.
6. Pang KP, Sethi DS (2002) Nasal septal abscess: an unusual complication of acute spheno-ethmoiditis. J Laryngol Otol 116: 543-5.
7. da Silva M, Helman J, Eliachar I, Joachims HZ (1982) Nasal septal abscess of dental origin. Arch Otolaryngol 108: 380-1.
8. Canty PA, Berkowitz RG (1996) Hematoma and abscess of the nasal septum in children. Arch Otolaryngol Head Neck Surg 122: 1373-6.
9. Eavey RD, Malekzakeh M, Wright HT (1977) Bacterial meningitis secondary to abscess of the nasal septum. Pediatrics 60: 102-4.
10. Shah SB, Murr AH, Lee KC (2000) Nontraumatic Nasal Septal Abscesses in the Immunocompromised: Aetiology, Recognition, Treatment and Sequelae. Am J
Rhinol 14: 39-43.
11. Naik SM, Naik SS (2010) Nasal Septal Abscess: A Retrospective Study of 20 Cases in KVG Medical College and Hospital, Sullia. Clin Rhinol: An Int J 3: 135-40.
12. Beck AL (1945) Abscess of the nasal septum complicating acute ethmoiditis. Arch Otolaryngol 42: 275-9.
13. Salam B, Camilleri A (2009) Non-Traumatic Nasal Septal Abscess in an Immunocompetent Patient. Rhinology 47: 476-7.
14. Chung J C-k, Wong A T-K, Ho W-k (2013) Spontaneous Nasal Septal Abscess Presenting as Complete Nasal Obstruction. Int J Otolaryngol Head Neck Surg 2:
79-81.
15. George A, Smith WK, Kumar S, Pfleiderer AG (2008) Posterior Nasal Septal Abscess in a Healthy Adult Patient. J Laryngol Otol 122: 1386-8.
16. Dispenza C, Saraniti C, Dispenza F, Caramanna C, Salzano FA (2004) Management of Nasal Septal Abscess in Childhood: Our Experience. Int J Pediatr Otorhi-
nolaryngol 68: 1417-21.
17. Menger DJ, Tabink IC, Trenite GJ (2008) Nasal Septal Abscess in Children: Reconstruction with Autologous Cartilage Grafts on Polydioxanone Plate. Arch
Otolaryngol Head Neck Surg 134: 842-7.
18. Cho JG, Lim HW, Zodpe P, Kang HJ, Lee HM (2006) Nasal Septal Abscess: An Unusual Presentation of Dentigerous Cyst. Eur Arch Otorhinolaryngol 263:
1048-50.
19. Thomson STC (1955) Diseases of the septum, in Diseases of the Nose and Throat: a Textbook for Students and Practitioners, (6th rev edn) Negus VE, Bateman
GH (eds), Cassell, London.
20. Simon RR, Brenner BE (2002) Emergency Procedures and Techniques (4th ed). Philadelphia, United States.
21. Fry HJ (1969) The pathology and treatment of haematoma of the nasal septum. Br J Plast Surg 22: 331-5.
22. Jalaludin MA (1993) Nasal Septal Abscess--Retrospective Analysis of 14 Cases from University Hospital, Kuala Lumpur. Singapore Medical Journal 34: 435-7.
23. Huang PH, Chiang YC, Yang TH, Chao PZ, Lee FP (2006) Nasal Septal Abscess. Otolaryngol Head Neck Surg 135: 335-6.
24. Walker R, Gardner L, Sindwani R (2007) Fungal Nasal Septal Abscess in the Immunocompromised Patient. Otolaryngol Head Neck Surg 136: 506-7.
Submit your manuscript to Annex Publishers and
benefit from:
→ Convenient online submission
→ Rigorous peer review
→ Immediate publication on acceptance
→ Open access: articles freely available online
→ High visibility within the field
→ Better discount for your subsequent articles
Submit your manuscript at
http://www.annexpublishers.com/paper-submission.php
Annex Publishers | www.annexpublishers.com Volume 3 | Issue 3
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Japan's Statistic Bureau of Japan 2021Document95 pagesJapan's Statistic Bureau of Japan 2021Ren SuzakuNo ratings yet
- Wa0094.Document9 pagesWa0094.lider vigilanciaNo ratings yet
- Synopsis - Anu Varghese and Dr. M H Salim, 2015 - Handloom Industry in Kerala A Study of The Problems and ChallengesDocument8 pagesSynopsis - Anu Varghese and Dr. M H Salim, 2015 - Handloom Industry in Kerala A Study of The Problems and ChallengesNandhini IshvariyaNo ratings yet
- O IntegratedscienceDocument36 pagesO IntegratedscienceFarai FaustosNo ratings yet
- First Aid 10Document16 pagesFirst Aid 10Oswaldo TorresNo ratings yet
- IOT Based Health Monitoring SystemDocument3 pagesIOT Based Health Monitoring SystemInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Altius Annual Leave Policy Wef 1st January 2012 Ver 1.1Document11 pagesAltius Annual Leave Policy Wef 1st January 2012 Ver 1.1Mudassar HakimNo ratings yet
- Understanding Desistance From Crime Laub and SampsonDocument70 pagesUnderstanding Desistance From Crime Laub and Sampsonchrisgoss1No ratings yet
- Play Therapy FinalDocument8 pagesPlay Therapy FinalChandru KowsalyaNo ratings yet
- Congestive Heart Failure Pathophysiology Schematic DiagramDocument3 pagesCongestive Heart Failure Pathophysiology Schematic DiagramJasleen KaurNo ratings yet
- SBMWSM2016Document491 pagesSBMWSM2016maimaiyeuem123100% (1)
- EffectiveTeaching Full ManualDocument340 pagesEffectiveTeaching Full ManualHabtamu AdimasuNo ratings yet
- CSEC Biology June 2012 P2Document17 pagesCSEC Biology June 2012 P2Joy BoehmerNo ratings yet
- Tsoukaki 2012Document8 pagesTsoukaki 2012Marina JoelNo ratings yet
- Below The Breadline: The Relentless Rise of Food Poverty in BritainDocument28 pagesBelow The Breadline: The Relentless Rise of Food Poverty in BritainOxfamNo ratings yet
- Ewald Hecker's Description of Cyclothymia As A Cyclical Mood Disorder - Its Relevance To The Modern Concept of Bipolar IIDocument7 pagesEwald Hecker's Description of Cyclothymia As A Cyclical Mood Disorder - Its Relevance To The Modern Concept of Bipolar IItyboyoNo ratings yet
- Effect of A Physiotherapy Program in Women With Primary DysmenorrheaDocument6 pagesEffect of A Physiotherapy Program in Women With Primary DysmenorrheaPaula RangelNo ratings yet
- Material Safety Data Sheet: Liquefied Petroleum GasDocument1 pageMaterial Safety Data Sheet: Liquefied Petroleum GasardhanhendroNo ratings yet
- Mobile Health Clinic InitiativeDocument47 pagesMobile Health Clinic InitiativededdyNo ratings yet
- Urinary Tract InfectionDocument10 pagesUrinary Tract Infectionjaah diazNo ratings yet
- 2018 Tooth Sectioning For Coronectomy How To Perform?Document9 pages2018 Tooth Sectioning For Coronectomy How To Perform?kaarlaamendezNo ratings yet
- Statistical EstimationDocument37 pagesStatistical EstimationAmanuel MaruNo ratings yet
- Cbse Term 1 Final Exam Instructions 2021-21Document9 pagesCbse Term 1 Final Exam Instructions 2021-21Eshaan123thebestNo ratings yet
- SAFed Tests PDFDocument88 pagesSAFed Tests PDFDanNo ratings yet
- 978 3 642 25446 8Document166 pages978 3 642 25446 8Gv IIITNo ratings yet
- Bar Coding Near MissDocument8 pagesBar Coding Near Missenorth1234No ratings yet
- IZONE Academic WordlistDocument59 pagesIZONE Academic WordlistTrung KiênNo ratings yet
- 1 s2.0 S2667368123000116 MainDocument24 pages1 s2.0 S2667368123000116 MainCelia MartinezNo ratings yet
- Topic 5 DQ 2.Document3 pagesTopic 5 DQ 2.Emmanuel OpiyoNo ratings yet
- HypnotherapyDocument16 pagesHypnotherapyAnonymous lsnDTjvNo ratings yet