Professional Documents
Culture Documents
Anak Bangsal
Uploaded by
Regina AyediaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anak Bangsal
Uploaded by
Regina AyediaCopyright:
Available Formats
Prune Belly syndrome: A rare case report
Sunil Kumar Samal and Setu Rathod
Abstract
Prune Belly syndrome (PBS) is a rare congenital anomaly of uncertain etiology almost exclusive to males. We report a case of
term male baby born to a 39-year-old grand multipara with previous four normal vaginal births. There was no history of
genetic or congenital anomaly in her family. Examination of the baby revealed hypotonia, deficient abdominal muscle,
cryptorchidism, palpable kidney, and bladder. Ultrasound examination of the abdomen revealed bilateral gross hydronephrosis
and megaureter. Provisional diagnosis of PBS was made and the baby was admitted in neonatal intensive care units for further
management. Routine antenatal care with ultrasonography will help in detecting renal anomalies, which can be followed
postnatally. Early diagnosis of this syndrome and determining its optimal treatment are very important in helping to avoid its
fatal course.
Keywords: Cryptorchidism, hydroneprosis, megaureter, Prune Belly syndrome
INTRODUCTION
Prune Belly syndrome (PBS) is a rare congenital disorder affecting about 1 in 30,000 births[1] of which about 96% of those
affected are male.[2] It is characterized by deficient development of abdominal muscles that causes the skin of the abdomen to
wrinkle like a prune, bilateral cryptorchidism, abnormalities of the urinary tract such as bilateral gross hydronephrosis,
megaureter and megacystitis.[2] The exact etiology of PBS is not known; however, some of the studies reveal the possibility
of genetic inheritance and possible association with trisomy 18 and 21.[2,3] The prognosis of babies with PBS is poor with
stillbirths and early infant deaths being common. We report a case of male baby with PBS because of its rarity and term birth.
CASE REPORT
A 39 years old unbooked G5P4L4A0 at 39 weeks 5 days of gestation was admitted to our labor room complaining of labor
pain. She had four previous normal vaginal deliveries. There was no history of prior antenatal care and she belonged to a tribal
community with lower socioeconomic status. There was history of consanguineous marriage with her husband who was 42
years old and a daily laborer. There was no history of drug intake, radiation exposure or fever with rashes in this pregnancy.
Neither was she a known case of diabetes nor was there any history of genetic or congenital anomaly in her family.
On examination, she was in the second stage of labor in cephalic presentation and regular fetal heart rate with fully dilated and
taken up cervix. She delivered a term 2700 g female baby and the Apgar score was 7 and 9 at 1 and 5 min. Physical
examination of the infant showed hypotonia. Abdominal examination revealed a distended abdomen with thin wrinkled skin
and visible peristalsis [Figure 1] with palpable kidneys and bladder. Scrotal skin showed little rugae and no testes in the sac.
Other systemic examination revealed no abnormality. Ultrasonography of the abdomen showed bilateral gross hydronephrosis
with megaureter. The baby was referred to pediatric surgery department of higher center for further management.
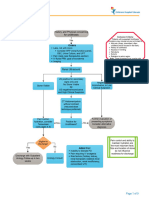
Figure 1
Prune Belly syndrome: Distended abdomen, thin wrinkled skin with visible peristalsis
DISCUSSION
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4367054/ 27/01/19 10.02
Halaman 1 dari 4
Although PBS (also known as Eagle-Barrett syndrome) is characterized by the classical triad of urinary tract anomalies,
deficient abdominal musculature, and bilateral cryptorchidism, association with other anomalies including musculoskeletal,
cardiovascular, pulmonary and genital malformations have been reported in the literature.[2] The etiology of PBS is unclear
and possible familial genetic inheritance was reported in some of the studies.[3] Haeri et al. in 2010[4] have reported the
association of PBS with an apparently de novo 1.3 megabase interstitial 17q12 microdeletion that includes the hepatocyte
nuclear factor-1-beta gene at 17q12, and the authors suggested that haploinsufficiency of hepatocyte nuclear factor-1-beta may
be causally related to the production of the PBS phenotype through a mechanism of prostatic and ureteral hypoplasia that
results in severe obstructive uropathy with urinary tract and abdominal distension. History of consanguinity and the mother
being elderly gravida indicate the hereditary etiology in our case. The massive bladder distension and urinary ascites due to
severe obstructive uropathy leads to degeneration of the abdominal wall musculature and failure of testicular descent. The
impaired elimination of urine from the bladder leads to oligohydramnios and pulmonary hypoplasia.[2]
Although the primary molecular defect underlying PBS remains unclear, clinical studies have given rise to two main
pathogenic hypotheses; these are the mesodermal defect hypothesis and the urethral obstruction malformation complex
hypothesis. According to mesodermal defect hypothesis[5] aberrant development of the derivatives of the first lumbar
myotome between 6 and 10 weeks of gestation leads to a patchy muscular deficiency or hypoplasia of the abdominal wall as
well as to urinary tract abnormalities. The urethral obstruction malformation complex hypothesis[6] proposes that pressure
atrophy of the abdominal wall muscles occurs when urethral obstruction leads to massive distension of the bladder and
ureters. Bladder distension would also interfere with descent of the testes and thus be responsible for the bilateral
cryptorchidism. PBS is rare in females, with fewer than 30 cases reported in the literature.[7] More complex morphogenesis of
the male urethra may be the possible cause of obstructive anomalies at several levels indicating the higher incidence of this
syndrome in males. After clinical examination, ultrasonography of abdomen, plain X-ray, intravenous pyelography and
micturating cystourethrography can confirm the diagnosis.
Our patient comes under category 2 PBS as described by Woodard in 1985 [Table 1].[8] Management requires proper co-
ordination among neonatology, nephrology, urology and other departments. Further management options include voiding
cystourethrography with antibiotic cover in suspected cases of renal insufficiency or bladder outlet obstruction (BOO),
suprapubic catheter in BOO to prevent urinary tract infections (UTI), orchidopexy and chest X-ray to rule out pneumothorax,
pulmonary hypoplasia and pneumomediastinum. In category 2 patients with renal insufficiency; reduction cystoplasy, ureteric
shortening tapering and reimplantation with or without abdominoplasty (Monfort technique) may be performed. Careful
surveillance with intervention for repeated febrile UTI or renal deterioration is also recommended.
Table 1
Classification of PBS (Woodard 1985)
The prognosis of PBS is usually poor as many infants are either stillborn or die within the first few weeks of life due to
pulmonary hypoplasia or renal failure or a combination of congenital anomalies. Chronic failure is the most common
complication and found in 25-30% of cases.[2] Diao et al. have reported renal failure to be the main cause of death in PBS.[9]
Serum creatinine levels is a useful predictor of long term renal function and levels less than 60 µmol/l indicate good
prognosis. Although the condition is usually incompatible with life due to visceral abnormalities especially that of renal
function, there are cases who survived into adult life after urinary tract repair and abdominal reconstruction surgery.[10] When
diagnosed in the antenatal period by ultrasonography intrauterine therapeutic option including in utero placement of a
vesicouterine shunt can be done to prevent the development of PBS, as reported by Leeners et al.[11]
CONCLUSION
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4367054/ 27/01/19 10.02
Halaman 2 dari 4
PBS is a rare congenital anomaly which has no known prevention other than the routine use of screening for fetal anomalies.
Routine antenatal care with ultrasonography will help in detecting renal anomalies early and optimal treatment thereafter can
avoid fatal course of PBS.
ACKNOWLEDGMENT
We thank the Department of OBGYN, SCB Medical College, Cuttack for their valuable support and co-operation of patients
and their families admitted to the hospital.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
Article information
J Nat Sci Biol Med. 2015 Jan-Jun; 6(1): 255–257.
doi: 10.4103/0976-9668.149218
PMCID: PMC4367054
PMID: 25810678
Sunil Kumar Samal and Setu Rathod
Department of Obstetrics and Gynaecology, Mahatma Gandhi Medical College and Research Institute, Puducherry, India
Address for correspondence: Dr. Sunil Kumar Samal, T-D, Type II Staff Quarters, Mahatma Gandhi Medical College and Research Institute,
Pillaiyarkuppam, Puducherry - 607 402, India. E-mail: drsksamal1981@gmail.com
Copyright : © Journal of Natural Science, Biology and Medicine
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits
unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article has been cited by other articles in PMC.
Articles from Journal of Natural Science, Biology, and Medicine are provided here courtesy of Wolters Kluwer -- Medknow Publications
REFERENCES
1. Baird PA, MacDonald EC. An epidemiologic study of congenital malformations of the anterior abdominal wall in more than half a
million consecutive live births. Am J Hum Genet. 1981;33:470–8. [PMC free article] [PubMed]
2. Tagore KR, Ramineni AK, Vijaya Lakshmi AR, Bhavani N. Prune Belly syndrome. Case Rep Pediatr. 2011:1–3.
3. Ramasamy R, Haviland M, Woodard JR, Barone JG. Patterns of inheritance in familial Prune Belly syndrome. Urology. 2005;65:1227.
[PubMed]
4. Haeri S, Devers PL, Kaiser-Rogers KA, Moylan VJ, Jr, Torchia BS, Horton AL, et al. Deletion of hepatocyte nuclear factor-1-beta in an
infant with Prune Belly syndrome. Am J Perinatol. 2010;27:559–63. [PubMed]
5. Moore KL. Clinically Oriented Embryology. Philadelphia, USA: W. B. Saunders Company; 1988. The Developing Human.
6. Greskovich FJ, 3rd, Nyberg LM., Jr The Prune Belly syndrome: A review of its etiology, defects, treatment and prognosis. J Urol.
1988;140:707–12. [PubMed]
7. Reinberg Y, Shapiro E, Manivel JC, Manley CB, Pettinato G, Gonzalez R. Prune Belly syndrome in females: A triad of abdominal
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4367054/ 27/01/19 10.02
Halaman 3 dari 4
musculature deficiency and anomalies of the urinary and genital systems. J Pediatr. 1991;118:395–8. [PubMed]
8. Woodard JR. Prune Belly syndrome. In: King LR, Kelalis PP, Belman AB, editors. Clinical Pediatric Urology. Philadelphia: WB
Saunders; 1985. pp. 805–24.
9. Diao B, Diallo Y, Fall PA, Ngom G, Fall B, Ndoye AK, et al. Prune Belly syndrome: Epidemiologic, clinic and therapeutic aspects. Prog
Urol. 2008;18:470–4. [PubMed]
10. Woodhouse CR. Prospects for fertility in patients born with genitourinary anomalies. J Urol. 2001;165:2354–60. [PubMed]
11. Leeners B, Sauer I, Schefels J, Cotarelo CL, Funk A. Prune-Belly syndrome: Therapeutic options including in utero placement of a
vesicoamniotic shunt. J Clin Ultrasound. 2000;28:500–7. [PubMed]
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4367054/ 27/01/19 10.02
Halaman 4 dari 4
You might also like
- Update On The Prenatal Diagnosis and Outcomes of Fetal Bilateral Renal AgenesisDocument5 pagesUpdate On The Prenatal Diagnosis and Outcomes of Fetal Bilateral Renal AgenesisShynta AmeliaNo ratings yet
- Renal NursingDocument17 pagesRenal Nursingrlinao100% (3)
- ARPCKD Bombay J 2012Document4 pagesARPCKD Bombay J 2012micamica451No ratings yet
- Pseudo Prune Belly Syndrome in FemaleDocument6 pagesPseudo Prune Belly Syndrome in Femalereza kurniawanNo ratings yet
- Gastro SCH Is IsDocument13 pagesGastro SCH Is IsferoNo ratings yet
- 2022ClinPerinatology Mowrer AbdominalWallDefect AReviewDocument11 pages2022ClinPerinatology Mowrer AbdominalWallDefect AReviewdarkangelmx1No ratings yet
- Idiopathic Sclerosing Encapsulating Peritonitis: Abdominal CocoonDocument6 pagesIdiopathic Sclerosing Encapsulating Peritonitis: Abdominal CocoonRameshKumarNo ratings yet
- S - Cervical Ectopic PregnancyDocument8 pagesS - Cervical Ectopic PregnancyCitra Wahyu Tri UtamiNo ratings yet
- Neonatal Necrotizing Enterocolitis: Clinical Challenges, Pathophysiology and ManagementDocument10 pagesNeonatal Necrotizing Enterocolitis: Clinical Challenges, Pathophysiology and ManagementFahmi SyarifNo ratings yet
- Neonatal ObstructionDocument27 pagesNeonatal ObstructionJoão Vitor MizaelNo ratings yet
- Review of Necrotizing Enterocolitis and Spontaneous Intestinal PerforationDocument10 pagesReview of Necrotizing Enterocolitis and Spontaneous Intestinal PerforationDraalexNo ratings yet
- 44 Danfulani EtalDocument3 pages44 Danfulani EtaleditorijmrhsNo ratings yet
- Neonatal Bowel Obstruction: David Juang,, Charles L. SnyderDocument27 pagesNeonatal Bowel Obstruction: David Juang,, Charles L. SnyderNaty BmNo ratings yet
- Child JournalDocument8 pagesChild JournalVijayakanth VijayakumarNo ratings yet
- Case 16737: Duodenal Atresia in A Fetus With Trisomy 21Document5 pagesCase 16737: Duodenal Atresia in A Fetus With Trisomy 21NasriNo ratings yet
- A Holistic Approach To CAKUT (Congenital Anomalies of The Kidney and Urinary Tract)Document3 pagesA Holistic Approach To CAKUT (Congenital Anomalies of The Kidney and Urinary Tract)Kusuma IntanNo ratings yet
- Advances in Prenatal and Perinatal Diagnosis and Management of GastroschisisDocument36 pagesAdvances in Prenatal and Perinatal Diagnosis and Management of GastroschisisLondonNo ratings yet
- Kayatsha - Gastroschisis and Omphalocele A Case ReportDocument4 pagesKayatsha - Gastroschisis and Omphalocele A Case ReportAffannul HakimNo ratings yet
- Prune Belly SyndromeDocument39 pagesPrune Belly SyndromeHudaNo ratings yet
- Unusual Cause of Neonatal Intestinal Obstruction: Zikavska T Brucknerova I Cervenova O Vidiscak M Hustavova LDocument4 pagesUnusual Cause of Neonatal Intestinal Obstruction: Zikavska T Brucknerova I Cervenova O Vidiscak M Hustavova LanillodepeneNo ratings yet
- Gastroschisis: Case ReportDocument2 pagesGastroschisis: Case ReportMuhammad Syamil RozlanNo ratings yet
- Lec 1Document52 pagesLec 1zainabd1964No ratings yet
- Ecgds 09 00916Document4 pagesEcgds 09 00916Houda El MoufidNo ratings yet
- 10 Urogynecologic Problems in Pregnancy and Puerpurium TOG 2022Document9 pages10 Urogynecologic Problems in Pregnancy and Puerpurium TOG 2022Anna JuniedNo ratings yet
- Laparoscopic Splenectomy For Pediatric Wandering Spleen - A Case ReportDocument11 pagesLaparoscopic Splenectomy For Pediatric Wandering Spleen - A Case ReportAdlyn Bea Albesa-BernaldezNo ratings yet
- 1 s2.0 S2221618914600718 MainDocument3 pages1 s2.0 S2221618914600718 MainElizabeth Joan SalimNo ratings yet
- Short Bowel Syndrome: Epidemiology and Etiology: Paul W. Wales, MD, Emily R. Christison-Lagay, MDDocument7 pagesShort Bowel Syndrome: Epidemiology and Etiology: Paul W. Wales, MD, Emily R. Christison-Lagay, MDSubha ManivannanNo ratings yet
- Paediatric Cholestatic Liver Disease: Diagnosis, Assessment of Disease Progression and Mechanisms of FibrogenesisDocument16 pagesPaediatric Cholestatic Liver Disease: Diagnosis, Assessment of Disease Progression and Mechanisms of FibrogenesiswintannNo ratings yet
- Prune BellyDocument33 pagesPrune BellyPrasanna KumarNo ratings yet
- Biliary AtresiaDocument25 pagesBiliary Atresiajulius billiNo ratings yet
- Imaging Patients With Acute Abdominal PainDocument16 pagesImaging Patients With Acute Abdominal PainNaelul IzahNo ratings yet
- International Journal of Pharmaceutical Science Invention (IJPSI)Document3 pagesInternational Journal of Pharmaceutical Science Invention (IJPSI)inventionjournalsNo ratings yet
- Short Bowel SyndromeDocument64 pagesShort Bowel Syndromeeztouch12No ratings yet
- Prenatal Diagnosis of Anterior Abdominal Wall Defects: Pictorial EssayDocument12 pagesPrenatal Diagnosis of Anterior Abdominal Wall Defects: Pictorial EssayNurul ArdaniNo ratings yet
- Biliary SystemDocument15 pagesBiliary SystemDjabhi SpinzzNo ratings yet
- Ginglen 2022 - Necrotizing Enterocolitis - StatPearlsDocument8 pagesGinglen 2022 - Necrotizing Enterocolitis - StatPearlsBee GuyNo ratings yet
- Intestinal Malrotation in Neonates With Nonbilious Emesis: Perinatal/Neonatal Case PresentationDocument3 pagesIntestinal Malrotation in Neonates With Nonbilious Emesis: Perinatal/Neonatal Case PresentationSaurav SultaniaNo ratings yet
- Medicine: A Newborn Patient With Both Annular Pancreas and Meckel 'S DiverticulumDocument5 pagesMedicine: A Newborn Patient With Both Annular Pancreas and Meckel 'S DiverticulumAdrian UmbriaNo ratings yet
- 33 34 IV 12 Atresia BiliarisDocument13 pages33 34 IV 12 Atresia BiliarisTasia AmeliaNo ratings yet
- GastroschisisDocument17 pagesGastroschisisAsterisa PutriNo ratings yet
- From Functional Imaging in Nephro-Urology (Alain Prigent Etc.) (Z-Library)Document10 pagesFrom Functional Imaging in Nephro-Urology (Alain Prigent Etc.) (Z-Library)Francisco BotelhoNo ratings yet
- Embryonic Biliary Atresia in A Very-Low-Birth-Weight Premature InfantDocument7 pagesEmbryonic Biliary Atresia in A Very-Low-Birth-Weight Premature InfantWiwi Dwi PutriiNo ratings yet
- Abdomina Wall Defects 2Document12 pagesAbdomina Wall Defects 2pamellapesseNo ratings yet
- Hirschsprung 1socaDocument34 pagesHirschsprung 1socaDianNo ratings yet
- Congenital Anomalies of The KidneyDocument21 pagesCongenital Anomalies of The KidneyRaghu Rajan100% (1)
- Jejunojejunal Intussusception As Initial Presentation of Coeliac Disease: A Case Report and Review of LiteratureDocument6 pagesJejunojejunal Intussusception As Initial Presentation of Coeliac Disease: A Case Report and Review of Literatureellya theresiaNo ratings yet
- Necrotizing EnterocolitisDocument7 pagesNecrotizing EnterocolitisWardah AlAkrahNo ratings yet
- Hollym Necrotizing Enterocolitis - Pathophysiology and Prevention 4Document14 pagesHollym Necrotizing Enterocolitis - Pathophysiology and Prevention 4api-346859104No ratings yet
- Aipm 17 71Document4 pagesAipm 17 71Iful SaifullahNo ratings yet
- Biliary Atresia Pathology Etiology and PathogenesiDocument17 pagesBiliary Atresia Pathology Etiology and Pathogenesijohn lemonNo ratings yet
- High Output Enterocutaneous Fistula (Case Study) 2011Document6 pagesHigh Output Enterocutaneous Fistula (Case Study) 2011Joon RaynerNo ratings yet
- Biliary Atresia UP To DATEDocument21 pagesBiliary Atresia UP To DATECarlos CuadrosNo ratings yet
- Pedsinreview 2021005196Document4 pagesPedsinreview 2021005196Claudio MontiNo ratings yet
- Tubular Ileal Duplication Causing Small Bowel Obstruction in A ChildDocument5 pagesTubular Ileal Duplication Causing Small Bowel Obstruction in A ChildDiego Leonardo Herrera OjedaNo ratings yet
- Cholestasis of PregnancyDocument6 pagesCholestasis of Pregnancywael123 456No ratings yet
- GastroschisisDocument19 pagesGastroschisiskunaidongNo ratings yet
- Dor Abdominal e FalcidromeDocument7 pagesDor Abdominal e FalcidromeVinicius SpazzapanNo ratings yet
- Imaging of Congenital Anomalies of The Gastrointestinal TractDocument12 pagesImaging of Congenital Anomalies of The Gastrointestinal TractMateen ShukriNo ratings yet
- SyedDocument3 pagesSyededitorijmrhsNo ratings yet
- Nascimento Et Al. - 2012 - Bloody Nipple Discharge in Infancy - Report of Two CasesDocument3 pagesNascimento Et Al. - 2012 - Bloody Nipple Discharge in Infancy - Report of Two CasesflashjetNo ratings yet
- Diseases of the Liver and Biliary TreeFrom EverandDiseases of the Liver and Biliary TreeAnnarosa FloreaniNo ratings yet
- Glandula Pankreas Glandula Adrenal: EndokrinDocument1 pageGlandula Pankreas Glandula Adrenal: EndokrinRegina AyediaNo ratings yet
- Pdca Bab 4Document21 pagesPdca Bab 4Regina AyediaNo ratings yet
- Typhoid JournalDocument7 pagesTyphoid JournalRegina AyediaNo ratings yet
- TRANSLATE Diagnosis and Risk Factors of Acute Kidney Injury in Very Low Birth Weight InfantsDocument1 pageTRANSLATE Diagnosis and Risk Factors of Acute Kidney Injury in Very Low Birth Weight InfantsRegina AyediaNo ratings yet
- Quality Tuberculosis Care in Indonesia: Using Patient Pathway Analysis To Optimize Public-Private CollaborationDocument9 pagesQuality Tuberculosis Care in Indonesia: Using Patient Pathway Analysis To Optimize Public-Private CollaborationRegina AyediaNo ratings yet
- Besteher 2017Document7 pagesBesteher 2017Regina AyediaNo ratings yet
- Atrial Fibrillation and Mechanisms of StrokeDocument7 pagesAtrial Fibrillation and Mechanisms of StrokeRegina AyediaNo ratings yet
- Kasmita KinerjaPosyanduDanStatus 2000 No2!1!10Document10 pagesKasmita KinerjaPosyanduDanStatus 2000 No2!1!10Regina AyediaNo ratings yet
- Carroz Zino 2017Document9 pagesCarroz Zino 2017Regina AyediaNo ratings yet
- Definition of NephrolithiasisDocument30 pagesDefinition of Nephrolithiasiszz_13No ratings yet
- Master Radiology Notes UrologyDocument106 pagesMaster Radiology Notes UrologySafwan ShaikhNo ratings yet
- HydronephrosisDocument4 pagesHydronephrosisNxxxNo ratings yet
- NucRadSHARE Kamal Singh USDocument9 pagesNucRadSHARE Kamal Singh USFurman BorstNo ratings yet
- 5550-Article Text-42309-3-10-20220104Document8 pages5550-Article Text-42309-3-10-20220104the OGs. 96No ratings yet
- Complex Case of Ureteropelvic Junction Obstruction 2024 International JournaDocument3 pagesComplex Case of Ureteropelvic Junction Obstruction 2024 International JournaRonald QuezadaNo ratings yet
- (03241750 - Acta Medica Bulgarica) Horseshoe Kidney With Hydronephrosis - Tales of The UnexpectedDocument3 pages(03241750 - Acta Medica Bulgarica) Horseshoe Kidney With Hydronephrosis - Tales of The UnexpectedTeodorNo ratings yet
- ملزمة القبالة-dddd4Document120 pagesملزمة القبالة-dddd4Shama Awwad100% (1)
- Poncobirowo - NephrolithotomyDocument7 pagesPoncobirowo - NephrolithotomyyuliaydjwNo ratings yet
- Hydronephrosis LWDocument8 pagesHydronephrosis LWvitauxianaNo ratings yet
- UrolithiasisDocument9 pagesUrolithiasisJessa MaeNo ratings yet
- Scan Report PDFDocument1 pageScan Report PDFsrikanth PosaNo ratings yet
- Urinary Tract ObstructionDocument56 pagesUrinary Tract ObstructionMicky FantaNo ratings yet
- PPTDocument27 pagesPPTmonicanasutionNo ratings yet
- DR Shirin Surani Resident Year 1Document29 pagesDR Shirin Surani Resident Year 1arjumandNo ratings yet
- Urology DNB Old QuestionsDocument8 pagesUrology DNB Old QuestionssjulurisNo ratings yet
- Kidney and Ureteral StonesDocument12 pagesKidney and Ureteral StonescubirojasNo ratings yet
- Pathology of Urinary SystemDocument384 pagesPathology of Urinary SystemNzau MuangeNo ratings yet
- Imaging in Genitourinary SystemDocument36 pagesImaging in Genitourinary SystemAlkaustariyah LubisNo ratings yet
- OU SumberDocument5 pagesOU SumberAnggaNo ratings yet
- 7.-El-Husseinys-Essentials-of-Nephrology @eduwaves360Document160 pages7.-El-Husseinys-Essentials-of-Nephrology @eduwaves360Samir C ChNo ratings yet
- Ultrasound in Acute Kidney InjuryDocument70 pagesUltrasound in Acute Kidney InjuryaandakuNo ratings yet
- Renal SystemDocument18 pagesRenal SystemS GNo ratings yet
- Anorectal MalformationDocument29 pagesAnorectal Malformationbimaindra97No ratings yet
- Urology OralDocument2 pagesUrology OralCorina TeteleaNo ratings yet
- Nephrectomy - An OverviewDocument4 pagesNephrectomy - An OverviewNikesh DoshiNo ratings yet
- Siddhars Thought On Renal CalculaiDocument78 pagesSiddhars Thought On Renal CalculaiSabaRajooNo ratings yet
- Benign Prostatic Hyperplasia Concept MapDocument1 pageBenign Prostatic Hyperplasia Concept MapSarah RonquilloNo ratings yet
- Prune Belly SyndDocument11 pagesPrune Belly SyndnadiaryNo ratings yet