Professional Documents
Culture Documents
How Great Thou Art
Uploaded by
Renz Marion AlemaniaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
How Great Thou Art
Uploaded by
Renz Marion AlemaniaCopyright:
Available Formats
872
REVIEW ARTICLE
Rehabilitation of Guillain-Barr Syndrome
Jay M. Meythaler, MD, JD
ABSTRACT. Meythaler JM. Rehabilitation of Guillain- as many as 50,000 persons in the United States have residual
Barr6 syndrome. Arch Phys Med Rehabil 1997;78:872-9. functional deficits of GBS.
Historically, ascending paralytic illness has been recognized
Guillain-Barr6 syndrome (GBS) is the most common cause for centuries but it was Osler7 who offered the first reasonable
of acute neuromuscular paralysis in developed countries. GBS clinical description. Later, Guillain, Barr6, and Strohl 8published
is a significant cause of new long-term disability for at least a report that more adequately described the syndrome of a radic-
1,000 persons per year in the United States, and more elsewhere. uloneuritis associated with elevated protein in the cerebrospinal
Given the young age at which GBS sometimes occurs and the fluid without a "cellular reaction." The definition of GBS is
relatively long life expectancies following GBS, it is likely still largely a descriptive one. Most of the literature reviewed
that at least 25,000 and perhaps 50,000 persons in the US are in this article consists of descriptive case reports, sequential
experiencing some residual effects of GBS. Approximately 40% case series, or retrospective reviews unless otherwise specified.
of patients who are hospitalized with GBS will require admis-
sion to inpatient rehabilitation. For GBS persons necessitating CLINICAL PRESENTATION
admission to inpatient rehabilitation, the requirement of prior Briefly stated, GBS is an immunopathy with an acute, often
ventilator support most strongly predicts an extended length of fulminate evolution of a demyelinafing inflammatory polyradic-
stay on inpatient rehabilitation. Other issues that affect rehabili- uloneuropathy.6 The duration of the illness is usually less than
tation are dysautonomia, cranial nerve involvement, and various 12 weeks in the majority of patients, with most expected to a
medical complications associated with GBS. Deafferent pain have a favorable outcome (generally this is equated to mean
syndrome is common in the early stages of recovery. Multiple ambulation without assistive devices). 1 With an approximate
medical complications, including deep venous thrombosis, joint 5,000 new cases per year and an expected poor outcome of
contractures, hypercalcemia of immobilization, and decubitii, 20% with regard to mobility or pulmonary function in those
may develop in the early stages of recovery and interfere with who survive, 1-3one can conclude this is a significant and under-
the rehabilitation program. Anemia is a frequent finding in the studied cause of disability.
first few months of illness but does not appear to interfere with Classically, GBS has an acute onset (table 1). A devastating
functional recovery. Therapy should not overfatigue the motor acute course may take a person from being absolutely normal
unit, which has been associated with paradoxical weakening. to bedridden and on a respirator within 2 or 3 days. The progres-
Little is known of the long-term implications of the disability sion usually occurs over 10 to 12 days before a plateau is
caused by GBS. Work similar to that performed for postpolio reached, followed by gradual recovery. Some patients may have
syndrome and spinal cord injury should be started in the rehabil- a stuttering onset, while others may present with a rather slow
itation setting. progression that can take place over a few weeks. 9 Approxi-
© 1997 by the American Congress of Rehabilitation Medicine mately 40% to 60% of patients have some antecedent infectious
and the American Academy of Physical Medicine and Rehabili- process. 6'1°In interviews with patients, nonspecific or "flulike"
tation upper respiratory infections are reported most frequently.1 These
usually occur approximately 2 to 4 weeks before the onset of
weakness. Gastrointestinal illnesses, often relatively mild, are
UILLAIN-BARRI~ syndrome (GBS) is the most common
G cause of acute nontraumatic neuromuscular paralysis in
developed countries, afflicting 1 to 2 per 100,00 people annu-
reported as the second most common type of illness. ~ Viruses
which have been most often implicated are cytomegalovirus
and Epstein-Barr virus. TM Surgical procedures and trauma are
ally. 1-3 There is almost a 2:1 preponderance towards males. ~ predisposing events in a small percentage of patients, certainly
Approximately 10% of patients die and 20% are left with defi- less than 2% or 3%. 9 Flu vaccines have been implicated in some
cits in ambulation or require ventilator assistance a year later.4-6 cases, 9'a2 and more recently human immunodeficiency virus
There are an approximately 5,000 new cases per year in the (HIV) has been implicated in the development of GBS. 11
United States, which is half the incidence of spinal cord in- Campylobacter jejuni enteritis has recently been recognized as
jury. 1-3 Therefore, GBS is a significant cause of new long-term an important preliminary disease 1° and has been linked to the
disability for at least 1,000 persons per year in the United States. more severe axonal variety. 13 Epidural anesthesia, as well as
The prevalence of those who have long-term disability second- drugs, including thrombolytic agents and heroin, have been as-
ary to GBS is unknown. Given the young age at which GBS sociated with a few cases.l° Underlying systemic disease such as
can occur however, it is likely that at least 25,000 and perhaps lupus erythematosis, sarcoidosis, Hodgkin's disease, and other
neoplasms have been recognized to cause a small number of
From the Spain Rehabilitation Center, and Department of Rehabilitation Medi- "symptomatic" cases of GBS] °'14
cine, University of Alabama School of Medicine, Birmingham, AL. Acute GBS typically begins with fine paresthesias in the toes
Submitted for publication August 2, 1996. Accepted in revised form January or fingertips (tables 1, 2) followed within days by the major
21, 1997. clinical manifestation, weakness, which evolves more or less
No commercial party" having a direct financial interest in the results of the
research supporting this article has or will confer a benefit upon the authors or symmetrically over several days. Leg weakness may make
upon any organization with which the authors are associated. walking and stair climbing difficult. Variable arm, facial, and
Reprint requests to Jay M. Meythaler, MD, JD, Associate Professor, Spain oropharyngeal weakness follows as paresthesias extend proxi-
Rehabilitation Center, Department of Rehabilitation Medicine, University of Ala- mally. 14,~5
bama School of Medicine, 1717 6th Avenue South, Birmingham, AL 35233-7330.
© 1997 by the American Congress of Rehabilitation Medicine and the American
Early in the illness there are many clinical features that sug-
Academy of Physical Medicine and Rehabilitation gest the disease. Initially, the patient will demonstrate approxi-
0003-9993/97/7808-419953.00/0 mately symmetric limb weakness, absent or greatly diminished
Arch Phys Med Rehabil Vol 78, August 1997
REHABILITATION OF GBS, Meythaler 873
Table 1: Frequency of Features and Clinical Variants of Acute GBS than 20% of normal; (3) summed distal motor amplitude less
% Frequency than 20% of normal.9
Fully
There is described a primary axonal variety of GBS ~7 that
Developed may account for part of the discrepancy between the clinical
Condition Initially Illness diagnostic criteria and the electrodiagnostic criteria.
Features of Syndrome A confirmatory workup should include an examination of
Paresthesia 70 85 cerebrospinal fluid, which usually reveals a normal pressure,
Weakness few or no cells, and a protein concentration of >.55g/L after
Arms 20 90
Legs 60 95 the first week of illness.I°
Face 35 60
Oropharynx 25 50 CLINICAL AND P A T H O P H Y S I O L O G I C MODELS
Ophthalmoparesis 5 15
Sphincter dysfunction 15 5 Pathologically, GBS is an inflammatory polyradiculoneuro-
Ataxia 10 15 pathy that resembles experimental allergic neuritis (EAN) in
Arefiexia 75 90
Pain 25 30 animals) 1 Both EAN and GBS share common histopathologic
Sensory Loss 40 75 features, characterized by the presence of perivascular mononu-
Respiratory failure 10 30 clear cell inflammation, demyelination, and edema. Experiments
CSF protein >0.55 g/liter 50 90 in various animal models have demonstrated that the sensitiza-
Clinical variants*
Fisher's syndrome 5 tion of T-lymphocytes of the CD4 subclass to proteins in the
Weakness without paresthesia or loss 3 myelin sheath is necessary for disease induction.2~The principle
Pha ryngeal-cervical-brachial weakness 3 electrophysiologic finding that accounts for the weakness noted
Paraparesis 2 in GBS, at least early in the disease, is the conduction block
Facial paresis with paresthesia 1
Pure ataxia 1 produced when a portion of the axon fails to transmit impulses
in a segment where myelin has been destroyed or rendered
* Variants are associated with diminished reflexes, demyelinating fea- nonfunctional)2
tures as detected on electrophysiologic studies, and elevated cerebrospi-
nal concentrations of fluid protein. Frequencies shown are those found Recently, the presence of antiganglioside antibodies, such as
in fully developed illness. antiganglioside GM1 antibodies or antiganglioside GQlb anti-
Adapted and reprinted by permission of The New England Journal of bodies, has been associated with axonal damage and a poorer
Medicine, Ropper AH, The Guiilain-Barr6 syndrome, 326:1130-6, copy-
right 1992, Massachusetts Medical Society; and adapted and reprinted
outcome. 23 GMt gangliosides are used clinically to reduce the
from Asbury and Cornblath, 12with permission. amount of neurological injury in SCI. A suggested link between
the use of gangliosides and GBS has not been established.2427
Furthermore, there has been a proposed link between the pres-
tendon reflexes, and minimal loss of sensation despite the pares- ence of IgG anti-GDta and anti-GMt antibodies and a more
thesias. 1° Pain is common, presenting as either a bilateral sciat- severe presentation of GBS. 28'29
ica or aching in large muscles of the upper legs, flanks, or
back. 16 Weakness of the facial muscles occurs in about one DIFFERENTIAL DIAGNOSIS
third of all cases, to In severe cases the disease affects respiration,
and may result in cranial nerve palsies with associated func- GBS as a recognizable entity is based on descriptive criteria.
tional losses in eye movements and deglutition.1° Disturbances The features required for diagnosis are a progressive motor
of autonomic function (sinus tachycardia and, less often, brady- weakness of more than one limb and areflexia. 1° The current
cardia and facial flushing, fluctuating hypertension and hypoten- proposed electrodiagnostic criteria for GBS are for the demy-
sion, loss of sweating or episodic profuse diaphoresis) are com- elinating versions of the disease and do not cover the primary
mon, but in the majority of patients these abnormalities do not axonal variety. 3°
persist for more than a week or two. t°
There are many variants of GBS that may cause diagnostic Table 2: Diagnostic Criteria for Typical GBS
difficulty, including Fisher's syndrome, which involves ophthal-
moplegia, ataxia and areflexia with little weakness and accounts Features required for diagnosis
Progressive weakness in both arms and both legs
for approximately 5% of the cases14'17; weakness without pares- Areflexia
thesias or sensory loss; isolated weakness of the arm and oro- Features strongly supporting the diagnosis
pharynx, or of the leg~8; bilateral weakness of facial muscles Progression of symptoms over days to 4 wks
with distal paresthesias; severe ataxia and sensory loss; acute Relative symmetry of symptoms
Mild sensory symptoms or signs
pandysantonomia, an autonomic polyneuropathy often com- Cranial-nerve involvement, especially bilateral weakness
bined with sensory featurest9; and "axonal" GBS with rapid, of facial muscles
almost complete paralysis and electrically inexcitable motor Recovery beginning 2 to 4 weeks after progression ceases
nerves.2° The effect of these many "subtypes" on the ultimate Autonomic dysfunction
Absence of fever at the onset
functional outcome or disability of the afflicted patients is not Elevated concentration of protein in cerebrospinal fluid,
sufficiently known (table 2). with fewer than 10 cells per cubic millimeter
Typical electrodiagnostic features
Features making the diagnosis doubtful
E M G and Laboratory Findings
Diagnosis of botulism, myasthenia, poliomyelitis,
Abnormalities of nerve conduction, reflecting demyelination, or toxic neuropathy
are the most sensitive and specific laboratory findings in GBS, Abnormal porphyrin metabolism
Recent diphtheria
and there are proposed diagnostic criteria for the demyelinating Purely sensory syndrome, without weakness
versions of the disease t2 (table 3).
Adapted and reprinted by permission of The New England Journal of
Electrodiagnostic and physiologic parameters associated with Medicine, Ropper AH, The Guillain-Barre syndrome, 326:1130-6, copy-
a poor outcome include (1) summed motor velocity less than right 1992, Massachusetts Medical Society; and adapted and reprinted
80% of normal, (2) summed proximal motor amplitude less from Asbury and Cornblath, 1=with permission.
Arch Phys Med Rehabil Vol 78, August 1997
874 REHABILITATION OF GBS, Meythaler
Table 3: Proposed Electrodiagnostic Criteria for Demyelination of Peripheral Nerve
These criteria concern nerve conduction studies (including proximal nerve segments) in which the predominant process is demyelination.
Must have three of the following four features:
1. Reduction in conduction velocity in two or more motor nerves.
a. <80% of lower limit of normal (LLN) if amplitude >80% of LLN.
b. <70% of LLN if amplitude <80% of LLN.
2. Conduction block or abnormal temporal dispersion in one or more motor nerves: either peroneal nerve between ankle and below fibular head,
median nerve between wrist and elbow, or ulnar nerve between wrist and below elbow,
Criteria for partial conduction block:
a. <15% change in duration between proximal and distal sites and >20% drop in negative-peak area of peak-to-peak amplitude between
proximal and distal sites.
Criteria for abnormal temporal dispersion and possible conduction block:
a. >15% change in duration between proximal and distal sites and >20% drop in negative-peak area or peak-to-peak amplitude between
proximal and distal sites.
3. Prolonged distal latencies in two or more nerves,
a. >125% of upper limit or normal (ULN) if amplitude >80% of LLN.
b. >150% of ULN if amplitude <80% of LLN.
4. Absent F-waves or prolonged minimum F-wave latencies (10-15 trials) in two or more motor nerves.
a. >120% of ULN if amplitude >80% of LLN,
b. >150% of ULN if amplitude <80% of LLN.
Adapted and reprinted from Annals of Neurology V27 (Suppl), $21-$24, 1990, by permission of Little, Brown and Company (Inc.).
The differential diagnosis is generally determined by the clin- use of infused immunoglobulins (IVIg). 35 Infusion of immuno-
ical course and the pattern of weakness and includes spinal cord globulin has been associated with a beneficial outcome in other
compression, transverse myelitis, myasthenia gravis, basilar ar- immunologically mediated diseases. 9'22Results from a prospec-
tery occlusion, neoplastic meningitis, vasculitic neuropathy, tive, randomized Dutch trial of 100 GBS patients treated with
polymyositis, metabolic myopathies, and paraneoplastic neu- IVIg compared to plasmapheresis suggests that IVIg is as good,
ropathy. I° Other diagnoses that can be confused with GBS in- if not better, than plasmapheresis. 36 There have been reports,
clude hypophosphatemia, heavy-metal intoxication, neurotoxic however, of a high incidence of relapses following IVIg. 23 Al-
fish poisoning, botulism, poliomyelitis, and tick paralysis. 1° though treatment with plasma exchange and immunoglobulins
Various syndromes present with many of the same clinical has decreased the duration of mechanical ventilation by half,
and diagnostic findings of GBS, including chronic immune de- GBS still remains the most common cause of acute neuromuscu-
myetinating polyneuropathy, autoimmnne neuropathies caused lar ventilatory failure. 37
by connective tissue diseases, cancer, toxic neuropathies, and
hormonal and metabolic neuropathies. 10 ' 12' 14'31 The greatest diag- Steroids
nostic controversy surrounds chronic inflammatory demyelinat- The use of steroids in treatment of acute GBS has been con-
ing polyneuropathy (CIDP) and relapsing inflammatory poly- troversial.38 Their use was based on promising trials with EAN
neuropathy, which are considered by some to be separable from in animals,39 and in early clinical trials with humans it was
GBS. 1° This separation may indeed be arbitrary or logically suggested that steroids were useful in decreasing the severity
defensible as separating the various clinical presentations of of illness.38 However, in a large randomized prospective study
multiple sclerosis. What is important from a rehabilitation stand- of 242 patients treated with 500mg methylprednisolone, it was
point is that the clinical course may vary considerably in these concluded that steroids were ineffective.2
other presentations from those of classically described GBS, so CLINICAL COURSE
an accurate diagnosis and prognosis is important. The course of illness may be more prolonged in adults, partic-
ularly older adults, than in children.9 Persons who have suffered
TREATMENT GBS may continue to improve for up to 2 years after injury,4°'41
Progress is being made in the treatment of GBS. It has been although there is little information other than general descrip-
suggested that improved rates of survival are related to the tions on the rate or variability of the neurological recovery.
special care units staffed by personnel who are experienced in Prognostic factors with regard to a poor outcome recently identi-
handling the complications of the disease. 1° Most of these spe- fied in a North American study9'42 were older age, requirement
cial care units are located in regional medical centers that treat for respiratory support, rate of progression, abnormal physiolog-
the majority of cases. Many GBS patients die of avoidable ical characteristics of peripheral nerve function, or if no plasma-
medical complications such as sepsis, adult respiratory distress pheresis was performed. 9'42 There has been no correlation be-
syndrome, pulmonary emboli (usually secondary to deep venous tween recovery from GBS and sex, occupation, the presence of
thrombosis), or cardiac arrest perhaps related to dysautonomia. diabetes mellitus, previous steroid use, or prior immuniza-
With appropriate medical supportive care, the rate of mortality tion.9,43
could be reduced to less than 5%. w The point of maximal neurologic dysfunction is reported as
the "disease nadir."9 The average period from the clinical onset
symptoms to nadir of illness is 8 days. 1The point of time before
Plasmapheresis and Intravenous Immunoglobulin or at disease nadir has frequently has been considered critical
Plasmapheresis and intravenous immunoglobulin (IVIg) are with regard to the success of therapeutic interventions utilizing
the accepted therapy for GBS. The North American and French plasmapheresis or IVIg, 9 but this has never been established
prospective, randomized clinical trials clearly demonstrate that and in one study did not correlate with outcome. 44 Yet many
plasmapheresis shortens the time required to achieve indepen- institutions will not intervene with plasmapheresis or IVIg if
dent walking and the time a patient stays on a respiratory sup- the patient has already begun neurological recovery or has not
port. In addition, plasmapheresis is reported to improve func- deteriorated neurologically for several days. More work is nec-
tional improvement of mobility at 6 months. 32~34 essary to delineate whether late intervention after the point of
Besides plasmapheresis, another alternative treatment is the disease nadir is useful.
Arch Phys Med Rehabil Vol 78, August 1997
REHABILITATION OF GBB, Meythaler 875
In our experience, patients with GBS who were so severely 100 patients, 11 developed cardiac arrhythmias sufficient to
involved as to require admission to inpatient rehabilitation had compromise their circulation and 7 of the 1 1 died. 48 Despite
an extended period to disease nadir. Clearly, patients with GBS the recent attention to dysautonomia and its relevance to both
requiring inpatient rehabilitation are the more severely involved. morbidity and mortality,48 there have been no prospective stud-
The development of relapses may be related to a more extended ies on predicting its onset or evaluating various interventions
course of the disease in these patients. Frequent neurologic to limit its impact.
evaluations will detect the development of relapses, and inter-
vention with plasmapheresis and/or IVIg may be of therapeutic
Pain and Sensory Involvement
benefit.
There are multiple medical complications that may develop Most reports of GBS describe pain as a prominent clinical
from GBS. Many of these complications may persist for some feature of the diagnosis, and it has been reported to be the sole
time, interfering with rehabilitation or even leading to perma- initial presenting symptom in some cases. 5° The types of pain
nent functional deficits. described include paraesthesia, dysaesthesia, axial and radicular
pain, meningism, myalgia, joint pain, and visceral discomfortfi
Requirement of Ventilatory Support In one small prospective study 16early pain was reported in 55%
of the patients and in 72% of the patients throughout the whole
Little is known regarding the predisposing factors that result
in the need for support. It has been noted that autonomic dys- course of illness. Symptoms of mild depression that continues
function is related to the requirement of ventilatory support. 14'is long after the initial onset, indicated by persistent mental fa-
tigue, are common. I° This may be exacerbated by deafferent
In epidemiologic studies it is estimated that 10% to 30% of
pain syndromes.
patients will require mechanical ventilation, 5% to 10% will
remain seriously disabled, and 3% to 8% will die. 37 Intubation
should be considered when the vital capacity decreases to Immobilization
<lSmL/kg. 1° The need for-ventilatory support correlates with
GBS patients are usually hypotonic or flaccid as well as
outcome as evaluated by ambulatory function. 15 More recently,
immobilized. They develop complications of decubitis ulcers,
ventilatory support has been correlated with longer lengths of
tendon shortening, joint contractures, and malalignment, as well
stay and increased costs for inpatient rehabilitation.43
as peroneal nerve palsies. 1° Yet the treatment approach has been
Respiratory failure and pneumonia may occur in 30% of
similar to that used for many patients who have an upper motor
patients in the acute phases of illness (first 12 weeks), but many
neuron lesion such as spinal cord injury or traumatic brain
will have adequate recovery of their respiratory function]° As
injury. How these medical complications and functional deficits
many as 25 % of these patients will develop pneumonia.I° Those
affect the final disability of these patients is unknown. The
who do not have full respiratory recovery may have complica-
incidence of immobilization on the development of functional
tions leading to long-term morbidity secondary to antecedent
deficits is not well understood in GBS. Can the same treatment
chronic obstructive disease, restrictive pulmonary disease from
milieu be utilized in this lower motor neuron disease when the
pulmonary scarring secondary to pneumonia, tracheitis from
predisposing factors and impact of these therapies are not well
chronic intubation, or respiratory musculature insufficiencyY
delineated?
Dysfunction of bone and calcium metabolism can occur in
Deep Venous Thrombosis
GBS. Heterotopic ossification has been reported in GBS. 52's3
Deep venous thrombosis (DVT) is considered to be common Hypercalcemia of immobilization of such a severe nature as to
in GBSY The incidence of DVT in GBS is unknown because require aggressive medical intervention has been noted in a few
it has never been systematically studied. In one early study,46 case reports of GBS. 52'54 Both of these conditions are fairly
pulmonary embolus (PE) was believed to occur in up to one common in spinal cord injury, but the incidences of both have
third of patients who suffered from GBS. However, predispos- not been well defined in GBS and are believed to be the result
ing factors such as the severity of disease or the length of of prolonged immobilization.52
immobilization have not been well delineated.46 While prophy-
lactic treatment for DVT is recommended by some authors, 1°'45
without knowing the incidence or risk factors for the develop- Anemia
ment of DVT, it is hard to make informed judgments regarding Anemia in persons with GBS with such severe involvement
the type and length of prophylaxis necessary. as to require inpatient rehabilitation is more common than that
found in the corresponding spinal cord population.5s'56The ane-
Dysautonomia mia may in part be related to immobilization. In a retrospective
Dysautonomia in GBS is indicated by orthostatic hypoten- study, 79% of persons admitted to acute inpatient rehabilitation
sion, unstable blood pressure, or abnormal heart rates. This from GBS had anemia with hematocrits and hemoglobin two
definition has recently been expanded to include bowel and standard deviations below the mean.55 Patients with a history
bladder dysfunction.47 Autonomic dysfunction without bladder of receiving plasmapheresis had a higher mean hemoglobin and
and bowel dysfunction is related to the need for ventilatory hematocritY A study on the effects of immobilization in healthy
support. 14A5'48'49Dysautonomia has been found in particularly male subjects who were confined to bed rest found that the
severe versions of GBS, extending the acute care length of stay red cell count and reticulocyte count declined slowly over 5
in previous epidemiological studies,48'49 and is believed to be weeks. 57'~8All these changes reversed with mobilization. Plas-
clinically related to life-threatening cardiac arrhythmias.47 Uro- mapheresis may be a factor, by reducing inflammatory immuno-
logic dysfunction may develop early in the disease process but globulins that may interact with bone marrow precursorsY It
it is believed to resolve in most cases; however, this conclusion has been suggested that correcting anemia may aid in the treat-
appears to be based totally on anecdotal evidence, m2 Some ment of orthostatic hypotension in persons with GBS 9 Anemia
men will develop residual impotence, l° Dysautonomia has been appears not to relate to rehabilitation outcome or length of stay
linked to cardiac arrhythmias, cardiovascular collapse, and for those persons with such severe involvement as to require
death in various case reports of GBS. 47 In one case series of inpatient rehabilitation.55
Arch Phys Med Rehabil Vol 78, August 1997
876 REHABILITATION OF GBS, Meythaler
Cranial Nerve Involvement healthy; 1, minor symptoms or signs; 2, able to walk 5m without
Crania/ nerve involvement has been described in the more assistance; 3, able to walk 5m with assistance; 4, chair-bound
severe cases of GBS.14'~5In one study cranial nerve involvement or bed-bound; 5, requiring assisted ventilation for at least part
was associated with an increased total length of hospital stay of the day or night; 6, dead. One problem with this scale is that
(acute and rehabilitation combined) for persons with such severe the length of time patients are followed varies between 6 months
involvement as to require inpatient rehabilitation.43In a previous and 12 months, while recovery may continue for up to 18
study, cranial nerve involvement was associated with a pro- months, nor has this 6-point functional scale ever been corre-
longed duration to reach the plateau phase of illness, but did lated with more traditional, and more frequently employed,
not aid in predicting future motor deficitJ 5 Cranial nerve scales that measure function and aid in the assessment of disabil-
involvement may result in dysphagia, bilateral vocal cord paral- ity. More importantly, this scale may not be sensitive enough to
ysis, optic neuritis, and hearing loss. I4'15'60-63 detect subtle changes in function with various treatment options.
Furthermore, the interrater reliability and reproducibility of this
scale has never been established. Consequently, the validity and
REHABILITATION reliability of studies regarding the effectiveness of therapeutic
Approximately 40% of the patients who are hospitalized with interventions such as plasmapheresis,4z IVIg, 36 or steroids 2 may
GBS will require inpatient rehabilitation.4°'43They are generally be in question. The usefulness of this scale in relation to the
considered the more severely involved patients. One study4° more traditional scales used to measure outcome in rehabilita-
described an incidence of persistent plegia in 54% of these tion has yet to be established.
patients, ranging from monoplegia to tetraplegia of 54%. Reha- Another important issue that needs to be addressed by rehabil-
bilitation requires an organized program with defined end itation research is how GBS patients age with a functional defi-
points, yet no long-term rehabilitation outcome studies have cit. The extent of muscle strength recovery after GBS may be
been done. The lack of systematic studies on rehabilitation out- a major determinant of the patient's ultimate functional poten-
come has been noted in the literature recently. 1° Consequently, tial.2.a0.28
most rehabilitation approaches for measuring functional out-
come in GBS have been adopted on the basis of experience REHABILITATION THERAPEUTICS
with other diseases. The only studies reported are largely de-
scriptive with no well-defined functional outcomes except for Motor Recovery and Musculoskeletal Complications
physical findings regarding weakness or alterations in gait. 4°'41'44 There have been no systematic studies on the efficacy of
There are patients who will have a relapse of the disease; physical therapy in GBS. l° Generally, therapy approaches have
these relapses are believed to be more frequent with the current been adapted from experiences with other neuromuscular ill-
treatments, particularly IVIg. 23 Since the course of GBS remains nesses and diseases. GBS patients may present with such diverse
clinically unpredictable at its onset, and patients are in general findings as significant involvement with quadriparesis, or iso-
being transferred to rehabilitation more quickly, close supervi- lated weakness of the arm, leg, facial muscles, or oropharynx.
sion on an inpatient rehabilitation service is warranted. This It has been suggested that overfatiguing the affected motor unit
evaluation should include detailed daily physical examinations, in therapy may impede recovery. 67'6sClearly, overworking mus-
documenting motor and sensory tests, to evaluate for relapses cle groups in patients with peripheral nerve involvement has
and/or complications. been clinically associated with paradoxical weakening.68
Functional motor gain and recovery on inpatient rehabilita- Motor weakness has been associated with muscle shortening
tion as measured by the admit motor and discharge FIM Rasch and resultant joint contractures. These complications can be
motor converted score on admission to rehabilitation correlate prevented with daily range-of-motion exercises. 69Depending on
strongly with the requirement for ventilatory support, 43 and the amount of weakness, exercise can be passive, active-as-
agree with other epidemiologie studies which generally evalu- sistive, or active. Proper positioning in patients is necessary.
ated outcome by ambulatory function.4'15 Initial exercise, even in the acute phases, may include a program
Poor proprioceptive function has been associated with a of gentle strengthening involving isometric, isotonic, isokinetic,
longer length of stay on inpatient rehabilitation.43 There was, manual-resistive, and progressive resistive exercises carefully
however, no association with propfioceptive changes and func- tailored to the clinical condition of the patient.69 Orthotics
tional status as measured by the admit motor and discharge FIM should be prescribed for proper positioning and optimizing re-
Rasch motor converted score on admission to rehabilitation, so sidual motor function.
the connection is unclear.43 Also, there appears to be no relation
between the presence of relapses and rehabilitation outcome Sensory Dysfunction and Pain
except for lower FIM Rasch-converted motor discharge scores The treatment of pain has generally been directed clinically,
from in-patient rehabilitation.43 This relation may be related to noted by the prominent use of antidepressants and, in some
the more extended course of the disease in these patients, but cases, the use of carbamazepine. More recently, there have been
requires further study. verbal reports on the use of topical capsaicin and/or transeutane-
GBS is a disease that often leads to a functional deficit. Little ous electrical stimulation to the specific well-localized anatomic
is known about the true incidence of disability in GBS patients. areas of deafferent pain. Pain in the limbs and axial skeleton
The absence of deep tendon reflexes in upper or lower extremi- has been linked in one report to impaired joint mobility in
ties, as well as severe distal upper extremity weakness or lower GBS. 7° GBS patients with severe pain may have a poor tolerance
extremity weakness, are all indicative of incomplete recovery. 44 for activity resulting in a longer lengths of stay. Various desensi-
This may lead to an impairment, which is defined as "any tization techniques utilized in the therapies may be clinically
loss or abnormality of psychological, physical, or anatomical useful. At our institution medical intervention usually starts with
structure or function. ''64 Disability, as defined by the World tricyclic antidepressants, capsaicin, and transeutaneous nerve
Health Organization exists when an impairment prohibits one stimulation. Second-line agents include anticonvulsants (carba-
from accomplishing a task required for personal independence.64 mazepine, gabapentin) that are reported to be possibly effective
Assessment of disability in GBS has usually been on a crude in neurogenic pain. 71'72 Occasionally, in patients who have unre-
6-point ordinal scale, or some modification thereof2'28'32'65'66:0, mitting pain, pain medications such as tramad01 or narcotics
Arch Phys Med Rehabil Vol 78, August 1997
REHABILITATION OF GBS, Nleythaler 877
are indicated in the early stages of treatment to give relief peripheral nervous system, makes proper positioning a necessity
until the above measures have time to become effective. Many to protect peripheral nerves that may be compressed between
patients will relate a history of severe pain in the early stages body prominences and the bed. 69 The nerves most frequently
of recovery from GBS, yet there are few studies on the nature or involved are the ulnar, peroneal, and the lateral femoral cuta-
duration of this pain. There are no significant studies regarding neous sensory nerves.
interventions for deafferent pain syndrome in GBS. In patients with immobilization hypercalcemia, early mobili-
There are patients with significant involvement in vibratory zation, even in a therapeutic pool, was correlated with a thera-
sensation and joint position. Proprioceptive losses cause ataxia peutic decrease in the serum calcium level. 52 The use of aggres-
and incoordination, resulting in functional deficits. For these sive range of motion may also impede the effects of heterotopic
patients, therapy should include techniques of sensory reintegra- ossification on joint mobility and function.
tion and repetitive exercises to redevelop coordination. These No studies have been performed on the nutritional needs
techniques will aid in developing motor engrams that are based of these patients. In our clinical experience, close nutritional
on the altered sensory perception. monitoring is warranted as patients tend to lose weight in the
acute stage of illness. Interestingly, with immobilization and
Dysautonomia reduced activity, many patients who can eat tend to gain weight
after the first few weeks of illness. The consequent weight gain
Any suggestion that dysautonomia is uncommon, and insig- impedes the potential functional gains in transfers and mobility
nificant clinically, is incorrect. Most patients who come to inpa- one would expect with motor recovery.
tient rehabilitation are probably not as threatened by cardiac
an-hythmias; however, because these patients are the more se- Psychological and Social Issues
verely involved, they may still have problems with postural
Psychosocial variables affect outcome in the rehabilitation of
hypotension, hypertension, and excessive sympathetic outflow,
many other diagnoses. Symptoms of mild depression long after
or bladder and bowel dysfunction. Postural hypotension, which
the initial onset, indicated by persistent mental fatigue, are com-
can be disruptive to therapy, is frequently found in those patients mon, although GBS itself does not result in chronic fatigue
who are so severely involved as to require inpatient rehabilita-
syndromeY Clearly, an extended period in the intensive care
tion. A recent review of the literature involving dysautonomia
setting, due to ventilatory support, can affect cognitive function.
estimates that between 19% to 50% of all GBS patients in a
Research could establish whether severely involved GBS pa-
hospital setting will have evidence of postural hypotension. 47
tients have many of the same psychological and social issues
Patients who have excessive sympathetic outflow and hyperten-
that spinal cord injury patients have. This could then result in
sion appear to have extreme sensitivity to vasoactive drags. 47'73
the use of already established interventions.
These patients are particularly likely to develop these episodes
of hypotension or hypertension with suctioning. 74 This is of Respiratory Complications
concern because some patients are prone to cardiac arrhyth-
Respiratory failure and pneumonia may be found in 30% of
mias. 75 Treatment should be directed toward physical modalities
the acute cases in the first 12 weeks. 44 Aggressive respiratory
such as compression hose, abdominal binders, and proper hydra-
therapy with pulmonary toilet is necessary in the early stages
tion. of disease, including acute inpatient rehabilitation, as it would
Bowel and bladder dysfunction is generally of the lower mo-
be with any patient with a neuromuscular disease affecting pul-
tor neuron variety. Urological dysfunction may develop early
monary function. Because this issue appears to be the strongest
in the disease process but is believed to resolve in most predictor of hospital length of stay~ 43'48 close monitoring is nec-
cases. 1°'~2Initial management of the bladder should be directed
essary. Patients with cranial nerve involvement are particularly
toward avoiding overdistention of the bladder with consequent
susceptible to pulmonary infections, due to aspiration. Perhaps
bladder wall disruption. Furthermore, up to 30% of patients
this is why cranial nerve involvement has been so closely linked
acquire urinary tract infections, x°
to ventilatory dependence and severity of GBS. 43'48
GBS leads to restrictive pulmonary function that may persist
Immobilization for some time after ventilatory assistance is discontinued. Re-
The incidence of DVT in GBS in the rehabilitation setting is strictive pulmonary conditions in other diseases have been asso-
unknown because it has never been studied. Predisposing factors ciated with sleep hypercapnea and hypoxia during rapid eye
for DVT development, such as the severity of disease or the movement (REM) sleep, because within the central nervous
length of immobilization, have not been well delineated.46 Since system, the centrally mediated ventilatory response to hypoxia
the most severely involved patients are those referred to inpa- and hypercapnia are diminished during sleep, ys-sl Many patients
tient rehabilitation, most rehabilitation physicians utilize pro- may be assessed on the floor by the use of frequent nighttime
phylaxis for DVT. Judgments regarding the type and length of observations using a pulse oximeter. Treatment with bilevel
prophylaxis are difficult without knowing the incidence of, or positive airway pressure (BiPAP) may be indicated for patients
risk factors for, DVT development. Early mobilization appears who develop sleep hypoxia or hypercapnia. More recently it
to be beneficial in similar patient groups. has been suggested that theophylline may benefit patients who
Clearly, prolonged immobilization leads to a reduction of present with reduced hypercapnia or hypoxia at night due to
blood volume 76'v7 and increased episodes of postural hypoten- central respiratory control mechanisms accommodating to pro-
sion in the rehabilitation setting. 43 In other immobilized patients, longed blood gas alterations. 82
a tilt table has been a useful therapeutic tool. Clearance of secretions to reduce the work of breathing is
These patients tend to lose a significant amount of body mass necessary, s3 Often this will require the use of resistive inspira-
because of immobilization, particularly muscle mass. When this tory training. Since many of these patients will initially have a
is combined with a significant sensory loss, patients are suscep- tracheostomy, a proper tracheostomy tube capping protocol with
tible to the development of decubitis ulcers from immobiliza- fl'equent rest periods needs to be instituted. One must be careful
tion. Proper bed positioning with frequent postural changes is not to overfatigue the muscles of respiration during the initial
required to prevent the development of decubitii. period of motor unit recovery, because this may push the patient
The loss of body mass, coupled with an already compromised into respiratory failure.
Arch Phys Med Rehabil Vo178, August 1997
878 REHABILITATION OF GBS, Meythaler
OUTPATIENT AND LONG-TERM FOLLOW-UP 15. Hughes RAC. Guillain-Ban'6 syndrome. London: Springer-Verlag;
1990.
The extent and duration of physically disabling sequelae with 16. Ropper AH, Shahani BT. Pain in Guillain Barr6 syndrome. Arch
GBS, including the incidence of secondary medical complica- Neurol 1984;41:511-4.
tions, has never been adequately described. With regard to mo- 17. Fisher M. An unusual variant of acute idiopathic polyneuritis (syn-
tor function, poliomyelitis and GBS have many similar clinical drome of ophthalmoplegia, ataxia, and areflexia). N Engl J Med
issues. It is not known whether the same long-term problems 1956; 255:57-65.
will develop in this population because of loss in the number 18. Ropper AH, Unusual clinical variants and signs of Guillain-Barr6
of active motor units. Furthermore, there have been no long- syndrome. Arch Neurol 1986; 43:1150-2.
term studies on aging in patients who have GBS. It is likely 19. Young RR, Asbury AK, Corbett JL, Adams RD. Pure pan-dysanto-
that these patients will have a loss of function as they age, nomia with recovery: Description and discussion of diagnostic crite-
ria. Brain 1975;98:613-36.
similar to patients with postpoliomyelitis. 84 One can assume
20. Feasby TE, Gilbert JJ, Brown WF, et al. An acute axonal form of
that there are outpatient therapy programs that can aid in the Guillain-Barr6 polyneuropathy. Brain 1986; 109:1115-26.
maintenance of functional capacity. Until studies are performed, 21. Brosnan CF, Clandio L, Tansey FA, Martiney J. Mechanisms of
much of the rehabilitation of GBS will be based on the experi- autoimmune neuropathies. Ann Neurol 1990;27:$75-$79.
ence gleaned from similarly presenting conditions. 22. Soueidan SA, Dalakas MC. Treatment of autoimmune neuromuscu-
The incidence of GBS, which is half that of SCI, is the most lar diseases with high-dose intravenous immune globulin. Pediatr
prevalent cause of acute nontranmatic neuromuscular paralysis Research 1993;33:$95-$100.
in the US. Undoubtedly, a significant number of the patients 23. Hughes RA, Rees JH. Guillain-Barr6 syndrome. Curr Opin Neurol
discharged directly to home could benefit from outpatient reha- 1994;7:386-92.
bilitative services. Furthermore, vocational and psychosocial 24. Samson JC, Fiori MG. Gangliosides and Guillain-Barr~ syndrome:
no casual link. BMJ 1994;308:653.
outcomes have not been addressed in any studies. The services
25. Diez-Tejedor E, Gutierez-Rivas E, Gil-Peralta A. Gangliosides and
for patients disabled by GBS, however, are as fragmented as Guillain-Barr6 syndrome: the Spanish data. Neuroepidemiology
those originally described two decades ago for TBI and SCI. 1993; 12:251-6.
This fragmentation led to the creation of model systems of 26. Beghi E. Exposure to exogenous gangliosides and Guillaln-Barr6
care, which developed a comprehensive continuum of care to syndrome. Neuroepidemiology 1995; 14:45-8.
improve the lives of patients with TBI or SCI. In GBS, there 27. Grigoletto F. Gangliosides and Guillain-Barr6 syndrome. Apparent
is a similar need for research to estimate the needs of this association is a coincidence. BMJ 1994; 308:653-4.
population and obtain more accurate data on functional out- 28. Yuki N, Yamada M, Sato S, Ohama E, Kawase Y, Ikuta F, et al.
comes. Currently, there is negligible federally-funded rehabilita- Association of IgG anti-GD TM antibody with severe Guillain-Barr6
tion research into GBS. Considering that GBS research could syndrome. Muscle Nerve 1993; 16:642-7.
be utilized as a model for other disabling peripheral neuropa- 29. Kornberg AJ, Pestronik A. The clinical and diagnostic role of anti-
GM 1 antibody testing. Muscle Nerve 1994; 17:100-4.
thies and deafferent syndromes, it is an area worth exploring.
30. Cornblath DR. Electrophysiology in Guillain-Barr6 syndrome. Ann
Neurol 1990;27:S17-$20.
References 31. Asbury AK, Amason BG, Karl? HR, McFarlin DE. Criteria for
1. Alter M. The epidemiology of Guillain-Barr6 syndrome. Ann Neu- diagnosis of Guillaln-Barr6 Syndrome. Ann Neurol 1978;3:565-6.
rol 1990;27:$7-S12. 32. Guillain-Barr6 Study Group. Plasmapheresis and acute Guillain-
2. Guillain-Barr6 Syndrome Steroid Group. Double-blind trial of intra- Barr6 syndrome. Neurology 1985; 35:1096-104.
venous methyl-prednisilone in Guillain-Barr6 syndrome. Lancet 33. Osterman PO, Fagius J, Lundemo G, Pihlstedt P, Pirskanen R, Siden
1993; 341:586-90. A, et al. Beneficial effects of plasma exchange in acute inflammatory
3. McLean M, Duclos P, Jacob P, Humphreys P. Incidence of Guillain- polyradiculoneuropathy. Lancet 1984;2:1296-9.
Barr6 syndrome in Ontario and Quebec, 1983-1989, using hospital 34. French Cooperative Group on Plasma Exchange in Guillain-Barr6
service databases. Epidemiology 1994;5:443-8. syndrome. Efficiency of plasma exchange in Guillain-Barr6 syn-
4. Wirier JB, Hughes RAC, Osmond C. A prospective study of acute drome: role of replacement fluids. Ann Neurol 1987;22:753-61.
idiopathic neuropathy: clinical features and their prognostic value. 35. Vermeulen M, van der Meche FGA, Speelman JD, Weber A, Busch
J Neurol Neurosurg Psychiatry 1988; 51:605-12.
HF. Plasma and gamma-globulin infusion in chronic inflammatory
5. Raphael JC, Masson C, Morice V, Bronel D, Goulon M. Le Syn-
polyneuropathy. J Neurol Sci 1985;70:317-26.
drome de Gnillain-Barrt: etude retrospective de 233 observations.
36. van der Meche FGA, Schmitz PIM, the Dutch Guillain-Barr6 Study
Sem Hop Pares 1984;60:2543-6.
Group. N Engl J Med 1992; 326:1123-9.
6. Asbury AK. Guillaln-Barr6 syndrome: historical aspects. Ann Neu-
rol 1990;27:$2-$6. 37. Teitbaum JS, Borel CO. Respiratory dysfunction in Guillain-Barr6
7. Osler W. The principles and practice of medicine. New York: Ap- syndrome. Clin Chest Med 1994; 15:705-14.
pleton; 1892. p. 777-8. 38. Feasby TE. Inflammatory-demyelinating polyneuropathies. Neuro-
8. Guillain G, Barr6 JA, Strohl A. Sur un syndrome de radiculonevrite logic Clinics 1992; 10:651-70.
avec hyperalbuminose du liquide cephalorachidien sans reaction 39. Watts PM, Taylor WA, Hughes RAC. High-dose methylpredniso-
cellulaire: remarques sur les caracteres cliniques et graphiques des lone suppresses experimental allergic neuritis in the Lewis rat. Exp
reflexes tendineurx. Bull Soc Med Hop Paris 1916;40:1462-70. Neurol 1989; 103:101-4.
9. McKhann GM. Guillain-Barr6 syndrome: clinical and therapeutic 40. Zelig G, Ohry A, Shemsesh Y, Bar-On Z, Blumen M, Brooks ME.
observations. Ann Neurol 1990;27 Suppl:S13-S16. The rehabilitation of patients with severe Guillain-Barr6 syndrome.
10. Ropper AH. The Guillaln-Barr6 Syndrome. N Engl J Med 1992; Paraplegia 1988;26:250-4.
326:1130-6. 41. Costa EG. Rehabilitation of patients with Guillain-Barr~ syndrome.
11. McFarlin DE. Immunological parameters in Guillain-Barr6 syn- Revista De Neuro-Psiquiatra 1970; 33:219-32.
drome. Ann Neurol 1990;27 Suppl:S25-S28. 42. Mckhann GM, Griffin JW, Cornblath DR, Mellits ED, Fisher RS,
12. Asbury AK, Comhlath DR. Assessment of current diagnostic criteria Quaskey SA. Plasmapheresis and Gnillain-Barr6 syndrome: analysis
for Guillaln-Barr6 Syndrome. Ann Neurol 1990;27 Suppl:S21-S24. of prognostic factors and the effect of plasmapheresis. Ann Neurol
13. Rees JH, Soudaln SE, Gregson NA, Hughes RAC. Campylobacter 1988; 23:347-53.
jejuni infection and Guillain-Barr6 Syndrome. N Engl J Med 1995; 43. Meythaler JM, DeVivo MJ, Clausen GC, Braswell WC. Prediction
333:1374-9. of outcome in Guillain-Barr6 syndrome patients admitted to rehabil-
14. Ropper AH, Wijdicks EFM, Truax BT. Guillaln-Barr6 syndrome. itation [abstract]. Arch Phys Med Rehabil 1994;75:1027.
Philadelphia: F.A. Davis; 1991. 44. Eberle E, Brink J, Azen S, White D. Early predictors of incomplete
Arch Phys Med Rehabil Vol 78, August 1997
REHABILITATION OF GBS, Meythaler 879
recovery in children with Guillain-Barr~ polyneuritis. J Pediatrics 65. Walsh FS, Cronin M, Koblar S, Doherty P, Winer J, Leon A, et al.
1975;86:356-9. Association between glycoconjugate antibodies and campylobacter
45. Gareth PJ. Guillain-Barr~ syndrome. New York: Thieme Medical infection in patients with Guillain-Barr6 syndrome. J Neuroimmunol
Publishers; 1993. 1991;34:43-51.
46. Raman TK, Blake JA, Harris TM. Pulmonary embolism in Landry- 66. Hughes RAC, Newsom-Davis JM, Perdin GD, Pierce JM. Con-
Guillain-Strohl syndrome. Chest 1971;60:555-7. trolled trial of prednisolone in acute polyneuropathy. Lancet 1978;
47. Zochodne DW. Autonomic involvement in Guillain-Barr6 syn- 2:750-3.
drome: a review. Muscle Nerve 1994; 17:1145-55. 67. Bensman A. Strenuous exercise may impair muscle function in
48. Sedano MJ, Calleja J, Canga E, Berciano Guillain-Barr6 syndrome Guillain-Barr~ patients. JAMA 1970;214:468-9.
in Cantabria, Spain: an epidemiological and clinical study. Acta 68. Herbison GJ, Jaweed M, Dimnno JF. Exercise therapies in periph-
Neurologica Scand 1994;89:287-92. eral neuropathies. Arch Phys Med Rehabil 1983;64:201-5.
49. Taly AB, Gupta SK, Vasanth A, Suresh TG, Rao U, Nagaraja D 69. Bushbacber L. Rehabilitation of patients with peripheral neuropa-
Samy HS, et al. Critically ill Guillain-Barr6 syndrome. J Assoc thies. In: Braddom RL, editor. Physical medicine and rehabilitation.
Physicians India 1994;42:871-4. Philadelphia: W.B. Saunders; 1995. p. 972-89.
50. Ravn H. The Landry-Guillain-Barr6 syndrome: a survey and a clini- 70. Soryal I, Sinclaire E, Hornby J, Pentland B. Impaired joint mobility
cal report on 127 cases. Acta Neurol Scand 1967;43($30):8-64. in Guillain-Barr~ syndrome: a primary or a secondary phenomenon?
51. Pentland B, Daonald SM. Pain in the Guillain-Barr6 syndrome: a J Neurol Neurosurg Psychiatry 1992;55:1014-7.
clinical review. Pain 1994;59:159-64. 71. Calissi PT, Jaber LA. Peripheral diabetic neuropathy: current con-
52. Meythaler JM, Korkor AB, Nanda T, Kumar NA, Fallon M. Immo- cepts in treatment. Ann Pharmacother 1995;7-8:69-77.
bilization hypercalcemia associated with Landry-Guillain-Barr6 72. Rosner H, Rubin L, Kestenbaum A. Gabapenfin adjunctive therapy
syndrome: successful therapy with combined calcitonin and etidro-
in neuropathic pain states. Clin J Pain 1996; 12:56-8.
nate sodium. Arch Intern Med 1986; 146:1567-71.
73. Lichtenfield P. Autonomic dysfunction in the Guillain-Barr6 syn-
53. Gitter AJ, Haselkorn JK. Landry Guillain-Barr6 syndrome and het-
erotopic ossification: case report [abstract]. Arch Phys Med Rehabil drome. Am J Med 1971;50:772-80.
1990;71:823. 74. Eiben RM, Gersony WM. Recognition, prognosis and treatment of
54. Evans RA, Bridgeman M, Hills E, Dunstan CR. Immobilization the Guillain-Barr6 syndrome (acute idiopathic polyneuritis). Med
hypercalcemia. Miner Electrolyte Metab 1984; 10:244-8. Clin North Am 1963;47:1371-80.
55. Meythaler JM, DeVivo MJ, Clausen GC, Braswell WC. Anemia in 75. Winer JB, Hughes RAC. Identification of patients at risk of arrhyth-
Guillain-Barr6 syndrome patients admitted to rehabilitation [ab- mia in the Guillaln-Barrg syndrome. Q J Med 1988;68:735-9.
stract]. Arch Pbys Med Rebabil 1994; 75:1051. 76. Johnson PC, Fisher CL, Leach C. Hematological implications of
56. Hirsch GH, Menard MR, Anton HA. Anemia after traumatic spinal hypodynamic states. In: Murray RH, McCally M, editors. Hypo-
cord injury. Arch Phys Med Rehabil 1991;72:195-201. gravic and hypodynamic environments. Washington (DC): NASA;
57. Johnson PC, Fisher CL, Leach C. Hematological implications of 1971. p. 27-34.
hypodynamic states. In: Murray RI-I, McCally M, editors. Hypo- 77. Lancaster MC. Hematologic aspects of bed rest. In: Murray RH,
gravic and hypodynamic environments. Washington (DC): NASA; McCally M, editors. Hypogravic and hypodynamic environments.
1971. p. 27-34. Washington (DC): NASA; 1971. p. 299-307.
58. Lancaster MC. Hematologic aspects of bed rest. In: Murray RH, 78. Bach JR. Rehabilitation of the patient with resperatory dysfunction.
McCally M, editors. Hypogravic and hypodynamic environments. In: DeLisa JA, editor. Rehabilitation medicine: principles and prac-
Washington (DC): NASA; 1971. p. 299-307. tice. 2nd ed. Philadelphia: J.B. Lippincott; 1993. p. 952-72.
59. Low PA. Autonomic neuropathies. Curr Opin Neurol 1994; 7:402- 79. Redding GJ, Okamoto GA, Guthrie RD, Rollevson D, Milstein JM.
6. Sleep patterns in nonambulatory boys with Duchenne Muscular
60. Sridharan GV, Tallis RC, Gantman PC. Guillain-Barr~ syndrome dystrophy. Arch Phys Med Rehabil 1985;66:818-21.
in the elderly. A retrospective comparative study. Gerontology
80. Shneerson J. Disorders of ventilation. Boston: Blackwell Scientific
1993;39:170-5.
Publications; 1988.
61. Panosian MS, Quatela VC. Guillain-Barr6 syndrome presenting as
81. Smith PEM, Edwards RHT, Calverley PMA. Ventilation and
acute bilateral vocal cord paralysis. Otolaryngol Head Neck Surg
1993; 108:171-3. breathing pattern during sleep in Duchenne muscular dystrophy.
62. Nadkarni N, Lisak RP. Guillain-Barr~ syndrome with bilateral optic Chest 1989;96:1346-51.
neuritis and central white matter disease. Neurology 1993;43:842- 82. Javaheri S, Parker TJ, Wexler L, Liming JD, Lindower P, Roselle
3. GA. Effect of theophylline on sleep-disordered breathing in heart
63. Herinckx C, Deggouj N, Gersdorff M, Evrard P, Guerit JM. Guil- failure. N Engl J Med 1996;335:562-7.
lain-Barr6 syndrome and hypacusia. Acta Oto-Laryngologica Bel- 83. Alba AS. Concepts in pulmonary rehabilitation. In: Braddom RL,
gica 1995;49:63-7. editor. Physical medicine and rehabilitation. Philadelphia: W.B.
64. World Health Organization. International Classification of Impair- Saunders; 1995. p. 671-85.
ments, Disabilities, and Handicaps: a Manual of Classification Re- 84. Trojan DA, Cashman NR, Shapiro S, Tansey CM, Esdaile JM.
lating to the Consequences of Disease. Geneva: World Health Orga- Predictive factors for post-poliomyelitis syndrome. Arch Phys Med
nization; 1980. Rehabil 1994;75:770-7.
Arch Phys Med Rehabil Vol 78, August 1997
You might also like
- How Great Thou Art PDFDocument1 pageHow Great Thou Art PDFchindukNo ratings yet
- Prayer of ST Francis of Assisi (Il Signore)Document5 pagesPrayer of ST Francis of Assisi (Il Signore)galatogaNo ratings yet
- Mary Did You Know PDFDocument7 pagesMary Did You Know PDFRenz Marion AlemaniaNo ratings yet
- Holistic Health Care and WellnessDocument36 pagesHolistic Health Care and Wellnessiproamh0% (1)
- Rehabilitation in Guillian Barre SyndromeDocument6 pagesRehabilitation in Guillian Barre Syndromeanon_681345291No ratings yet
- Guillian Barré GBS Pediatrics in ReviewDocument10 pagesGuillian Barré GBS Pediatrics in ReviewJohnnathan MolinaNo ratings yet
- Ampalaya Chips With Sweet DipDocument31 pagesAmpalaya Chips With Sweet DipJayson San Juan86% (7)
- gbs4 171105053149Document71 pagesgbs4 171105053149Theresia Avila KurniaNo ratings yet
- 2018 Internal Medicine ArrhythmiasDocument24 pages2018 Internal Medicine ArrhythmiasRenz Marion AlemaniaNo ratings yet
- Ob OsceDocument13 pagesOb OsceMark Lopez100% (3)
- The Insulin Receptor and Mechanism of ActionDocument5 pagesThe Insulin Receptor and Mechanism of ActionMonica AbabeiNo ratings yet
- New Yorker MarchDocument86 pagesNew Yorker Marchloco100% (1)
- Clinical Review - FullDocument5 pagesClinical Review - FullsarandashoshiNo ratings yet
- Vital Signs Reference Chart 1.2 - 1 PDFDocument1 pageVital Signs Reference Chart 1.2 - 1 PDFSerious Leo100% (1)
- Guillain-Barre Syndrome: Practice EssentialsDocument18 pagesGuillain-Barre Syndrome: Practice EssentialsAna-Maria DuMiNo ratings yet
- Gullain Barre SindromeDocument8 pagesGullain Barre SindromeSamuel WilliamsNo ratings yet
- GbsDocument8 pagesGbszhoujNo ratings yet
- Guillen BarreDocument7 pagesGuillen BarreDouglas QuispeNo ratings yet
- Guillain-Barré Syndrome in Adults - Clinical Features and DiagnosisDocument14 pagesGuillain-Barré Syndrome in Adults - Clinical Features and DiagnosisElsyAlegríaNo ratings yet
- DR RobertDocument39 pagesDR Robertbenny christantoNo ratings yet
- Dampd 5 Manual Del Jugador EspDocument24 pagesDampd 5 Manual Del Jugador EspClaudio ReichelNo ratings yet
- p191 PDFDocument7 pagesp191 PDFdessriyaNo ratings yet
- Guillain-Barré Syndrome Literature OverviewDocument4 pagesGuillain-Barré Syndrome Literature OverviewArlentinaNo ratings yet
- Cardiovascular Complications of The Guillain-Barré Syndrome.Document4 pagesCardiovascular Complications of The Guillain-Barré Syndrome.Cocosul Cocosului CocosaruluiNo ratings yet
- Guillian BarrettDocument12 pagesGuillian BarrettOmar MadrigalNo ratings yet
- Guillain-Barré Syndrome Pediatrico 2018Document4 pagesGuillain-Barré Syndrome Pediatrico 2018Mariam Plata100% (1)
- Who Guillain Barre SyndromeDocument3 pagesWho Guillain Barre SyndromeDevaricaNo ratings yet
- An Update in Guillain-Barré Syndrome: January 2014Document7 pagesAn Update in Guillain-Barré Syndrome: January 2014Elisabeth TikalakaNo ratings yet
- Sydenham Chorea 2019Document3 pagesSydenham Chorea 2019Hajrin PajriNo ratings yet
- Guillain Barre SyndromeDocument13 pagesGuillain Barre SyndromeAdreiTheTripleANo ratings yet
- Guillain-Barre Syndrome: Practice EssentialsDocument16 pagesGuillain-Barre Syndrome: Practice EssentialsUKMBasketNo ratings yet
- Guillain-Barre Syndrome (GBS) PDFDocument13 pagesGuillain-Barre Syndrome (GBS) PDFerikafebriyanarNo ratings yet
- Laporan Kasus Tonsilofaringitis AkutDocument8 pagesLaporan Kasus Tonsilofaringitis AkutAvhindAvhindNo ratings yet
- Guillain BarreDocument12 pagesGuillain BarreerikaNo ratings yet
- Consensus: StatementDocument13 pagesConsensus: StatementElfrida FernandesNo ratings yet
- Guillain BarreDocument17 pagesGuillain Barrerk_s7No ratings yet
- Guillain-Barre Syndrome GuideDocument13 pagesGuillain-Barre Syndrome GuideUzra ShujaatNo ratings yet
- Manejo Del SGB 10 PasosDocument13 pagesManejo Del SGB 10 PasosRonald ReyesNo ratings yet
- Immunoglobulin and Monoclonal Antibodi Therapies in GbsDocument12 pagesImmunoglobulin and Monoclonal Antibodi Therapies in GbsSyafiraNo ratings yet
- BAB I JurnalDocument6 pagesBAB I JurnalRaja Fauzan FahleviNo ratings yet
- Jurnal GBSDocument15 pagesJurnal GBSfajar sugandaNo ratings yet
- Guillain-Barré Syndrome in Children: Epidemiology, Clinical Features, and DiagnosisDocument21 pagesGuillain-Barré Syndrome in Children: Epidemiology, Clinical Features, and Diagnosisgocelij948No ratings yet
- 2021_Neuromuscular Disorders in the Intensive Care UnitDocument21 pages2021_Neuromuscular Disorders in the Intensive Care UnitOlga Manco GuzmánNo ratings yet
- Guía Basada en La Evidencia. Diagnóstico Y Manejo Del Síndrome de Guillain-Barré en Diez PasosDocument20 pagesGuía Basada en La Evidencia. Diagnóstico Y Manejo Del Síndrome de Guillain-Barré en Diez PasosMichelle CortesNo ratings yet
- GBS A ReviewDocument6 pagesGBS A ReviewNurul Kartika SariNo ratings yet
- cprl1 0708Document3 pagescprl1 0708adlbrlnNo ratings yet
- Guillain Barre Syndrome and Its VariantsDocument12 pagesGuillain Barre Syndrome and Its VariantsShauki AliNo ratings yet
- Kogos JR - A Descriptive Study of Pain and Quality of Life Following Guillain-Barre Syndrome - One Year LaterDocument6 pagesKogos JR - A Descriptive Study of Pain and Quality of Life Following Guillain-Barre Syndrome - One Year LaterkarinaNo ratings yet
- 2016 Guillain Barre LancetDocument11 pages2016 Guillain Barre LancetPoly Israel Ramos ChuquimiaNo ratings yet
- AstraZeneca COVID-19 Vaccine and Guillain - Barre Syndrome in Tasmania PDFDocument5 pagesAstraZeneca COVID-19 Vaccine and Guillain - Barre Syndrome in Tasmania PDFMelissa GuerreroNo ratings yet
- Aan ?event Print&disorder - Id 935: TreatmentDocument3 pagesAan ?event Print&disorder - Id 935: TreatmentclaudiaNo ratings yet
- Miller Fisher Syndrome and Guillain-Barré Syndrome: Dual Intervention Rehabilitation of A Complex Patient CaseDocument11 pagesMiller Fisher Syndrome and Guillain-Barré Syndrome: Dual Intervention Rehabilitation of A Complex Patient CaseGeysel SuarezNo ratings yet
- GB Syndrome, Lancet 2005Document14 pagesGB Syndrome, Lancet 2005Saymin S GlezNo ratings yet
- Benzathine Penicillin G For The Management of RHDDocument8 pagesBenzathine Penicillin G For The Management of RHDDidikPrasetyoSuliNo ratings yet
- A Rare Presentation of Guillain-Barre Syndrome: Pharyngeal Cervical-Brachial VariantDocument2 pagesA Rare Presentation of Guillain-Barre Syndrome: Pharyngeal Cervical-Brachial VariantdzakiyahNo ratings yet
- Immunotherapy of Guillain-Barre Syndrome 2018Document12 pagesImmunotherapy of Guillain-Barre Syndrome 2018victorcdNo ratings yet
- Pneumoniae), Vaccines (E.g., Rabies, Tetanus, and Influenza), Lymphoma, Surgery, and TraumaDocument7 pagesPneumoniae), Vaccines (E.g., Rabies, Tetanus, and Influenza), Lymphoma, Surgery, and TraumaKenn yahweexNo ratings yet
- Gbs HarshaDocument34 pagesGbs HarsharobyanaoktvNo ratings yet
- Guil LianDocument18 pagesGuil LianPdianghunNo ratings yet
- Writing Assigmmet Lab 1 Heri Sastre. 2023Document10 pagesWriting Assigmmet Lab 1 Heri Sastre. 2023heri crackNo ratings yet
- Guillain Barre SyndromeDocument8 pagesGuillain Barre SyndromeStephanie AureliaNo ratings yet
- Guillain-Barre Syndrome Presenting With Sensory Disturbance Following A Herpes Virus Infection: A Case ReportDocument5 pagesGuillain-Barre Syndrome Presenting With Sensory Disturbance Following A Herpes Virus Infection: A Case ReportAsep MetrikaNo ratings yet
- Campylobacter Species and Guillain-Barre SyndromeDocument13 pagesCampylobacter Species and Guillain-Barre SyndromeMaximeNo ratings yet
- Ankylosing Spondylitis Review JournalDocument12 pagesAnkylosing Spondylitis Review Journaloccha_fun08100% (1)
- Education and Self-Assessment: The Epidemiology of Epilepsy: The Size of The ProblemDocument11 pagesEducation and Self-Assessment: The Epidemiology of Epilepsy: The Size of The ProblemKhalvia KhairinNo ratings yet
- ChoreaDocument6 pagesChoreamainehoonaNo ratings yet
- GBS PDFDocument9 pagesGBS PDFNur Dede Rifki FaturNo ratings yet
- GBS1Document20 pagesGBS1Yenza FaheraNo ratings yet
- 10) Guillain-Barre Syndrome, Neuroborreliosis, orDocument4 pages10) Guillain-Barre Syndrome, Neuroborreliosis, orRoxana AndreeaNo ratings yet
- Celebrate JesusDocument7 pagesCelebrate JesusRenz Marion AlemaniaNo ratings yet
- Functional Recovery After Rehabilitation For Cerebellar StrokeDocument5 pagesFunctional Recovery After Rehabilitation For Cerebellar StrokeRenz Marion AlemaniaNo ratings yet
- Pedia Charts GirlsDocument15 pagesPedia Charts GirlsRenz Marion AlemaniaNo ratings yet
- Structured Reporting of Multiphasic CT For Hepatocellular Carcinoma: Effect On Staging and Suitability For TransplantDocument9 pagesStructured Reporting of Multiphasic CT For Hepatocellular Carcinoma: Effect On Staging and Suitability For TransplantRenz Marion AlemaniaNo ratings yet
- Positron Emission Tomography in The Diagnostic Work-Up of Screening-Detected Lung NodulesDocument10 pagesPositron Emission Tomography in The Diagnostic Work-Up of Screening-Detected Lung NodulesRenz Marion AlemaniaNo ratings yet
- Patient with Eustachian Tube Dysfunction and Otitis MediaDocument5 pagesPatient with Eustachian Tube Dysfunction and Otitis MediaRenz Marion AlemaniaNo ratings yet
- Emerging Applications of Abdominal 4D Flow MRIDocument9 pagesEmerging Applications of Abdominal 4D Flow MRIRenz Marion AlemaniaNo ratings yet
- 70s Opm Pop20180419022015824 PDFDocument9 pages70s Opm Pop20180419022015824 PDFRenz Marion AlemaniaNo ratings yet
- Stay With Me Lord Ferdzmb SATB LAOmmxviii PDFDocument2 pagesStay With Me Lord Ferdzmb SATB LAOmmxviii PDFRenz Marion AlemaniaNo ratings yet
- Aleluya Verse 12, 13, 14Document1 pageAleluya Verse 12, 13, 14Renz Marion AlemaniaNo ratings yet
- Mary Did You Know PDFDocument7 pagesMary Did You Know PDFRenz Marion AlemaniaNo ratings yet
- AAP 2017 Guidelines for Childhood HypertensionDocument81 pagesAAP 2017 Guidelines for Childhood HypertensionMira Mariana UlfahNo ratings yet
- Pgi Groupings and Schedule Rotation For 2018 2019Document3 pagesPgi Groupings and Schedule Rotation For 2018 2019Renz Marion AlemaniaNo ratings yet
- Wms GINA 2018 Strategy Report V1.1 PDFDocument161 pagesWms GINA 2018 Strategy Report V1.1 PDFEdson ArmandoNo ratings yet
- On Bended Knee Boyz II Men PDFDocument9 pagesOn Bended Knee Boyz II Men PDFRenz Marion AlemaniaNo ratings yet
- Six reasons to drink warm water for health benefitsDocument17 pagesSix reasons to drink warm water for health benefitsRenz Marion AlemaniaNo ratings yet
- Health 10: (Consumer Rights and Laws)Document14 pagesHealth 10: (Consumer Rights and Laws)Clint Harvey C. BicoNo ratings yet
- NDocument136 pagesNLove HumanNo ratings yet
- Alc Intra1 Questionnaire HypertensiveDocument5 pagesAlc Intra1 Questionnaire HypertensiveAndrea Blanca100% (1)
- Pengaruh Senam Terhadap Penurunan Tekanan Darah Pada Lansia Dengan Hipertensi (Literature Review)Document15 pagesPengaruh Senam Terhadap Penurunan Tekanan Darah Pada Lansia Dengan Hipertensi (Literature Review)damarNo ratings yet
- Retraction: Retracted: Detection of Abnormal Hemoglobin Variants by HPLC Method: Common Problems With Suggested SolutionsDocument11 pagesRetraction: Retracted: Detection of Abnormal Hemoglobin Variants by HPLC Method: Common Problems With Suggested SolutionsHaziq WahidNo ratings yet
- Chelating Therapy: Azeem ImamDocument14 pagesChelating Therapy: Azeem Imamazeem imamNo ratings yet
- Mini Lecture Morphology of Skin LesionDocument48 pagesMini Lecture Morphology of Skin LesionAlkaustariyah LubisNo ratings yet
- USF Cancer BiologyDocument21 pagesUSF Cancer BiologyAmanda RelphNo ratings yet
- Boron DeficiencyDocument2 pagesBoron DeficiencyManu MandaNo ratings yet
- CUI Texto Examen Multimedia Nivel 6 Curso BasicoDocument2 pagesCUI Texto Examen Multimedia Nivel 6 Curso BasicobertoniramiroNo ratings yet
- Dc81b Colour Out of Space Ver 001Document3 pagesDc81b Colour Out of Space Ver 001Victor Guido PinheiroNo ratings yet
- Christopher, 2017 PDFDocument10 pagesChristopher, 2017 PDFsri noviyanty yusufNo ratings yet
- Management and prevention of head injuryDocument6 pagesManagement and prevention of head injuryAndreas LaseNo ratings yet
- Intracellular AccumulationDocument38 pagesIntracellular AccumulationElena PoriazovaNo ratings yet
- 1 s2.0 S0269749120365866 MainDocument10 pages1 s2.0 S0269749120365866 MainPEDRO NETO DOMINGOS SIGUIMNo ratings yet
- Gestational Hypertension and Preeclampsia ACOG Practice Bulletin, Number 222 1605448006Document24 pagesGestational Hypertension and Preeclampsia ACOG Practice Bulletin, Number 222 1605448006xibalba.edNo ratings yet
- Sirshasana: Sirsasana 001 Sirsasana 002 Sirsasana 003 Sirsasana 004Document2 pagesSirshasana: Sirsasana 001 Sirsasana 002 Sirsasana 003 Sirsasana 004Karisma SenapatiNo ratings yet
- Report of Mr. Shivam TyagiDocument1 pageReport of Mr. Shivam Tyagiakshan kambojNo ratings yet
- The Anatomy and Regulation of Cerebral Blood FlowDocument33 pagesThe Anatomy and Regulation of Cerebral Blood FlowKadek Dwipa DyatmikaNo ratings yet
- Second Announcement JASS RevisiDocument28 pagesSecond Announcement JASS RevisiPoco BlueNo ratings yet
- Thyroid Disorders in Children and AdolescentsDocument12 pagesThyroid Disorders in Children and AdolescentsCharity TololiuNo ratings yet
- Top Communicable Diseases in The Philippines 2019Document4 pagesTop Communicable Diseases in The Philippines 2019Nicole cuencosNo ratings yet
- CDC Boys 0 - 36 Mths - Length-For-AgeDocument1 pageCDC Boys 0 - 36 Mths - Length-For-AgepmverlaanNo ratings yet
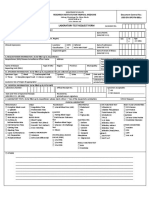
- LRD DIV SPE FM 001a RITM Lab Test Request Form - Clinical Lab 1Document1 pageLRD DIV SPE FM 001a RITM Lab Test Request Form - Clinical Lab 1Megen PLCNo ratings yet
- Data 25-01-2021 Jadwal Ujian CBT Umum Sektor Manufaktur Tahun 2020 Gelombang 2 SemarangDocument189 pagesData 25-01-2021 Jadwal Ujian CBT Umum Sektor Manufaktur Tahun 2020 Gelombang 2 SemarangArdhi Imron SholihinNo ratings yet
- Heart Rate Analysis (R)Document72 pagesHeart Rate Analysis (R)Raja LakshmiNo ratings yet