Professional Documents
Culture Documents
Hiper Inggris PDF
Uploaded by
AyaeFitriasHafinissaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hiper Inggris PDF
Uploaded by
AyaeFitriasHafinissaCopyright:
Available Formats
http://informahealthcare.
com/ceh
ISSN: 1064-1963 (print), 1525-6006 (electronic)
Clin Exp Hypertens, Early Online: 1–5
! 2013 Informa Healthcare USA, Inc. DOI: 10.3109/10641963.2013.804547
Neutrophil to lymphocyte and platelet to lymphocyte ratio
in patients with dipper versus non-dipper hypertension
Murat Sunbul1, Fethullah Gerin2, Erdal Durmus1, Tarik Kivrak1, Ibrahim Sari1, Kursat Tigen1, and Altug Cincin1
1
Department of Cardiology and 2Department of Biochemistry, Marmara University, Faculty of Medicine, Istanbul, Turkey
Abstract Keywords
Background: Neutrophil to lymphocyte ratio (NLR) and platelet to lymphocyte ratio (PLR) are
Clin Exp Hypertens Downloaded from informahealthcare.com by 78.176.66.211 on 06/20/13
Neutrophil to lymphocyte ratio, platelet to
associated with worse outcome in various diseases. Non-dipping blood pressure pattern is lymphocyte ratio, dipper, non-dipper,
associated with higher cardiovascular mortality. The aim of this study was to explore the hypertension
association between NLR and PLR in patients with dipper versus non-dipper hypertension.
Methods: The study included 166 patients with hypertension. Eighty-three patients (40 male, History
mean age: 49.1 ! 10.5 years) had dipper hypertension, while 83 patients (41 male, mean age:
52.3 ! 12.7 years) had non-dipper hypertension. Received 2 March 2013
Results: Baseline demographic characteristics were similar in both groups. Patients with non- Revised 24 March 2013
dipper hypertension had significantly higher NLR compared to dipper hypertension (2.3 ! 0.9 Accepted 27 March 2013
versus 1.8 ! 0.5, p50.001). Patients with non-dipper hypertension had significantly higher PLR Published online 20 June 2013
compared to dipper hypertension (117.7 ! 35.2 versus 100.9 ! 30.5, p ¼ 0.001). In univariate
analysis, hyperlipidemia, smoking, presence of diabetes, PLR more than 107 and NLR more than
For personal use only.
1.89 were among predictors of dipper and non-dipper status. In logistic regression analyses,
only hyperlipidemia (odds ratio: 2.96, CI: 1.22–7.13) and PLR more than 107 (odds ratio: 2.62, CI:
1.13–6.06) were independent predictors of dipper and non-dipper status. A PLR of 107 or higher
predicted non-dipper status with a sensitivity of 66.3% and specificity of 68.7%.
Conclusion: We demonstrated that patients with non-dipper hypertension had significantly
higher NLR and PLR compared to dipper hypertension, which has not been reported previously.
Moreover PLR more than 107 but not NLR was independent predictor of non-dipper status.
Introduction damage (7). Although there is usually circadian variation in
blood pressure (BP), such as more than 10% decrease in
Previous studies have shown that inflammation seems to play
systolic and diastolic BP during sleep compared to daytime
an important role in the initiation and progression of
(dipper), some hypertensive subjects who have not had this
cardiovascular diseases (1,2). White blood cell count and its
circadian variation have been entitled non-dippers. Patients
subtypes are associated with increased cardiovascular risk
with non-dipper hypertension are associated with increased
factors (3–5). The neutrophil to lymphocyte ratio (NLR) has
cardiovascular risk such as myocardial infarction (MI)
been investigated as a new predictor for cardiovascular risk
(4). NLR has emerged as an important inflammatory marker,
compared to patients with dipper hypertension. Patients 13
with non-dipper hypertension had three times the risk of
20
and high level of NLR is associated with increased mortality
atherosclerotic events than dipper hypertension (8).
in non-cardiac disorders such as some malignancies. While
The etiology of essential hypertension is multifactorial,
NLR has recently been investigated as a new predictor for
and inflammation is an important factor in the pathogenesis of
cardiovascular risk, recent studies have demonstrated that
hypertension (9). Despite the importance of non-dipper
platelet to lymphocyte ratio (PLR) is associated with major
hypertension on cardiovascular outcomes, there is not
adverse cardiovascular outcomes. Increased platelet activation
enough data whether PLR and NLR are associated with
plays a major role in the initiation and progression of
non-dipper hypertension. The aim of this study was to explore
atherosclerosis (6).
the association between NLR and PLR in patients with dipper
Hypertension is a common chronic disease and associated
versus non-dipper hypertension.
with increased risk of heart attacks, strokes and target organ
Materials and method
The investigation complies with the principles outlined in the
Correspondence: Murat Sunbul, MD, Marmara University Education and Declaration of Helsinki. The study was approved by the local
Research Hospital, Fevzi Cakmak Mahallesi, Mimar Sinan Caddesi,
No: 41, Pendik/Istanbul, Turkey. Tel: 90 506 581 90 15. Fax: 90 216 657 ethics committee, and all participants gave written informed
06 95. E-mail: drsunbul@yahoo.com.tr consent before participating.
2 M. Sunbul et al. Clin Exp Hypertens, Early Online: 1–5
Patients were selected among cases referred to cardiology Receiver operating characteristic (ROC) curve analysis was
outpatient clinic to evaluation of hypertension from performed to determine the cut-off level of PLR to predict the
November 2012 to January 2013. The study included 166 dipper versus non-dipper status. p Values less than 0.05 were
patients with essential hypertension. All patients underwent a considered statistically significant.
24-h ambulatory BP monitoring for evaluation of dipper or
non-dipper status after diagnosis of the hypertension. Results
Ambulatory BP monitoring was performed regularly every The study population was consisted of 166 consecutive
30 min during the 24-h period. The cuff was placed around patients who were diagnosed with hypertension. All patients
the non-dominant arm of the patients. Patients were ques- were divided into two groups according to status of dipper or
tioned about their sleep quality and 24-h BP assessments were non-dipper hypertension after 24-h ambulatory BP monitor-
repeated if necessary. Sleep and awake periods were assessed ing. While 83 patients had non-dipper hypertension, 83
based on the self-information of patients. Nocturnal BP patients had dipper hypertension (52.3 ! 12.7 versus
dipping was calculated as: (%) 100 # [1 $ (sleep systolic 49.1 ! 10.5, p ¼ 0.082). Baseline characteristics and clinical
BP/awake systolic BP)]. Patients with dipper hypertension data were similar in both groups (Table 1). The hemodynamic
were defined as more than 10% decrease in systolic and data of study population was shown in Table 2. While mean
diastolic BP measurements. Patients with less than 10% BP measurements were similar in both groups, heart rate
decrease in either systolic or diastolic BP were defined as value was significantly higher in patients with dipper
non-dipper hypertension (10).
Clin Exp Hypertens Downloaded from informahealthcare.com by 78.176.66.211 on 06/20/13
hypertension compared to non-dipper hypertension.
Complete blood counts, which included total white blood Laboratory findings, NLR and PLR are shown in Table 3.
cells, neutrophils, lymphocytes, and platelets were obtained at Patients with non-dipper hypertension had significantly
the time of admission. NLR and PLR were calculated as the higher NLR compared to dipper hypertension (2.3 ! 0.9
ratio of neutrophil count to lymphocyte count and as the ratio versus 1.8 ! 0.5, p50.001). Patients with non-dipper
of platelet count to lymphocyte count, respectively. All
patients were evaluated for presence of cardiovascular risk
Table 1. Baseline caharacteristics and clinical data of the study
factors such as hypertension, hyperlipidemia, diabetes population.
mellitus and smoking. Hypertension was defined as systolic
BP %140 mmHg and/or diastolic BP %90 mmHg, previously Non-dipper group Dipper group
For personal use only.
diagnosed hypertension, or use of any antihypertensive (n ¼ 83) (n ¼ 83) p
medications. Diabetes mellitus was defined as fasting Age (years) 52.3 ! 12.7 49.1 ! 10.5 0.082
plasma glucose levels more than 126 mg/dL in multiple Sex (male – n) 41 40 0.937
measurements, previously diagnosed diabetes mellitus or use Height (cm) 167.6 ! 10.3 166.1 ! 7.6 0.531
of antidiabetic medications such as oral anti-diabetic agents or Weight (kg) 76.7 ! 19.3 81.8 ! 13.9 0.253
Smoking (n) 16 21 0.351
insulin. Hyperlipidemia was defined as serum total choles- Diabetes mellitus (n) 12 10 0.642
terol %240 mg/dl, serum triglyceride %200 mg/dl, low-density Hyperlipidemia (n) 30 38 0.269
lipoprotein cholesterol %130 mg/dl, previously diagnosed
Data are expressed as mean ! SD or as number of patients.
hyperlipidemia, or use of lipid-lowering medication.
Smoking status was defined as the history of tobacco use at
admission or in the 6 months prior to visit. Patients with Table 2. Hemodynamic data of the study population.
systemic disease and using of medical treatment to affect the
white blood cell counts, such as hematopoietic system Non-dipper Dipper
group group
disorders, history of malignancies and/or treatment with (n ¼ 83) (n ¼ 83) p
chemotherapy, evidence of any concomitant inflammatory
Systolic blood pressure 128.6 ! 15.7 126.5 ! 13.1 0.355
disease, acute infection, and chronic inflammatory status, (total) – mmHg
acute coronary syndrome and percutaneous coronary inter- Systolic blood pressure 129.3 ! 15.6 130.8 ! 13.6 0.529
vention within the past 6 months, history of using the (awake) – mmHg
glucocorticoid therapy within the past 3 months, secondary Systolic blood pressure 125.6 ! 16.4 112.6 ! 11.9 50.001
(sleep) – mmHg
hypertension, heart failure, history of chronic renal or hepatic Diastolic blood pressure 80.4 ! 11.7 79.9 ! 10.3 0.778
disease and cerebrovascular disease were excluded from (total) – mmHg
the study. Diastolic blood pressure 81.8 ! 11.9 83.2 ! 11.1 0.424
(awake) – mmHg
Diastolic blood pressure 76.0 ! 11.8 69.1 ! 9.7 50.001
Statistical analysis (sleep) – mmHg
Mean blood pressure 102.4 ! 12.7 101.2 ! 10.8 0.503
Statistical analyses were performed using SPSS 20.0 statis- (total) – mmHhg
tical package for Windows (Somers, NY). Continuous data Mean blood pressure 103.6 ! 12.8 104.9 ! 11.5 0.485
(awake) – mmHg
were expressed as mean ! standard deviation, while categor- Mean blood pressure 98.8 ! 13.2 88.9 ! 10.3 50.001
ical data were presented as number of patients. Chi-square test (sleep) – mmHg
was used for comparison of categorical variables, while Pulse rate (total) – beat/min 73.0 ! 11.8 76.6 ! 10.5 0.037
student-t test was used to compare continuous variables. Pulse rate (awake) – beat/min 75.1 ! 12.3 79.3 ! 11.0 0.026
Pulse rate (sleep) – beat/min 65.9 ! 10.8 65.1 ! 9.9 0.584
Logistic regression analysis was performed to determine the
independent predictors of dipper versus non-dipper status. Data are expressed as mean ! SD.
DOI: 10.3109/10641963.2013.804547 Neutrophil and platelet to lymphocyte ratio in hypertension 3
Table 3. Comparison of laboratory findings of dipper and non-dipper
patients.
Non-dipper Dipper
group group
(n ¼ 83) (n ¼ 83) p
$3
Leukocytes (mm ) 7608 ! 1859 7825 ! 1795 0.446
Neutrophils (mm$3) 4612 ! 1397 4470 ! 1261 0.492
Lymphocyes (mm$3) 2176 ! 671 2539 ! 719 0.001
NLR 2.3 ! 0.9 1.8 ! 0.5 50.001
(neutrophil/lymphocyte ratio)
Platelets (103/mm$3) 244.2 ! 62.7 243.8 ! 62.4 0.970
PLR 117.7 ! 35.2 100.9 ! 30.5 0.001
(platelet/lymphocyte ratio)
Hemoglobin (g/dl) 13.6 ! 1.5 13.9 ! 1.5 0.245
Fasting glocose (mg/dl) 108.5 ! 46.8 97.8 ! 24.5 0.132
Creatinine (mg/dl) 0.86 ! 0.24 0.82 ! 0.28 0.393
Total cholesterol (mg/dl) 197.5 ! 51.7 212.4 ! 41.8 0.068
Triglycerides (mg/dl) 144.5 ! 80.7 149.5 ! 74.8 0.713
Low dencity lipoprotein (mg/dl) 118.4 ! 45.6 126.4 ! 38.1 0.276
High dencity lipoprotein (mg/dl) 52.0 ! 14.3 50.5 ! 14.4 0.547
2.1 ! 1.8 2.0 ! 1.3
Clin Exp Hypertens Downloaded from informahealthcare.com by 78.176.66.211 on 06/20/13
TSH (mIU/ml) 0.837
AST (U/l) 22.6 ! 11.0 20.4 ! 5.9 0.253
ALT (U/l) 22.8 ! 13.4 23.3 ! 9.7 0.840
Na (mmol/l) 140.1 ! 2.7 140.7 ! 2.4 0.240
K (mmol/l) 4.4 ! 0.5 4.4 ! 0.5 0.749
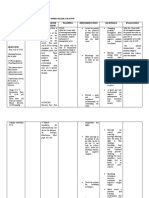
Figure 1. ROC analysis for PLR to predict non-dipper status (area under
Data are expressed as mean ! SD. curve is 0.661).
hypertension had significantly higher PLR compared to levels of endothelial progenitor cells, which play an important
dipper hypertension (117.67 ! 35.15 versus 100.89 ! 30.46, role in the endothelial homeostasis and vascular repair, was
p ¼ 0.001). In univariate analysis, hyperlipidemia, smoking,
For personal use only.
decreased in patients with non-dipper BP compared with
presence of diabetes, PLR more than 107 and NLR more than dipper hypertensive patients (17). Hypertension cause left
1.89 were among predictors of dipper and non-dipper status. ventricle hypertrophy (LVH) and diastolic dysfunction (DD).
In logistic regression analyses, only hyperlipidemia (odds Compared with dipper hypertensive patients, non-dipper
ratio: 2.96, CI: 1.22–7.13) and PLR more than 107 (odds hypertensive patients had higher incidence of LVH and DD
ratio: 2.62, CI: 1.13–6.06) were independent predictors of (18). Non dipping BP pattern was associated higher cardio-
non-dipper status. ROC analysis was performed to determine vascular mortality, poor long-term survival and autonomic
the cut-off value of PLR to predict the dipper versus non- dysfunction (19,20).
dipper status. A PLR of 107 or higher predicted non-dipper Chronic inflammation is associated with lots of chronic
status with a sensitivity of 66.3% and specificity of 68.7% disease such as malignancy, diabetes mellitus, hypertension,
(Figure 1). connective tissue disease, chronic kidney disease and coron-
ary artery disease (21–24). White blood cell count, C reactive
Discussion protein and neutrophil lymphocyte ratio (NLR) are some of
In this study, we demonstrated that patients with non-dipper the predictors of chronic inflammation. Leukocytes play a
hypertension had significantly higher NLR and PLR com- major role in inflammatory processes. Neutrophils are the
pared to dipper hypertension. Moreover, PLR more than 107 most abundant type of the white blood cells. They take
but not NLR was independent predictors of non-dipper status. important roles in inflammatory response. Neutrophils are the
Clinical use of 24-h ambulatory BP monitoring gives first cells responding to inflammation especially due to
information about BP during the night. BP falling during the bacterial infection, cancer and environmental exposure.
night time compared with day time, which is more than 10%, They release many kinds of cytokines and activate other
is called as dipper BP pattern. If BP drop is less than 10%, it is cells of the immune system to trigger and amplify inflam-
called non-dipper BP pattern (11). Non-dipper BP pattern is matory reactions. The relationship between white blood cell
always associated with autonomic dysfunction. count and increased cardiovascular risk is well known. NLR,
Endocrinologic disorders such as hypercortisolism (12), which can be derived from the white blood cell count is an
pheochromocytoma, sleep apnea syndrome (13) and chronic inexpensive, routinely used, reproducible test and has shown
kidney disease (14) may be associated with non-dipper up as a marker of systemic inflammatory response. Previous
hypertension. Non-dipper BP pattern has been proven to be studies have shown that NLR is associated with poor clinical
associated with target end-organ damages and increased outcomes in cardiac diseases and several malignancies
cardiovascular mortality (15). Adverse effects of non-dipper (25,26). Kruk et al. showed that increased level of inflam-
BP pattern on cardiovascular risk were observed independent mation was associated with poor prognosis in coronary artery
of BP level that was normal or higher than normal limits (16). disease (27). NLR is a parameter that gives us information not
Adverse effect of non-dipper BP may be related with only about the systemic inflammation but also the stress
endothelial damage. In a previous study, it was shown that response of the patient. While mainly high neutrophil counts
4 M. Sunbul et al. Clin Exp Hypertens, Early Online: 1–5
reflect to inflammation, low lymphocyte counts reflect poor revascularisation. A systematic review on more than 34 000
subjects. Thromb Haemost 2011;106:591–9.
general health and physiologic stress (28). Blood NLR is an 4. Tamhane UU, Aneja S, Montgomery D, et al. Association between
indicator of the overall inflammatory and stress status of the admission neutrophil to lymphocyte ratio and outcomes in patients
body, and an alteration in NLR may be found in hypertensive with acute coronary syndrome. Am J Cardiol 2008;102:653–7.
patients. Recently published trials established that NRL was 5. Uthamalingam S, Patvardhan EA, Subramanian S, et al. Utility of
the neutrophil to lymphocyte ratio in predicting long-term
associated with increased mortality and poor prognosis in
outcomes in acute decompensated heart failure. Am J Cardiol
acute coronary syndromes especially ST segment elevation 2011;107:433–8.
MI (29). NRL was also increased in patients with diabetes 6. Tsiara S, Elisaf M, Jagroop IA, Mikhailidis DP. Platelets as
mellitus and hypertension. NLR can be a useful and cost- predictor of vascular risk: is there a practical index of platelet
effective method to evaluate inflammatory state. activity? Clin Appl Thromb Hemost 2003;9:177–90.
7. Kannel WB. Blood pressure as a cardiovascular risk factor:
Previous studies have demonstrated that higher platelet and prevention and treatment. JAMA 1996;275:1571–6.
lower lymphocyte counts were associated with adverse 8. Seo HS, Kang TS, Park S, et al. Non-dippers are associated with
cardiovascular outcomes. Azab et al. showed that higher adverse cardiac remodeling and dysfunction. In J Cardiol 2006;112:
value of PLR as a marker of long-term mortality in patients 171–7.
9. Turak O, Ozcan F, Tok D, et al. Serum uric acid, inflammation, and
with non-ST segment elevation MI (30). In patients with nondipping circadian pattern in essential hypertension. J Clin
various malignancies such as ovarian cancer and pancreatic Hypertens (Greenwich) 2013;15:7–13.
ductal adenocarcinoma, it has been demonstrated that eleva- 10. Pickering TG. The clinical significance of diurnal blood pressure
tion of neutrophils, platelets, NLR or PLR were associated variations. Dippers and nondippers. Circulation 1990;81:700–2.
Clin Exp Hypertens Downloaded from informahealthcare.com by 78.176.66.211 on 06/20/13
11. Birkenhäger AM, van den Meiracker AH. Causes and consequences
with some adverse clinico-pathologic events (31,32). of a non-dipping blood pressure profile. Neth J Med 2007;65:
Although the association between NLR and cardiovascular 127–31.
disease has been demonstrated in numerous studies, the 12. Zacharieva S, Orbetzova M, Stoynev A, et al. Circadian blood
association between PLR and cardiovascular diseases pressure profile in patients with Cushing’s syndrome before and
after treatment. J Endocrinol Invest 2004;27:924–30.
remained unclear except a few clinical studies (30,33). To 13. Sasaki N, Ozono R, Yamauchi R, et al. Age-related differences in
date, there is no study investigating the relationship between the mechanism of nondipping among patients with obstructive
PLR and dipper versus non-dipper status. Our study, for the sleep apnea syndrome. Clin Exp Hypertens 2012;34:270–7.
first time demonstrated that PLR was not only higher in the 14. Liu M, Takahashi H, Morita Y, et al. Non-dipping is a potent
predictor of cardiovascular mortality and is associated with
non-dipper group than the dipper group it also emerged as an autonomic dysfunction in haemodialysis patients. Nephrol Dial
For personal use only.
independent predictor of non-dipper status. In a recent study, Transplant 2003;18:563–9.
Demir (34) showed for the first time that patients with non- 15. Mancia G, Parati G. The role of blood pressure variability in end-
dipper hypertension had higher NLR compared with dipper organ damage. J Hypertens Suppl 2003;21:S17–23.
16. Hermida RC, Ayala DE, Mojón A, Fernández JR. Blunted sleep-
patients. However, the number of sample size was smaller in time relative blood pressure decline increases cardiovascular risk
his study and he did not report whether NLR was an independent of blood pressure level – the ‘‘Normotensive
independent predictor of non-dipper status (34). Non-dipper’’ paradox. Chronobiol Int 2013;30:87–98.
17. Kim S, Kim NH, Kim YK, et al. The number of endothelial
Study limitations progenitor cells is decreased in patients with non-dipper hyperten-
sion. Korean Circ J 2012;42:329–34.
Our study had some limitations. One of them was the small 18. Ersoylu ZD, Tuğcu A, Yildirimtürk O, et al. Comparison of the
sample size. We were also not able to evaluate the prognostic incidences of left ventricular hypertrophy, left ventricular diastolic
dysfunction, and arrhythmia between patients with dipper and non-
value of the NLR and PLR in patients with hypertension. Our dipper hypertension. Turk Kardiyol Dern Ars 2008;36:310–17.
study had a cross-sectional design, and it would be better if 19. Liu M, Takahashi H, Morita Y, et al. Non-dipping is a potent
we had followed the patients and explore the relation between predictor of cardiovascular mortality and is associated with
adverse cardiac events and NLR and/or PLR in these patients. autonomic dysfunction in haemodialysis patients. Nephrol Dial
Transplant 2003;18:563–9.
20. Ino-Oka E, Yumita S, Sekino H, et al. The effects of physical
Conclusions activity and autonomic nerve tone on the daily fluctuation of blood
pressure. Clin Exp Hypertens 2004;26:129–36.
We demonstrated that patients with non-dipper hypertension 21. Lee S, Choe JW, Kim HK, Sung J. High-sensitivity C-reactive
had significantly higher NLR and PLR compared to dipper protein and cancer. J Epidemiol 2011;21:161–8.
hypertension. Moreover, PLR more than 107 but not NLR was 22. Pitsavos C, Tampourlou M, Panagiotakos DB, et al. Association
between low-grade systemic inflammation and type 2 diabetes
independent predictors of non-dipper status. mellitus among men and women from the ATTICA study.
Rev Diabet Stud 2007;4:98–104.
Declaration of interest 23. Okyay GU, Inal S, Oneç K, et al. Neutrophil to lymphocyte ratio in
evaluation of inflammation in patients with chronic kidney disease.
The authors report no conflicts of interest. The authors alone Ren Fail 2013;35:29–36.
are responsible for the content and writing of this article. 24. Torun D, Ozelsancak R, Yiğit F, Micozkad|oğlu H. Increased
inflammatory markers are associated with obesity and not with
target organ damage in newly diagnosed untreated essential
References hypertensive patients. Clin Exp Hypertens 2012;34:171–5.
25. Tamhane UU, Aneja S, Montgomery D, et al. Association
1. Ross R. Atherosclerosis – an inflammatory disease. N Engl J Med
between admission neutrophil to lymphocyte ratio and outcomes
1999;340:115–26.
in patients with acute coronary syndrome. Am J Cardiol 2008;102:
2. Libby P. What have we learned about the biology of atheroscler-
653–7.
osis? The role of inflammation. Am J Cardiol 2001;88:3J–6J.
26. Halazun KJ, Aldoori A, Malik HZ, et al. Elevated preoperative
3. Guasti L, Dentali F, Castiglioni L, et al. Neutrophils and clinical
neutrophil to lymphocyte ratio predicts survival following hepatic
outcomes in patients with acute coronary syndromes and/or cardiac
DOI: 10.3109/10641963.2013.804547 Neutrophil and platelet to lymphocyte ratio in hypertension 5
resection for colorectal liver metastases. Eur J Surg Oncol 2008;34: elevation myocardial infarction. J Thromb Thrombolysis 2012;34:
55–60. 326–34.
27. Kruk M, Przyłuski J, Kalińczuk Ł, et al. Association of non-specific 31. Asher V, Lee J, Innamaa A, Bali A. Preoperative platelet
inflammatory activation with early mortality in patients with lymphocyte ratio as an independent prognostic marker in ovarian
ST-elevation acute coronary syndrome treated with primary cancer. Clin Transl Oncol 2011;13:499–503.
angioplasty. Circ J 2008;72:205–11. 32. Bhatti I, Peacock O, Lloyd G, et al. Preoperative hematologic
28. Gibson PH, Cuthbertson BH, Croal BL, et al. Usefulness of markers as independent predictors of prognosis in resected
neutrophil/lymphocyte ratio as predictor of new-onset atrial fibril- pancreatic ductal adenocarcinoma: neutrophil-lymphocyte versus
lation after coronary artery bypass grafting. Am J Cardiol 2010; platelet-lymphocyte ratio. Am J Surg 2010;200:197–203.
105:186–91. 33. Erdem K, Ayhan S, Ozturk S, et al. Usefulness of the mean platelet
29. Park JJ, Jang HJ, Oh IY, et al. Prognostic value of neutrophil to volume for predicting new-onset atrial fibrillation after isolated
lymphocyte ratio in patients presenting with ST-elevation myocar- coronary artery bypass grafting. Platelets 2013. [Epub ahead of
dial infarction undergoing primary percutaneous coronary inter- print]. doi:10.3109/09537104.2013.767443.
vention. Am J Cardiol 2013;111:636–42. 34. Demir M. The relationship between neutrophil lymphocyte ratio
30. Azab B, Shah N, Akerman M, McGinn Jr JT. Value of platelet/ and nondipper hypertension. Clin Exp Hypertens 2013. [Epub
lymphocyte ratio as a predictor of all-cause mortality after non-ST- ahead of print]. doi:10.3109/10641963.2013.764893.
Clin Exp Hypertens Downloaded from informahealthcare.com by 78.176.66.211 on 06/20/13
For personal use only.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- 1 SMDocument8 pages1 SMNadya AgithaNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- 1 SMDocument8 pages1 SMNadya AgithaNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hiper InggrisDocument5 pagesHiper InggrisAyaeFitriasHafinissaNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Jurnal HipertensiDocument9 pagesJurnal HipertensiAyaeFitriasHafinissaNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Bahasa IndonesiaDocument9 pagesBahasa Indonesiananda adiNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- SCDocument13 pagesSCPerawatSpasiSusanaNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Jurnal HipertensiDocument9 pagesJurnal HipertensiAyaeFitriasHafinissaNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Hiper InggrisDocument5 pagesHiper InggrisAyaeFitriasHafinissaNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Clinical Classification of Pulmonary Hipertension PDFDocument8 pagesClinical Classification of Pulmonary Hipertension PDFRaras MayangNo ratings yet
- Clinical Classification of Pulmonary Hipertension PDFDocument8 pagesClinical Classification of Pulmonary Hipertension PDFRaras MayangNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Journal MidlifeDocument10 pagesJournal MidlifeAyaeFitriasHafinissaNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- PH PDFDocument58 pagesPH PDFjosephiraNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hiper InggrisDocument5 pagesHiper InggrisAyaeFitriasHafinissaNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- JurnalDocument11 pagesJurnalAyaeFitriasHafinissaNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Jurnal Kanker AnakDocument8 pagesJurnal Kanker AnakAyaeFitriasHafinissaNo ratings yet
- Hiper InggrisDocument5 pagesHiper InggrisAyaeFitriasHafinissaNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Journal MidlifeDocument10 pagesJournal MidlifeAyaeFitriasHafinissaNo ratings yet
- JurnalDocument11 pagesJurnalAyaeFitriasHafinissaNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Health Checklist: NG:) Lumunok)Document2 pagesHealth Checklist: NG:) Lumunok)Rose Duron GumaNo ratings yet
- Astrazenica 2nd Dose 8-13-21 AlkieDocument109 pagesAstrazenica 2nd Dose 8-13-21 AlkieGanie Mar BiasonNo ratings yet
- European University of Lefke: Eczacılık Fakültesi / Faculty of PharmacyDocument3 pagesEuropean University of Lefke: Eczacılık Fakültesi / Faculty of PharmacyMariem Ben HediaNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Pediatric AnesthesiaDocument70 pagesPediatric AnesthesiaEliyan KhanimovNo ratings yet
- Icd X: Diagnose ICD Diagnosa ICDDocument33 pagesIcd X: Diagnose ICD Diagnosa ICDannisa statiraNo ratings yet
- Helping Psychiatry Residents Cope With Patient SuicideDocument5 pagesHelping Psychiatry Residents Cope With Patient SuicidedrguillermomedinaNo ratings yet
- Lecture 3 PsychopharmacologyDocument99 pagesLecture 3 PsychopharmacologyPavan chowdaryNo ratings yet
- Chronic MegacolonDocument3 pagesChronic Megacolondrnareshkumar3281No ratings yet
- Female Sexual DysfunctionDocument18 pagesFemale Sexual DysfunctionRisky SetiawanNo ratings yet
- The Uses and Limitations of The Fetal Biophysical Profile.Document18 pagesThe Uses and Limitations of The Fetal Biophysical Profile.Diego Ortecho100% (1)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- 01-2020 - Tactical Emergency Casualty Care (TECC)Document5 pages01-2020 - Tactical Emergency Casualty Care (TECC)pibulinNo ratings yet
- Bochdalek Hernia - Wikipedia, The Free Encyclopedia PDFDocument5 pagesBochdalek Hernia - Wikipedia, The Free Encyclopedia PDFMilda InayahNo ratings yet
- Aron FinalDocument70 pagesAron FinalJaime Pastrana Jr.No ratings yet
- PARM LBP CPG 2nd Edition 2017 PDFDocument293 pagesPARM LBP CPG 2nd Edition 2017 PDFGumDropNo ratings yet
- Dengue Outbreak Declared in CaviteDocument5 pagesDengue Outbreak Declared in CaviteDoc AlexNo ratings yet
- Inroduction To Homoeopathic Materia Medica 2023Document10 pagesInroduction To Homoeopathic Materia Medica 2023mahitha sujithNo ratings yet
- CONJUNCTIVITIS or Pink Eye, Emotional and Spiritual MeaningDocument1 pageCONJUNCTIVITIS or Pink Eye, Emotional and Spiritual MeaningSarah g.No ratings yet
- FHSISDocument15 pagesFHSISThon Lopez MagpantayNo ratings yet
- Group 5 - Case Study Presentation PDFDocument7 pagesGroup 5 - Case Study Presentation PDFAkash HalsanaNo ratings yet
- Gastritis CronicaDocument12 pagesGastritis CronicaKati RondonNo ratings yet
- Bromocriptine Tablet Product LeafletDocument6 pagesBromocriptine Tablet Product Leafletadam malikNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 3 NURSING-CARE-PLAN FinaaalDocument7 pages3 NURSING-CARE-PLAN FinaaalSam PothNo ratings yet
- ID-IM-SQ-E ToolDocument9 pagesID-IM-SQ-E TooltriciacamilleNo ratings yet
- How To Prepare For ExamDocument4 pagesHow To Prepare For ExamJaspreet KaurNo ratings yet
- S Tahel 2005Document12 pagesS Tahel 2005Catherine MorrisNo ratings yet
- Introduction To Cerebral Palsy 2022Document53 pagesIntroduction To Cerebral Palsy 2022Namakau MuliloNo ratings yet
- Participant Final Exam Answer Sheet: Emergency First Response Primary Care (CPR)Document2 pagesParticipant Final Exam Answer Sheet: Emergency First Response Primary Care (CPR)Zirak Maan HussamiNo ratings yet
- OTC and PRESCRIPTION DRUGS Ppt. (TANTICO)Document10 pagesOTC and PRESCRIPTION DRUGS Ppt. (TANTICO)Ladyfair TanticoNo ratings yet
- LewisDocument12 pagesLewisLewis Nimsy Tunde100% (1)
- Ludwig Heinrich Bojanus (1776-1827) On Gall's Craniognomic System, Zoology - UnlockedDocument20 pagesLudwig Heinrich Bojanus (1776-1827) On Gall's Craniognomic System, Zoology - UnlockedJaime JaimexNo ratings yet
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (2)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (28)