Professional Documents
Culture Documents
Hyponatremia Review. Clinician's Brief: January 2010
Uploaded by
david alonsoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hyponatremia Review. Clinician's Brief: January 2010
Uploaded by
david alonsoCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/260122444
Hyponatremia review. Clinician's Brief
Article · January 2010
CITATIONS READS
0 1,606
1 author:
Cristina Pérez Vera
Tierklinik Aarau West
15 PUBLICATIONS 153 CITATIONS
SEE PROFILE
All content following this page was uploaded by Cristina Pérez Vera on 11 February 2014.
The user has requested enhancement of the downloaded file.
Consultant on Call INTERNAL MEDICINE
Cristina Perez Vera, DVM, &
Sally Bissett, BVSc, MVSc, Diplomate ACVIM,
North Carolina State University
Hyponatremia
PROFILE
Definition
Hyponatremia is defined as a plasma sodium (Na+) concentration < 140 mEq/L in dogs
and 150 mEq/L in cats.1 Because plasma Na+ concentration is the main determinant of
plasma osmolality (Posm), hyponatremia usually reflects hypoosmolality. Since the kid-
neys are highly efficient in excreting water, hypoosmolality almost always implies a
defect in renal water excretion and excess of water in the body due to one of the
following mechanisms:
● Impaired diluting ability in the loop of Henle and distal tubule (volume depletion,
renal failure, diuretics)
● Increased collecting-tubule permeability due to the presence of antidiuretic hormone
(ADH) (effective circulating volume depletion, inappropriate ADH secretion, pain,
adrenal insufficiency, or hypothyroidism)
CONTINUES
ADH = antidiuretic hormone; Na+ = sodium; Posm = plasma osmolality
Consultant on Call / NAVC Clinician’s Brief / February 2010 ................................................................................................................................................................49
Consultant on Call CONTINUED
KEY WORDS
Signalment Pathophysiology: Why is there too
Na+ concentration: Reflects the Hyponatremia is a common electrolyte disor- much water?
content of sodium relative to der occurring in a broad spectrum of patients, Body fluid balance depends largely on the
the volume of water in the from ones without clinical signs to the criti- interrelationship of salt and water. Although
body, not total sodium content. cally ill. effective circulating volume is largely con-
Therefore, hyponatremic trolled by sodium balance, maintaining osmo-
patients can have decreased, Causes lality depends on regulation of water balance
increased, or normal total The principal causes of hyponatremia are: (Table 1).
sodium content. ● Disorders associated with impaired renal ● Na+ balance: Several sensors in the body
Na+ content: Reflects the total water excretion (more common): detect changes in extracellular fluid vol-
amount of sodium in ◗ Volume depletion ume (which is largely determined by total
extracellular fluid and is • Extrarenal losses: Gastrointestinal dis- sodium content).
calculated by multiplying the orders (vomiting, diarrhea); third-space ● Water balance: Although extracellular fluid
concentration of sodium by the disorders (pancreatitis, peritonitis) and intracellular fluid have different com-
volume of extracellular fluid. • Renal losses: Diuretic therapy (thiazide), positions, they must maintain the same
Osmolality: Concentration of osmotic diuresis (glucose, mannitol), tonicity. The balance is sensed and con-
osmotically active particles in a advanced renal failure (decreased trolled by thirst and osmoregulation sys-
solution. glomerular filtration rate) tems. Osmoreceptors of the hypothalamus
• Plasma osmolality (Posm) is • Edematous states: Congestive heart fail- and neurohypophysis are sensitive to alter-
the main determinant of ure, liver disease, nephrotic syndrome ations in plasma osmolality and hydro-
water distribution in the body. ◗ ADH excess: static pressure; they respond to plasma
Because water can move • Inappropriate ADH secretion hypertonicity by increasing thirst and
freely across almost all cell (SIADH) ADH secretion. When the osmolality is
membranes, the osmolalities • Mineralocorticoid deficiency low, ADH secretion is suppressed and
of intracellular and • Hypothyroidism urine is diluted.
extracellular fluids are the ● Disorders associated with normal renal
same. water excretion: Signs
◗ Excessive water intake (primary Depending on the severity of hyponatremia,
• Normal plasma osmolality
polydipsia) patients may have no clinical signs or present
ranges from 290 to 310
◗ Reset osmostat syndrome with varying degrees of neurologic signs.
mOsm/kg in dogs and 290 to
◗ Rapid infusion of hypotonic fluids Cerebral edema and water intoxication occur
330 mOsm/kg in cats.
● Disorders associated with pseudohypona- as serum sodium concentration decreases, and
Posm = 2 × Na+ + glucose/18 +
tremia or translocational hyponatremia: the osmotic gradient that develops makes
BUN/2.8
◗ Hyperlipidemia water move into the brain. Typical neurologic
• The contributions of glucose ◗ Hyperproteinemia signs include the following:
and BUN to Posm are ◗ Hyperglycemia ● Lethargy
normally small, except in ● Irritability
diabetes mellitus and renal Risk Factors ● Nausea/vomiting
failure. Urea can freely cross There are currently no reports of risk factors ● Mental dullness or depression
cell membranes; its for hyponatremia in dogs and cats, but serum ● Stupor
contribution to Posm can be Na+ concentration should be measured in ● Seizures
excluded: small animals with: ● Coma
Effective Posm = ● Suspected hypoadrenocorticism
measured Posm – BUN/2.8 ● Vomiting and diarrhea Clinical signs related to the underlying cause
Tonicity: Osmotic pressure of a ● Diuretic use of the hyponatremia may also be present:
solution. It determines the ● Effusive disorders ● Tachycardia
ability of a solution to move ● Polyuria and polydipsia ● Hypotension
across a membrane. ● Abnormal mental status or behavior ● Prolonged capillary refill time
● Seizures ● Weakness
Na+ expressed as mEq/L; glucose
● Ascites
expressed as mg/dL; BUN expressed
as mg/dL ● Edema
50 ................................................................................................................................................................NAVC Clinician’s Brief / February 2010 / Consultant on Call
Table 1. Regulation of Body Fluid Balance
Water Balance Na+ Balance (Volume Regulation)
Signal Plasma osmolality Effective circulating volume
Sensors Hypothalamic osmoreceptors • Baroreceptors of the aorta, carotid sinus, and
afferent glomerular arteriole
• Atrial distension
Effectors Antidiuretic hormone • Sympathetic nervous system
• Renin-angiotensin aldosterone system
• Atrial natriuretic peptide
• Antidiuretic hormone
• Pressure natriuresis
Response • Water excretion (via antidiuretic Na+ excretion
hormone)
• Water intake (via thirst)
ties on T2-weighted scans, which represent an
DIAGNOSIS increase in water density associated with
inflammation, gliosis, edema, or necrosis.
Definitive Diagnosis Central nervous system lesions may not
● Hyponatremia: Serum Na+ concentration always be visible on MRI early in the course
< 140 mEq/L in dogs or < 150 mEq/L in of neurologic disease.
cats.
● Neurologic signs are not usually seen unless Clinical Approach
Na+ concentrations are < 120 mEq/L in dogs If the cause of hyponatremia is not readily appar-
or < 130 mEq/L in cats. However, the devel- ent (also see Diagnostic Tree: Hyponatremia,
opment of neurologic signs is also related to page 55):
rapidity of onset of hyponatremia. In chronic ● Evaluate blood sample for lipemia and meas-
disorders, the signs are more subtle and non- ure plasma protein concentration to rule out ADH = antidiuretic hormone;
BUN = blood urea nitrogen:
specific because the brain has had enough pseudohyponatremia. Lipemia and hyperpro- MRI = magnetic resonance
time to adapt to plasma hypotonicity. teinemia underestimate Na+ concentration imaging; Na+ = sodium; SIADH
= syndrome of inappropriate
when flame photometry is used, but this does
antidiuretic hormone secretion
Laboratory Findings & Imaging not happen with ion-selective electrode tech-
● Laboratory data should ideally include plasma niques. Plasma osmolality is normal because
osmolality, Na+, potassium, chloride, bicarbon- lipids and proteins contribute little to plasma
ate, BUN, and glucose concentrations, and, osmolality.
where necessary, urine Na+ concentration and ● Measure glucose concentration to rule out
osmolality and venous or arterial pH (see translocational hyponatremia. The following
Clinical Approach). formula can be used to correct sodium in the
● MRI (after rapid correction of hyponatremia presence of hyperglycemia:
and myelinolysis):2,3 Extrapontine lesions are Corrected Na+ = Measured Na+ +
most common, especially lesions within the 1.6 [(Serum glucose - 100)/100]
thalamus. The lesions are described as nonen-
hancing, symmetrical increased signal intensi- CONTINUES
Consultant on Call / NAVC Clinician’s Brief / February 2010 ................................................................................................................................................................51
Consultant on Call CONTINUED
● Measure or calculate Posm, other electrolytes, ● Volume-depleted patients require inpatient
and urea concentrations with or without pH: management with IV fluids.
◗ Posm < 290 mOsm/kg confirms hypoosmo- ● Normovolemic or edematous patients may be
lality. However, increased BUN may cause able to be managed as outpatients.
FIND MORE plasma osmolality to be normal or high
while the effective osmolality is reduced. Medical
A case study ◗ Metabolic alkalosis and hypokalemia sug- ● Two basic goals of therapy for hyponatremia:
addressing
treatment for
gest vomiting or diuretic use. ◗ Treat underlying cause
hyponatremia ◗ Metabolic acidosis and hyperkalemia sug- ◗ Increase plasma Na+ concentration at a safe
in a dog with gest Addison’s disease or gastrointestinal rate
lethargy, disease (eg, trichuriasis) when renal func- ● In general, hyponatremia is corrected by giv-
vomiting, and
diarrhea can
tion is normal. ing Na+ to patients who have extracellular
be viewed at ● Measure urine osmolality (Uosm) to determine fluid volume depletion and by restricting
whether water excretion is normal or impaired. sodium in patients who are hyponatremic but
cliniciansbrief.com The normal response to hyponatremia is to normovolemic or edematous (eg, sodium-
>>Go to Journal suppress ADH secretion, resulting in maxi- retaining states, such as congestive heart fail-
Extras on our mally dilute urine (< 100 mOsm/kg or urine ure, cirrhosis, and nephrotic syndrome).
homepage.
specific gravity < 1.003).
◗ Hyponatremia with Posm and Uosm Rate of Correction
< 100 mOsm/kg (ADH suppression) ● Ideally, the rate of correction should be similar
suggests primary polydipsia. to that at which hyponatremia developed. For
● Measure urine Na+ concentration (Una) to example, acute (< 24–48 hours’ duration)
differentiate volume depletion and SIADH hyponatremia with clinical signs should be
when urine osmolality is high. treated aggressively to reverse cerebral edema.
◗ Una should be < 20 mEq/L with hypovolemia. However, most patients develop hyponatremia
◗ Una should be > 20 mEq/L with Addison’s over 2 or more days (chronic hyponatremia), a
disease, diuretic therapy, or SIADH. While situation in which the brain has had time to
SIADH is a common cause of hypona- adapt to hypoosmolarity. Under these circum-
tremia in humans, it is rarely described in stances a conservative approach of no more
veterinary patients. than 0.5 mEq/L per hour or 10 mEq/L per
● Perform a fecal examination to rule out gas- day of sodium replacement is generally recom-
trointestinal parasitism.4 mended to avoid rapid correction of
● Consider an ACTH stimulation test to rule sodium.1,2,6
out Addison’s disease. Hypoadrenocorticism ● Rapid correction of chronic hyponatremia
leads to urinary loss of sodium chloride, vol- (generally > 15 mEq Na/L per day) can lead
ume depletion, and ADH release. As many as to a neurologic disorder called demyelinating
81% of dogs with hypoadrenocorticism are encephalopathy, or myelinolysis. The mecha-
hyponatremic at presentation.5 nism is not clear, but brain cells adapted to
● Consider measurement of T4 and/or TSH. hyponatremia may be at particular risk. Clini-
Myxedema coma due to hypothyroidism may cal signs typically develop 3 to 4 days after
cause hyponatremia in people and dogs, possi- correction of hyponatremia and are character-
bly because of ADH release secondary to ized by paraparesis or tetraparesis, dysphagia,
decreased cardiac output and decreased coma, and seizures.1–3
glomerular filtration rate (rare).6,7 ● In correcting severe hyponatremia, formulas
may be helpful, but serum Na+ concentrations
TREATMENT should be measured frequently (eg, every 3–6
hours) and therapy adjusted accordingly.
Inpatient or Outpatient ● Conventional crystalloid solutions are gener-
● Patients with neurologic signs or severe ally recommended for correcting hypovolemic
hyponatremia should be treated in an inten- hyponatremic patients. Table 2 provides the
sive care unit.
52 ................................................................................................................................................................NAVC Clinician’s Brief / February 2010 / Consultant on Call
Table 2. Na+ Content & Main Composition of Various Crystalloid Fluids
Fluid Na+ Cl K Ca Mg Dextrose (%) Buffer Osmolality
7.5% NaCl 1283 1283 - - - - - 2567
0.9% NaCl 154 154 - - - - - 308
Normosol-R (hospira.com) 140 98 5 - 3 - 27 acetate 294
23 gluconate
Lactated Ringer’s solution 130 109 4 3 - - 28 lactate 272
2.5% dextrose in 0.45% NaCl 77 77 - - - 2.5 - 280
0.45% NaCl 77 - - - - - 155
Normosol-M (hospira.com) 40 40 13 - 3 5 16 acetate 364
Dextrose 5% (D5W) - - - - - 5 - 253
Ions & buffers are expressed as mEq/L; osmolality is expressed as mOsmol/L
Ca = calcium; Cl = chloride; k = potassium; Mg = magnesium; Na+ = sodium
main composition of several crystalloid fluids. at cliniciansbrief.com). Therapy is then
● The degree to which a given fluid will adjusted on the basis of serial serum Na+
increase serum Na+ can be estimated by using concentrations.
the following formula (infusate Na+ = Na+
concentration of the corrective fluid): IN GENERAL
∆ Serum Na+ =
Infusate Na+ – Serum Na+/TBW + 1 Relative Cost
● The amount of sodium required (sodium The cost of investigating and treating hypona-
deficit) can also be estimated by using the tremia depends on the cause and severity. If the Cost Key
following formula: patient has no clinical signs and underlying dis-
$ = < $100
∆ Na+ deficit = TBW × (desired Na+ – actual Na+) ease is treatable, the treatment may be relatively
$$ = $100–$250
● Unfortunately, the above formulas are only inexpensive ($$–$$$$). However, if the patient is
$$$ = $250–$500
estimates and do not account for the effect of showing neurologic signs, has severe hypona-
$$$$ = $500–$1000
concurrent potassium administration (which tremia, or needs intensive care because of the
will increase serum Na+ because of extracellu- underlying disease process, the cost will be much $$$$$ = > $1000
lar movement), the effect volume replacement higher ($$$$$).
has on ADH secretion, or ongoing fluid
losses. Prognosis & Course
● In general, for most patients with chronic Outcome depends on the cause of hyponatremia
hyponatremia and hypovolemia, the initial and the presence of neurologic signs. Many
fluid type and volume administered are based patients without clinical signs have an excellent
on the severity of hyponatremia, degree of prognosis, whereas patients with acute severe
volume depletion, estimated ongoing losses, hyponatremia that display neurologic signs
and maintenance fluids; the goal is a Na+ cor- (either before or during treatment) will have a
rection rate less than 0.5 mEq/kg per hour. At prognosis from good to guarded.
our institution, this usually results in the con-
current administration of maintenance (hypo- See Aids & Resources, back page, for references
tonic) and replacement (relatively isotonic) and suggested reading.
crystalloid solutions (Case Study available
ACTH = adrenocorticotropic hormone; ADH = antidiuretic hormone; BUN = blood urea nitrogen; Na+ = sodium; Posm = plasma
osmolality; SIADH = syndrome of inappropriate antidiuretic hormone secretion; T4 = thyroxine; TBW = total body weight;
TSH = thyroid-stimulating hormone; Una = urine concentration; Uosm = urine osmolality
Consultant on Call / NAVC Clinician’s Brief / February 2010 ................................................................................................................................................................53
View publication stats
You might also like
- The Little Book of Sexual HappinessDocument40 pagesThe Little Book of Sexual Happinesswolf4853100% (2)
- Fluid and Electrolytes for Nursing StudentsFrom EverandFluid and Electrolytes for Nursing StudentsRating: 5 out of 5 stars5/5 (12)
- CBSE Class 7 English - Comprehension PassageDocument7 pagesCBSE Class 7 English - Comprehension PassagemotherhoodNo ratings yet
- Reminiscences of An Old TimerDocument524 pagesReminiscences of An Old TimersuneelmadhavNo ratings yet
- Fluids and Electrolytes Study GuideDocument13 pagesFluids and Electrolytes Study GuideElizabeth McKeeNo ratings yet
- Fluid Electrolyte Imbalance n132 160210135651Document100 pagesFluid Electrolyte Imbalance n132 160210135651Shahan FarooqNo ratings yet
- Fluid and Electrolyte Management of Surgical Patient PDFDocument37 pagesFluid and Electrolyte Management of Surgical Patient PDFJie CuetoNo ratings yet
- Prepartion of Blood Smear Hematology PresentationDocument44 pagesPrepartion of Blood Smear Hematology PresentationArslan ArshadNo ratings yet
- Fluid Electrolyte Imbalance NvertedDocument111 pagesFluid Electrolyte Imbalance Nvertedchitrakshi khairnarNo ratings yet
- Oncology EmergencyDocument41 pagesOncology Emergencyomad pendaftaranPPDS100% (2)
- Cusack Protocol .. Supplement Dosages Information Chart. Word PDFDocument2 pagesCusack Protocol .. Supplement Dosages Information Chart. Word PDFNaomy DC100% (6)
- Follow Site Quarantine ProceduresDocument67 pagesFollow Site Quarantine ProceduresJohn James100% (3)
- Vocabulary Exercises: 1) Complete in The Correct WayDocument5 pagesVocabulary Exercises: 1) Complete in The Correct Waylaura1pinilla1domingNo ratings yet
- Acute Renal Failure Nursing Care PlanDocument15 pagesAcute Renal Failure Nursing Care PlanRanusha AnushaNo ratings yet
- Conivaptan MedicalDocument38 pagesConivaptan MedicalSanjay NavaleNo ratings yet
- NCP Liver CirrhosisDocument2 pagesNCP Liver Cirrhosismarlx5100% (3)
- Chest RadiographyDocument65 pagesChest RadiographyMunish Dogra100% (1)
- Hyponatremia: Consultant On CallDocument5 pagesHyponatremia: Consultant On CallDanilo JimenezNo ratings yet
- Fluid Volume ExcessDocument34 pagesFluid Volume ExcessajNo ratings yet
- Dapus 30Document25 pagesDapus 30Titi SulistiowatiNo ratings yet
- 82 Siadh PDFDocument10 pages82 Siadh PDFSalsabilla SaharaNo ratings yet
- Cerebral Salt WastingDocument7 pagesCerebral Salt WastingVALERIAARIZANo ratings yet
- Sodium and Potassium DisordersDocument7 pagesSodium and Potassium DisordersShia LevyNo ratings yet
- Neurointensivismo Metabolismo Del SodioDocument11 pagesNeurointensivismo Metabolismo Del SodioAlanNo ratings yet
- 110-Dehydration and Disorders of Sodium BalanceDocument5 pages110-Dehydration and Disorders of Sodium BalancepelinNo ratings yet
- Disorders-Of-Sodium-Balance - CAMBRIDGEDocument10 pagesDisorders-Of-Sodium-Balance - CAMBRIDGEDenisa Carmen ColiofNo ratings yet
- Disorders of Sodium and Water Balance in Hospitalized Patients Les Troubles de L'e Quilibre Hydrosode Chez Les Patients Hospitalise SDocument17 pagesDisorders of Sodium and Water Balance in Hospitalized Patients Les Troubles de L'e Quilibre Hydrosode Chez Les Patients Hospitalise SJuliane SilvaNo ratings yet
- FILE 20201125 231142 Hyponatremia A Practical ApproachDocument12 pagesFILE 20201125 231142 Hyponatremia A Practical ApproachTrọng ThuNo ratings yet
- Dysnatremia in The ICU: Milap Pokaharel and Clay A. BlockDocument13 pagesDysnatremia in The ICU: Milap Pokaharel and Clay A. BlockJonathan Gustavo MenaNo ratings yet
- Diabetes Insipidus and SIADH Reference Sheet: Normal Lab Values Siadh DIDocument13 pagesDiabetes Insipidus and SIADH Reference Sheet: Normal Lab Values Siadh DIJohn TusselNo ratings yet
- Fispatologjia e CreegullimeveDocument16 pagesFispatologjia e CreegullimeveArmar MendoNo ratings yet
- Hiponatremia in The ClinicaDocument19 pagesHiponatremia in The ClinicaHugo GonzálezNo ratings yet
- Sodium Potassium Imbalances MedsurgDocument5 pagesSodium Potassium Imbalances Medsurgchi kNo ratings yet
- Hyponatraemia: Dr. Peter Allan Dr. Saibal GangulyDocument8 pagesHyponatraemia: Dr. Peter Allan Dr. Saibal Gangulynur khadijahNo ratings yet
- Syndrome of Inappropriate Vasopressin Sexretion (Siadh)Document22 pagesSyndrome of Inappropriate Vasopressin Sexretion (Siadh)Moni RethNo ratings yet
- Sodium ImbalancesDocument6 pagesSodium ImbalancesJade CentinoNo ratings yet
- Guidelines For Management Of: HypernatremiaDocument7 pagesGuidelines For Management Of: HypernatremiaSarly Puspita AriesaNo ratings yet
- Fluid and Electrolyte DisordersDocument9 pagesFluid and Electrolyte DisordersRehab weridaNo ratings yet
- Distúrbios de SodioDocument19 pagesDistúrbios de SodioRafaelNo ratings yet
- Patho SlidesDocument26 pagesPatho Slidesapi-725203846No ratings yet
- Assessment Diagnosis Planning Intervention-Rationale Evaluation Fluid Volume Excess Related ToDocument3 pagesAssessment Diagnosis Planning Intervention-Rationale Evaluation Fluid Volume Excess Related ToJen BallesterosNo ratings yet
- Activity On Pituitary Disorders and Diabetes MellitusDocument8 pagesActivity On Pituitary Disorders and Diabetes MellitusSherlyn Miranda GarcesNo ratings yet
- Electrolyte and Acid Base BalanceDocument26 pagesElectrolyte and Acid Base BalanceMysheb SSNo ratings yet
- Content 71 639Document12 pagesContent 71 639Vinoth LakshmikanthNo ratings yet
- Electrolyte Imbalances ReviewerDocument14 pagesElectrolyte Imbalances ReviewerhoneyNo ratings yet
- SAJAA (V27) p126-130 2691 FCA SupplementDocument5 pagesSAJAA (V27) p126-130 2691 FCA SupplementVivek PatangeNo ratings yet
- Hyponatremia: Annals of Internal MedicineDocument19 pagesHyponatremia: Annals of Internal MedicineAbdallahMousaNo ratings yet
- Osmoregulation and Control of Icfv Lecture-IDocument50 pagesOsmoregulation and Control of Icfv Lecture-IfadhiliNo ratings yet
- Nefrologia 30 Dias Electrolitos - 2Document31 pagesNefrologia 30 Dias Electrolitos - 2JUAN ANDRES GUARDIAS GARZONNo ratings yet
- Reynolds, RM Padfield, PL Seckl, JR (2006) Disorders of Sodium BalanceDocument4 pagesReynolds, RM Padfield, PL Seckl, JR (2006) Disorders of Sodium BalanceMerlin MuktialiNo ratings yet
- HyponatremiaDocument9 pagesHyponatremiaFebe ChristiantoNo ratings yet
- I.V. Fluid Therapy IDocument4 pagesI.V. Fluid Therapy IPrabath ChinthakaNo ratings yet
- Neuro-Hiponatremia 4Document11 pagesNeuro-Hiponatremia 4Kim Escobedo HurtadoNo ratings yet
- NCP AkdDocument3 pagesNCP AkdJb RosillosaNo ratings yet
- Hiponatremia JonessDocument11 pagesHiponatremia JonessEfi AdriánNo ratings yet
- 344 Full PDFDocument3 pages344 Full PDFfadhylNo ratings yet
- Electrolyte Disturbaces - Hyponatremia and HypernatremiaDocument41 pagesElectrolyte Disturbaces - Hyponatremia and HypernatremiaMohammad AliNo ratings yet
- Intravenous Fluid Therapy - Knowledge For Medical Students and PhysiciansDocument6 pagesIntravenous Fluid Therapy - Knowledge For Medical Students and PhysiciansNafiul IslamNo ratings yet
- Nursing Care Plan HypovolemiaDocument8 pagesNursing Care Plan HypovolemiaGusmila SariNo ratings yet
- Mechanisms and Management of Diuretic Resistance I PDFDocument5 pagesMechanisms and Management of Diuretic Resistance I PDFErensina M MansnandifuNo ratings yet
- Electrolyte Imbalances ReviewerDocument14 pagesElectrolyte Imbalances ReviewerhoneyNo ratings yet
- How To Respond To Abnormal Serum Sodium LevelsDocument3 pagesHow To Respond To Abnormal Serum Sodium LevelsNixNo ratings yet
- Class 1Document3 pagesClass 1JennNo ratings yet
- Diabetes Insipidus: Nursing Care PlansDocument6 pagesDiabetes Insipidus: Nursing Care PlansSewyel GarburiNo ratings yet
- Management of Edema in Nephrotic Syndrome PDFDocument10 pagesManagement of Edema in Nephrotic Syndrome PDFmolenNo ratings yet
- HYPO and HYPERNATREMIA IN NEONATESDocument10 pagesHYPO and HYPERNATREMIA IN NEONATESraghava mbbsNo ratings yet
- Legrand Et Al-2019-Intensive Care MedicineDocument4 pagesLegrand Et Al-2019-Intensive Care MedicineJustin DodaneNo ratings yet
- Determinacindevaloresecocardiogrficosenel Perrosin Pelodel PerdetamaomedianoDocument9 pagesDeterminacindevaloresecocardiogrficosenel Perrosin Pelodel Perdetamaomedianodavid alonsoNo ratings yet
- Obat NsadsDocument20 pagesObat NsadsZaki MubaraqNo ratings yet
- CITI - Collaborative Institutional Training Initiative 1Document16 pagesCITI - Collaborative Institutional Training Initiative 1david alonsoNo ratings yet
- CITI - Collaborative Institutional Training Initiative 8Document21 pagesCITI - Collaborative Institutional Training Initiative 8david alonsoNo ratings yet
- Half-Life Valve Software'sDocument6 pagesHalf-Life Valve Software'sdavid alonsoNo ratings yet
- KoboLibra2 UserGuide enDocument48 pagesKoboLibra2 UserGuide endavid alonsoNo ratings yet
- Buenona Salazar 2020 01 20 1454 PDFDocument2 pagesBuenona Salazar 2020 01 20 1454 PDFdavid alonsoNo ratings yet
- Half-Life Valve Software'sDocument6 pagesHalf-Life Valve Software'sdavid alonsoNo ratings yet
- Half-Life Valve Software'sDocument6 pagesHalf-Life Valve Software'sdavid alonsoNo ratings yet
- Seroprevalenceof Salmonellaand MycoplasmaDocument7 pagesSeroprevalenceof Salmonellaand Mycoplasmadavid alonsoNo ratings yet
- Liver L1 15Document26 pagesLiver L1 15Jacqueline SyNo ratings yet
- 1 Renal 20191 EVADocument28 pages1 Renal 20191 EVAdavid alonso0% (1)
- Hyponatremia Review. Clinician's Brief: January 2010Document6 pagesHyponatremia Review. Clinician's Brief: January 2010david alonsoNo ratings yet
- Venipuncture Techniques in Chelonian Species: Lab Animal August 2008Document3 pagesVenipuncture Techniques in Chelonian Species: Lab Animal August 2008david alonsoNo ratings yet
- Effectiveness of Self Myofascial Release On Pain and Functional Ability in Recreational Runners With Medial Tibial Stress SyndromeDocument3 pagesEffectiveness of Self Myofascial Release On Pain and Functional Ability in Recreational Runners With Medial Tibial Stress SyndromePaulRajNo ratings yet
- Cestode Parasites: Medical Parasitology, 2009 University of Palangkaraya Agus HaryonoDocument45 pagesCestode Parasites: Medical Parasitology, 2009 University of Palangkaraya Agus HaryonoMeylisa Gerson BayanNo ratings yet
- Annotated BibliographyDocument31 pagesAnnotated BibliographyLara MelissaNo ratings yet
- Treatment of CellulitisDocument2 pagesTreatment of CellulitistreatmentcellNo ratings yet
- A Case of Subcorneal Pustular Dermatosis Successfully Treated With AcitretinDocument3 pagesA Case of Subcorneal Pustular Dermatosis Successfully Treated With Acitretindr_RMNo ratings yet
- Housing of Sheep and GoatsDocument12 pagesHousing of Sheep and Goatsglennpuputi10No ratings yet
- English ChillaDocument8 pagesEnglish ChillaChilla Adis ViolitaNo ratings yet
- Đề 4. Đề Thi Thử TN THPT Môn Tiếng Anh Theo Cấu Trúc Đề Minh Họa 2021 - Cô Oanh - Có Lời GiảiDocument15 pagesĐề 4. Đề Thi Thử TN THPT Môn Tiếng Anh Theo Cấu Trúc Đề Minh Họa 2021 - Cô Oanh - Có Lời GiảiBình Bùi thanhNo ratings yet
- Shier - Hole's Human Anatomy & Physiology 13e-1Document30 pagesShier - Hole's Human Anatomy & Physiology 13e-1ptchiquynhNo ratings yet
- HSC 430 Lesson PlanDocument13 pagesHSC 430 Lesson Planapi-486607583No ratings yet
- BIOLOGY RevisionNotes SaveMyExamsDocument7 pagesBIOLOGY RevisionNotes SaveMyExamsAli AshrafNo ratings yet
- Venomous Snakes of IraqDocument5 pagesVenomous Snakes of IraqLisa3000No ratings yet
- Effect of Adding Different Levels of Olive Leaf Powder To The Diet On The Production Performance and Some Physiological Characteristics of BroilersDocument9 pagesEffect of Adding Different Levels of Olive Leaf Powder To The Diet On The Production Performance and Some Physiological Characteristics of BroilersreviewjreNo ratings yet
- Ocw Humanos y Otros AnimalesDocument4 pagesOcw Humanos y Otros Animalesmiguel6789No ratings yet
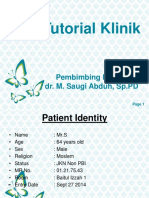
- Tutorial Dr. SaugiDocument33 pagesTutorial Dr. SaugifemmytaniaNo ratings yet
- Studi Deskriptif Mengenai Resiliensi Pada ODHA Di Komunitas KDS Puzzle Club BandungDocument7 pagesStudi Deskriptif Mengenai Resiliensi Pada ODHA Di Komunitas KDS Puzzle Club BandungArif GustyawanNo ratings yet
- Year 9 Term 2 Science Formative AssessmentDocument2 pagesYear 9 Term 2 Science Formative AssessmentAditya N WardhanaNo ratings yet
- Blood Pressure RegulationDocument11 pagesBlood Pressure RegulationPaulShaneHerreraZorrillaNo ratings yet
- Physiology of Autonomic Nervous System: J J M Medical College, Davangere. Dept of AnesthesiaDocument117 pagesPhysiology of Autonomic Nervous System: J J M Medical College, Davangere. Dept of AnesthesiaKithminaNo ratings yet
- Reproduction SystemDocument38 pagesReproduction SystemNurfatin AdilaNo ratings yet
- SONAC-Aqua Feed MarketDocument4 pagesSONAC-Aqua Feed MarketDiel MichNo ratings yet
- EsquistocitosDocument10 pagesEsquistocitoswillmedNo ratings yet