Professional Documents
Culture Documents
ID12 Infectious Diseases Gastrointestinal Infections Toronto Notes 2016
Uploaded by
evangelineOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ID12 Infectious Diseases Gastrointestinal Infections Toronto Notes 2016
Uploaded by
evangelineCopyright:
Available Formats
ID12 Infectious Diseases Gastrointestinal Infections Toronto Notes 2016
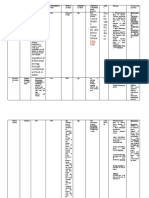
Table 13. Bacteria in Infectious Diarrhea
Pathogen Source or Mode of Incubation Clinical Features Duration Antimicrobial Therapy Notes
Transmission
Fever Bloody Abdo N/V
Stool Pain
B. cereus – Type A Rice dishes 1-6 h – – – + <12 h None Preformed exotoxin
(emetic)
B. cereus – Type B Meats, vegetables, 8-16 h – – – – <24 h None Secondary endotoxin
(diarrheal) dried beans, cereals
Campylobacter jejuni Uncooked meat, 2-10 d + ± + ± <1 wk Macrolide or fluoroquinolone Most common bacterial
especially poultry if diarrhea >1 wk, cause of diarrhea in Canada
bloody diarrhea, or Associated with Guillain-
immunocompromised Barré syndrome
Clostridium difficile Can be normally Unclear ± ± ± – Variable Stop culprit antibiotic Usually follows
present in therapy, if possible antibiotic treatment
colon in small Supportive therapy (IV fluids) (especially clindamycin,
numbers (primary Mild-moderate disease: fluoroquinolones, penicillins,
risk factor for metronidazole PO x 10-14 d cephalosporins)
disease is exposure Severe disease: vancomycin Can develop
to antimicrobials) PO x 10 - 14 d pseudomembranous colitis
Toxic Megacolon:
metronidazole IV +
vancomycin PO (as above)
and general surgery consult
Clostridium perfringens Contaminated food, 8-12 h ± – + – <24 h None Clostridium spores are heat
especially meat and resistant
poultry Secondary enterotoxin
Enteroinvasive E. coli Contaminated 1-3 d + ± + – 7-10 d None Relatively uncommon
(EIEC) food/water
Enterotoxigenic E. coli Contaminated 1-3 d – – + – 3d Fluoroquinolone or Most common cause of
(ETEC) food/water azithromycin for moderate to traveller's diarrhea
severe symptoms Heat-labile and heat-stable
toxins
Enterohemorrhagic Contamination 3-8 d – + + ± 5-10 d None: antibiotics increase Shiga toxin production
E. coli (EHEC/STEC) of hamburger, raw risk of HUS Monitor renal function:
i.e. O157:H7 milk, drinking, and 10% develop HUS
recreational water Antidiarrheals increase risk
of HUS
Salmonella typhi Fecal-oral 10-14 d + ± + ± <5-7 d Empiric treatment with Salmonella typhi: "Rose
S. paratyphi Contaminated ceftriaxone or azithromycin spot" rash (on anterior
(i.e. Enteric Fever, food/water, travel Fluoroquinolone resistance thorax, upper abdomen),
Typhoid) to endemic area is increasing fever, and abdominal pain
precedes diarrhea
Non-typhoidal Contaminated 12-72 h + ± + + 3-7 d Ciprofloxacin only in severe
Salmonellosis animal food illness, extremes of age,
S. typhimurium, products, especially joint prostheses, valvular
S. enteritidis eggs, poultry, meat, heart disease, severe
milk atherosclerosis, cancer,
uremia
Shigella dysenteriae Fecal-oral 1-4 d + ± + + <1 wk Fluoroquinolone Very small inoculum needed
Contaminated for infection
food/water Complications include toxic
megacolon, HUS
Antidiarrheals may increase
risk of toxic megacolon
Staphylococcus Unrefrigerated meat 2-4 h – – + + 1-2 d None Heat-stable preformed
aureus and dairy products exotoxin
(custard, pudding,
potato salad, mayo)
Vibrio cholerae Contaminated 1-3 d – – – – 3-7 d Tetracycline or quinolones Massive watery diarrhea
food/water, (ciprofloxacin) (1-3 L/d)
especially shellfish Mortality <1% with
treatment
Yersinia Contaminated food 5d + ± + ± Up to Fluoroquinolone only for Majority of cases in children
Unpasteurized milk 3 wk severe illness 1-4 yr
Mesenteric adenitis and
terminal ileitis can occur
without diarrhea, mimicking
appendicitis
ID13 Infectious Diseases Gastrointestinal Infections Infectious Diseases ID13
Table 14. Parasites in Infectious Diarrhea
Pathogen Source or Mode of Incubation Clinical Features Duration Antimicrobial Therapy Notes
Transmission
Fever Bloody Abdo N/V
Stool Pain
Cryptosporidium Fecal-oral 7d ± – – + 1-20 d Paromomycin + nitazoxanide Immune reconstitution if
immunosuppressed
Entamoeba histolytica Worldwide 2-4 wk ± + – + Variable Metronidazole + If untreated, potential for
endemic areas iodoquinol or paromomycin liver abscess
Fecal-oral if symptomatic infection Sigmoidoscopy shows flat
Only iodoquinol or ulcers with yellow exudates
paromomycin for
asymptomatic cyst passage
Giardia lamblia Fecal-oral 1-4 wk – – + + Variable Metronidazole or Higher risk in: day care
Contaminated nitazoxanide children, intake of untreated
food/water Treatment of asymptomatic water ("beaver fever"), MSM,
carriers not recommended immunodeficiency
Toronto Notes 2016 (decreased IgA)
May need duodenal biopsy
Table 15. Viruses in Infectious Diarrhea
Pathogen Source or Mode of Incubation Clinical Features Duration Antimicrobial Therapy Notes
Transmission
Fever Bloody Abdo N/V
Stool Pain
Norovirus Fecal-oral 24 h – – + + 24 h None Noroviruses includes
Norwalk virus
Rotavirus Fecal-oral 2-4 d ± – – ± 3-8 d None Can cause severe
dehydration
Virtually all children are
infected by 3 yr of age
Oral vaccine given at 2 and
4 mo of age
Traveller's Diarrhea
• see Acute Diarrhea, ID10
Epidemiology
• most common illness to affect travellers
• up to 50% of travellers to developing countries affected in first 2 wk and 10-20% after returning
home
Etiology
• bacterial (80-90%): E. coli most common (ETEC), Campylobacter, Shigella, Salmonella, Vibrio
(non-cholera); wide regional variation (e.g. Campylobacter more common in Southeast Asia)
• viral: norovirus, rotavirus, and astrovirus account for 5-8%
• protozoal (rarely): Giardia, Entamoeba histolytica, Cryptosporidium, and Cyclospora for ~10% in
long-term travellers
• pathogen-negative traveller's diarrhea common despite exhaustive microbiological workup
Treatment
• rehydration is the mainstay of therapy
rehydrate with sealed beverages
in severe fluid loss use oral rehydration solutions (1 package in 1 L boiled or treated water)
• treat symptoms: antidiarrheal agents (e.g. bismuth salicylate, loperamide)
• empiric antibiotics in moderate or severe illness: ciprofloxacin or azithromycin or rifaximin
note: there is increasing fluoroquinolone resistance in causative agents, especially in
Southeast Asia
Prevention
• proper hygiene practices
avoid consumption of: foods or beverages from establishments with unhygienic conditions
(e.g. street vendors), raw fruits or vegetables without a peel, raw or undercooked meat and
seafood
avoid untreated water
• bismuth salicylate (Pepto-Bismol®): 60% effective (2 tablets qid according to CDC website)
• CDC Guidelines: antibiotic prophylaxis not recommended Bismuth salicylate (Pepto-Bismol®) can
increased risk of infection with resistant organisms cause patients to have black stools,
which may be mistaken for melena
high risk groups (e.g. immunocompromised) likely to be infected with pathogen not covered
by standard antimicrobial agents
You might also like
- Bacteria ChartsDocument11 pagesBacteria ChartsFlowerNo ratings yet
- Infectious Disease - BoardsDocument8 pagesInfectious Disease - BoardsSoojung NamNo ratings yet
- 911 Pigeon Disease & Treatment Protocols!From Everand911 Pigeon Disease & Treatment Protocols!Rating: 4 out of 5 stars4/5 (1)
- Swine 2Document40 pagesSwine 2Keegan McElroyNo ratings yet
- Gram Positive: CoccusDocument8 pagesGram Positive: CoccusLM MysNo ratings yet
- Food PoisoningDocument19 pagesFood PoisoningHemanathan PraemNo ratings yet
- Microbiology NotesDocument13 pagesMicrobiology NotesMalekNo ratings yet
- Chapter 43: Nursing Care of A Family When A Child Has An Infectious Disorder The Infectious Process #1 Infectious Disease in ChildrenDocument20 pagesChapter 43: Nursing Care of A Family When A Child Has An Infectious Disorder The Infectious Process #1 Infectious Disease in ChildrenMark oliver Gonzales100% (1)
- Thermobacteriology I: Food Microbiology and Public HealthDocument28 pagesThermobacteriology I: Food Microbiology and Public HealthHasan TheMcNo ratings yet
- YersiniosisDocument2 pagesYersiniosisMaisarah RepinNo ratings yet
- PertussisDocument13 pagesPertussisRhuthree Mabalacat100% (1)
- Approach To Patient With Diarrhea and VomitingDocument4 pagesApproach To Patient With Diarrhea and VomitingRed DevilNo ratings yet
- Digestive System InfectionsDocument30 pagesDigestive System InfectionsGoNo ratings yet
- Birao Sas 13 Microbiology and ParasitologyDocument9 pagesBirao Sas 13 Microbiology and ParasitologyFrancis Jacob Dejecacion GarcesNo ratings yet
- Daren G. Linatoc, RN, RM, LPT, Man, MaedDocument36 pagesDaren G. Linatoc, RN, RM, LPT, Man, MaedMike Faustino SolangonNo ratings yet
- Waterborne Diseases: Group 2Document21 pagesWaterborne Diseases: Group 2Jay RickNo ratings yet
- IMG EmpAposterDocument1 pageIMG EmpAposterChiu LeoNo ratings yet
- Infectious Diseases Tabelle (Examen 6. Jahr)Document34 pagesInfectious Diseases Tabelle (Examen 6. Jahr)Aastha SethNo ratings yet
- Infectious DocumentDocument8 pagesInfectious DocumentMohan SrinivasNo ratings yet
- Diarrhoea in MedicineDocument10 pagesDiarrhoea in MedicineMohd NadeemNo ratings yet
- Guidelines Emporical Antibiotic Therapy in AdultDocument2 pagesGuidelines Emporical Antibiotic Therapy in Adultgulf jobsNo ratings yet
- Approach To UTIDocument3 pagesApproach To UTIRochelle CionNo ratings yet
- PHARMA MIDTERM 2ndyrnsgDocument38 pagesPHARMA MIDTERM 2ndyrnsgquincy fajardoNo ratings yet
- Virus - SystemsDocument9 pagesVirus - SystemsHanunNo ratings yet
- Food Poisoning, Bacterial - ClinicalKeyDocument19 pagesFood Poisoning, Bacterial - ClinicalKeyclarestaNo ratings yet
- BenadrylDocument2 pagesBenadrylsamfandood10No ratings yet
- Beta-Lactams: Ampicillin, Amoxicillin, Third-Generation Cephalosporins (Cefixime, Ceftriaxone)Document2 pagesBeta-Lactams: Ampicillin, Amoxicillin, Third-Generation Cephalosporins (Cefixime, Ceftriaxone)Angelo MichaelNo ratings yet
- Staph. Aureus Staph. Epidermidis Staph. SaprophyticusDocument5 pagesStaph. Aureus Staph. Epidermidis Staph. SaprophyticusTom PedersonNo ratings yet
- Oxidase - : EnterobacteriaceaeDocument1 pageOxidase - : EnterobacteriaceaeTaylor EdgleyNo ratings yet
- Summarize Notes On ImciDocument6 pagesSummarize Notes On ImciI'm Just A BurgerNo ratings yet
- Clostridoides DifficileDocument2 pagesClostridoides Difficileyabhas chhetriNo ratings yet
- Pathologic and NonDocument11 pagesPathologic and NonAisha DoreenNo ratings yet
- DIPTHERIADocument2 pagesDIPTHERIADr KhatidjaNo ratings yet
- Diarrhea in The Elderly: Initial or 1 RecurrenceDocument1 pageDiarrhea in The Elderly: Initial or 1 Recurrencedewi wulandariNo ratings yet
- Infectious Diarrhea: Gail S. Itokazu, David T. Bearden, and Larry H. DanzigerDocument23 pagesInfectious Diarrhea: Gail S. Itokazu, David T. Bearden, and Larry H. DanzigerRismaAjhaNo ratings yet
- Diarrhea PEDSDocument10 pagesDiarrhea PEDSOasis LimitedNo ratings yet
- 2021 Infection Management PosterDocument1 page2021 Infection Management PosterBosco WoodsNo ratings yet
- Gastroenteritis Dan DehidrasiDocument5 pagesGastroenteritis Dan DehidrasiSelly TiyaningrumNo ratings yet
- Micro by DR - Hesham (GIT)Document65 pagesMicro by DR - Hesham (GIT)abcde990075No ratings yet
- Food Microbiolog - Modified & CorrectedDocument25 pagesFood Microbiolog - Modified & CorrectedssalahNo ratings yet
- Pertemuan Ke-3 GASTRODocument36 pagesPertemuan Ke-3 GASTROwidya melianitaNo ratings yet
- Tuberculosis and CestodesDocument4 pagesTuberculosis and CestodesRizalyn Padua ReyNo ratings yet
- Foodborne Illness: Members: Nguy Minh Hoang Pham Nhat Thao Linh Le Thi Huyen Trang Instructor: Vo Le Dinh TamDocument13 pagesFoodborne Illness: Members: Nguy Minh Hoang Pham Nhat Thao Linh Le Thi Huyen Trang Instructor: Vo Le Dinh TamThảo LinhNo ratings yet
- HelminthsDocument11 pagesHelminthsTienneNo ratings yet
- Tinywow Communicable-Diseases 48897647 15Document1 pageTinywow Communicable-Diseases 48897647 15JULIUS CEZAR QUINAYNo ratings yet
- Diarrhea UpdatedDocument66 pagesDiarrhea UpdatedAna KarlaNo ratings yet
- FBD 2021Document99 pagesFBD 2021Ruth Mary PadaNo ratings yet
- 0506hoENTEROVIRAL INFECTIONSDocument57 pages0506hoENTEROVIRAL INFECTIONSAmandeep SinghNo ratings yet
- Infectious Disease of The Gastro Intestinal TractDocument12 pagesInfectious Disease of The Gastro Intestinal TractCj PajarillagaNo ratings yet
- Test 2 ChartDocument29 pagesTest 2 Chartapi-26938624No ratings yet
- PEDIA Bacterial Infections Part 2 Dr. E. Lim FinalDocument5 pagesPEDIA Bacterial Infections Part 2 Dr. E. Lim FinalClaire DuNo ratings yet
- OrganismDocument3 pagesOrganismJoanne Alyssa Hernandez LascanoNo ratings yet
- DIPTHERIADocument1 pageDIPTHERIAGrace StephanieNo ratings yet
- FST-602 Food Safety Bacterial Food Infections (Part-3) Lecture # 5Document18 pagesFST-602 Food Safety Bacterial Food Infections (Part-3) Lecture # 5muqaddasNo ratings yet
- Micro Part 3Document180 pagesMicro Part 3Perlie CNo ratings yet
- NCM116 CDN Gastrointestinal LECDocument18 pagesNCM116 CDN Gastrointestinal LECMilcah NuylesNo ratings yet
- Common Foodborne PathogensDocument3 pagesCommon Foodborne PathogensO PNo ratings yet
- Summary Final 2022Document12 pagesSummary Final 2022Rana zaatrehNo ratings yet
- Biology Investigatory Project Viral DiseasesDocument16 pagesBiology Investigatory Project Viral DiseasesAman MujeebNo ratings yet
- Ampicillin Sodium (Polypen)Document3 pagesAmpicillin Sodium (Polypen)Charlene Serino JavierNo ratings yet
- Foodborne IllnessDocument13 pagesFoodborne IllnessThảo LinhNo ratings yet
- Week 5 Past Perfect Practice 2Document4 pagesWeek 5 Past Perfect Practice 2Soldjair Mantari SotoNo ratings yet
- Staphylococci 18 StudentDocument42 pagesStaphylococci 18 StudentJulia MartinezNo ratings yet
- Compilation of Infectious Diseases: A Project in Community and Public HealthDocument8 pagesCompilation of Infectious Diseases: A Project in Community and Public HealthAbigail VirataNo ratings yet
- 61Document205 pages61Carlos HernándezNo ratings yet
- Pharmacology II Sem V Question BankDocument11 pagesPharmacology II Sem V Question BankabcNo ratings yet
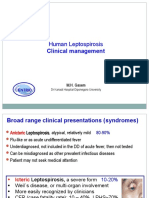
- Lepto Clinical Management GLEAN 2019 - M GasemDocument42 pagesLepto Clinical Management GLEAN 2019 - M GasemSelfie C RijalNo ratings yet
- Cause and Effects of PneumoniaDocument1 pageCause and Effects of PneumoniaAlmer OstreaNo ratings yet
- Diseases of The Pharynx: BY DR Arif Raza Khan Assistant Professor E.N.T. K.T.HDocument29 pagesDiseases of The Pharynx: BY DR Arif Raza Khan Assistant Professor E.N.T. K.T.HSuleman MuhammadNo ratings yet
- Background: Pediatric Chickenpox Next Section: PathophysiologyDocument12 pagesBackground: Pediatric Chickenpox Next Section: PathophysiologyRachel Johann Aquinto100% (1)
- Hamester: Submitted To: DR - Waqas Ahmed Submitted By: Shahbaz Ahmed Registration No:2017-Dvmn-040Document43 pagesHamester: Submitted To: DR - Waqas Ahmed Submitted By: Shahbaz Ahmed Registration No:2017-Dvmn-040Shahbaz AhmedNo ratings yet
- Bacterial Skin InfectionsDocument73 pagesBacterial Skin InfectionsAnthony Bravo CortezNo ratings yet
- COVID 19 Bharat India Report November09 2022 DailyCases 1116 Deaths 5 Based 781 DaysAnalysis Fbclid IwAR2orDocument225 pagesCOVID 19 Bharat India Report November09 2022 DailyCases 1116 Deaths 5 Based 781 DaysAnalysis Fbclid IwAR2orP Eng Suraj SinghNo ratings yet
- Humaniora Ii - 26 Maret 20 - 1 Jam - Endah - Kebudayaan Dan KesehatanDocument70 pagesHumaniora Ii - 26 Maret 20 - 1 Jam - Endah - Kebudayaan Dan KesehatanpkmsoboNo ratings yet
- Whooping CoughDocument72 pagesWhooping Coughwengie100% (1)
- 2011 - 4 Annual Report Detail Idsp Banaskantha 2011Document63 pages2011 - 4 Annual Report Detail Idsp Banaskantha 2011Pankaj ModhNo ratings yet
- 1 - Norovirus Care Home Poster 2018Document1 page1 - Norovirus Care Home Poster 2018GarryNo ratings yet
- ID4013 - SPW103 - Assessment - 2 - Response Template - 230321 2Document20 pagesID4013 - SPW103 - Assessment - 2 - Response Template - 230321 2SUCHETA DASNo ratings yet
- SeqdumpDocument7 pagesSeqdumpAnayantzin AyalaNo ratings yet
- JBNJN - Docx ENGLISHDocument2 pagesJBNJN - Docx ENGLISHمحسن حدوان عليخانNo ratings yet
- UntitledDocument5 pagesUntitledCresensia ElkesiaNo ratings yet
- Reference PDFDocument5 pagesReference PDFWina BudiartiNo ratings yet
- 16/09/2015 1 Mujtaba AshrafDocument44 pages16/09/2015 1 Mujtaba Ashrafதீரன் சக்திவேல்No ratings yet
- DHQ HPC Cord Questionnairev1Document3 pagesDHQ HPC Cord Questionnairev1DalokeshNo ratings yet
- BF Builders and Construction Corporation Hiv/Aids Workplace Policy and ProgramDocument4 pagesBF Builders and Construction Corporation Hiv/Aids Workplace Policy and Programglenn dalesNo ratings yet
- MCM Fact Sheet 191009Document6 pagesMCM Fact Sheet 191009Ruth CandorNo ratings yet
- Icd 10 CM Pcs Coding Theory and Practice 2017 Edition 1st Edition Lovaasen Test BankDocument12 pagesIcd 10 CM Pcs Coding Theory and Practice 2017 Edition 1st Edition Lovaasen Test Bankgisellephongejs100% (36)
- Avion FluDocument1 pageAvion FluImaan RiazNo ratings yet
- Limitations Results: Congenital Syphilis: Management Dilemmas Using Reverse ScreeningDocument1 pageLimitations Results: Congenital Syphilis: Management Dilemmas Using Reverse ScreeningFaye Cabotaje LinganNo ratings yet