Professional Documents
Culture Documents
COPD (D.E.P.C.I.T) : Done By: Miya Wong
Uploaded by
Kyra KhalidOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
COPD (D.E.P.C.I.T) : Done By: Miya Wong
Uploaded by
Kyra KhalidCopyright:
Available Formats
COPD (D.E.P.C.I.
T)
Chronic Obstructive Pulmonary Disease
Definition - Disease state characterized by presence of airflow obstruction
due to Chronic Bronchitis + Emphysema
Etiology MEDS GiRL
M- Male > female
E- Environmental pollution
D- Dusty occupation(gold,coal miners, farmers, grain, cement,cotton)
S- Smoking
G- Genetic Deficiency – alpha 1- antitrypsin
R- Recurrent bronchopulm. Infection
L- Low socioeconomic status
Pathophysiology Chronic Bronchitis Emphysema
and classification Def- Cough and expectoration Def- Abnormal permanent
of most days for 3 successive enlargement of gas-exhanging
months in at least 2 successive of the lungs (acini) + destruction
years and cannot diagnosed as of alveolar walls +/- fibrosis
other pulmonary or cardiac
causes
Classification-
1. Simple CB- Chr
productive cough +
normal airflow
2. Chronic Obstructive
bronchitis – Chr
productive cough +
progressive decline
airflow
Pathological feature:
A. Chronic Bronchitis
1. Mucous Gland Hypertrophy – neutrophils, T lymphocytes)
2. Cartilage atrophy-> scarring and remodelling that thickens the
wall of bronchi
3. Muscle hypertrophy
Pathophysiology:-
Inflammation -> changes of cilia -> cilia lose fx -> cilia is replaced with goblet cells ->
goblet cells produce a lot of mucus -> that mucus provide a good medium for bacterial
growth (pseudominas or staph) -> mucus infected and discoloured by the overgrowth
of bacteria -> swelling,mucus hypersecretion -> swelling of bronchi + bronchioles ->
problem airflow to and from the lungs -> meanwhile, muscle of airways is stimulated
by this irritants -> bronchospasm -> further narrowing of resp. airway -> long standing
inflammation -> fixed, non-reversible narrowing of airway
-> COPD
Done by: Miya Wong
B. Emphysema Pathological Feature:
Types of emphysema
Centrilobular Part – proximal central part
Lungs – upper lobe
Associates w smoking, COPD, CB
Panacinar Part – complete resp- lobules
Lungs- lower lobes anterior margin
Associates with A1AT deficiency
Paraseptal Part- Distal
Lungs – Upper half
Associates – pneumothorax, smoking,
Findings – enlarged airspaces <0.5 cm > 2cm
Bullae formation
Done by: Miya Wong
Pathophysiology:
Clinical Picture HACOWA
History of heavy smoking
Age > mid – old
Cough > 1st upon walking up -> throughout the day
- Productive cough – mucoid -> purulent sputum + exarcebation of
dse but not excessive
Onset – insidious – dyspnea on exertion and slowly progressive
Wheezes- persistent
Associated symptoms – wt loss, insomnia -> severe COPD
Done by: Miya Wong
Objective: Investigation and principles of treatment of COPD
Severe Dyspnea, Orthopnea,
1. Physical Examination: Tachypnea, + scanty sputum
a. Pink Puffer (Type 1)
Expiratory pursed lips
Elevated shoulder
Congested neck vein on Inspiratory tracheal tug
expiration;
Prominent accessory ms in
Pulsus Paradoxus
neck (scalene)
Abdominal Protuberance
Indrawing suprasternal + Usually thin build
supraclavicular fossae
General Muscle wasting in
advanced cases
Professorial attitude
b. Blue Bloater (Type 2)
Cyanosis
Mild dyspnea
Usually Obese
Large Sputum
Edema @ ankles
Done by: Miya Wong
2. Local Examination
a. Inspection and Palpation
i. Large barrel shaped chest + widening of Xiphersternal angle due to increase
Of A-P diameter
ii. Diminished chest expansion
iii. Hoover’s sign
Due to horizontal position
of diaphragm it acts to pull
inwards the lower ribs
during inspiration causing
retraction of costal margin
during inspiration
iv. In mild cases : no abnormality
v. s/s of resp. failure like cor-pulmonale + RSHF may present
vi. Blue Bloater Vs Pink Puffer (like the first page)
b. Percussion
i. Hyperresonance with encroachment on hepatic + cardiac dullness
(hyperinflation)
ii. Depressed liver due to flat diaphragm not enlarged
c. Auscultation
i. Diminished vesicular breath sound
ii. Distant heart sound -> damping of heart sound due to shifted position of
ventricles. Right ventricle is more anterior > Left ventricle (vertical narrow
heart seen in x-ray of COPD patient esp. the ones that has emphysema)
iii. Expiratory wheezes (constrict bronchioles)
iv. Crackles at lung base + crepitations (fluid in alveoli) during inspiration
Done by: Miya Wong
Investigation:
1. Imaging study
a. CXR
i. Hyperinflation of the lungs
ii. Flat diaphragm
iii. Hyperlucent lung fields (many air)
iv. Increased AP diameter
v. Increased retrosternal air
vi. Vertical narrow heart
vii. Peripheral vascular attenuation -> less vascular marking due to chronic
hypoxemia
b. CT
i. To diagnose early cases
2. PFT
a. Spirometer
i. Decreased FEV1 < 80%
ii. Decreased FEV1/FVC : <70%
stage FEV1 (%) FEV1/FVC (%)
0 At risk >80 N
1 Mild >80 <70
2 Moderate 50 -80 <70
3 Severe 30-50 <70
4 Very severe <30 <70
b. Bronchodilator test: Bronchial asthma improves FEV1 >15% , COPD <15%
improvement
3. ABG
a. Type A (Type 1) -> only 1 thing -> Hypoxemia no hypercapnia
b. Type B (Type 2) -> got 2 things -> Hypoxemia + Hypercapnia
c. 2ry polycythemia -> chronic hypoxia
d. May be deficiency of A1AT: N( 2 – 4 gm/L)
4. ECG
a. P-pulmonale (Peaked P wave in inferior leads) -> RVE
b. RVE in cor-pulmonale
c. Low voltage QRS complex especially in precordial leads
5. Echocardiography
a. Assess cardiac function
i. Contractility
ii. Pulmonary artery pressure (N: >30mmhg)
Done by: Miya Wong
Normal X-ray
Done by: Miya Wong
Done by: Miya Wong
Done by: Miya Wong
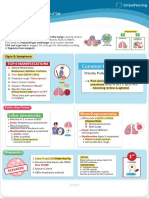
Management of COPD:
Pharmacological treatment:
Non pharmacological management:
1. Good nutrition
2. Rehab (Chest physiotherapy) -> to increase ms strength
Done by: Miya Wong
You might also like
- The Respiratory Tract in Pediatric Critical CareDocument258 pagesThe Respiratory Tract in Pediatric Critical CareririlibertiNo ratings yet
- Watts Aggregate Autopsy ReportsDocument26 pagesWatts Aggregate Autopsy ReportsEKilloran85% (78)
- Resp Lecture NotesDocument18 pagesResp Lecture Notessurviving nursing schoolNo ratings yet
- Chronic Obstructive Pulmonary DiseaseDocument36 pagesChronic Obstructive Pulmonary DiseaseHazel ManuelNo ratings yet
- Pleural Effusion, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandPleural Effusion, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- The System: RespiDocument219 pagesThe System: Respilalaine22dale100% (1)
- Detecting Heartbeats and Diagnosing Chest PainDocument113 pagesDetecting Heartbeats and Diagnosing Chest PainNasan Shehada100% (1)
- Respiratory Disorders & TB in Children (Part I and Ii) - Dr. MendozaDocument17 pagesRespiratory Disorders & TB in Children (Part I and Ii) - Dr. MendozaRea Dominique CabanillaNo ratings yet
- Pneumonia Patho & SignsDocument1 pagePneumonia Patho & SignsVishalNo ratings yet
- Midterm Last TopicDocument3 pagesMidterm Last TopicLynette BalodNo ratings yet
- Sheet - Respiratory ExaminationDocument11 pagesSheet - Respiratory ExaminationbakesamiNo ratings yet
- MEDICAL - SURGICAL by John RicafortDocument9 pagesMEDICAL - SURGICAL by John RicafortTazneem Apostol Esmael100% (2)
- Pulmonology Short CasesDocument10 pagesPulmonology Short CasesRZ Ng100% (1)
- Revision Notes On FRCRDocument385 pagesRevision Notes On FRCRObaidy Albushaher100% (2)
- Test Bank For Mechanical Ventilation 7th Edition J M CairoDocument13 pagesTest Bank For Mechanical Ventilation 7th Edition J M CairocalliopesilasaagyNo ratings yet
- NCM 112-Mod3Document19 pagesNCM 112-Mod3Samantha BolanteNo ratings yet
- Respiratory Physiology Adaptations To High-Level Exercise 2012Document5 pagesRespiratory Physiology Adaptations To High-Level Exercise 2012Maria GrigoreNo ratings yet
- Impaired Gas Exchange NCPDocument4 pagesImpaired Gas Exchange NCPkimglaidyl bontuyanNo ratings yet
- Respiratory MCQDocument24 pagesRespiratory MCQfrabziNo ratings yet
- Chest RadiologyDocument129 pagesChest RadiologyNadiya SafitriNo ratings yet
- COPDDocument4 pagesCOPDitsmailbbkNo ratings yet
- Chronic CoughDocument6 pagesChronic CoughironNo ratings yet
- Acute Bronchiolitis Pathophysiology and ManagementDocument5 pagesAcute Bronchiolitis Pathophysiology and ManagementAtiqah ShahNo ratings yet
- Vih MT#2Document8 pagesVih MT#2cjNo ratings yet
- CLINICAL BronchiectasisDocument3 pagesCLINICAL BronchiectasisSyximsh FPNo ratings yet
- Chronic CoughDocument6 pagesChronic CoughironNo ratings yet
- Copd - Midterm NotesDocument2 pagesCopd - Midterm NotesInday BertaNo ratings yet
- Respiratory System SummaryDocument6 pagesRespiratory System SummaryKiara GovenderNo ratings yet
- Respiratory SystemDocument38 pagesRespiratory Systemjsreyes.402No ratings yet
- Nursing Care of Clients With Ventilation DisordersDocument6 pagesNursing Care of Clients With Ventilation DisordersLuna MarieNo ratings yet
- PneumoniaDocument2 pagesPneumoniama7moud farsNo ratings yet
- Respiratory SystemDocument55 pagesRespiratory SystemEndla SriniNo ratings yet
- Chest 2012-2013 Dr. Sameh LabibDocument83 pagesChest 2012-2013 Dr. Sameh LabibMahmoud AbouelsoudNo ratings yet
- PleurisyDocument4 pagesPleurisyJohiarra Madanglog TabigneNo ratings yet
- Lesson 6 -THORAX AND LUNGSDocument2 pagesLesson 6 -THORAX AND LUNGSKuldip GillNo ratings yet
- Vomiting of Gastrointestinal OriginDocument4 pagesVomiting of Gastrointestinal OriginFathimathNo ratings yet
- COPD: Chronic Obstructive Pulmonary Disease ExplainedDocument15 pagesCOPD: Chronic Obstructive Pulmonary Disease ExplainedMary Grace AgataNo ratings yet
- Acute Respiratory Failure Concept MapDocument1 pageAcute Respiratory Failure Concept Mapjenievysenerez100% (1)
- Respiration Short Cases: Why Recovering From DHF?Document1 pageRespiration Short Cases: Why Recovering From DHF?Darian AngNo ratings yet
- 242 - Respiratory Pathology COPD - Clinical FeaturesDocument3 pages242 - Respiratory Pathology COPD - Clinical FeaturesPranav PunjabiNo ratings yet
- Sweat Chloride Test: 1. Splenic Rupture 2. Avoid Sports and Physical Activity 3. Atypical LymphocytesDocument7 pagesSweat Chloride Test: 1. Splenic Rupture 2. Avoid Sports and Physical Activity 3. Atypical LymphocytesAnonymous GfqHQ5SNwNo ratings yet
- P1 Medworld Academy: Respiratory SystemDocument123 pagesP1 Medworld Academy: Respiratory SystemThenunda തേനുണ്ടNo ratings yet
- Suppurative Lung Diseases: DR Taher El Naggar Prof of Pulmonary Medicine Ain Shams UniversityDocument65 pagesSuppurative Lung Diseases: DR Taher El Naggar Prof of Pulmonary Medicine Ain Shams UniversitykingmedicNo ratings yet
- Alteration in Ventilatory FunctionDocument5 pagesAlteration in Ventilatory FunctionMary Danielle SaludarioNo ratings yet
- NCM 112 Lesson1Document9 pagesNCM 112 Lesson1Trisha LopezNo ratings yet
- CA1 MidtermsDocument30 pagesCA1 MidtermsJhonny pingolNo ratings yet
- Unit 1 5ADocument7 pagesUnit 1 5AArvin O-CaféNo ratings yet
- PEDIATRIC CHEST RADIOLOGY FINDINGSDocument2 pagesPEDIATRIC CHEST RADIOLOGY FINDINGSAnonymous HH3c17osNo ratings yet
- Lower Respiratory Tract DiseasesDocument4 pagesLower Respiratory Tract DiseasesJulia ManaloNo ratings yet
- 4.1 PEDIA-Pneumonia, Tuberculosis, Interstitial Lung Diseases (Dr. Bermejo)Document6 pages4.1 PEDIA-Pneumonia, Tuberculosis, Interstitial Lung Diseases (Dr. Bermejo)Monique BorresNo ratings yet
- Ca - MS (Respiratory)Document4 pagesCa - MS (Respiratory)kyleNo ratings yet
- PEDIA-Emphysema and Atelectasis, Overinflation Diseases of The Pleura, Pleural Effusion, Tumors (Dr. Talatala)Document2 pagesPEDIA-Emphysema and Atelectasis, Overinflation Diseases of The Pleura, Pleural Effusion, Tumors (Dr. Talatala)Monique BorresNo ratings yet
- Pneumonia Study GuideDocument5 pagesPneumonia Study GuideMartha Marty BalintNo ratings yet
- Respiratory FailureDocument5 pagesRespiratory Failureta CNo ratings yet
- FMAM2bis BPOCDocument38 pagesFMAM2bis BPOCLorena ZaroniuNo ratings yet
- MS LEC Reviewer Oxygenation Problems 1Document4 pagesMS LEC Reviewer Oxygenation Problems 1Shekinah GeriosaNo ratings yet
- Case Study: Submitted By: Jane Arian Berzabal Nbb2Document14 pagesCase Study: Submitted By: Jane Arian Berzabal Nbb2Jane Arian BerzabalNo ratings yet
- NCM 112 LEC Topic 2 Oxygenation Current Health History Physical Examination Normal Abnormal Breath Sounds Breathing PatternsDocument7 pagesNCM 112 LEC Topic 2 Oxygenation Current Health History Physical Examination Normal Abnormal Breath Sounds Breathing PatternsViviene Faye FombuenaNo ratings yet
- Ineffective Airway ClearanceDocument6 pagesIneffective Airway ClearanceKarl Angelo MontanoNo ratings yet
- AIR WAY DISEASE IMAGINGDocument60 pagesAIR WAY DISEASE IMAGINGMuhammad Faried FahdaNo ratings yet
- MCN KweenDocument4 pagesMCN KweenAngelo SigueNo ratings yet
- Respi PACES - V2Document6 pagesRespi PACES - V2Rebecca Teng Siew YanNo ratings yet
- NCM 112 NotesDocument6 pagesNCM 112 NotesKatrina Jhane MercadoNo ratings yet
- Patho RevDocument21 pagesPatho RevJo CastilloNo ratings yet
- Respiratory System I. FunctionDocument6 pagesRespiratory System I. Functionjgcriste100% (3)
- Pleural Conditions Arf Ards PeDocument4 pagesPleural Conditions Arf Ards PeNoreen PadillaNo ratings yet
- Bronchiolitis 44Document7 pagesBronchiolitis 44Fati NurNo ratings yet
- Fever and Cough 1Document34 pagesFever and Cough 1Alusio Navosailagi VUNIIVINo ratings yet
- Textbook Discussion On Acute Community-Acquired Pneumonia (BSN 3A-Group 6)Document9 pagesTextbook Discussion On Acute Community-Acquired Pneumonia (BSN 3A-Group 6)Jica Marie Bandiola GicaroNo ratings yet
- L95 NecropsyDocument7 pagesL95 NecropsyKING 5 News100% (1)
- Bronchopulmonary Dysplasia (BPD)Document13 pagesBronchopulmonary Dysplasia (BPD)Joan BuiNo ratings yet
- A and P Week 7Document3 pagesA and P Week 7api-316035237No ratings yet
- Chest PhysioDocument6 pagesChest PhysioGoha BashaNo ratings yet
- Diaphragm Dysfunction and Rehabilitation Strategy in Patients With Chronic Obstructive Pulmonary DiseaseDocument14 pagesDiaphragm Dysfunction and Rehabilitation Strategy in Patients With Chronic Obstructive Pulmonary DiseaseAdriana MartinezNo ratings yet
- 4th Quarter ExamDocument18 pages4th Quarter ExamSheba SalidoNo ratings yet
- Lung AuscultationDocument62 pagesLung AuscultationOlea CroitorNo ratings yet
- Department of Education Division of Leyte Taberna National High SchoolDocument5 pagesDepartment of Education Division of Leyte Taberna National High SchoolSheila May Tapales TabonNo ratings yet
- Ambush of Political Rivals Leaves 7 Dead, 1 WoundedDocument21 pagesAmbush of Political Rivals Leaves 7 Dead, 1 WoundedMarcus GilmoreNo ratings yet
- Lung Disease and Copd Seminar PresentationDocument14 pagesLung Disease and Copd Seminar Presentationapi-402325622No ratings yet
- Nursing Catalog - NascoDocument26 pagesNursing Catalog - NascomodiezhamNo ratings yet
- General principles of first aid aboard shipDocument10 pagesGeneral principles of first aid aboard shipCk DhiyanNo ratings yet
- HSNS264 A1 COPDDocument2 pagesHSNS264 A1 COPDKC Nilam100% (1)
- 4.6.3.cavitary Syndrome (19525)Document3 pages4.6.3.cavitary Syndrome (19525)Ioana DucaNo ratings yet
- G9 - Lesson 2Document9 pagesG9 - Lesson 2Khrean Kae SantiagoNo ratings yet
- Bill Nye RespirationDocument1 pageBill Nye RespirationJoseeNo ratings yet
- Bone and Joint AnatomyDocument6 pagesBone and Joint AnatomyMarco Tulio VázquezNo ratings yet
- Lung Expansion 1Document31 pagesLung Expansion 11trindogg100% (2)
- 4444444412Document5 pages4444444412Demiar Madlansacay QuintoNo ratings yet
- What Happens When You Breath Niric Acid FumesDocument4 pagesWhat Happens When You Breath Niric Acid FumesAFLAC ............No ratings yet