Professional Documents
Culture Documents
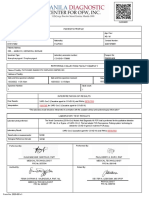
MEDICAL CERTIFICATION
Uploaded by
Dasha VeeOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
MEDICAL CERTIFICATION
Uploaded by
Dasha VeeCopyright:
Available Formats
F.
08 MEDICAL CERTIFICATION OF DEATH REGISTRABLE ACTS & VITAL EVENTS
Dr. Tubera-Panes | May 7, 2019
DEATH
Outline refers to the permanent disappearance of all evidence of life
I. Death Registration at any time after live birth has taken place, or
A. Place of Registration the postnatal cessation of vital functions without capability of
B. Persons Responsible to Report, Prepare and Certify Death resuscitation
II. Guidelines in Filling out and Completing a Death Certificate For those patients whom you will make a death certificate, it
III. Guidelines for Reporting Causes of Death in Specific Groups and means that they also have a birth certificate. You cannot
Conditions make a death certificate without a birth certificate.
“We have to be careful in filling up a death certificate because only a FETAL DEATH
doctor can certify the cause of death.” a. death prior to the complete expulsion or extraction from its
mother of a product of conception, irrespective of the
I. DEATH REGISTRATION duration of pregnancy
b. the death is indicated by the fact that after such separation the
Importance of Vital Statistics for Health Sector fetus does not breathe nor show any other evidence of
Primary source of public health information on births and causes of infant, life, such as beating of the heart, pulsation of the umbilical
neonatal and maternal deaths in a defined population. cord, or definite movement of voluntary muscles.
1. Data on prevalence and distribution of mortality by cause c. If the fetus has an intra-uterine life of less than 7 months, it is
2. Identification of health inequalities not deemed born if it dies within twenty-four hours after
3. Resource allocation its complete delivery from the maternal womb.
4. Assessment of health systems performance
5. Understanding emerging health challenges
Act. No 3753
CIVIL REGISTRY LAW
Approved on November 26, 1930 and took effect on February 27,
1931
Made compulsory the registration of all facts and acts
concerning the civil status of persons from birth to death,
including the changes in civil status taking place therein in
appropriate civil registry books
Sec. 6: Death Certificate and Register:
No human body shall be buried unless the proper death
certificate has been presented and recorded in the office of the local
civil registrar.
PD 856
CODE OF SANITATION OF THE PHILIPPINES Guide to when to register the fetus and what form to use.
Approved on December 23, 1975 ** COBD: Certificate of Live Birth; COD: Certificate of Death
The burial or cremation of remains is subject to the following
requirements: THE CIVIL REGISTRATION PROCESS
a) No remains shall be buried without a Certificate of
Death, which shall be issued by the attending DEATH
physician. ↓
Person Responsible
b) If there has been no physician in attendance, it shall be Attendant at Death/ Local Health Officer/ Informant
issued by the mayor or the secretary of the (Within 30 days from the time of occurrence)
municipality where the death occurred.
↓
c) The death certificate shall be forwarded to the local civil Local Civil Registrar (City/ Municipal)
registrar within 48 hours after death (Sec. 91). Registers event and combines events on a monthly basis;
Should be done and submitted within 10 days following the month
d) For Muslim Filipinos, of registration
In accordance with Islamic law and jurisprudence,
the dead body may be buried without a Certificate ↓
of Death provided that the death shall be reported by PSA-Provincial Office
the person who performed the burial rites (or by the Should submit within 60 days after the reference month
nearest kin) to the local health officer within 48 hours
after the date of burial. ↓
- It is their tradition that the body has to be buried PSA-Central Office
within 24 hours.
Transcribers: AQUINO, VARGAS, BALINO Page 1 of 7
A. PLACE OF REGISTRATION The surgical pathology report signed and issued by the pathologist
As a general rule, the place of registration is the city or shall serve as the Certificate of Dismembered Body Part
municipality where the event occurred. which may be used for burial purposes or proper disposal.
For example, a vehicular accident happened in Tuba, Benguet. The practice of issuing a Certificate of Death by the attending
Where will they report the death? In Tuba. Not in Baguio General physician for the dismembered body part is not necessary.
Hospital even if the patient was brought there.
DEATHS THAT OCCURRED OUTSIDE THE HOSPITAL
Reporting of Vital Events of Filipinos Occurring Abroad If the deceased died without medical attendance, the nearest
(Living permanently or temporarily) relative or any person who has knowledge of the death is
shall be reported to the Philippine Foreign Service Establishment of responsible for reporting the event to the local health officer
the country of residence; or within 48 hours.
where the vital event took place; or The local health officer is the one who will prepare the Certificate
where none is located thereat, in the Philippine Foreign Service of Death, certify the cause(s) of death, review and direct its
Establishments of the country nearest the place of residence of registration at the Office of the Local Civil Registrar (LCRO)
the party concerned; or within 30 days.
where the vital event occurred
When the death occurs in the ambulance while a patient is being
B. PERSONS RESPONSIBLE TO REPORT, PREPARE & CERTIFY transferred to another healthcare facility, the attending
DEATH physician during the transport of the patient shall
accomplish the death certificate.
HOSPITAL DEATH
The physician who last attended the deceased or the In the absence of the local health officer, the death should be
reported to the mayor, or to any member of the Sangguniang
administrator of the hospital or clinic where the person died
Bayan, or to the municipal secretary who shall issue the
is responsible to prepare the Certificate of Death and certify as to
the cause of death. Certificate of Death for burial purposes.
The certificate is forwarded, within 48 hours after death, to the
Issue the death certificate for burial purposes only and not to
local health officer who will review the certificate and affix his
certify the death. It will just ascertain that death has occurred
signature in the “Reviewed By” portion and direct its
for burial purposes.
registration at the Office of the LCR within 30 days.
o DEATH IN HOSPITAL EMERGENCY ROOM (ER) DEATH UNDER MEDICO-LEGAL EXAMINATION
Refers to deaths of patients occurring in the ER, including When faced with the duty of completing the Medical Certificate
patients who were revived by initial resuscitative measures at the portion of the Certificate of Death, the physician has to determine
ER but eventually died there, regardless of the time of stay in first and foremost whether the death is reportable or not and then,
ER. determine whether another physician is more qualified to
In such cases, the Certificate of Death shall be accomplished complete the certificate especially if the deceased was attended by
by the ER Officer if he can provide a definite diagnosis. another physician prior to his death.
Otherwise, the death should be referred to the medico- For a medico legal case and there is someone is more competent
legal officer of the hospital or the local health officer who shall than you then you let that someone (medico-legal officer) fill that up.
cause the issuance of the Certificate of Death.
If the physician has reasons to believe or suspect that the cause
If the ER doctor cannot come up with a definite diagnosis, of death was due to violence or crime (or that he is dealing with a
then the medico-legal officer of the hospital will prepare the medico-legal case), then he is duty-bound to immediately report
certificate. to the authorities of the Philippine National Police (PNP) or
the National Bureau of Investigation (NBI) concerned.
o DEATH IN THE AMBULANCE
When a death occurs in the ambulance while the patient is being DEATH OF A MUSLIM OR INDIGENOUS PEOPLE
transferred to another healthcare facility, the attending physician For Filipino Muslim, Indigenous Cultural Communities/Indigenous
during the transport of the patient shall accomplish the Certificate Peoples (ICCs/IPs), the dead body may be buried even without a
of Death. Certificate of Death provided that the death shall be reported to the local
health officer within 48 hours after the date of burial.
Death Registration Process The local health officer shall prepare the COD, certify the cause
Death in a Hospital of death and submit the COD to the LCR for registration.
↓ (48 hours) Aside from the COD/COFD, it is required to have an attachment
Local Health Officer which shall constitute the facts of occurrence of the event.
↓ (28 days) Municipal Form 103 - Attachment for Muslim Death
Local Civil Registrar IP Form 2 – Attachment for death of ICCs/Indigenous Peoples
CERTIFYING DISMEMBERED BODY PARTS REMINDER:
In cases when a dismembered body part which is non-viable for Entries in the Medical Certificate must be accomplished by
attachment is brought to the ER, such body part shall be the attending physician/local health officer/medico-legal officer
forwarded to the surgical pathology section of the correctly and completely before registration since there is
laboratory for gross and microscopic examination and prohibition against change or correction of entries without
documentation. judicial order.
*Art. 412, Civil Code of the Philippines
Transcribers: AQUINO, VARGAS, BALINO Page 2 of 7
Please do not sign a blank death certificate just because you are in III. GUIDELINES FOR REPORTING CAUSES OF DEATH IN
a hurry. There was an instance where a blank death certificate was SPECIFIC GROUPS OR CONDITIONS
signed and they placed the name of a living criminal so the criminal
is at large but registered that he died. It is a legal document so Specific Groups/Condition
you can lose your license because of that. 1. Elderly
2. Maternal Death
3. Fetal Death
PERSON/S RESPONSIBLE TO CERTIFY DEATH 4. Infant Death
5. Death involving External Injuries
If there is a medical attendant at death, the certifying officer is the
6. Death from Infection
attendant at death.
7. Death from Neoplasm
If there is no medical attendant at death the certifying officer is the
Local Health Officer
In medico-legal cases, the certifying officer is the medico-legal 1. ELDERLY DECEDENT
officer Some elderly people may have several established medical
In ALL cases, the cause of death shall be reviewed and signed by conditions and they seem not to die from them but from “old
the Local Health Officer age”
Most of the elderly apparently die “with the disease” and not from
the disease
USES OF CERTIFICATE OF DEATH
Old age
Prima facie evidence of death
Senility Little value on public
Claim of benefits, pensions, insurance, or tax exemption
Senescence health planning and
Evidence for settlement of estate
Advanced age research
Remarriage purpose of surviving spouse
Multi-organ failure
Designation of a guardian or foster parent for minor
Determine health priorities for prevention of deaths due to similar
causes in the future
These are not accepted as a cause of death. If you place one of
The information is also important for family members so that they
these diagnoses, then it becomes a garbage code. It will not
know what caused the death and are aware of conditions that may
be part of our statistics. You can put it in other causes.
occur or could be prevented in other family members
REMEMBER!
II. GUIDELINES ON FILLING OUT AND COMPLETING A
Entry for the age of deceased is already recorded elsewhere
CERTIFICATE OF DEATH
and it serves no purpose repeating the apparent age of the
Be familiar with the form
deceased in the cause of death statement.
Certificate of Death Form (light blue)
To be useful, the cause-of-death entry must be specific,
o Municipal Form no. 103
clear and with distinct etiological sequence.
Certificate of Fetal Death Form (pink)
o Municipal Form no. 103A
If there is uncertainty in the entries for the causes of death,
** Green is for the birth certificate.
it is always acceptable to use qualifying terms such as
“probable” or “presumed”.
GENERAL GUIDELINES
If the cause of death cannot be determined with reasonable
1. NO ERASURES/ALTERATIONS medical probability but seems to be due solely to a natural cause,
Affect validity of the certificate the certifier may report “Undetermined Natural Cause” as
Altered certificate may be rejected by the Local Civil Registry entry in the cause-of-death statement.
2. NO ABBREVIATIONS OR MEDICAL SYMBOLS CASE SAMPLE:
No T/C, 2°, no NSVD, no TB, etc. A 95-year old man was found dead on bed by his wife. He had chronic mild
The only acceptable abbreviations are HIV and AIDS. hypertension controlled by medication. His previous chest x-ray shows mild
cardiomegaly, consistent with chronic hypertension. There was no suspicion
3. Complete each item LEBIGLY of evidence of foul play. No specific cause of death could be identified.
Computer printer (Black ink)
Typewriter (Black ribbon)
Print with pen (permanent Black ink)
We do not already accept a hand written COD.
When signing the document use black ink not blue. If you
use blue ink, the signatures cannot be seen once PSA
photocopies them.
The certifier must also be aware of common complications that may cause
one to overlook and fail to report the underlying cause in elderly decedent
Transcribers: AQUINO, VARGAS, BALINO Page 3 of 7
3. FETAL DEATH
Death of a fetus prior to complete expulsion of a product of
conception irrespective of the period of pregnancy
For fetus to have NO evidence of life:
2. DEATH INVOLVING WOMEN OF CHILD-BEARING AGE No heart beat
No Umbilical cord pulsation
o MATERNAL DEATH: No voluntary movement
Death of woman while pregnant or within 42 days of
termination of pregnancy, irrespective of the duration and the
site of pregnancy, from any cause related to or aggravated by the
pregnancy or its management but not from accidental or incidental
causes
CASE SAMPLE 1
A 38 year old G3P2 was admitted at a birthing facility while 34 weeks
pregnant. After six hours of premature labor, she delivered a stillborn
baby boy with cord around his neck. The fetus is cyanotic with no gross
fetal movement and no heartbeat.
**19c. Maternal Condition (if the deceased is female 15-19 y.o)
The fact that women died during pregnancy or within 42 days
of the termination of pregnancy should be clearly indicated under
Maternal Condition.
CASE SAMPLE 2
A 40-year old G8P7 was admitted at a District Hospital for induction of
Information from Maternal Condition labor. Ultrasound of the fetus at 36 weeks revealed the presence of
Used in health research and statistics anencephaly. A stillborn anencephalic fetus weighing 1500g was
Used to identify those cases that need to be included in the Maternal delivered.
Death Review
CASE SAMPLE:
A 36-year old G5P3A1 woman who delivered a full-term baby boy at home
was brought to the ER because of placental retention. The woman
apparently had severe bleeding and was hypotensive on her arrival at ER.
She was transfused whole blood and manual extraction of the placenta
was performed. However, the woman died four hours after delivery.
Transcribers: AQUINO, VARGAS, BALINO Page 4 of 7
4. INFANT DEATH REMEMBER!
Death involving infants aged 0-7 days o Enter in narrative form, a brief but specific and clear
Same form of COD (Municipal Form 103) description of how the injury occurred
Fell off ladder while painting house
Medical Certificate portion (item 19a) found at the back of the Driver of car ran off roadway
form is filled out instead of the one in front
o Specify
Type of gun (handgun, hunting rifle, etc.)
Type of vehicle (car, bulldozer, train,…)
o For motor vehicle accident, indicate whether the decedent was a
driver, passenger, or pedestrian
o Activity in which the decedent was engaged during the injury (Playing
sports, working at house, hanging out of bar)
o Fill out all the blanks as much as possible. Always specify if autopsy
is done *Yes/No. The interval between the onset and death should
The mode of dying (asphyxia, heart failure, anoxia), including always be in hours or minutes (not the exact time).
prematurity, should not be entered in section (a) unless it was the only
known condition.
CASE SAMPLE:
A 38-year old G3P0A2 was admitted at a birthing facility while 24 weeks
pregnant. She has been having premature labor for six hours. She
subsequently delivered 700g infant who was treated at the intensive
neonatal care unit but subsequently died after 24 hours. Chest X-ray of
the infant shows dense lung fields consistent with severe hyaline
membrane disease.
CASE SAMPLE 1
A 21 year-old female was critically injured in an automobile accident and
died from a fractured skull causing cerebral contusion soon after 30 min
of being brought to the hospital. Police records show that she was the
driver in a two-car collision that occurred at 2:15 am at the corner of 21st
Street and Ash Street.
5. DEATH INVOLVING EXTERNAL INJURIES
External cause or events Underlying Cause
Identify the bodily trauma Antecedent Cause
caused by the external events
Fatal derangement from bodily Immediate Cause
trauma
CASE SAMPLE 2
A 25 year old male was admitted to the hospital with a gunshot wound
to the head. He had been home in his study cleaning his gun when the
External Events External agent or force, usually physical or shot was fired at approximately 9 pm. He died at 11:05 pm on the same
chemical in nature, that causes trauma. day. Autopsy showed contact gunshot of right temple.
Trauma Injury or damage to bodily tissues or its
functions.
Fatal The resulting anatomic or functional
derangement derangement that causes death.
Transcribers: AQUINO, VARGAS, BALINO Page 5 of 7
o Help identify the underlying cause of death
o More often than not, the primary site is the underlying
cause of death.
6. DEATH DUE TO INFECTIONS If a secondary growth is included in the sequence of events
The certifier has to report: leading to death, state the site of secondary growth as due to the site of
Manifestation or body site primary growth.
Causative agent (if known) / “Cause Unknown”
Source and Route of Infection
E.g. food poisoning, contaminated blood product, health care
associated infection
o Behavior of the tumor – benign or malignant
o Nature or histological type (if known)
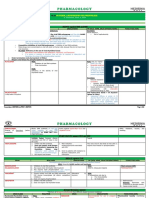
QUICK POINTS
CONDITION GUIDELINE
1. ELDERLY SENILITY, OLD AGE, SENESCENCE, etc. are
Specify also any underlying disease that may have suppressed the DEATHS not causes of death
patient’s imunity that made him susceptible to the infection that led to RULE OUT: abuse, neglect, suicides,
his death. (e.g. malnutrition -> Made the patient susceptible to inconspicuous injuries
gastroenteritis) DETERMINE: if the conditions is a
COMPLICATION of the true underlying
cause
2. MATERNAL Fill out #19c: Maternal Condition
DEATHS
3. FETAL DEATHS Fill out C O F D
4. INFANT Fill our C O D
DEATHS BACK, for infants aged <7 days old
FRONT, for infants ages >8 days old
5. EXTERNAL FATAL DERANGEMENT is the ICOD
INJURY BODILY TRAUMA is the ACOD
EXTERNAL EVENT is the UCOD
o HIV Fill out #19d: Manner of death, Place of
HIV is accepted as underlying cause of death except death
when due to conditions requiring blood transfusion 6. INFECTION Specify site/ manifestation
Haemophilia and anaemia Specify causative organism/ “cause
Major injuries unknown”
Surgeries Specify if primary or secondary
Drug addictions If PRIMARY: specify if bacterial or viral
If SECONDARY: specify primary infection
If the health care associated infection was part of the sequence Specify ROUTE: community-acquired,
leading to death, it should be reported in Part I, then include all conditions hospital/heathcare-acquired, etc.
in sequence of events back to the original disease being treated. Specify CONDITION causing
immunosuppresion
7. NEOPLASM/ Specify:
7. DEATH FROM NEOPLASM TUMOR BEHAVIOR (Benign or Malignant)
Specific site of neoplasm LOCATION
Public health prevention strategies differ markedly from one PRIMARY (if known) and/or SECONDARY
type of neoplasm to another IF SECONDARY: identify the primary as the
UCOD
Primary site must be stated HISTOLOGY (if known)
o Even if it has long been removed before death
o If unknown, write “Primary Unknown”
Transcribers: AQUINO, VARGAS, BALINO Page 6 of 7
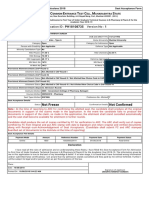
PERSONS RESPONSIBLE QUICK POINTS CHECKPOINT:
DEATH REPORT PREPARE CERTIFY T/F:
Hospital Attendant Attending Attending 1. All death certificates must be hand written in blue ink.
at Death physician physician to 2. The color of the infant death certificate is pink while green for
be reviewed adults
by LHO 3. No remains shall be buried without a Certificate of Death, which
ER Attendant If can provide Attending shall be issued by the attending physician, regardless of race,
at Death definitive physician to religion and culture.
diagnosis: ER be reviewed 4. Filipinos who were born in the country but died outside the
officer by LHO country does not need to be reported to Filipino authorities
5. Identify the Cause of death:
If not: medico- A 25 year old male was admitted to the hospital with a gunshot
legal officer of the wound to the head. He had been home in his study cleaning
hospital his gun when the shot was fired at approximately 9 pm. He
Ambulance Attendant Attending Attending died at 11:05 pm on the same day. Autopsy showed contact
at Death physician during physician to gunshot of right temple.
the transport be reviewed
by LHO Answers: 1-4. F 5. Page 5
Dismembered Informant Surgical Pathology section will
Body Parts accomplish Certificate of
Dismembered Body Part for REMARKS:
disposal and burial purposes. For more examples and step-by-step guide: Kindly refer to the
Outside Nearest Local Health Local Health Medical Certification of Death: Handbook for Filipino Physicians by DOH
Hospital, relative or Officer (LHO) Officer (LHO)
without any person https://www.doh.gov.ph/sites/default/files/publications/MEDICAL_CERT
medical who has If LHO is not IFICATION_OF_DEATH_0.pdf
attendance knowledge available: Mayor
of the or Sangguniang
death Bayan, or
Municipal
Secretary
Under Physician Physician has to Medico-legal
Medico-legal has to determine Officer
Examination determine whether another
if it is physician is more
reportable qualified to
or not complete the
certificate; OR
PNP/ NBI/ Medico-legal
LHO officer
Muslim Nearest Local Health Local Health
relative or Officer Officer
any person
who has
knowledge
of the
death
Transcribers: AQUINO, VARGAS, BALINO Page 7 of 7
You might also like
- Overview of New Death Certificate PDFDocument59 pagesOverview of New Death Certificate PDFFaisol KabirNo ratings yet
- 87 Year Old Man Dies in ChennaiDocument1 page87 Year Old Man Dies in ChennaiAdmirable AntoNo ratings yet
- QSTR06319 Oliver John PDFDocument1 pageQSTR06319 Oliver John PDFJohn OliverNo ratings yet
- Government of Assam Department of Health and Family Welfare Urban PHC SilcharDocument1 pageGovernment of Assam Department of Health and Family Welfare Urban PHC Silcharurbanphcsilchar094No ratings yet
- Member Data Record: Philippine Health Insurance CorporationDocument1 pageMember Data Record: Philippine Health Insurance CorporationKristine OgalescoNo ratings yet
- T2100001419 ML2100001252 115620 6691600 19370729 $mole-DefauDocument2 pagesT2100001419 ML2100001252 115620 6691600 19370729 $mole-DefauPeony03No ratings yet
- QSTR06409 Jovenal Jomar PDFDocument1 pageQSTR06409 Jovenal Jomar PDFJohn OliverNo ratings yet
- Ticf Kà¡Mà) ©MB V Hip V: Name of Local Government Issuing Certificate Adimaly Grama PanchayatDocument1 pageTicf Kà¡Mà) ©MB V Hip V: Name of Local Government Issuing Certificate Adimaly Grama PanchayatjmsmediaNo ratings yet
- S60 - Fofo Greater Noida Shop No.-5, LGF, Amrapali Leisure Valley Greater Noida West (U.P)Document2 pagesS60 - Fofo Greater Noida Shop No.-5, LGF, Amrapali Leisure Valley Greater Noida West (U.P)Deepanshu Singh KushwahaNo ratings yet
- Sars-Cov-2 (Covid 19) Detection (Qualitative) by Real Time RT PCRDocument3 pagesSars-Cov-2 (Covid 19) Detection (Qualitative) by Real Time RT PCRAmbareen AbidNo ratings yet
- Lab No. Age/Gender Coll. On Name Reg. On Ref. Dr. Approved On 16/aug/2021 03:05PM Rpt. Centre Printed OnDocument1 pageLab No. Age/Gender Coll. On Name Reg. On Ref. Dr. Approved On 16/aug/2021 03:05PM Rpt. Centre Printed OnPratik GargNo ratings yet
- Medical Report Umum, TkiDocument3 pagesMedical Report Umum, Tkimater0% (1)
- InvoiceNo 44515Document1 pageInvoiceNo 44515sabumathewNo ratings yet
- COVID-19 Diagnostic Report SummaryDocument2 pagesCOVID-19 Diagnostic Report SummaryHemant ChaurasiaNo ratings yet
- Lab ResultDocument1 pageLab ResultShubhNo ratings yet
- End of Report : Scan To Validate ReportDocument1 pageEnd of Report : Scan To Validate ReportDharmendra KumarNo ratings yet
- Amit Sahoo - 25 08 2021Document2 pagesAmit Sahoo - 25 08 2021Fan Of MinecraftNo ratings yet
- RTPCR 28191Document1 pageRTPCR 28191Venkatesh LGNo ratings yet
- Admission LetterDocument18 pagesAdmission LetterBridget WardNo ratings yet
- Youth LoanDocument7 pagesYouth LoanKASHIF NAWAZNo ratings yet
- Rellance: Laikshmlovaa PDST, Dasanaputa Holl Tanna LnreDocument16 pagesRellance: Laikshmlovaa PDST, Dasanaputa Holl Tanna LnreSanthosh RNo ratings yet
- Lab Report NewDocument3 pagesLab Report Newhacebe2685No ratings yet
- Laboratory Report /:: Dis. At:::::: 31 Years 0122201673 Male Mr. Shakti Singh GaurDocument2 pagesLaboratory Report /:: Dis. At:::::: 31 Years 0122201673 Male Mr. Shakti Singh GaurShakti singh gaur100% (1)
- Lab ReportDocument1 pageLab ReportNishantNo ratings yet
- Hematology report shows reactive neutrophilic leucocytosisDocument1 pageHematology report shows reactive neutrophilic leucocytosis112345678900No ratings yet
- West Bengal Health Recruitment Board: Advertisement NoDocument2 pagesWest Bengal Health Recruitment Board: Advertisement NoSoumya BhattacharyaNo ratings yet
- Behram KhanDocument29 pagesBehram KhanAmrinder SinghNo ratings yet
- Information About Machine Readable PassportDocument7 pagesInformation About Machine Readable Passportnedian_2006No ratings yet
- Form PDocument2 pagesForm PMega No01No ratings yet
- Homepage Verisys Individual-Record: January 1, 1985Document2 pagesHomepage Verisys Individual-Record: January 1, 1985Zeeshan QadriNo ratings yet
- Molecular Diagnostics: Assay Name Result Sars Cov-2 (Real Time RT-PCR)Document2 pagesMolecular Diagnostics: Assay Name Result Sars Cov-2 (Real Time RT-PCR)AdibNo ratings yet
- COVID-19 RT-PCR Test ReportDocument1 pageCOVID-19 RT-PCR Test ReportDv RasminaNo ratings yet
- CLL PatientReportDocument1 pageCLL PatientReportabdullahqqNo ratings yet
- A (I) Domicile Certificate Issuing UP State Authority SDM A (Ii) Date of Issuing Domicile Certificate (DD/MM/YYYY)Document2 pagesA (I) Domicile Certificate Issuing UP State Authority SDM A (Ii) Date of Issuing Domicile Certificate (DD/MM/YYYY)Anonymous oF3LBeZAdQNo ratings yet
- Lab Reports CancellationDocument46 pagesLab Reports CancellationArely Rea LariosNo ratings yet
- Im MegrationDocument4 pagesIm MegrationProf Dr Md Saifur RahmanNo ratings yet
- Sy2zgra5gtbxj1pd1jwv4sfoDocument2 pagesSy2zgra5gtbxj1pd1jwv4sfoDivin IychandaNo ratings yet
- 05062023CA6901RDocument1 page05062023CA6901Rasad922No ratings yet
- Application Form 40757Document3 pagesApplication Form 40757SHAX OP100% (1)
- Kolej Teknologi Darulnaim: Darulnaim College of TechnologyDocument5 pagesKolej Teknologi Darulnaim: Darulnaim College of TechnologyDaryanto SutejiNo ratings yet
- Aadhaar Update Form: Aadhaar Enrolment Is Free & VoluntaryDocument4 pagesAadhaar Update Form: Aadhaar Enrolment Is Free & VoluntarySið PrasaðNo ratings yet
- Medical CertificateDocument1 pageMedical CertificateAkhilesh KumarNo ratings yet
- Pak IdentityDocument5 pagesPak Identityfatima GhazanfarNo ratings yet
- Ashish Nursingofficer - Aiimsexams.org - RegistrationSlip PDFDocument2 pagesAshish Nursingofficer - Aiimsexams.org - RegistrationSlip PDFAru VermaNo ratings yet
- Official MDR PDFDocument1 pageOfficial MDR PDFBesarioLouiseCassandraNo ratings yet
- Fulbright Certificate of HealthDocument8 pagesFulbright Certificate of HealthLinda Klimavicius100% (1)
- LabResultTempPDF CJ0304865Document2 pagesLabResultTempPDF CJ0304865Jahred EstebanNo ratings yet
- Print Application FormDocument8 pagesPrint Application FormbonfaceNo ratings yet
- S C E T C M S: Application ID: PH18108735 Version No: 1Document1 pageS C E T C M S: Application ID: PH18108735 Version No: 1nirbhay mouryaNo ratings yet
- Lab Report 13747633 20230722013611Document5 pagesLab Report 13747633 20230722013611FazilNo ratings yet
- IKPEOGU MARTIN IFEANYI 2023-05-18-12-38 Incomplete ApplicationDocument12 pagesIKPEOGU MARTIN IFEANYI 2023-05-18-12-38 Incomplete ApplicationDp100% (1)
- Naheed Imtiaz family certificateDocument1 pageNaheed Imtiaz family certificateHassan ChaudhryNo ratings yet
- Indian-Patient: Christian Medical CollegeDocument1 pageIndian-Patient: Christian Medical Collegesasthi100% (1)
- Government of Andhra Pradesh Panchayat Raj Department Form - A (See Section - 12)Document1 pageGovernment of Andhra Pradesh Panchayat Raj Department Form - A (See Section - 12)y.d.dastagiriNo ratings yet
- Financial AnalysisDocument6 pagesFinancial AnalysisRinceNo ratings yet
- Uzair Baloch JitDocument36 pagesUzair Baloch JitanymanNo ratings yet
- Appointment SlipDocument3 pagesAppointment SlipAbdullahi AbdulbadiuNo ratings yet
- Admission Form: Ma-Pakistan Studies-Part-I (Fresh), 2nd Annual-2022Document2 pagesAdmission Form: Ma-Pakistan Studies-Part-I (Fresh), 2nd Annual-2022sikanderNo ratings yet
- Claim Form - Part A' To 'Claim Form For Health Insurance PolicyDocument6 pagesClaim Form - Part A' To 'Claim Form For Health Insurance PolicyMruthunjaya Reddy LakkamNo ratings yet
- Its Is If Is in of Of: Only Also, or ThisDocument1 pageIts Is If Is in of Of: Only Also, or ThisMonica BorjaNo ratings yet
- OB OSCE.06 OB GYNE ULTRASOUND (Dr. Ursua) PDFDocument1 pageOB OSCE.06 OB GYNE ULTRASOUND (Dr. Ursua) PDFDasha VeeNo ratings yet
- Pulmonary Disorders in PregnancyDocument5 pagesPulmonary Disorders in PregnancyDasha VeeNo ratings yet
- F.07 STD AND INFECTIONS IN PREGNANCY (DR - Jandoc) 05-03-2019 (Part 2)Document3 pagesF.07 STD AND INFECTIONS IN PREGNANCY (DR - Jandoc) 05-03-2019 (Part 2)Dasha VeeNo ratings yet
- F.03 HEMATOLOGIC DISEASES IN PREGNANCY (DR - Taguiling) 04-25-2019 (Part 1) PDFDocument4 pagesF.03 HEMATOLOGIC DISEASES IN PREGNANCY (DR - Taguiling) 04-25-2019 (Part 1) PDFDasha VeeNo ratings yet
- Pulmonary Disorders in PregnancyDocument5 pagesPulmonary Disorders in PregnancyDasha VeeNo ratings yet
- Philippine Journal of Gynecologic Oncology Volume 9 Number 1 2012Document48 pagesPhilippine Journal of Gynecologic Oncology Volume 9 Number 1 2012Dasha VeeNo ratings yet
- WJR 5 113Document13 pagesWJR 5 113Valian IndrianyNo ratings yet
- Practice Bulletin: Management of Adnexal MassesDocument14 pagesPractice Bulletin: Management of Adnexal MassesDasha VeeNo ratings yet
- The Characteristic Ultrasound Features of Specific Types of Ovarian Pathology (Review) PDFDocument14 pagesThe Characteristic Ultrasound Features of Specific Types of Ovarian Pathology (Review) PDFDasha VeeNo ratings yet
- Diagnostico y Manejo de Masas AnexialesDocument6 pagesDiagnostico y Manejo de Masas AnexialesChristopher Hernán Valenzuela ArancibiaNo ratings yet
- F.01 NEUROLOGIC AND PSYCHIATRIC DISEASES IN PREGNANCY (Dr. Arcellan) 04-10-2019 PDFDocument10 pagesF.01 NEUROLOGIC AND PSYCHIATRIC DISEASES IN PREGNANCY (Dr. Arcellan) 04-10-2019 PDFDasha VeeNo ratings yet
- F.02 DERMATOLOGIC DISEASES IN PREGNANCY (Dr. Taguiling) 04-12-2019 PDFDocument5 pagesF.02 DERMATOLOGIC DISEASES IN PREGNANCY (Dr. Taguiling) 04-12-2019 PDFDasha VeeNo ratings yet
- 2011 Full Page Calendar - TomKat StudioDocument12 pages2011 Full Page Calendar - TomKat StudioThe TomKat StudioNo ratings yet
- P.09 OBSTETRIC HEMORRHAGE (Dr. Ursua) 02-07-2019 (Part 1)Document3 pagesP.09 OBSTETRIC HEMORRHAGE (Dr. Ursua) 02-07-2019 (Part 1)Dasha VeeNo ratings yet
- F.07 STD AND INFECTIONS IN PREGNANCY (DR - Jandoc) 05-03-2019 (Part 2)Document3 pagesF.07 STD AND INFECTIONS IN PREGNANCY (DR - Jandoc) 05-03-2019 (Part 2)Dasha VeeNo ratings yet
- Antiviral Chemotherapy and Prophylaxis: Acyclovir, Valacyclovir, and FamciclovirDocument8 pagesAntiviral Chemotherapy and Prophylaxis: Acyclovir, Valacyclovir, and FamciclovirDasha VeeNo ratings yet
- F.06 STD and Infections in Pregnancy (Dr. Jandoc) 05-03-2019 (Part 1)Document5 pagesF.06 STD and Infections in Pregnancy (Dr. Jandoc) 05-03-2019 (Part 1)Dasha VeeNo ratings yet
- Obstetrics 2: Obstetric Hemorrhage (Part 2)Document4 pagesObstetrics 2: Obstetric Hemorrhage (Part 2)Dasha VeeNo ratings yet
- P.07 Thyroid and Parathyroid Glands Dr. Manalo 9-8-16Document4 pagesP.07 Thyroid and Parathyroid Glands Dr. Manalo 9-8-16Dasha VeeNo ratings yet
- DiagnosisDocument8 pagesDiagnosisDasha VeeNo ratings yet
- Thyroid PDFDocument9 pagesThyroid PDFDasha VeeNo ratings yet
- Embryogenesis & Fetal DevelopementDocument38 pagesEmbryogenesis & Fetal DevelopementDasha Vee100% (1)
- Mental HealthDocument4 pagesMental HealthDasha VeeNo ratings yet
- m.13 Dietary Supplements & Herbal Medications (Dr. Buñag) 04-04-18Document4 pagesm.13 Dietary Supplements & Herbal Medications (Dr. Buñag) 04-04-18Dasha VeeNo ratings yet
- F.09 BONE RADIOLOGY - Dr. GalangDocument11 pagesF.09 BONE RADIOLOGY - Dr. GalangDasha VeeNo ratings yet
- M.10B Drugs Used in Gastrointestinal DisordersDocument3 pagesM.10B Drugs Used in Gastrointestinal DisordersDasha VeeNo ratings yet
- Philippine CPG On The Diagnosis and Management of Urinary Tract Infections in Adults-2015 Update - Part 2 PDFDocument140 pagesPhilippine CPG On The Diagnosis and Management of Urinary Tract Infections in Adults-2015 Update - Part 2 PDFspringdingNo ratings yet
- Ob Osce.04 CTG ReadingDocument6 pagesOb Osce.04 CTG ReadingDasha VeeNo ratings yet
- f.02 Intellectual Disabilities (Dr. Rebucal) 04-11-2019Document4 pagesf.02 Intellectual Disabilities (Dr. Rebucal) 04-11-2019Dasha VeeNo ratings yet
- Olivia Gant Case/ Turner Kelly Renee IndictmentDocument17 pagesOlivia Gant Case/ Turner Kelly Renee IndictmentLeigh EganNo ratings yet
- MRI BRAIN FINAL DR Shamol PDFDocument306 pagesMRI BRAIN FINAL DR Shamol PDFDrSunil Kumar DasNo ratings yet
- Infectia Cu H Pylori 2020Document18 pagesInfectia Cu H Pylori 2020alexandra elenaNo ratings yet
- Skin Pigmentation + Hari DisorderDocument113 pagesSkin Pigmentation + Hari DisorderAfiqah So JasmiNo ratings yet
- Rate ListDocument34 pagesRate ListIrum QayyumNo ratings yet
- Medorog Visheshank March 2008Document8 pagesMedorog Visheshank March 2008Mitra PathakNo ratings yet
- Nursing Care Plan FinalDocument16 pagesNursing Care Plan FinalErickson OcialNo ratings yet
- Orthopedics TraumatologyDocument8 pagesOrthopedics TraumatologyCpopNo ratings yet
- Chapter 12 Prenatal CareDocument7 pagesChapter 12 Prenatal CareTristan Paolo RamosNo ratings yet
- Notice: Meetings: Genetics, Health, and Society, Secretary's Advisory CommitteeDocument2 pagesNotice: Meetings: Genetics, Health, and Society, Secretary's Advisory CommitteeJustia.comNo ratings yet
- Erythema Ab IgneDocument4 pagesErythema Ab IgneCezar Adrian SimereaNo ratings yet
- Dermatovenerology CS 253 PDFDocument36 pagesDermatovenerology CS 253 PDFIvanes IgorNo ratings yet
- Health Activity Sheet QTR1 LC1-9Document14 pagesHealth Activity Sheet QTR1 LC1-9Nota BelzNo ratings yet
- Thesis On HPV VaccineDocument8 pagesThesis On HPV Vaccinegjftqhnp100% (2)
- New Drug Approval From Cdsco Till DateDocument5 pagesNew Drug Approval From Cdsco Till DateAshish1pharmaNo ratings yet
- Detailed Micro ChartDocument6 pagesDetailed Micro Chartmatt100% (1)
- Sataloff Chs 6-11 - 2Document79 pagesSataloff Chs 6-11 - 2Dwiki GumelarNo ratings yet
- Cancer Germany 2015 2016Document158 pagesCancer Germany 2015 2016Sebas ArmasNo ratings yet
- Endometrial Cancer Diagnosis and TreatmentDocument9 pagesEndometrial Cancer Diagnosis and TreatmentAhmed Butt100% (1)
- Basal Cell CarcinomaDocument134 pagesBasal Cell CarcinomaMore AmoNo ratings yet
- 2011 - MCQ It Blok 19Document12 pages2011 - MCQ It Blok 19Mohamad Fiqih ArrachmanNo ratings yet
- Ihe680 032911Document62 pagesIhe680 032911cecsdistancelab100% (2)
- Clinical Picture: Groove Sign in Eosinophilic FasciitisDocument1 pageClinical Picture: Groove Sign in Eosinophilic FasciitisRicardo López HernandezNo ratings yet
- Fungi and DiseaseDocument5 pagesFungi and Diseaseharold_gravity9885No ratings yet
- Handout - ADocument13 pagesHandout - AMadhu UpadhyayNo ratings yet
- BPH (Benign Prostatic Hyperplasia)Document11 pagesBPH (Benign Prostatic Hyperplasia)AviZhafiraNo ratings yet
- Event ProposalDocument2 pagesEvent ProposalSudhakar Parthasarathy50% (2)
- DK Chakra Chart 2017Document2 pagesDK Chakra Chart 2017Tuxita SuryaNo ratings yet
- THE INDEPENDENT Issue 579Document44 pagesTHE INDEPENDENT Issue 579The Independent Magazine0% (1)
- Unit Plan Owaisi College of NursingDocument5 pagesUnit Plan Owaisi College of NursingSiva0726No ratings yet