Professional Documents
Culture Documents
The Systemic Therapy of Atopic Dermatitis in Outpatient Clinic Division of Allergy and Immunology at DR - Soetomo General Hospital in 2013 - 2
Uploaded by
yolandajuly19Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Systemic Therapy of Atopic Dermatitis in Outpatient Clinic Division of Allergy and Immunology at DR - Soetomo General Hospital in 2013 - 2
Uploaded by
yolandajuly19Copyright:
Available Formats
The Systemic Therapy of Atopic Dermatitis in Outpatient clinic Division of Allergy and Immunology at Dr.
Soetomo
General Hospital in 2013
Authors : Yolanda1 Gwenny Ichsan Prabowo2 Damayanti3
Medical Faculty of Airlangga University, Surabaya, East Java
Email: yolandajuly19@gmail.com
Abstract
Background
Atopic Dermatitis (AD) is a chronic skin disease which often relapsed and associated with abnormallity skin
barrier, allergen sensitization, and recurrent skin infection. This research was conducted to figured out the prevalence
of AD patients which treated by the systemic therapy in Outpatient Clinic of Allergic and Immunology Division of
DR.Soetomo Hospital in 2013. As well as there is a lack information of this issue in Indonesia.
Methods
The authors used observational descriptive as a research design. The instrument are used from medical
records. The new patients of AD who treated by systemic therapy as a sample. The variable are the types of systemic
therapy their used and the profile of patient.
Result
All of AD patients used Cetirizine the antihistamin as the mayor systemic therapy (100%). 32 patients took
corticosteroid Dexamethasone (34,7%). 2 patients used antibiotics (2.2%). The Algorithms of therapy according to
Consensus guideline for management atopic dermatitis in asia pacific.
Keyword: Atopic dermatitis, The Systemic therapy, antihistamine, Corticosteroid, antibiotic
Background
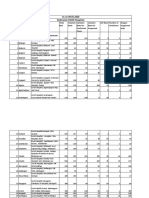
Atopic Dermatitis (AD) is a chronic skin Result
disease which often relapse and associate with
abnormality skin barrier, allergen sensitization, and The amount of AD patients who got systemic
recurrent skin infection. Babies and children are therapy in throughout a year in 2013 was 92 patients.
common. Insidence of AD at Outpatient Clinic is Table 1. The prevalence of a chief complaint of the AD
increasing every year. The Amount of AD patients in pateints at Outpatient clinic Division of Allergy and
2006 was 116 (8,14%), in 2007 was 148 (11,05%) and Immunology Dr.Soetomo General Hospital Surabaya in
2008 was 230 (17,65%).1,2 2013
Gender
AD research was limited especially about the Age Total
Men (%) Women (%)
prevalence of the systemic therapy. The unsatisfied
therapy of AD caused by long term therapy and 1-4 years
0 (0,0%) 1 (1,1%) 1 (1,1%)
old
relapsed was still happens. 5-14 years
0 (0,0%) 2 (2,2%) 2 (2,2%)
old
Methods 15-24 years
9 (9,8%) 26 (28,3%) 35 (38%)
old
The design of this research are observational 25-34 years 10
descriptive. The sample was all of the new AD 4 (4,3%) 6 (6,5%)
old (10,9%)
patients at Outpatient Clinic in 2013. The variable 35-44 years
6 (6,5%) 15 (16,3%)
21
taken by the type of the systemic therapy that patient old (22,8%)
45-54 years
consumed, age, gender, jobs, the chief complaint, the old
2 (2,2%) 6 (6,5%) 8 (8,7%)
onset, the atopic history, the morphology of lesion, and 55-64 years
4 (4,3%) 4 (4,3%) 8 (8,7%)
predilection of lesion. The secondary data from old
medical records as the instrument. The data has been 65-74 years
1 (1,1%) 3 (3,3%) 4 (4,3%)
old
collected and assembled in descriptive. The result will
>75 years
be presented in tables and images. 1 (1,1%) 2 (2,2%) 3 (3,3%)
old
92
Total 27 (29,3%) 65 (70,7%)
(100%)
1 : Student at Medical Faculty of Airlangga University
2 : Biochemistry department of Medical Faculty of Airlangga University
3 : Dermatology department of Medical Faculty of Airlangga University
According Table 1, women are more common The most common systemic therapy were given to 92
in AD who treated by the sytemmic therapy, there are patients are antihistamine (figure 1). Another options
approximately 65 patients (70,7%). The group of 15- are corticosteroid and antibiotics. The most given
24 years old are most dominant to acquired AD, 35 antihistamine are Cetirizine 78,2%. Dexamethasone
patients (38%). Based on the collected data, the jobs are popular corticosteroid for AD, approximately
of AD patients are 40 patients an employee of non 34,7%. The rarely therapy that used among AD are
government (43,5%), 15 patients are a housewife antibiotics, Erythromycin and Amoxycillin 1,1%.
(16,3%) and 6 patients are a public servants (6,5%).
100
Table 2. The prevalence of chief complaint in AD patients at Cetirizine
Outpatient clinic Division of Allergy and
80
Immunology Dr.Soetomo General Hospital
Mebhidroline
Surabaya in 2013
The Chief Complaint Amounts (%) 60 napadysilate
Pruritus 70 (76,1%) Loratadine
Pruritus and redness skin 21 (22,8%) 40 78,2
Redness skin 1 (1,1%)
Total 92 (100%) 20 14 16 CTM
4 1,1
0
According Table 2, the most chief complaint THE ANTIHISTAMINE (%) Cimetidine
that brought patients to the hospital are the pruritus
skin, there are 70 patients (76,1%). The onset of the
Figure 2. The Prevalence Of Antihistamine in AD patients at
chief complaint were begun less than one year 47,8%, Outpatient clinic Division of Allergy and Immunology Dr
in between 1-12 months as 32,6%, more than one year Soetomo General Hospital in 2013
about 16,3%.
The history of atopic in AD patients Type of Atopic (%)
themselves are 23,9%. Meanwhile, the history of
atopic in family member of AD patients are Asthma bronchiale
approximately 19,6%. The most types of atopic which
experienced by patients are rhinitis allergic 14,1%.
On the other hand, there are asthma bronchiale 3% Rhinitis allergic
21% 31%
10,9%, urticaria 2,2%, both asthma bronchiale and
rhinitis allergic 7,6%. Asthma bronchiale, rhinitis 6%
allergic, and urticarial in the same patient 1,1%. Urticaria
39%
In Physical examination were found the most
morphologic are erythema as 68 patients (73,9%).
Asthma bronchiale
Another morphologic are papule 46,7%, lichenification & Rhinitis Allergic
41,3%, erossion 36,9%, xerosis 29,3%, Ichthyosis
26,1%, excoriation 20,6%, hyperpigmentation 8,7%,
pustule 8,7%, vesicle 2.2%. The predilection were Figure 3. The Prevalence of the type of Antihistamine in AD
found are the extensor 89,2%, on the face 9,8%, the patients at Outpatient clinic Division of Allergy and
trunks 9.8%, the neck 3,3%, and the flexor 2,2%. Immunology Dr Soetomo General Hospital 2013
The systemic therapy (%)
3; 2%
36; 28% Antihistamine
92; 70% Corticosteroid
Antibiotic
Figure 1. The prevalence of the systemic Therapy in AD
patients at Outpatient clinic Division of Allergy and
Immunology Dr.Soetomo General Hospital Surabaya in
2013
excoriation, vesicle, and the serous exudate.
8,7 Then, in subacute lesion are arised the erythema,
26,1 excoriation with scaling papule. In chronic lesion
20,6
8,7 marked by thickening plaque, protruded of skin
The Morphology (%) 46,7
29,3 markings, and fibrotic papule (prurigo nodule). The
41,3
36,9 predilection of lesion could be classified based on age
2,2
73,9 and the disease activity. In the babies patient,
the lesion often appear on face region, scalp, and
0 20 40 60 80 extensor extremity. In adolescence who has AD
longger than the babies, might developed to chronic
Hyperpigmentation Icthyosis AD with lichenification and located erythema in the
Excoriation Pustule flexor folds. In adult patient, the lesion mostly on cubiti
fossa, popliteal fossa, neck and wrist. The lesion may
Papule Xerosis
appeared are papule, vesicle, and lichenification. 6,8
Lichenification Erossion
The management of AD with systemic therapy
Vesicle Erythema in dermatology department of Dr.Soetomo General
Hospital such as, antihistamine, corticosteroid, and
Figure 4. The prevalence of morphology in AD patients at antibiotic. The antihistamine has given are Cetirizine,
Outpatient clinic Division of Allergy and Immunology Dr. Chlorpheniramine maleat, Dipenhydramine HCL, and
Soetomo General Hospital Surabaya in 2013 Loratadine. The corticosteroid mostly given are
Prednisone and Dexamethasone. If there are
Discussion secondary infection on AD lesion, could be given
In this research women are the most gender Erythromycin. The secondary infection in AD usually
who suffering AD. It was matched with the research in caused by S.aureus.6
korea that shown women are common in AD than The antihistamine are agonist substance
men. There are literature which revealed babies and which binding to the histamine receptor, thus the
toddler are most in AD and tend to developed until they receptor could stand in inactive state. Antihisamine H1
grow up. FLG gene are allegedly play a role to decreasing the proinflamation cytokines production,
increasing the AD risk in babies. However in adhesion molecule expression, and eosinophil
Dr.Soetomo General Hospital, the patients below 14 chemotaxis. Antihistamine H1 divided into two groups.
years old admitted in pediatric outpatient clinic.1,4,5 The first generation of antihistamine H1 (sedative) and
According table 2, the most chief complaint the secondary generation of antihistamine H2
made patients seek the doctor are pruritus. (non sedative). Antihistamine H1 has sedative effect
The pruritus may appear caused by skin barrier that acts on muscarinic, α adrenergic, and serotonine.
disfunction called FLG gene mutation. FLG took a part On the other hand, sedative antihistamine also acts on
for filagrin coding. Filagrin is a cornoecytes stabilizer cardiac ion channel. It has heterocyclic rings which
which forming the skin barrier. When filargrin been increasing lipophilic, then could entry to the brain
interrupted, the allergen are free to made penetration barrier. The examples of H1 sedative are
into the skin and became the pruritus skin. In AD Chlorpheniramine, Cyproheptadine, Dipenhydramine,
patients there are immunologic deficiency, those are Hydroxyzine, and Tripenelamine. Non sedative H1
increasing IgE and lymphocyte T dysfunction. On early binding in non competitive on H1 receptor and it has
phase reaction of AD, after the allergen bind to IgE on longer half time than the sedative H1. Non sedative H1
the surface of the mast cell, then degranulation of mast has selectivity of H1 receptor, it makes less lipophilic
cell occurred. Thus, the histamine and the cytokines and less sedative. Therefore, from the safety aspect
came out of the mast cells then appeared symptoms H1 non sedative saftier than sedative. There are some
such as dominant pruritus and redness of the skin.6,7 examples non sedative H1 such as Cetirizine,
Loratadine, Acrivastine, Azelastine, and fexofenadine.
Children with AD might increasing Antihistamine has been chosen as an effort to
the susceptibility to suffering asthma bronchiale and decreasing the pruritus symptoms. Thus, the
rhinitis allergic, mainly a child who has AD below 2 antihistamine could be increasing the quality of
year old approximately 50% to acquired asthma patiens life. In the literature Cetirizine has been the
bronchiale. The patients who has atopic history tend choice of AD in children, approximately 8-16 years old,
to experienced clinical manifestation heavier than caused it could relief the symptoms of AD. Cetirizine
patients with no atopic history.4 could be given at 10mg/dose, once in oral route.6,9,10,11
The acute lesion of AD, commonly marked by The corticosteroid mechanism of action are
the intensed pruritus, papule erythema with binds to cytoplasmic receptors then makes
translocation to the nucleus to regulate the B, Paller A, & Leffell, D. (EDS) Fitzpatrick’s
transcription of gene which involved in inflammation Dermatology in General Medicine. 8th ed.
cascade in AD, hence could fixed the clinical feature NewYork, Mc GrawHill: 146-181.
of patients as fast as possible. Corticosteroid sytemic 2. Zulkarnain I. 2009. Manifestasi Klinis dan
would be chosen if the topical therapy and Diagnosis Dermatitis Atopik. Dalam:
antihistamine could not give an effect as much as Boediarja, S.A, Sugiarto, T.L, Indraitmi, W,
expected. Dose of Dexamethasone for adult patient Devita, M, Prihanti, S, (ED). Dermatitis Atopik.
are 0,5-1 mg/dose could give 2-3 times a day and for Balai Penerbit FKUI. Jakarta. Hal 39-51.
child are 0,1 mg/kg/day and do the tapering dose to 3. Rubel D, Thirumoorthy T, Soebaryo RW,
minimize the suppression of adrenal glands.6,12,13 Weng SCK, Gabriel TM, Villafuerta LL et al.
2013. Consensus guideline for management
The administration of antibiotics if there is a of atopic dermatitis: an asia-pacific
symptoms lead to secondary infection. It could perspective. Journal of Dermatology: 40: 160-
happens caused by decreasing of skin barrier function 171
in AD patients. The most common infection that have 4. James W, Berger T, Elston D. 2006. Andrews’
found caused by Staphylococcus aureus. In adult Diseases of The skin: Clinical Dermatology
patients are found 107 unit of S.aureus in 10th ed. USA, Saunders ElSevier: 75-76.
approximately 90% culture result. Erythromycin dose 5. Jung-Seok Yu, Chang-Jong Lee, Ho-Seok
in adut are 250-500 mg/dose could given 3-4 times a Lee, Jihyun Kim, Youngshin Han, Kangmo
day in oral route, while child 15-25 mg/dose, 3 times a Ahn, Sang-II Lee. 2012. Prevalence of Atopic
day in oral route.6,14 Dermatitis in Korea: Analysis by Using
Conclusion and advice National Statistics. J Korean Med Sci; 27:681-
685.
The result of profile evaluation in therapy 6. Hutomo M, Pohan S, Agusni I. 2005.
systemic for AD patients are matched with asia pacific Dermatitis Atopik. Dalam: Pedoman Diagnosa
guideline for AD. Antihistamine are the most sytemic dan Terapi BAG/SMF Ilmu Penyakit Kulit dan
therapy in Dr. Soetomo hospital. The most chosen Kelamin. Ed 3. Surabaya: Rumah Sakit
antihistamine are Cetirizine. Dexamethasone are Umum Dokter Soetomo.1-3.
popular corticosteroid for relieve the AD inflammation 7. Boediardja, S.A. 2006. Etiopatogenesis
in Dr. Soetomo hospital. Antibiotics that have been Beberapa Dermatitis pada Bayi dan Anak.
used are Erythromycin and Amoxicillin. The result of Dalam: Djajakusumah, T.S., ed. Antiinflamasi
gender prevalence that common in AD are woman. Topikal pada Pengobatan Dermatitis Bayi dan
The age group that popular in AD are 15-24 years old. Anak. Jakarta: Balai Penerbit FKUI, 1-11.
The most predilection are the extensor extremity in AD 8. Oranje, AP. 2014. Evidence-Based
patients in Dr.Soetomo hospital. Pharmacological Treatment of Atopic
Dermatitis: An Expert Opinion an New
The advice for Division of allergy and Expectations. Indian J Dermatol: 59(2): 140-
immunology in Dr.Soetomo are the responds of 142.
therapy systemic in AD patients could be input in 9. Sidbury, R et al. 2014. Section 3.
medical record for evaluation. Then, SCORAD index Management and treatment with
could be applicated in the future in clinical phototherapy and systemic agents. Guideline
assessment. The research of AD still necessary of care for the management of atopic
because the therapy of AD still unsatisfied and made dermatitis. 1-23.
AD still relapsed. 10. Wood, AR. 2012. Atopic Dermatitis (atopic
eczema). Dalam: Wolff K, Goldsmith L, Katz
Acknowledgement
S, Gilchrest B, Paller A, & Leffell, D, (Eds)
All praise and thanks to god that has blessed Fitzpatrick’s Dermatology in General
us then, this research have been done. The authors Medicine.8th ed. NewYork, Mc GrawHill: 2767-
said thanks to Prof.Dr.Soetojo, dr., Sp.U, as Dean for 2775.
Medical Faculty of Airlangga University., Harsono, MD 11. Diepgen TL. 2002. Longterm treatment with
as a chairman of Dr.Soetomo General Hospital., who cetirizine of infants with atopic dermatitis: a
supported this research then it could be done. multi-country, double-blind, randomized,
placebo controlled trial (the ETAC trial) over
The Reference 18 months. Pediatr Allergy Immunol; 13: 278-
286.
1. Leung D, Eichenfield L & Boguniewicz M. 12. Wailing HW, Swick BL. 2010. Update on the
2012. Atopic Dermatitis (atopic eczema).
management of chronic eczema: new
Dalam: Wolff K, Goldsmith L, Katz S, Gilchrest
approaches and emerging treatment options.
Dove press Journal 100-117.
13. Sidbury, R et al. 2014. Guideline of care for
the management of atopic dermatitis. J Am
Acad Dermatol; 71:327-49.
14. Goh CL, Wong Js, Giam Yc. 1997. Skin
colonization of Staphylococcus aureus in
atopic dermatitis patients seen at the National
skin Center, Singapore. Int J Dermatol: 653-7.
You might also like
- Profile of Tinea Corporis and Tinea Cruris in Dermatovenereology Clinic of Tertiery Hospital: A Retrospective StudyDocument6 pagesProfile of Tinea Corporis and Tinea Cruris in Dermatovenereology Clinic of Tertiery Hospital: A Retrospective StudyMarwiyahNo ratings yet
- Profile of Tinea Corporis and Tinea Cruris in Dermatovenereology Clinic of Tertiery Hospital: A Retrospective StudyDocument6 pagesProfile of Tinea Corporis and Tinea Cruris in Dermatovenereology Clinic of Tertiery Hospital: A Retrospective StudyRose ParkNo ratings yet
- Scenario of Retinoblastoma Among Bangladeshi Children - A Single Center Experience of 10 YearsDocument5 pagesScenario of Retinoblastoma Among Bangladeshi Children - A Single Center Experience of 10 YearsBOHR International Journal of Current Research in Optometry and Ophthalmology (BIJCROO)No ratings yet
- Research Article: Prevalence and Risk Factors For Adult Cataract in The Jingan District of ShanghaiDocument7 pagesResearch Article: Prevalence and Risk Factors For Adult Cataract in The Jingan District of ShanghaiIndermeet Singh AnandNo ratings yet
- Medication Errors, P.reddy, Mallesh.Document9 pagesMedication Errors, P.reddy, Mallesh.gnaneshwerNo ratings yet
- Paper Iralivelya PDocument5 pagesPaper Iralivelya Pbless goodNo ratings yet
- A Study On Hivaids Knowledge Among Nursing StudentDocument6 pagesA Study On Hivaids Knowledge Among Nursing Studentanastasia mumeckhNo ratings yet
- A Retrospective Study: Stevens-Johnson Syndrome and Toxic Epidermal NecrolysisDocument9 pagesA Retrospective Study: Stevens-Johnson Syndrome and Toxic Epidermal NecrolysisedisanjanaNo ratings yet
- DermatologyDocument5 pagesDermatologyYuliana DaisongNo ratings yet
- Characteristics and Demofigures Features of Patients With Age-Related Macular Degeneration at Tertier Center in Denpasar, BaliDocument13 pagesCharacteristics and Demofigures Features of Patients With Age-Related Macular Degeneration at Tertier Center in Denpasar, BaliUdayanaNo ratings yet
- Research ArticleDocument10 pagesResearch ArticlePratama Imanuel RawungNo ratings yet
- An Analytical Study: Survival Rate of Laryngeal Carcinoma Patients Among Indonesian PopulationDocument5 pagesAn Analytical Study: Survival Rate of Laryngeal Carcinoma Patients Among Indonesian PopulationAmalia Tri UtamiNo ratings yet
- Comprehensive Survival Analysis of A Cohort of Patients With Stevens-Johnson Syndrome and Toxic Epidermal NecrolysisDocument8 pagesComprehensive Survival Analysis of A Cohort of Patients With Stevens-Johnson Syndrome and Toxic Epidermal NecrolysisKuro ChanNo ratings yet
- Rina La Distia Nora. September 2021 JACINDocument46 pagesRina La Distia Nora. September 2021 JACINMuliaNo ratings yet
- Risk Factor TaiwanDocument5 pagesRisk Factor TaiwanMira ApriliaNo ratings yet
- Research A Clinical Evalution of Efficacy of Certain Ayurvedic Formulations in The Management of Arsha (Haemorrhoids) - Ayur ResearchDocument16 pagesResearch A Clinical Evalution of Efficacy of Certain Ayurvedic Formulations in The Management of Arsha (Haemorrhoids) - Ayur ResearchDrHassan Ahmed ShaikhNo ratings yet
- Jurnal 4Document11 pagesJurnal 4Kholifatu UlfaNo ratings yet
- Migraine Trigger Factors in The 2012-2014 Dental Medicine Students in Dental Hospital and Yarsi Hospitals From Islamic ViewsDocument10 pagesMigraine Trigger Factors in The 2012-2014 Dental Medicine Students in Dental Hospital and Yarsi Hospitals From Islamic ViewsShifa KhaunanNo ratings yet
- Original: Spectrum of Opportunistic Infections in HIV-AIDS PatientsDocument4 pagesOriginal: Spectrum of Opportunistic Infections in HIV-AIDS Patientsputri1114No ratings yet
- Pharmaceutical Sciences: Recent Advances and Treatments of Childhood Nephrotic SyndromeDocument3 pagesPharmaceutical Sciences: Recent Advances and Treatments of Childhood Nephrotic SyndromeiajpsNo ratings yet
- Rahul Kamble Pediatrics Article 1Document9 pagesRahul Kamble Pediatrics Article 1Rahul KambleNo ratings yet
- Jurnal Mata Corneal UlcerDocument7 pagesJurnal Mata Corneal UlceronjieeNo ratings yet
- A Study On The Bacteriological Profile of Urinary PDFDocument4 pagesA Study On The Bacteriological Profile of Urinary PDFcendy oktariNo ratings yet
- Adverse Cutaneous Drug Reactions (Acdrs) in Sardjito General HospitalDocument122 pagesAdverse Cutaneous Drug Reactions (Acdrs) in Sardjito General HospitalOpung HokiNo ratings yet
- 2013 3 2 PDFDocument4 pages2013 3 2 PDFEpi PanjaitanNo ratings yet
- EPICOH 2013 PosterDocument1 pageEPICOH 2013 PosterSutheeRattanamongkolgulNo ratings yet
- Research Article: Clinical Profile of Dengue Fever in Children: A Study From Southern Odisha, IndiaDocument6 pagesResearch Article: Clinical Profile of Dengue Fever in Children: A Study From Southern Odisha, IndiazuliaahmadNo ratings yet
- Urinary Tract Infections in A Tertiary Hospital in Abuja, NigeriaDocument5 pagesUrinary Tract Infections in A Tertiary Hospital in Abuja, NigeriaRazkhal KunmoNo ratings yet
- Evaluating RisksDocument33 pagesEvaluating RisksDavid TribeNo ratings yet
- Corona Children Studies Co-Ki First Results of A GDocument15 pagesCorona Children Studies Co-Ki First Results of A GFernando LoaizaNo ratings yet
- Self Medication Among Medical University Staff at Taibah University, Al-Madinah. 2012Document7 pagesSelf Medication Among Medical University Staff at Taibah University, Al-Madinah. 2012ijasrjournalNo ratings yet
- Morbidity Pattern Among The Geriatric Population in South India: An Observational StudyDocument7 pagesMorbidity Pattern Among The Geriatric Population in South India: An Observational StudyAdvanced Research PublicationsNo ratings yet
- 2012 PDMnonscarringalopeciaDocument5 pages2012 PDMnonscarringalopeciaStella Gracia OctaricaNo ratings yet
- Jurnal 2Document7 pagesJurnal 2mtasaragihNo ratings yet
- ATGDocument4 pagesATGMonikaNo ratings yet
- www.iosrphr.orgDocument5 pageswww.iosrphr.orgIOSR Journal of PharmacyNo ratings yet
- Health Problems and Risk Factors Prevailing Among Garment Workers in TirupurDocument6 pagesHealth Problems and Risk Factors Prevailing Among Garment Workers in TirupursupriaprNo ratings yet
- Burden, Pattern, Associated Factors and Impact On Quality of Life of Dermatological Disorders Among The Elderly in Ilala Municipality, Dar Es Salaam A Cross-Sectional StudyDocument10 pagesBurden, Pattern, Associated Factors and Impact On Quality of Life of Dermatological Disorders Among The Elderly in Ilala Municipality, Dar Es Salaam A Cross-Sectional StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Clinico-Etiological Spectrum of Pancytopenia in Hospitalized ChildrenDocument4 pagesClinico-Etiological Spectrum of Pancytopenia in Hospitalized ChildrenNurul Huda KowitaNo ratings yet
- Psoriasis Biologics RegistryDocument6 pagesPsoriasis Biologics RegistryWei Sheng ChongNo ratings yet
- Otomycosis Clinical Features, Predisposing Factors and Treatment ImplicationsDocument14 pagesOtomycosis Clinical Features, Predisposing Factors and Treatment ImplicationsVela NazarNo ratings yet
- A Study of Haematological Profile of Malaria in A Tertiary Care Centre of Western Uttar Pradesh, IndiaDocument5 pagesA Study of Haematological Profile of Malaria in A Tertiary Care Centre of Western Uttar Pradesh, IndiaramperoughNo ratings yet
- Funit Copii 6 Luni - 12 AniDocument5 pagesFunit Copii 6 Luni - 12 AniLyova OrashanNo ratings yet
- Pharmaceutics 12 00713Document11 pagesPharmaceutics 12 00713noviantyramadhani12No ratings yet
- 956 3320 1 PBDocument5 pages956 3320 1 PBMelina JessicaNo ratings yet
- The Risk Level For Individuals To Suffering From NCDs Based On CERDIK BehaviorDocument6 pagesThe Risk Level For Individuals To Suffering From NCDs Based On CERDIK BehaviorIJPHSNo ratings yet
- EndometriosisDocument13 pagesEndometriosisDian NovitaNo ratings yet
- SSJ ConvertDocument8 pagesSSJ ConvertHarryPascaRullianNo ratings yet
- Quality of Life, Respiratory Symptoms, and Health Care Utilization 1 Year Following Outpatient Management of COVID 19: A Prospective Cohort StudyDocument4 pagesQuality of Life, Respiratory Symptoms, and Health Care Utilization 1 Year Following Outpatient Management of COVID 19: A Prospective Cohort StudyFranklin GuamanNo ratings yet
- Clinical Presentation and Outcome in Diabetic Foot Cases: A Prospective Study in A Tertiary Care Teaching Hospital of Uttarakhand, IndiaDocument4 pagesClinical Presentation and Outcome in Diabetic Foot Cases: A Prospective Study in A Tertiary Care Teaching Hospital of Uttarakhand, IndiaNaily Nuzulur RohmahNo ratings yet
- Vitiligo ObatDocument6 pagesVitiligo ObatLidwina DewiNo ratings yet
- Clinico-Epidemiological Study of Dermatophytosis in Teaching Hospital of North KarnatakaDocument4 pagesClinico-Epidemiological Study of Dermatophytosis in Teaching Hospital of North KarnatakaAldo NovaNo ratings yet
- Prakriti Analysis of COVID 19 Patients: An Observational StudyDocument12 pagesPrakriti Analysis of COVID 19 Patients: An Observational StudySaurabh SumanNo ratings yet
- Seroprevalensi Toksoplasmosis Di Gianyar Bali: Seroprevalence of Human Toxoplasmosis in Gianyar Bali ProvinceDocument6 pagesSeroprevalensi Toksoplasmosis Di Gianyar Bali: Seroprevalence of Human Toxoplasmosis in Gianyar Bali ProvinceKomang SuryaNo ratings yet
- Knowledge, Attitude and Practices Among Health Care Workers On Needle-Stick InjuriesDocument5 pagesKnowledge, Attitude and Practices Among Health Care Workers On Needle-Stick Injuriesnik adrianiNo ratings yet
- Antibiotic Induced Cutaneous Rash in Infectious Mononucleosis Overview Ofthe Literature 2155 6121 1000222Document6 pagesAntibiotic Induced Cutaneous Rash in Infectious Mononucleosis Overview Ofthe Literature 2155 6121 1000222Munshi KamrulNo ratings yet
- Sjs Ten KuchingDocument54 pagesSjs Ten KuchingChuaMinHuangNo ratings yet
- Jurnal Kanker Mamae-Survival Life Penderita Kanker Payudara Pada WanitaDocument7 pagesJurnal Kanker Mamae-Survival Life Penderita Kanker Payudara Pada WanitarosmawatiNo ratings yet
- Articlee OooDocument6 pagesArticlee OooLAL DIME 1No ratings yet
- A Bad Case of StripesDocument2 pagesA Bad Case of StripesRadhika RathoreNo ratings yet
- 1116005I Rev. 02Document2 pages1116005I Rev. 02kirubel demelashNo ratings yet
- Stacey Luneke ResearchfinalDocument9 pagesStacey Luneke Researchfinalapi-309088550No ratings yet
- Gen Bio 2 Q4 Module 4Document25 pagesGen Bio 2 Q4 Module 4Shoto TodorokiNo ratings yet
- Breastfeeding QuestionnaireDocument2 pagesBreastfeeding QuestionnaireDr Puteri Nur Sabrina Binti Mohd HanapiNo ratings yet
- Effectiveness of Workplace Counseling On Employee Performance. A Case of Mumias Sugar Company Limited, KenyaDocument10 pagesEffectiveness of Workplace Counseling On Employee Performance. A Case of Mumias Sugar Company Limited, KenyainventionjournalsNo ratings yet
- Effect of Dragon Fruit On Lipid ProfileDocument2 pagesEffect of Dragon Fruit On Lipid ProfileElindah Ayunin ArrumNo ratings yet
- Chapter 4 - Ornamental FishDocument34 pagesChapter 4 - Ornamental FishJuan Carlos SánchezNo ratings yet
- 04-15-21 Covid-19 Vaccine TrackerDocument52 pages04-15-21 Covid-19 Vaccine TrackerJohn Michael JetiganNo ratings yet
- ZOOLOGY LESSON 1 IntroductionbranchesofzoologyDocument25 pagesZOOLOGY LESSON 1 IntroductionbranchesofzoologyLeimarie BarsanaNo ratings yet
- Training Manual PDFDocument145 pagesTraining Manual PDFCalinnescuNo ratings yet
- Neonatal Pneumonia Case StudyDocument9 pagesNeonatal Pneumonia Case StudyMary hope DomalaonNo ratings yet
- Bivalirudin Anticoagulant1Document6 pagesBivalirudin Anticoagulant1walid hassanNo ratings yet
- Manual Terapia DigitalDocument38 pagesManual Terapia DigitalPaolaQuitian0% (1)
- CT/MRI Ordering Guide: Body Part Signs/Symptoms Exam To OrderDocument2 pagesCT/MRI Ordering Guide: Body Part Signs/Symptoms Exam To OrderCourtNo ratings yet
- Lab 1C PAR-Q and Health History QuestionnaireDocument4 pagesLab 1C PAR-Q and Health History Questionnaireskyward23No ratings yet
- March Case StudyDocument13 pagesMarch Case Studyapi-212894050No ratings yet
- Dosage Chapter 1 PDFDocument4 pagesDosage Chapter 1 PDFLena EmataNo ratings yet
- Warming Center New HavenDocument3 pagesWarming Center New HavenHelen BennettNo ratings yet
- 4-Stretching For Impaired Mobility ADocument47 pages4-Stretching For Impaired Mobility Aphysical therapy channel ptNo ratings yet
- Basal Osseointegrated Implants ClassificDocument7 pagesBasal Osseointegrated Implants ClassificAnkur SaladaNo ratings yet
- 3 Antenatal CareDocument24 pages3 Antenatal CareDrSabah Lotfy100% (1)
- Blood Transfusion Reactions: P Sunil Kumar Department of Haematology ST - John's Medical CollegeDocument48 pagesBlood Transfusion Reactions: P Sunil Kumar Department of Haematology ST - John's Medical CollegeFULGENCE RUHARARANo ratings yet
- WBC CountingDocument4 pagesWBC CountingMarx AsuncionNo ratings yet
- Anti Malarial Drugs by Salaria AnamikaDocument10 pagesAnti Malarial Drugs by Salaria AnamikaSalaria Anamika100% (1)
- List COVID Facilities State OdishaDocument3 pagesList COVID Facilities State OdishadrjyotivetNo ratings yet
- Tropical GastroenterologyDocument8 pagesTropical GastroenterologyAnonymous 9QxPDpNo ratings yet
- Portal HypertensionDocument25 pagesPortal HypertensionJainab SiddiquiNo ratings yet
- 10 12 15hematoo Edit 1Document10 pages10 12 15hematoo Edit 1Anonymous 18GsyXbNo ratings yet
- Nursing Care of HydronephrosisDocument19 pagesNursing Care of Hydronephrosisvictor zhefaNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (29)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (2)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)No ratings yet
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- To Explain the World: The Discovery of Modern ScienceFrom EverandTo Explain the World: The Discovery of Modern ScienceRating: 3.5 out of 5 stars3.5/5 (51)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (59)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (45)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)