Professional Documents
Culture Documents
By Intern Dr. Borhan Uddin
Uploaded by
manju0 ratings0% found this document useful (0 votes)
32 views12 pagespre rupture rupture of membrane
Original Title
Prematureruptureofmembrane-170319165542 (1) - Copy - Copy
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentpre rupture rupture of membrane
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
32 views12 pagesBy Intern Dr. Borhan Uddin
Uploaded by
manjupre rupture rupture of membrane
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 12
By Intern Dr. Borhan Uddin.
Definition- Spontaneous rupture of the membrane any
time after the age of viability but before the onset of
labor is called premature rupture of membrane.
Incidence of PROM- 10% of all pregnancy.
Causes of PROM-Exact cause is not known-
Obstetrical cause-
1. Multiple pregnancy.
2. Polyhydramnios
3. Malpresentation and contracted pelvis
Maternal infection-
1. UTI .
2. Lower genital tract infection.
3. Chorioamnionitis.
4. Cervical incompetence.
5. Frequent coitus in last month
Diagnosis of PROM-
a) History.
b) Examination
c) Investigation.
History- Sudden escape of watery discharge per vagina either
in the form of gush or slow leak.
Examination-If chorioamnionitis is developed then sign of
infection.
1) Fever.
2) Tachycardia.
3) Uterine tenderness.
4) Foul smelling discharge.
Confirmation of diagnosis- Sterile speculum examination
shows liquor escaping out through the cervix and then
examine the fluid.
How we confirm that it is liquor or other fluid?
Detection of PH by litmus or nitrazine paper- Normal vaginal
PH is -4.5-5.5.If it is liquor then PH-7-7.5.
Fern test- Fluid from posterior fornix is placed on a slide and
allowed to dry. Amniotic fluid from a fern like pattern of
crystallization.
Nitrazine test- a sterile cotton tipped swab should be used to
collect fluid from posterior fornix and apply it to nitrazine
paper. If it is amniotic fluid then the paper turns into blue.
Hydrorrhoea gravidarum.
Incontinence of urine especially in later month.
Investigations-
CBC-Neutrophilic leukocytosis in case of chorioamnionitis.
Urine for R/E.
High vaginal swab for culture and sensitivity test.
USG for monitoring the fetal well -being.
To start prophylactic antibiotics-
Need To asses gestational age.
Patient not in labor.
Absence of infection and fetal distress.
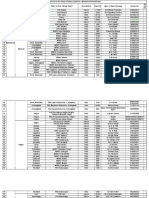
Pregnancy more than 34 weeks- Wait for Pregnency more than 38 weeks- Wait for
Pregnancy less than 34 weeks – Expectant spontaneous onset of labor for 24-48 24 hours.
treatment and continue for fetal maturity. hours • If fails either induction or caesarean
Hospitalization. • If fails- section.
Bed rest. • Induction with oxytocin
sterile valval pad. • caesarean section
prophylactic antibiotic.
Maternal monitoring- pulse, BP, Temp,
uterine tenderness.
Fetal monitoring- FHR, USG, Biophysical
profile.
Injection- Dexamethasone 12 mg 2 dose
12 hourly ( 2.5 amp) which stimulate
type-2 alveolar cell and release surfactant
which prevent RDS.
Maternal-
preterm labor.
Infection.
Increase chance of cord prolapse.
Prolong labor.
Fetal –
High perinatal mortality and morbidity.
Neonatal infection.
You might also like
- Csec CXC Caribbean History Paper 2 2021Document24 pagesCsec CXC Caribbean History Paper 2 2021raliegh47% (15)
- Case Study On PROMDocument11 pagesCase Study On PROMPabhat Kumar86% (7)
- Caring for a Pregnant Woman with PROM and Severe OligohydramniosDocument13 pagesCaring for a Pregnant Woman with PROM and Severe Oligohydramniosmanju100% (11)
- Extended Essay FinalDocument17 pagesExtended Essay Finalapi-490097708No ratings yet
- Combs Wines and Spirit V Combs Wines and Spirit MEMORANDUM of LAW I 36Document28 pagesCombs Wines and Spirit V Combs Wines and Spirit MEMORANDUM of LAW I 36Khristopher Brooks100% (2)
- The Lion King-Simba's JourneyDocument14 pagesThe Lion King-Simba's JourneyTati Murgic IriarteNo ratings yet
- Common Complications of PregnancyDocument34 pagesCommon Complications of PregnancyiwennieNo ratings yet
- PPROMDocument63 pagesPPROMSaraMohammedNo ratings yet
- Management of Pregnancy With Premature Rupture of Membranes (Prom)Document6 pagesManagement of Pregnancy With Premature Rupture of Membranes (Prom)Ryzka Izza MayFanyNo ratings yet
- Multiple PregnancyDocument26 pagesMultiple PregnancyRaj PatelNo ratings yet
- Abortion Guide: Causes, Types, Symptoms & TreatmentDocument36 pagesAbortion Guide: Causes, Types, Symptoms & TreatmentdimlyNo ratings yet
- IUFDDocument29 pagesIUFDfasyanneshaNo ratings yet
- Obg Procedures FinalDocument60 pagesObg Procedures FinalVeena DalmeidaNo ratings yet
- Premature Rupture of MembranesDocument33 pagesPremature Rupture of MembranesSarang Lee100% (1)
- BRN MN 21 01 Guideline 2013 Eng Management Preterm Prelabour Rupture MembranesDocument3 pagesBRN MN 21 01 Guideline 2013 Eng Management Preterm Prelabour Rupture Membranesd99452727No ratings yet
- PROM Case Study on Mrs. Bhagyabati DasDocument11 pagesPROM Case Study on Mrs. Bhagyabati DasPatricia Denise TiradoNo ratings yet
- 18 PromDocument8 pages18 PromRyubusa HayabusaNo ratings yet
- Pregnancy Diagnosis and Fetal AssessmentDocument41 pagesPregnancy Diagnosis and Fetal AssessmentKrystel Anne MilanNo ratings yet
- DIAGNOSTIC EvaluationDocument38 pagesDIAGNOSTIC EvaluationRKNo ratings yet
- Pregnancy Complication: Department of Gynaecology and ObstetricsDocument40 pagesPregnancy Complication: Department of Gynaecology and ObstetricssanjivdasNo ratings yet
- PLacenta PreviaDocument10 pagesPLacenta Previaeyestrain_ajpn5001No ratings yet
- Prenatal DiagnosisDocument5 pagesPrenatal DiagnosisSadaf AfzalNo ratings yet
- Obstructed Labor & Prolonged LaburDocument22 pagesObstructed Labor & Prolonged LaburOmari Kabelwa100% (1)
- CVS Procedure ExplainedDocument5 pagesCVS Procedure ExplainedpriyankaNo ratings yet
- Infertility - Definition, Causes, Diagnostic Procedures AND CouncellingDocument37 pagesInfertility - Definition, Causes, Diagnostic Procedures AND CouncellingvincentsharonNo ratings yet
- Biochemical Methods ObgDocument25 pagesBiochemical Methods ObgRupali AroraNo ratings yet
- High Risk Ob Notes 1Document20 pagesHigh Risk Ob Notes 1pinpindalgoNo ratings yet
- Maternal and Fetal Wellbeing AssessmentDocument46 pagesMaternal and Fetal Wellbeing AssessmentmariaNo ratings yet
- Premature Rupture of Membranes (Prom)Document12 pagesPremature Rupture of Membranes (Prom)KABERA RENENo ratings yet
- Antenatal Assessment of Foetal Wellbeing.Document30 pagesAntenatal Assessment of Foetal Wellbeing.Kavya S MohanNo ratings yet
- Placenta Previa Case StudyDocument5 pagesPlacenta Previa Case StudyKristine Castillo100% (2)
- Drug StudyDocument6 pagesDrug StudyIvy MoralesNo ratings yet
- Prenatal Care: Understanding Pelvic Exams and Fetal AssessmentDocument9 pagesPrenatal Care: Understanding Pelvic Exams and Fetal AssessmentBinita ShakyaNo ratings yet
- 2.induction of Labour & Prolonged PregnancyDocument20 pages2.induction of Labour & Prolonged PregnancyMiswar Abdul HalimNo ratings yet
- Ectopic Pregnancy: Causes, Symptoms and DiagnosisDocument60 pagesEctopic Pregnancy: Causes, Symptoms and DiagnosisAndrada Doţa100% (1)
- Types and Management of AbortionDocument6 pagesTypes and Management of AbortionJan Vincent BallesterosNo ratings yet
- Placent Previa Case Study With Pa Tho PhysiologyDocument6 pagesPlacent Previa Case Study With Pa Tho PhysiologyRey Deemsur Salvilla MolinosNo ratings yet
- GYN Module 3 Case 1: Gestational Trophoblastic NeoplasiaDocument21 pagesGYN Module 3 Case 1: Gestational Trophoblastic NeoplasiaElaine Marie Rendon PalmejarNo ratings yet
- Nursing care for reproductive health issuesDocument100 pagesNursing care for reproductive health issuesHassen ZabalaNo ratings yet
- NCM 109 SL Lesson 1Document3 pagesNCM 109 SL Lesson 1Martina Medrano100% (1)
- Management of Breast EngorgementDocument81 pagesManagement of Breast EngorgementNavid BabluNo ratings yet
- Aminotic Fluid DisordersDocument34 pagesAminotic Fluid DisordersCheru DugaseNo ratings yet
- Handouts in NCM 107 - Emotional Reactions - Diagnostic TestsDocument3 pagesHandouts in NCM 107 - Emotional Reactions - Diagnostic Tests22bgu0684msNo ratings yet
- Government College of Nursing Jodhpur: Procedure On-Cordocentesis Subject-Obstetrics & Gynecology Specialty-IDocument4 pagesGovernment College of Nursing Jodhpur: Procedure On-Cordocentesis Subject-Obstetrics & Gynecology Specialty-Ipriyanka100% (2)
- Placenta Previa: AdvertisementDocument27 pagesPlacenta Previa: Advertisementyoung_mizthizah25No ratings yet
- Seminar On Post Term PregnancyDocument21 pagesSeminar On Post Term PregnancyValarmathi100% (1)
- Prom Preterm and PosttermDocument127 pagesProm Preterm and PosttermgibreilNo ratings yet
- Antepartum Hemorrhage CausesDocument9 pagesAntepartum Hemorrhage CausesadiNo ratings yet
- Means Ebesate Montebon Patigayon Ulile TitoDocument38 pagesMeans Ebesate Montebon Patigayon Ulile TitoJheanAlphonsineT.MeansNo ratings yet
- 1 Mother (High Risk Childbearing-Maternal)Document62 pages1 Mother (High Risk Childbearing-Maternal)Maui TingNo ratings yet
- Protocol Book For OBGYNDocument41 pagesProtocol Book For OBGYNShabir BadakhshNo ratings yet
- कर हर मैदान फ़तेह - Abortion का संक्षिप्त विवरणDocument38 pagesकर हर मैदान फ़तेह - Abortion का संक्षिप्त विवरणdimlyNo ratings yet
- Abortion, Ectopic PregnancyDocument139 pagesAbortion, Ectopic PregnancyINFORMASI MENARIKNo ratings yet
- Premature Rupture of MembraneDocument17 pagesPremature Rupture of MembraneShimaa Abdel hameedNo ratings yet
- High Risk of PregnancyDocument16 pagesHigh Risk of PregnancyGeraldine PatayanNo ratings yet
- Obg AbortionDocument62 pagesObg Abortionkashyap priyankaNo ratings yet
- Pregnancy Trauma NotesDocument8 pagesPregnancy Trauma NotesHisham FahadNo ratings yet
- Care of The FetusDocument79 pagesCare of The FetusJerald FernandezNo ratings yet
- Writing Portfolio Presentation in Pastel Green Beige Light Brown Scrapbook Style - 20230909 - 004532 - 0000Document14 pagesWriting Portfolio Presentation in Pastel Green Beige Light Brown Scrapbook Style - 20230909 - 004532 - 0000Jaz BenitoNo ratings yet
- Guide to Pediatric Urology and Surgery in Clinical PracticeFrom EverandGuide to Pediatric Urology and Surgery in Clinical PracticeNo ratings yet
- Treatment Strategy for Unexplained Infertility and Recurrent MiscarriageFrom EverandTreatment Strategy for Unexplained Infertility and Recurrent MiscarriageKeiji KurodaNo ratings yet
- Fertilization Process ExplainedDocument37 pagesFertilization Process ExplainedmanjuNo ratings yet
- Fetalskull 180920160134Document30 pagesFetalskull 180920160134manjuNo ratings yet
- Oligohydramnios 171125104430Document27 pagesOligohydramnios 171125104430manjuNo ratings yet
- Staff Development: Sherrel M. FelisminoDocument32 pagesStaff Development: Sherrel M. FelisminomanjuNo ratings yet
- Cordprolpase 130312081224 Phpapp02Document20 pagesCordprolpase 130312081224 Phpapp02manjuNo ratings yet
- Fetalskull 150226020658 Conversion Gate02Document20 pagesFetalskull 150226020658 Conversion Gate02manjuNo ratings yet
- Inserviceeducation 141119085308 Conversion Gate02Document25 pagesInserviceeducation 141119085308 Conversion Gate02manju100% (1)
- Inserviceeducation 141119085308 Conversion Gate02Document25 pagesInserviceeducation 141119085308 Conversion Gate02manju100% (1)
- Diseases of OvaryDocument51 pagesDiseases of OvarymanjuNo ratings yet
- Luna vs. RodriguezDocument1 pageLuna vs. RodriguezMP ManliclicNo ratings yet
- Klasa - 7 - Placement - Test - Answer KeyDocument2 pagesKlasa - 7 - Placement - Test - Answer KeyKarolina PawlakNo ratings yet
- Various Cases in ConflictsDocument221 pagesVarious Cases in ConflictsHollyhock MmgrzhfmNo ratings yet
- Orders Relating To The National Anthem of IndiaDocument5 pagesOrders Relating To The National Anthem of IndiabharathpatriotNo ratings yet
- Active Lease Summary ReportDocument62 pagesActive Lease Summary ReportchangNo ratings yet
- Authorship of SuttasangahaDocument8 pagesAuthorship of SuttasangahaThan PhyoNo ratings yet
- Freshers' Moot - FM12 - Memorial For The PetitionerDocument29 pagesFreshers' Moot - FM12 - Memorial For The PetitionerAMITHAB SANKARNo ratings yet
- Aphra BehanDocument4 pagesAphra Behansushila khileryNo ratings yet
- Giving Directions Prepositions of Place PlacesDocument1 pageGiving Directions Prepositions of Place PlacesItzel MatiasNo ratings yet
- History Midterm NotesDocument2 pagesHistory Midterm Notesjerick DeligeroNo ratings yet
- Guaranty Agreement For Corporate Guarantor Dcma Form 1620Document2 pagesGuaranty Agreement For Corporate Guarantor Dcma Form 1620Tira MagdNo ratings yet
- PGK Precision Artillery KitDocument2 pagesPGK Precision Artillery KithdslmnNo ratings yet
- Commission On Audit Circular NoDocument6 pagesCommission On Audit Circular NoDondi AbacaNo ratings yet
- X 018 CurDocument4 pagesX 018 CurdedogNo ratings yet
- Livret - 0927 43181 2 PDFDocument82 pagesLivret - 0927 43181 2 PDFCarolina Caballero BastidasNo ratings yet
- MahaDocument4 pagesMahaKinjal KapadiaNo ratings yet
- Legal Aspects of Business: Indian Institute of Management, Rohtak Post Graduate ProgrammeDocument5 pagesLegal Aspects of Business: Indian Institute of Management, Rohtak Post Graduate ProgrammeAKANKSHA SINGHNo ratings yet
- CG Power and Industrial Solutions LimitedDocument27 pagesCG Power and Industrial Solutions LimitedMani KandanNo ratings yet
- MSc Zoology Merit List Fall 2019Document17 pagesMSc Zoology Merit List Fall 2019FarzanaNo ratings yet
- United States Court of Appeals, First CircuitDocument8 pagesUnited States Court of Appeals, First CircuitScribd Government DocsNo ratings yet
- Bmt5121 Corporate Goverance and Ethics Digital Assignment 3Document17 pagesBmt5121 Corporate Goverance and Ethics Digital Assignment 3Barani Kumar NNo ratings yet
- PEOPLE OF THE PHILIPPINES, Plaintiff-Appellee, JUAN BRIOSO and MARIANO TAEZA, Defendants-AppellantsDocument67 pagesPEOPLE OF THE PHILIPPINES, Plaintiff-Appellee, JUAN BRIOSO and MARIANO TAEZA, Defendants-AppellantsAngeli Pauline JimenezNo ratings yet
- 51st SMS Pan Atlantic Omnibus PollDocument32 pages51st SMS Pan Atlantic Omnibus PollDirigo BlueNo ratings yet
- Indonesia New PortsDocument5 pagesIndonesia New PortsyingmeitanNo ratings yet
- Korman Letter To WSSC RE Police DepartmentDocument2 pagesKorman Letter To WSSC RE Police DepartmentAnonymous sKgTCo2No ratings yet
- 25 CONVOCAca ODocument2 pages25 CONVOCAca OPr walcyr JuniorNo ratings yet