Professional Documents
Culture Documents
Occular Surface Injury
Uploaded by
JimmyCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Occular Surface Injury
Uploaded by
JimmyCopyright:
Available Formats
FROM OUR SOUTH ASIA EDITION
Ocular surface injuries
& management
(c) R P Centre of Ophthalmic Sciences, AIIMS
Clinical photograph of a case of conjunctival laceration with a foreign body
Anubha Rathi continuous epithelium. Alkali burns: The common alkaline
Senior Resident, Cornea, Cat- Being the most exposed part of the sources include ammonia, lime or
aract and Refractive surgery eye, the ocular surface is highly calcium hydroxide, lye or sodium
services, Dr R P Centre of
Ophthalmic Sciences, AIIMS prone to injury. This article covers the hydroxide and magnesium hydrox-
spectrum of various ocular surface ide. The most common alkali causing
injuries and their management. ocular surface burns is lime while the
Rajesh Sinha most severe is ammonia. Ammonia,
Additional Professor, Cornea,
Cataract and Refractive sur- Classification found in fertilisers and floor cleaners,
gery services, Dr R P Centre of Ocular surface injury is a broad term has the most rapid penetration into
Ophthalmic Sciences, AIIMS which includes the following: the surface due to its lipid as well as
• Ocular surface chemical and water solubility. Alkali burns are more
Neelima Aron thermal burns or injuries severe than acid burns as they lead to
Senior Resident, Cornea, Cat- • Conjunctival laceration saponification of cell membranes and
aract and Refractive surgery • Corneal perforation intercellular bridges facilitating rapid
services, Dr R P Centre of penetration into the deeper layers
Ophthalmic Sciences, AIIMS
• Eyelid laceration
and into aqueous and vitreous cavi-
ties. Alkali burns cause stimulation of
Namrata Sharma
Ocular surface chemical nerve endings of cornea and conjunc-
Professor, Cornea, Cataract and thermal burns tiva and hence are more painful.5
and Refractive surgery servic- Chemical injury may involve the Acid burns: Sulphuric acid is the
es, Dr R P Centre of Ophthal- ocular surface to a variable degree
mic Sciences, AIIMS most common acid implicated in
depending on the nature of the acid induced ocular surface burns.
chemical agent, duration of exposure, Hydroflouric acid leads to the most
Introduction concentration and volume of the severe burns as it is highly reactive
The term ‘ocular surface’ was first de- agent. Host factors such as the na- with rapid and deep penetration just
fined by Thoft in 1987 as a combined ture and health of the ocular surface like alkalis. Acids in general cause less
unit including the cornea, conjunctiva, itself also plays an important role in severe burns as compared to alkalis.
lacrimal glands and eyelids. Gibson deciding vulnerability of the surface They lead to coagulation and precip-
further described this term in 2007 to to injury. itation of proteins which in itself acts
include the surface and glandular epi- Most of the ocular surface chem- as a physical barrier, thus preventing
thelia of the cornea, conjunctiva, lacri- ical burns are due to either acids or further penetration of the agent.
mal gland, accessory lacrimal glands, alkalis. Alkali burns account for two- Several classication systems have
meibomian glands and the eyelashes thirds of these.3 A majority of these been suggested and proposed for oc-
with their associated glands of Moll burns occurs in young males with ular surface chemical injuries. Prom-
and Zeis along with the nasolacrimal increased risk of exposure to chemi- inent ones include Hughes classifica-
duct.1,2 These components of the cals in the workplace. tion4 (1946), Roper-Hall classification5
ocular surface are connected with a (1965) and Dua’s classification6 (2001).
Continues overleaf ➤
© The author/s and Community Eye Health Journal 2018. This is an Open Access
article distributed under the Creative Commons Attribution Non-Commercial License.
COMMUNITY EYE HEALTH JOURNAL | VOLUME 29 | ISSUE 99 | 2017 S11
OSD indexing_LB1.indd 11 25/04/2018 18:42
FROM OUR SOUTH ASIA EDITION
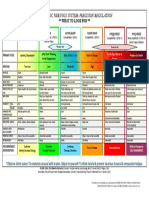
Table 1a. Roper-Hall classification
Table 1b. Dua’s classification
These classification systems hold true presents as a limitation in the prog- ent with peri limbal ischemia (Figure
for cases of acute chemical injuries. nostication of the burns according 1a), corneal and conjunctival epithe-
In chronic cases with already estab- to grade as the prognosis is highly lial defects (Figure 1b) and retained
lished sequelae of chemical burns, variable in burns with just 50% limbal chemical particles especially in the
the ocular surface health may be ischemia as compared to burns with fornices (Figure 1c). Milder burns
graded using the Holland-Mannis total limbal ischemia. Dua’s classifica- show re-epithelialisation gradually
classification system. tion in 2001 addressed this limitation with or without treatment. More
The two commonly used classi- and classified ocular surface chemical severe burns may develop compli-
fication systems , Dua’s (2001) and burns based on the clock hours of cations such as persistent epithelial
Roper-Hall (1964) are summarised conjunctival and limbal involvement. defects, dry eye, symblepharon, anky-
in Table 1a and Table 1b.5,6 The Clinical features of ocular surface loblepharon, cicatricial entropion or
Roper-Hall classification system has chemical burns: In the acute stage ectropion, and in rare and severe
classified all burns with more than up to one week post injury, ocular cases corneo scleral melt.
50% limbal ischemia in Grade IV. This surface chemical burns usually pres-
Figure 1. Clinical presentation of acute chemical injury
Figure 1a. Perilimbal ischemia Fig 1b. Persistent epithelial defect Fig 1c. Retained chemical parti-
cles in superior fornix
Continues overleaf ➤
© The author/s and Community Eye Health Journal 2018. This is an Open Access
article distributed under the Creative Commons Attribution Non-Commercial License.
COMMUNITY EYE HEALTH JOURNAL | VOLUME 29 | ISSUE 99 | 2017 S12
OSD indexing_LB1.indd 12 25/04/2018 18:42
FROM OUR SOUTH ASIA EDITION
Figure 2. Impact of a simple limbal epithelial transplantation (SLET)
Figure 2a. A pre-operative case of chronic Figure 2a. A pre-operative case of chronic
chemical injury with total LSCD chemical injury with total LSCD
Management of ocular surface Limbal stem cell transplantation in an emergency medical setting.
chemical burns: Ocular surface may be done using fellow eye limbal There may be associated adnexal
chemical burn is a medical emergen- stem cells or cadaveric limbal stem injuries, and /or scleral perforation.
cy. Immediate irrigation of the eye cells. Simple limbal epithelial trans- The major goals of management of
should be done with clean running plantation (SLET) has been done with a corneal perforation are to remove
water, ringer lactate or normal saline favourable outcomes in such cases any contaminants in the wound area,
until the pH of the ocular surface is (Figure 2a and Figure 2b). repair the tear and maintain the
neutralised. This has to be meticu- water tight integrity of the globe. Cor-
lously done using double eversion of Conjunctival laceration neal perforation may also be associ-
the eyelids. Conjunctival laceration may occur ated with a foreign body (Figure 4).
Timely treatment should then be following blunt or penetrating Partial thickness lacerations may
instituted. Medical treatment includes trauma. It presents with chemosis heal on their own with time. Such
topical antibiotics, cycloplegics, topi- and subconjunctival haemorrhage. cases may require patching in the
cal steroids, topical sodium ascorbate In such cases, it is important to rule immediate phase followed by topical
10%, topical sodium citrate 10%, oral out underlying scleral perforation. antibiotics. Full thickness lacerations
doxycycline, oral ascorbate and tear The fundus should be examined for may be repaired using interrupted
substitutes.7 any retinal tear or intraocular foreign 10-0 monofilament nylon sutures.
Amniotic membrane transplan- body. An ultrasound may be done In case of associated scleral involve-
tation is beneficial in moderate to for the posterior segment evalua- ment, the scleral wound should also
severe chemical burns. It promotes tion. Such cases are managed with be sutured using 6-0 vicryl suture.
re-epithelialisation, decreases the in- observation and topical antibiotics in In case of uveal prolapse, the uveal
cidence of symblepharon formation, mild cases and in large lacerations, tissue that is not necrotic and has
and decreases inflammation.8 surgical repair may be needed using protruded for less than 24 hours may
In chronic cases with already 8-0 vicryl suture (Figure 3). be reposited back or and any old or
established limbal stem cell defi- necrotic prolapsed tissue carefully
ciency or symblepharon formation, abscised. Other than conventional
ocular surface rehabilitation may be
Corneal perforation interrupted sutures, biological glue
Corneal lacerations and perforations
required with symblepharon release has also been used to seal the per-
represent approximately 1 in 10 of
with or without amniotic membrane forations especially those with tissue
ocular traumatic injuries presenting
transplantation. defect.
Figure 3. Conjunctival laceration Figure 4. Corneal perforation Figure 5. Medial eyelid lacera-
with a wooden foreign body with a metallic foreign body tion involving the canaliculus
© The author/s and Community Eye Health Journal 2018. This is an Open Access
article distributed under the Creative Commons Attribution Non-Commercial License.
COMMUNITY EYE HEALTH JOURNAL | VOLUME 29 | ISSUE 99 | 2017 S13
OSD indexing_LB1.indd 13 25/04/2018 18:42
FROM OUR SOUTH ASIA EDITION
Several studies have shown the For corneo scleral lacerations, it lacerations require surgical repair.
beneficial effect of isobutyl cyanoacr- is important to perform a 360 degree Uncomplicated lid lacerations with
ylate glue for treatment of corneal peritomy and see the extent of scleral no lacrimal system involvement can
perforations with tissue defect up to involvement, following which the lim- be repaired using interrupted silk
3 mm.9-10 bus is secured with vicryl or monola- sutures. In case of medial lid injuries
While suturing a corneal perfo- ment nylon suture. Corneal sutures (Figure 5) with damage to the lacrimal
ration, it is important to identify the are placed as described above. Scleral system, canalicular repair is required
major landmarks, especially limbus. wound is closed using ‘close as you along with lid laceration repair.
It is advisable to preserve as much go’ or zippering technique. Disinser-
anatomy as possible and not over tion and reinsertion of recti may be Conclusion
excise. The technique is to progres- required in posterior tears. Ocular surface injuries are fairly com-
sively halve the wound while passing mon owing to vulnerability of the ex-
sutures. They should be at 90% depth
in the cornea. ‘No touch technique’
Eyelid lacerations posed ocular surface to trauma. They
Eyelids and lacrimal system are as range from ocular surface chemical
while passing sutures ensures a burns, conjunctival laceration, corneal
much a part of the ocular surface as
maintained anterior chamber during perforation and eyelid laceration.
the cornea and conjunctiva. Simple
suturing. The central suture bites Effective and timely management of
eyelid lacerations, which are hori-
should be smaller and the length of these types of injuries is essential for
zontal follow skin lines and involve
suture should increase as one goes maintaining the integrity of the ocular
less than 25% of the lids, usually heal
towards periphery. surface.
well even without suturing. Larger lid
References & summary of present knowledge. Arch Ophthal. 1946; 35: Park WC et al. Amniotic membrane transplantation for acute
1 Gipson IK. The Ocular Surface: The Challenge to Enable and 423–449 chemical or thermal burns. Ophthalmology May;107(5):980-9
Protect Vision. Investigative ophthalmology & visual science. 5 Roper-Hall MJ. Themal and chemical burns. Trans Ophthalmol 2000
2007;48(10):4390-4398 Soc UK 1965;85:631–53 9 Vote BJ, Elder MJ. Cyanoacrylate glue for corneal perforations:
2 Kinoshita S, Adachi W, Sotozono C, et al. Characteristics of the 6 Dua HS, King AJ, Joseph A. A new classification of ocular surface a description of a surgical technique and a review of the
human ocular surface epithelium. Prog Retin Eye Res. burns. Br J Ophthalmol 2001;85:1379–83 literature. Clinical & Experimental Ophthalmology 2000,
2001;20:639–673 28(6):437-442
7 Haddox IL. Pster RR, Yuille-Barr D: The efficacy of topical citrate
3 Morgan SJ: Chemical burns of the eye: causes and after alkali injury is dependent on the period of time it is 10 Khalifa YM et al. Management of nontraumatic corneal
management. Br J Ophthalmol 1987; 71:854-857 administered. Invest Ophthalmol Vis Sci 1989; 30: 1062-1068 perforation with tectonic drape patch and cyanoacrylate glue.
Cornea. 2010 Oct;29(10):1173-5
4 Hughes Jr WF. Alkali burns of the cornea. I. Review of the litera. 8 Meller D, Pires RTF, Mack RJS, Figueiredo F, Heiligenhaus A,
© The author/s and Community Eye Health Journal 2018. This is an Open Access
article distributed under the Creative Commons Attribution Non-Commercial License.
COMMUNITY EYE HEALTH JOURNAL | VOLUME 29 | ISSUE 99 | 2017 S14
OSD indexing_LB1.indd 14 25/04/2018 18:42
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Foundations For Clinical Mental Health Counseling - 3rd EditionDocument369 pagesFoundations For Clinical Mental Health Counseling - 3rd EditionJamie Finotti100% (7)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Sistema NervosoDocument1 pageSistema NervosoPerisson Dantas100% (2)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Our Survival of SoulDocument463 pagesOur Survival of SoulAnonymous Mq8EkiAyhM100% (2)
- Response in OppositionDocument36 pagesResponse in OppositionForeclosure FraudNo ratings yet
- Sociology in NursingDocument8 pagesSociology in Nursingkamalab04100% (5)
- Altitude Diving PhysiologyDocument12 pagesAltitude Diving PhysiologyKarin Gandeswari100% (1)
- Intracranial Pressure: Current Perspectives On Physiology and MonitoringDocument11 pagesIntracranial Pressure: Current Perspectives On Physiology and MonitoringWander ValentimNo ratings yet
- Segmentos Ica 2022 PDFDocument9 pagesSegmentos Ica 2022 PDFRoberto RodríguezNo ratings yet
- ADHERENCE and INVASION ASSAYS A092Document2 pagesADHERENCE and INVASION ASSAYS A092Samrah Anwar0% (2)
- Computer Forensics As A Part of A Security Incident Response ProgramDocument32 pagesComputer Forensics As A Part of A Security Incident Response ProgrammanojNo ratings yet
- Concept of Health EducationDocument14 pagesConcept of Health EducationYou PanhamorokotNo ratings yet
- Triamcinolone AcetonideDocument12 pagesTriamcinolone Acetonideawais khanNo ratings yet
- Skema Modul Skor A+ Bab 5Document8 pagesSkema Modul Skor A+ Bab 5Siti MuslihahNo ratings yet
- Karyotype WorksheetDocument4 pagesKaryotype WorksheetKellieM.8406No ratings yet
- Genny Suwandi - DVIDocument18 pagesGenny Suwandi - DVIgennysuwandiNo ratings yet
- Philippine Health Care Delivery SystemDocument24 pagesPhilippine Health Care Delivery SystemoisloeNo ratings yet
- VST Electronic Medical RecordsDocument2 pagesVST Electronic Medical RecordsarunsahayakumarNo ratings yet
- Murli Deora v. Union of India (Banning of Smoking in Public Places)Document2 pagesMurli Deora v. Union of India (Banning of Smoking in Public Places)Prerna SinghNo ratings yet
- Health Economics: Which of The Following Is Not A Reason For Increased Health Spending?Document8 pagesHealth Economics: Which of The Following Is Not A Reason For Increased Health Spending?Arjun Aryal100% (1)
- Seal of Good Local Governance For Barangay (SGLGB)Document2 pagesSeal of Good Local Governance For Barangay (SGLGB)Ponciano AlveroNo ratings yet
- SP - Sindy MilaDocument2 pagesSP - Sindy MilaSindy MelindaNo ratings yet
- Seafarer Medical CertificateDocument2 pagesSeafarer Medical CertificateKoki ToNo ratings yet
- Giving Injection &applying InfusionDocument17 pagesGiving Injection &applying InfusionIsmaNo ratings yet
- Maxicare-Affiliated Providers - DOH-Certified Laboratories For COVID-19 Testing (Jan 22, 2021)Document2 pagesMaxicare-Affiliated Providers - DOH-Certified Laboratories For COVID-19 Testing (Jan 22, 2021)Marites BarnidoNo ratings yet
- Water Pollution Is The Contamination ofDocument36 pagesWater Pollution Is The Contamination ofsuradotNo ratings yet
- 2017-02-23 Calvert County TimesDocument24 pages2017-02-23 Calvert County TimesSouthern Maryland OnlineNo ratings yet
- REPORT ON YOGA RESEARCH STUDIES AT ACYTER, JIPMER: 2008 To 2012.Document126 pagesREPORT ON YOGA RESEARCH STUDIES AT ACYTER, JIPMER: 2008 To 2012.Yogacharya Dr Ananda Balayogi BhavananiNo ratings yet
- Dictation. Fill in The Gaps With A Word From The ListeningDocument1 pageDictation. Fill in The Gaps With A Word From The ListeningNU MaseNo ratings yet
- Prevalence of Water Borne Diseases Within Households in The Bamendankwemunicipalitynorth West Cameroon 2332 0893 1000122Document7 pagesPrevalence of Water Borne Diseases Within Households in The Bamendankwemunicipalitynorth West Cameroon 2332 0893 1000122Welly SuryaNo ratings yet
- AbraDocument4 pagesAbralhhjklllNo ratings yet