Professional Documents
Culture Documents
Evolutionary Consequences of Drug Resistance: Shared Principles Across Diverse Targets and Organisms
Uploaded by
Luis ZabalaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Evolutionary Consequences of Drug Resistance: Shared Principles Across Diverse Targets and Organisms
Uploaded by
Luis ZabalaCopyright:
Available Formats
REVIEWS
Evolutionary consequences of drug
resistance: shared principles across
diverse targets and organisms
Diarmaid Hughes and Dan I. Andersson
Abstract | Drug therapy has a crucial role in the treatment of viral, bacterial, fungal and
protozoan infections, as well as the control of human cancer. The success of therapy is
being threatened by the increasing prevalence of resistance. We examine and compare
mechanisms of drug resistance in these diverse biological systems (using HIV and
Plasmodium falciparum as examples of viral and protozoan pathogens, respectively) and
discuss how factors — such as mutation rates, fitness effects of resistance, epistasis
and clonal interference — influence the evolutionary trajectories of drug-resistant
clones. We describe commonalities and differences related to resistance development
that could guide strategies to improve therapeutic effectiveness and the development of
a new generation of drugs.
The success of modern medicine is mostly based on the influenza viruses — are also extremely clinically impor-
use of drug therapy to control or cure infections that are tant, but we have limited the scope of this Review in the
caused by various pathogens, as well as other diseases interests of space and because lessons learned from HIV
such as cancer 1. This legacy is currently threatened by can be applied to other human viruses. Each system has
the development and evolution of resistance to the drugs particular features that affect the trajectories of resist-
on which these therapies rely. ance evolution (TABLE 1). We highlight the features that
There are multifaceted aspects of drug resistance they have in common and the problems that are unique
that are being actively studied, such as the emergence to each system.
and molecular nature of the resistance mutations, the
fitness consequences of resistance (in the presence and Systems and their drug-resistance mechanisms
absence of drugs) and how these aspects influence the We ask below to what extent mechanisms of resistance
evolutionary trajectories of the resistant viruses or cells. development are common across systems and which, if
A more complete understanding of these features will be any, are unique.
crucial to predict resistance and to combat it through the
optimal use of existing drugs (concentrations, periodic HIV. HIV, the RNA virus that causes AIDS, has very high
drug removal or switching, and drug combinations) and spontaneous mutation rates of 10−4–10−5 per nucleotide
to guide the design of new drugs. per genome replication2,3, and it can also undergo inter-
In this Review, we discuss diverse aspects of drug viral recombination within the human host to generate
resistance, including mechanisms, evolutionary conse- novel virus variants4. Despite its high mutation rate,
Uppsala University, quences and therapeutic implications. We broadly cover genetic variation in HIV may be ultimately constrained
Department of Medical
viral (using HIV as an example), bacterial and fungal by the need of the virus to successfully transmit to a new
Biochemistry and
Microbiology, Biomedical infections, vector-borne parasites (using Plasmodium human host.
Center, BOX 582S‑75123, falciparum as an example), and the uncontrolled cell Three major classes of drugs are used to combat
Uppsala, Sweden. growth that is associated with human cancers. These AIDS caused by HIV. Nucleoside reverse transcriptase
Correspondence to D.H. choices were made for their importance in human health inhibitors (NRTIs) and non-nucleoside reverse tran-
e-mail: diarmaid.hughes@
imbim.uu.se
and the quality of data relating to the mechanisms and scriptase inhibitors (NNRTIs) result in the termination of
doi:10.1038/nrg3922 dynamics of drug-resistance development. We are aware reverse transcription and hence block viral replication5,6,
Published online 7 July 2015 that other systems — for example, the hepatitis and whereas viral protease inhibitors affect viral maturation7.
NATURE REVIEWS | GENETICS VOLUME 16 | AUGUST 2015 | 459
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
Table 1 | Distinctions and similarities of biological systems treated with drugs to control growth and transmission
HIV Pathogenic bacteria Pathogenic fungi Plasmodium Human cancer
falciparum
Host Human Human, animal, plant and Human, animal, plant and Human and Human
environmental environmental mosquito
Infection Intracellular Extracellular (either on Extracellular (either on Extracellular and Tumour cell growth and
lifestyle the host’s body surface the host’s body surface or intracellular metastasis
or an internal infection) an internal infection), and
and/or intracellular intracellular (microsporidia)
Genome size 9.7 kb, ssRNA 1.8 Mb (Haemophilus Varied: ≥2.5 Mb 22.9–26.8 Mb 3.2 Gb (only a subset of
genome influenzae) to 6.3 Mb (microsporidia), 14.9 Mb sequence is associated
(Pseudomonas (Candida albicans) and with cancer)
aeruginosa), dsDNA 29.4 Mb (Aspergillus
genome fumigatus)
Mutation rate ≈10−5 per nt ≈10−10 per nt per ≈10−10 per nt per ≈10−9 per bp per Mutation is an initiating
per genome generation11. Gene generation (Saccharomyces generation164 event; subsequently huge
replication2,3 amplification 10−2–10−5 cerevisiae)163 variation in mutation rate
per gene per generation13 as cancer develops
Mechanisms Mutation Mutation, genomic Mutation and genomic Mutation Mutation and genomic
of genetic and interviral rearrangements and rearrangements15 and genomic rearrangements29,32
diversification recombination4 horizontal gene transfer19 rearrangements24
In‑host 107–108 Highly variable Complicated by many fungi 103–4 × 104 Very varied: from 1 to 10
population productively depending on the having a dimorphic lifestyle merozoites (the form circulating tumour cells
size estimates infected human pathogen and infection (yeast and hyphal forms). that subsequently per 10 mL blood169, up
cells165 generating site. Up to 1011 per Candida albicans, ≥108 invades red blood to ~108 cells per gram
up to 1010 virions bladder in urinary tract cfu per gram caecum in a cells) per infected of tumour tissue67 (with
per day2,3 infections166 murine infection model167 liver cell168 tumours potentially
growing up to over 1 kg
in weight)
Major causes HIV viral growth Tissue damage as a result Tissue damage as a result Growth of Growth of cancer cells can
of disease leads to the of the immune system of the immune system Plasmodium exert pressure on various
symptoms destruction of CD4 response to bacterial response to fungal growth. falciparum within organs and tissues, reduce
human immune growth. Many pathogenic Some pathogenic fungi human red blood available energy supply,
system T cells, bacteria also release also release toxins that cells causes their release substances that
causing increased toxins that directly directly damage human destruction, leading change physiology and
susceptibility to damage human tissue tissue to the symptoms of affect the activity of the
other infections malaria immune system
Transmission Person to person Multiple routes: person Multiple routes: person to Vector-borne No transmission, but
routes via sexual contact to person (touch, sexual person; water; fomites; and (human to mosquito cancer may be induced
or exposure to intercourse, saliva and opportunistic infections to human) by infectious agents such
body fluids air); food; water; insects; in immunosuppressed as Helicobacter pylori or
and fomites individuals human papilloma virus
cfu, colony-forming unit; dsDNA, double-stranded DNA; nt, nucleotide; ssRNA, single-stranded RNA.
Resistance to NRTIs and NNRTIs arises by mutations genome, which is mediated by recombination between
that affect reverse transcriptase8. Resistance to protease repeated sequences in the genome13. Amplification
inhibitors also arises by mutation, usually by reducing the occurs at a rate of >10−2–10−5 per gene per replication
catalytic activity of the protease and conferring a fitness and can cause resistance, for example, by amplifying a
cost for resistance9 (see BOX 1 for a summary of meth- gene encoding a β‑lactamase with low intrinsic activity
ods for measuring fitness). To reduce the probability of against a particular drug substrate14. Bacteria can also
resistance development, combination therapy with three become resistant by horizontal gene transfer (HGT)
or more drugs is used to suppress HIV replication rates from a very extensive gene pool (via bacteriophage
to below the level of detection10. transduction, conjugation or transformation), whereas
genetic exchange in fungi is limited to recombination
Bacteria and fungi. Bacteria and fungi have much lower within species15. HGT processes in bacteria can cause
mutation rates than RNA viruses, of up to ~10−10 per multidrug resistance in a single genetic event 16. Most
nucleotide per replication cycle. These less frequent bacterial and fungal pathogens are not dependent on
mutations limit the rate of resistance development by their ability to infect humans for survival. As a con-
mutation11, although subpopulations of cells with muta- sequence, the selective forces that drive bacterial and
tor phenotypes have rates that are 1,000‑fold higher 12. fungal pathogen evolution include survival in patients
An important class of resistance-associated mutation in undergoing drug therapy and survival in environments
bacteria is duplication or amplification of parts of the in which drug exposure may be at a very low level.
460 | AUGUST 2015 | VOLUME 16 www.nature.com/reviews/genetics
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
The most important classes of antibacterial drugs in
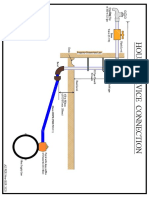
Box 1 | Methods for measuring fitness
terms of quantity used are the β‑lactams, fluoroquinolo-
Biological fitness, defined as replicative success relative to competing organisms in nes and macrolides. Mechanisms of resistance include
a particular environment, comprises survival, reproduction and transmission (see spontaneous mutation — in particular, mutations that
the figure, which summarizes how each component of fitness can be measured). alter the drug target or that upregulate drug efflux — and
Organisms in nature must often be capable of surviving in multiple spatial and the acquisition of resistance genes by HGT17. The relative
temporal environments. Although fitness measurements in a laboratory cannot
importance of mutation versus HGT depends on drug
capture the full complexity of real life, they can be a useful proxy to predict relative
class and bacterial species. In Mycobacterium tuberculosis,
fitness in the real world19. Assays of fitness in the laboratory include growth rate
and competitiveness in vitro, as well as survival, virulence and competitiveness in
resistance occurs exclusively by spontaneous muta-
animal or cell infection models. These methods are complemented by tion18. In Gram-negative and Gram-positive bacteria,
deep-sequencing approaches that increase the possibility of examining relative resistance to β-lactams occurs almost exclusively by the
fitness in complex populations, including in natural and host environments. acquisition of β‑lactamases by HGT, whereas resistance
Additionally, animal models and epidemiological studies, including population to fluoroquinolones is primarily associated with muta-
surveillance, can provide insights into real-life fitness over longer time periods in tions, although HGT also contributes17,19. HGT is very
clinical and natural environments and can be used to estimate the effects of important clinically because the genetic linkage of resist-
resistance on transmission to new hosts21,150,151. ance genes on mobile elements causes multidrug resist-
The gold standard for measuring relative fitness in vitro and in vivo is growth ance16. Finally, a resistance mechanism that is sometimes
competition of isogenic variants using genetically tagged strains19,80. For example, overlooked is the ability of bacteria to form biofilms dur-
the relative fitness of isogenic HIV variants was recently measured using ing infection, thus providing physical and physiological
synonymous nucleotide substitutions as tags36,152. Competition assays may need
protection against drug therapy 20.
to be complemented with whole-genome sequencing or deep sequencing to
The most important classes of antifungal drugs
overcome the potential complications that are caused by high frequencies of
genetic amplification (in bacteria) or point mutations (in viruses). In bacteria the are the azoles, the echinocandins and the polyenes15.
steady-state frequency of amplification is in the range of 10–2–10–4 per gene, and Resistance is caused by mutations that increase efflux,
they are frequently selectively maintained by antibiotics13,153. In RNA viruses, alter the drug target or change cell metabolism to reduce
extremely high mutation rates can generate a quasi-species of competing viral the accumulation of toxic products in the presence
genomes within the host154,155. Deep sequencing can reportedly detect viral variants of the drug 15. Fungi do not have access to a wide gene
at frequencies as low as 0.1% in a heterogeneous population156–158. Another very pool for HGT, and resistance development is dependent
promising method is lineage tracking, which uses sequencing of random genetic on mutation rates.
barcodes to observe evolutionary dynamics in populations, as was recently applied
in yeast159. Plasmodium falciparum. The vector-borne pathogen
Deep sequencing can also be used to predict drug efficacy and resistance P. falciparum must passage between an invertebrate
development. A recent study of domain 1 of the NS5A protein in hepatitis C virus, host — the mosquito — and a vertebrate host — the
targeted by daclatasvir, used mutagenesis to generate every possible amino acid
human — typically encountering drug selection only in
substitution, and then applied deep sequencing to quantify the effects of individual
mutations on replication fitness and drug sensitivity160. Such data could be used to
the human host 21. Successful transmission is essential,
quantify genetic barriers to resistance and to predict clinical outcomes using and any evolution of drug resistance is only possible to
mathematical models. the extent that it does not break the complex cycle of
Deep sequencing that is focused on a subset of genes also has an important role transmission.
in high-resolution studies of cancer evolution161. Heterogeneity within tumours The major drug classes used in the treatment of
creates an environment for the selection of the fittest clones (based on resource malaria are chloroquine, sulfadoxine–pyrimethamine
competition), and understanding these processes provides a basis for optimizing and artemisinin22. Chloroquine inhibits haemoglobin
drug therapy and for predicting tumour development. However, it is difficult to degradation, causing haem to accumulate to toxic levels
achieve sufficient sequence depth and resolution to detect small subpopulations in P. falciparum, and sulfadoxine–pyrimethamine inhib-
before they acquire additional critical mutations that facilitate expansion and its DNA and RNA synthesis by blocking the folate bio-
proliferation162. Currently, deep sequencing is the methodology that provides synthesis pathway 22. The mode of action of artemisinin
the best information on cancer cell fitness, but a caveat to interpretation is that the
is still controversial, but recent research suggests that it
most prevalent cell type may not necessarily be the most important cell type that
is activated by interaction with ferrous iron and that an
leads to patient death.
Fe–artemisinin adduct then interacts with a calcium
pump enzyme, PfATP6, which leads to the loss of
Survival Reproduction function of the calcium pump and to the death of the
• Viability in vitro over time at different • Exponential growth rates, lag
drug concentrations phases and yields for single strains P. falciparum23. Resistance to chloroquine and the anti-
• Survival assays in vitro (e.g. stationary cultured in different media folates caused by mutation is widespread, and the current
phase, serum resistance and survival during • Competition between strains standard of care is to use artemisinin-based combination
exposure to reactive oxygen species, in different media during
low pH, and so on) exponential growth and complete therapies as the first-line treatment for malaria caused by
• Survival assays in cell cultures growth cycles P. falciparum24. However, artemisinin-resistant malaria,
(e.g. phagocytic cells) • Deep-sequencing techniques to with a phenotype of delayed clearance after therapy, has
• Survival assays in hosts (animals or humans) monitor population dynamics
recently been identified in South-East Asia25,26, putting
the efficacy of this essential drug therapy at risk27,28. In
Transmission conclusion, resistance to antimalarial drugs arises by
• Epidemiological data
• Animal and human experimental point mutations, and there is no evidence that it is asso-
models of transmission ciated with a high mutation rate or HGT. The slow rate
of global resistance development, despite the very heavy
Nature Reviews | Genetics
NATURE REVIEWS | GENETICS VOLUME 16 | AUGUST 2015 | 461
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
Isogenic variants use of only a few antimalarial drugs over several decades, in the evolution of stable resistance13. Some resistance
Genetic variants that are may be a consequence of the small mutation supply rate mechanisms are specific to cancer, including the pro-
derived from a single cell and the difficulty in developing low-cost resistance by motion of the epithelial-to-mesenchymal transition by
or genotype. drug-target mutations. chemotherapy 32. This transition is an important step in
Epistatic
cancer metastasis, as cells develop a morphology that is
Refers to the phenomenon Human cancer. Human cancer cells are subjected to associated with increased motility and invasive capac-
of epistasis, which involves intense drug selection pressure, but as cancer develops ity 29. The growth environment of cancer cells in a solid
interactions (genetic, de novo in each individual, the only equivalent to trans- tumour is itself associated with an increased probability
regulatory, and physiological)
mission is within the individual in the form of metastasis of surviving drug therapy 33. This protection bears com-
between or within genes and
results in non-additive effects
— the movement of cancer cells to establish tumours parison to the resistance shown by bacteria growing as
with regard to phenotype. at other body sites. Thus, cancer differs from infectious biofilms, combining elements of physical protection with
diseases in that drug resistance and the relative fitness altered physiological states. Finally, epigenetic changes
of cancer cells are not properties that are transmitted (reversible DNA methylation patterns and histone modi-
between individuals. fication patterns) may influence cancer development 34
The targets of anticancer drugs include thymidylate and resistance to anticancer drugs35 by changing gene
synthase, DNA replication, topoisomerases I and II, expression patterns.
and tubulin, and resistance mechanisms include point
mutations, deletions and genetic rearrangements or Fitness costs of drug resistance
amplifications29. Chromosomal instability is a common Common mechanisms by which drug resistance arises
feature of cancers (amplifications, deletions and other are target alterations, reductions in internal drug con-
rearrangements) and is associated with tumour hetero- centration and inactivation of (or failure to activate)
geneity and drug resistance30,31. This association is analo- the drug (FIG. 1). Because drugs target important cel-
gous to the situation in bacteria in which amplifications lular mechanisms, mutational resistance is frequently
can protect against drug therapy and function as a step associated with reduced replicative fitness. There are
many documented examples of the fitness costs that
are associated with drug resistance in different systems.
Potential costs For example, a dual-infection competition assay
• Metabolic costs of activity with sequence-tagged HIV36 (BOX 1) measured replica-
• Reduced uptake or increased
loss of essential compounds tive fitness costs caused by mutations leading to resist-
ance to NNRTI drugs37. The relative magnitude of the
fitness costs depended on the HIV subtype (subtype B or
subtype C), suggesting epistatic effects on fitness38.
The fitness costs of resistance in bacteria have been
extensively reviewed19,39,40. Briefly, most mutations and
b Concentration HGT that cause resistance in bacteria are initially asso-
regulation
ciated with fitness costs. In most cases, the cost can be
ameliorated by the acquisition of compensatory muta-
tions. However, there are examples in which mutational
resistance is apparently cost-free, with clinical data sug-
gesting that there is no significant fitness cost in infected
individuals41,42.
There is also evidence that fitness costs have a role
in limiting the establishment of resistance to one of the
major antifungal drug classes, the polyenes. Resistance to
c Enzymatic the most commonly used polyene, amphotericin B, which
a Target alteration action
is a drug that has been in use for more than 50 years, is
very rare clinically. Analyses in vitro and in animal mod-
Potential costs Potential costs els showed that every resistance mutation imposed huge
• Reduced kinetic • Metabolic cost of expression fitness costs on fungal pathogenicity, making the fungi
efficiency • Toxic breakdown products
• Downstream effects • Transport cost of enzyme hypersensitive to the host immune system and unable
to invade or damage host tissue43. This may be an exam-
Figure 1 | The nature of fitness costs in different ple of a drug that is effective against the target pathogen
systems. The diagram of a cell illustratesNature Reviews | Genetics
the three major and for which the mechanism of resistance is strongly
mechanisms of drug resistance: reducing interaction associated with reduced fitness. However, a downside of
with the drug target by mutation, modification or this drug is frequent treatment failure due to poor tissue
protection8,12,15,17,19,24,41,48 (part a); restricting the internal
penetration and dose-limiting renal toxicity 43.
concentration of the drug by altering efflux or influx16,17,19
(part b); and reducing the concentration of the active drug
In malaria therapy, the evidence suggests that resist-
by enzymatic activity that either degrades or fails to ance to all classes of antimalarial drugs, including arte-
activate the drug17,19 (part c). Each alteration can incur misinin, is associated with significant fitness costs to
general metabolic costs in addition to mechanism-specific P. falciparum in the absence of drug selection44, possibly
costs that negatively affect physiology19,52. explaining the slow development of resistance.
462 | AUGUST 2015 | VOLUME 16 www.nature.com/reviews/genetics
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
Wild type Drug-resistant Drug-resistant mutant Frequencies of mutant variants in clinical isolates of
mutant with fitness compensation HIV correlate with relative replicative fitness, explain-
a ing why the most resistant variant is not necessarily
Intragenic the most frequent 50. Interestingly, the fitness cost
mutation of an NNRTI-resistant double mutant (K103N and
L100I in reverse transcriptase) was compensated by
the addition of a third mutation (L74V) that itself is
b selected to confer NRTI resistance. This triple mutant
Increased is found clinically 51, suggesting that it is selected as
dosage
a fitness-compensatory combination that confers
cross-resistance to different drug classes.
c Genetic compensation of fitness costs for antibiotic
Intergenic resistance has been extensively reviewed13,39,52. Briefly,
mutation a temporal relief of fitness costs in bacteria is fre-
quently conferred by tandem amplification mutations,
increasing, for example, the activity of a rate-limiting
d enzyme. Stable fitness compensation can be conferred
Bypass by point mutations that improve the activity of a target
GGTCAATAATAGC GGTCAATAATAGC GGTCAATAATAGC mechanism
protein or the flow through a biochemical pathway.
An additional mechanism of compensation is the
Figure 2 | Common fitness-compensatory mechanisms. The figure represents increase in resistance owing to mutations that cause
proteins in which drug-resistance mutations (red circles) arise that cause
Nature a reduction
Reviews | Genetics the increased catalytic efficiency of an enzyme but
in organism fitness, and illustrates several different mechanisms of fitness that also decrease the stability of the enzyme to reduce
compensation19. a | Compensation by an intragenic mutation (dark green circle) is
fitness. Mutations in the same gene that increase
shown46,47,53. b | Compensation by increased dosage of a low-fitness mutant protein
is shown13,56. c | Compensation by an intergenic mutation (dark green circle) is shown, thermodynamic stability of the enzyme can compen-
which is relevant when protein complexes or protein interactions are involved in sate for such costs53. Analysis of compensation shows
physiological activity48,51. Different proteins are shown as light blue and light green that there are frequent epistatic interactions between
colours. d | A bypass mechanism whereby, for example, an additional regulatory factor the drug target mutations and components of the
compensates for the reduced functionality of the mutant protein19,49. physiology of the cell54,55.
Evidence for fitness costs of resistance in fungal
systems and subsequent cost compensation is sparse15
The interplay between fitness costs and resistance except for the evidence that resistance to ampho-
is complicated when there are mixed infections or, in tericin B is both costly and apparently very difficult to
the case of cancers, mixed cell populations. In cancer reduce by compensatory evolution43.
therapy, in which lineages within a tumour compete Epistasis is also involved in fitness compensation
for space and nutrients, a less aggressive chemotherapy in drug-resistant P. falciparum 56. Mutations in dihy-
can sometimes improve patient survival, in compari- drofolate reductase (pfdhfr), which confer resistance
son to overwhelming drug treatment that removes sus- to pyrimethamine, reduce parasite fitness and can be
ceptible cell lineages, allowing drug-resistant lineages compensated for by the amplification of the first gene
to kill the patient 45. in the folate synthesis pathway, GTP cyclohydrolase 1
The overall conclusion from all of these studies is (pfgch1). Because the amplification of pfgch1 itself
that fitness costs are a frequent consequence of primary confers low-level resistance, this amplification is prob-
resistance mutations across all systems tested. ably selected early by the drug and reduces the cost of
acquiring subsequent mutations in pfdhfr that further
Mechanisms of fitness cost compensation increase resistance56.
The potential mechanisms of fitness compensation for In human cancers undergoing drug therapy, the
the costs of drug resistance are outlined in FIG. 2. We population of cells accumulates mutations that result
consider below whether these mechanisms are shared for some in increased growth rates and/or drug resist-
across pathogens and systems. ance, but result for others in reduced growth rates
Genetic analysis of recombinant HIV viruses car- and/or associated drug resistance57,58. The variety of
rying resistance mutations has shown that in some genetic alterations within a cancer cell, and the range
cases compensatory mutations were selected within of different cancer cell genotypes that compete for
the genes encoding the drug targets to improve their growth within a tumour, make it difficult to defini-
function46,47 but in other cases that the compensation tively identify individual mutations conferring fitness
involved mutations in other regions of the virus48. costs or fitness compensation. We assume that the
An interesting example is that of drug resistance in interplay between mutational fitness costs and com-
HIV that is caused by multiple mutations in the pro- pensatory mutations has a role in determining the
tease that reduce fitness: the fitness consequences can progress of a cancer and the emergence of a dominant
be rescued by mutations in the vicinity of the viral clone, but to the best of our knowledge there is no
Gag proteolytic cleavage sites, leading to improved definitive evidence that associates specific mutations
processing of Gag by the highly mutated protease49. with fitness compensation.
NATURE REVIEWS | GENETICS VOLUME 16 | AUGUST 2015 | 463
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
Population bottlenecks Evolutionary dynamics and mechanisms to a particular drug (FIG. 3) and how a selective pressure
The concept that only a limited The rate at which drug resistance emerges and spreads in influences which mutants are selected. Which muta-
number of individuals (and a population of organisms (or cells in the case of cancer) tions will be enriched depends on the factors discussed
thus genotypes) act as is determined by the interplay of several different factors, below, and a key question is: how can we describe,
founders of the next generation
of cells or organisms.
many of which are still poorly understood. Among the predict and slow down resistance evolution?
factors that influence the rate and trajectory of resist-
Fixation ance evolution, we can identify the following: mutation Mutation supply rate. The generation of genetic het-
When there are at least supply rate; relative fitness of the drug-resistant mutant erogeneity in a homogenous infecting population is
two variants of a gene in a
as a function of drug concentration; strength of selective determined by mutation supply rate and population
population, fixation refers
to the situation when,
pressure; clonal interference; compensatory evolution; dynamics within the host with regard to the occur-
owing to selection or chance and the presence of epistatic interactions between resist- rence of population bottlenecks59. Mutation supply rate
fluctuations, only one allele ance genes or interactions between drugs. We discuss is in turn determined by population size and rates of
remains. these in more detail below. Additionally, there are epide- mutation and HGT.
miological factors, including host population structure Mutation and HGT rates have been measured in
and density, immunity status and transmission control, both bacteria and viruses in vitro 60,61. Substitution
that are beyond the scope of this Review. mutation rates span at least eight orders of magnitude
A useful graphic illustration of resistance evolution from 10−3 to 10−5 per nucleotide per genome replica-
is to consider a mutational space: that is, all types of tion across different types of RNA viruses62, from 10−6
mutations or HGT events that can generate resistance to 10−8 in DNA viruses62, and ≤10−10 per nucleotide per
genome replication in bacteria and fungi11,63. Similarly,
HGT rates (most available data are for bacterial con-
jugation) vary extensively depending on the type of
Susceptible
‘wild type’
Weak selection transfer mechanism, organism, transfer conditions and
methodology used to assess the rates64.
Bacterial, fungal, viral and parasitic infections can
be caused by a single, or very few, infectious particles
(for example, see REF. 65). This makes the probability of
drug resistance at the time of infection highly depend-
ent on the frequency of resistance in the relevant com-
Strong selection
munity or hospital environment. For many pathogens,
Mutant fitness
High-risk space
we have a poor knowledge of the transmission bottle-
neck population or of census population sizes within
infected hosts, but for some infections we know that the
total pathogen population can be so large that, with
the mutation rates described above, resistant mutants
are likely to arise during the infection. For example,
in respiratory and wound infections, the number of
bacteria typically exceeds 10 10 per gram of tissue66.
Low-risk space Virus population sizes are also very large. During an
untreated HIV infection, population sizes are in the
Resistance level order of 1010 (REF. 2) and, with mutation rates of 10−4 to
10−5 per nucleotide per genome replication, all poten-
Figure 3 | The relationship between fitness, degree of resistance and rate| Genetics
Nature Reviews of tial single, double and triple mutants could arise in the
formation of drug-resistant mutants. The relationship between relative fitness, population, implying that the mutation supply rate is
resistance and rate of formation is shown for a hypothetical set of all possible unlikely to be rate limiting for the emergence of resist-
drug-resistant mutant variants. Each circle represents one specific resistant mutant, and
ance after the infection is established. In human cancer,
the size of each circle represents its rate of formation. The probability of fixation of a
resistant variant is dependent on the interplay between these three variables: that is, the if a tumour is nourished with a blood supply, it can
rate of formation, level of drug selection and relative fitness153. The negative correlation grow to weigh between several grams and several kilo-
shown between rate of formation and resistance level is intentional: there are more grams, with approximately 108 cells per gram of tissue67.
mutational events that are capable of generating small decreases in drug susceptibility The total cell population size will ensure that there is
than there are events capable of causing high-level resistance. These high-frequency little or no limitation in the supply of potential drug-
events include gene-knockout mutations and genetic duplications13,153. The solid line resistance mutations within the tumour, and methods
boxes indicate mutant types that would be selected at weak selection pressures (low are now available to measure the absolute numbers and
drug concentrations, <minimal inhibitory concentration (MIC)) and strong selection types of mutations in developing tumours68.
pressures (high drug concentrations, >MIC). The dashed line boxes indicate mutational
spaces in which the risk of resistance development is either high or low. In particular, a
Fitness. The relative fitness of a drug-resistant pathogen
high risk of sustained drug resistance is provided by mutations that confer substantial
drug resistance accompanied by negligible or minor detrimental effects on fitness80,82,83. (in the absence or presence of the drug) is a key param-
It is important to note that there is no necessary correlation between level of resistance eter in determining success within the host and trans-
and relative fitness, as shown by a recent comprehensive analysis of rifampicin-resistance mission between hosts for bacteria19,69–71, viruses72–75
mutations78. The solid line boxes, as illustrated in the figure, can in practice overlap, so and parasites44. Thus, the rate of emergence and fixation
that a low-cost mutation can confer high-level resistance42,80. of resistant mutants at a given mutation supply rate is
464 | AUGUST 2015 | VOLUME 16 www.nature.com/reviews/genetics
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
influenced by mutant fitness (FIG. 3). In addition, the Clonal interference. Depending on the number of
steady-state frequency of resistance at a given selective potential mutants available, and their respective rates
pressure, and the rate of reversibility when the selec- of emergence, one may predict that many types of resist-
tive pressure is reduced, is generally determined by the ant mutants are often simultaneously present in a given
fitness costs of the resistance mechanism. population. This is especially true for viruses with high
The influence of pathogen fitness on evolutionary mutation rates for which the number of variants might be
success in clinical settings with regard to emergence very high at any given point during infection84,85, but also
and transmission has been demonstrated in different for bacteria, as several types of mutants can emerge and
studies. That is not to say that we know which par- be simultaneously present in the same population86–88. In
ticular fitness components are most relevant in clinical this situation, clonal interference (competition between
settings or during epidemics (and this probably differs asexual clones) influences the evolutionary trajectory
between pathogens), or which components influence (FIG. 4). Thus, when different beneficial (for example,
growth within the host and which affect transmission resistance) mutations arise independently in different
between hosts. There is a dearth of knowledge in this individuals, they compete against each other, typically
important area. However, laboratory assays of relative leading to the loss of most clones and the appearance of a
growth fitness (BOX 1) together with epidemiological ‘dominant clone’ (REFS 70,89). Large population sizes and
studies of genetic allele prevalence in clinical isolates high mutation rates increase the number of competing
suggest that fitness measures made in vitro can have resistance mutations, thereby increasing the potential for
clinical relevance. An illustrative example is given by clonal interference. Clonal interference has been dem-
the studies of fitness and resistance in M. tuberculosis. onstrated during the adaptation of antibiotic resistance
It was shown that for aminoglycoside-resistant bacte- plasmids to their bacterial hosts90, adaptation of bacte-
ria the fitter bacteria (as determined by growth rate ria to the fitness cost of resistance91, and adaptation to
in vitro) were also the most frequent types found in various selective pressures in RNA viruses92, bacteria93
patients41,42. The level of resistance influenced success and yeast 94,95.
such that the most common clinical mutants not only
had high fitness but also had a sufficiently high level of Compensatory evolution. Most mutations that occur in
resistance76. Similarly, in clinical isolates of M. tuber- any organism are deleterious. Their fate in the absence
culosis and Staphylococcus aureus, the spectrum of of selection may be extinction, persistence at low fre-
rifampicin-resistance mutations is biased in favour quency, reversion to the susceptible state or compen-
of low-cost mutations77,78. Similar observations have satory evolution whereby the costs are reduced or
been made for P. falciparum44, and for HIV79 for which eliminated, thus increasing the probability of mainte-
low fitness cost variants have spread on a global scale, nance. Which process dominates depends on the rela-
whereas more costly mutations have remained local or tive rates of reversion and compensation, the relative
waned over time. fitness of the reverted and compensated mutants, and
the population size (FIG. 4). Generally, the compensatory
Selective pressures. In natural and clinical settings, bac- mutation rate is considerably higher than the reversion
terial, viral and parasitic pathogens are exposed to a rate because the mutational target for compensation is
wide range of drug concentrations, generating a vari- larger than the reversion target. Thus, the compensatory
able range of selective pressures. When drug concen- mutation rate versus the reversion rate is usually in the
trations are high enough to prevent pathogen growth, range of 10–100:1 (REFS 96–100). The revertant mutant
resistant mutants need to pre-exist and the rate of is often the fittest variant (in the absence of drugs), but
enrichment is determined by the number of mutants there are examples in which the compensated mutant
in the population and their fitness. By contrast, dur- reaches the same fitness level as the revertant 96,101.
ing a non-lethal selection, mutants may emerge and Whether a revertant or compensatory mutation evolves
their rate of enrichment is determined by the fitness from a resistant population also depends on the popula-
difference between susceptible and resistant cells. As tion size such that the more frequently occurring com-
shown by recent studies in bacteria, the rate of emer- pensatory mutation will dominate in small populations,
gence and the type of mutants selected differ between whereas in large populations, with both revertants and
weak and strong selective pressures39,80–82. At low drug compensatory mutations present simultaneously, the
concentrations, mutant phenotypes usually result from fitter revertants dominate96,102. Experimental and clini-
many mutations of small effect, whereas lethal selec- cal studies show that the fitness cost of resistance can
Deleterious tions typically enrich pre-existing mutations of large be reduced by compensatory mutations and that com-
A mutation that reduces effect. Thus, mutants with low fitness cost are selec- pensated mutants can rapidly sweep a drug-resistant
relative fitness under a
tively enriched at low antibiotic concentrations, and the population of bacteria19,103, viruses104–106 and parasites44
particular condition.
smaller the fitness differential relative to the susceptible (see the mechanisms of fitness cost compensation
Sweep wild-type or other mutants the lower the selective drug section above).
A selective sweep is the concentration that is required for enrichment (FIG. 3).
reduction or elimination of Furthermore, the stepwise selection of successive Interactions between resistance mutations. Recent data
variation within a population as
a result of an increase in the
small-effect mutations enriches for mutator strains that from bacterial, viral and eukaryotic systems show that
proportion of one ‘successful’ have an increased probability of acquiring resistance by epistasis is pervasive and that it might have an impact
variant. mutation or HGT83. on resistance evolution107–109.
NATURE REVIEWS | GENETICS VOLUME 16 | AUGUST 2015 | 465
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
Epistatic interactions with regard to fitness (FIG. 5) of fitness landscapes suggest that mutations within a
are observed in bacteria, including Escherichia gene show strong epistatic interactions that constrain
coli 110–113, Salmonella enterica subsp. enterica serovar the type and order of selected mutations and make the
Typhimurium55,96 and Pseudomonas aeruginosa114. These evolutionary trajectory contingent on the first random
studies showed that combinations of fitness-reducing mutation115,116.
chromosomal resistance mutations and/or resist-
ance plasmids can generate either no epistasis, posi- Interactions between drugs. Another type of interaction
tive epistasis (a double mutant has a higher fitness involves the effect of resistance to one drug on the sus-
than expected from the sum of the costs of individual ceptibility to other drugs117. An early study by Szybalski
mutations) or negative epistasis (a double mutant has a and Bryson 118 and several subsequent studies 119–123
lower fitness than expected from the sum of the costs have shown that resistance to one drug class might either
of individual mutations), with positive epistasis being increase resistance to another drug or result in increased
especially pervasive. In some cases, reciprocal sign susceptibility (so‑called collateral sensitivity). In most
epistasis was observed in which the fitness of the dou- cases, the mechanisms for collateral sensitivity are poorly
ble mutant was higher than that of either of the single understood, but an exception is vancomycin-resistant
mutants. This implies that the acquisition of additional strains of methicillin-resistant S. aureus (MRSA) that are
resistance mutations or plasmids can increase the fit- susceptible to a combination of vancomycin and oxacil-
ness of a resistant strain and that reversal of resist- lin but resistant to each drug when given individually 122.
ance might not be achievable merely by reducing or This synergy occurs because the oxacillin-resistant
withdrawing drug use. penicillin-binding protein 2A (PBP2A) enzyme can-
Epistasis can also occur within a gene. Studies of evo- not process peptidoglycan precursors ending in
lution of β‑lactam resistance in vitro and quantification d‑Ala–d‑Lac (which are present owing to glycopeptide
Susceptible Resistant cells or Compensatory Clonal interference Epistatic interactions Dominant cells
cells or organisms evolution Competition between In a multidrug- or organisms
organisms Different resistance Fitness is restored several different clones resistant cell or
genotypes emerging at to different degrees organism interactions
different rates and with by compensatory between different
varying effects on fitness mutations types of resistance
genotypes
influence fitness
Fitness
Time
Figure 4 | Evolutionary trajectories of drug-resistance development. Nature
will gradually be lost from the population39,40 (the Reviews
ordering Genetics
of the| thick and
Evolutionary progression from a wild-type pathogen or cell type undergoing thin arrows is not important). Multiple different mutant variants will
drug treatment to a drug-resistant variant is shown, displaying the effects frequently arise in a population, and the enrichment of specific successful
of fitness costs of resistance, compensatory evolution, clonal interference variants will be determined by their relative fitness, the effects of clonal
and epistatic interactions on the trajectory of evolution, leading interference on competition between variants91,92,95 and the effects of
to a dominant clone (cell or organism). Each arrow represents a specific epistasis on the expression of mutant phenotypes107,109. The multiple parallel
resistant mutant, and the thickness of the arrow represents arrows indicate that the population of competing cells or organisms may
the relative rate of emergence. At the top of the figure are examples of the contain many genetic variants, with some being driven to extinction and
relevant cells or organisms that are present at each stage, with mutations newer variants arising, before one or a few dominant cells or organisms
shown as different coloured stars. From the left-hand side of the figure: finally approach fixation in the population70,89. In the final panel on the
resistant genetic variants generally have lower fitness than the susceptible right-hand side of the figure, the emerging dominant clones are those that
parent, and in the absence of drug selection or of compensatory evolution, provide sufficient resistance without substantially impairing fitness.
466 | AUGUST 2015 | VOLUME 16 www.nature.com/reviews/genetics
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
induction of the vanA operon), and therefore cell wall catastrophe’ whereby the virus is mutagenized to
biosynthesis is inhibited. death131,132. Lethal mutagenesis has been demonstrated in
Recent large-scale studies have systematically exam- experiments with the drug ribavirin for several viruses,
ined the extent of cross-resistance and collateral sen- including hepatitis C133, poliovirus134 and foot-and-
sitivity 124–127 and demonstrated that both are common mouth disease virus135, and has been widely discussed
phenomena. Applying these findings to drug-cycling as a more general approach to treat viral infections such
experiments shows that, under in vitro conditions, an as HIV136,137. A concern is the extent to which resist-
alternating drug-cycling protocol may slow the rate of ance can develop to mutagenic drugs138–140. However,
resistance development124,125. Such interactions are also rel- these resistance mutations may also be associated with
evant to drug combinations because using synergistic drug reduced fitness and virulence141 and susceptibility to
combinations below the minimal inhibitory concentration another mutagen, implying that cycling of mutagenic
(MIC) could result in faster resistance development compounds might be a feasible approach to achieve virus
than antagonistic drug combinations128,129. These find- extinction142.
ings imply that antagonistic drug combinations (which Combinations of different classes of drugs have been
are usually avoided in clinical settings) might be better widely used in clinical settings, in particular for HIV,
than synergistic combinations in slowing resistance tuberculosis (TB), malaria and cancer, for which com-
development. Whether collateral sensitivity and antago- binations are standard therapy to increase efficacy and
nistic interactions can be applied to clinical situations to reduce resistance development 24,143–145, and they also
to reduce the rate of resistance evolution remains to be show promise in potentially creating fitness trade-offs
determined. that might limit resistance development when used in
antifungal therapy 146. An extension of drug combination
Therapeutic implications use is the search for collateral sensitivity networks in
Treatment. In principle, detailed knowledge of fitness
costs and interactions between resistance mutations
and between drugs could be applicable to clinical set-
tings to reduce resistance development. For example, 1.0
single drugs or drug combinations could be rationally
designed such that the drug itself or the resulting resist-
ance mechanism confers a reduction in pathogen fitness 0.8
or virulence. Alternatively, identification of epistatic
interactions between resistance mutations could allow 0.6
Relative fitness
the combined use of the corresponding drugs to reduce
resistance emergence.
Resistance will almost always develop to any drug 0.48
used in clinical settings, but there are exceptions in
which resistance is absent or slow to appear. For exam-
ple, in Streptococcus pyogenes, no cases of penicillin
resistance are known despite penicillin being the stand-
ard treatment of S. pyogenes infections for more than
60 years, and, in fungi, resistance to the polyene drug
amphotericin B has remained very low even after dec-
pe
ve
ive
ive
sig eci sis
is
ist al
nt
nt
as
iti
ty
ades of widespread use43. A similar example of a lack of
ep c
a
t
sit
n pro
a
ist
ga
d
ild
ut
ut
Po
Ad
ep
Ne
M
resistance development, but with a much shorter clinical
W
gn
R
Si
use, is the HIV integrase inhibitor dolutegravir (DTG),
which was recently introduced as a part of first-line HIV Epistasis
therapy. In these cases, it is likely that the lack of resist-
Single mutants Double mutants
ance development is due to high fitness costs (reduced
replication capacity and growth rates, or hypersensitivity Figure 5 | Epistasis and relativeNature
fitness. The relative
Reviews | Genetics
to the host immune system43) associated with resistance fitness of two drug-resistant mutants (mutant 1 with
and the absence of efficient compensatory mutations. a fitness of 0.8 and mutant 2 with a fitness of 0.6) is used to
Thus, DTG-resistant mutants with point mutations in illustrate different possible types of epistatic interaction
HIV integrase were dramatically impaired in replication between mutations. With no epistasis (additive effect), the
and the ability to acquire resistance against RTIs79,130. fitness of the double mutant is predictable from the fitness
These examples suggest that certain types of drug targets values of the individual single mutants (0.8 × 0.6 = 0.48).
Minimal inhibitory Epistasis is illustrated for the double mutant as negative
concentration or drugs are less prone to resistance development and
(the double mutant has a lower fitness than that predicted
(MIC). The lowest that this is strongly associated with a high fitness cost of
by an additive effect), positive (the double mutant has a
concentration of an resistance (see below). higher fitness than that predicted by an additive effect but
antimicrobial drug that, An interesting concept regarding the treatment
under a set of agreed a lower fitness than the single mutants), sign epistasis (the
conditions, inhibits the visible
of RNA viruses with intrinsically high mutation rates double mutant has a higher fitness than one of the single
growth of a microorganism is to increase the mutation rate beyond the level that is mutants) and reciprocal sign epistasis (the double mutant
after overnight incubation. compatible with virus survival by inducing an ‘error has a higher fitness than each of the single mutants).
NATURE REVIEWS | GENETICS VOLUME 16 | AUGUST 2015 | 467
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
which resistance to one drug confers increased suscepti- It was also thought that resistance development
bility to a second drug 123–126,147. In such a case, two drugs would be severely reduced if a drug acted on multiple
could be alternated to select against resistance to either targets149. However, experience with fluoroquinolones,
drug. Experimental data suggest that this approach can an antibiotic class that acts on two different essential
slow the rate of resistance development 124,125, but further and conserved bacterial targets (DNA gyrase and DNA
work is needed to determine whether it can impede topoisomerase IV) is not encouraging in this respect.
resistance evolution in patients. It should be noted that Resistance to fluoroquinolones developed easily and
this discussion about drug combinations is applicable to became clinically established, probably because the
mutationally acquired resistance but not necessarily relative activity of the drugs is not perfectly balanced
to horizontally transferred resistance, which is the most between the two targets, allowing resistance to develop
common mode of acquiring clinically relevant antibiotic first in one target and then in the other.
resistance in bacteria. Thus, using drug combinations An alternative strategy to developing one drug that
for bacteria for which the corresponding resistance is hits multiple targets is to develop and use multiple drugs
typically carried on a mobile element could speed up to hit multiple targets. This is routine practice in HIV10,
resistance development compared with monotherapy, TB18 and cancer therapy 29. This is an area of research that
adding to the complexity of the cost–benefit analysis of is now receiving increased interest for the development of
drug combination use. effective antibacterial and antifungal therapies146, using
available drugs in combination, or drug–potentiator
Drug design. Can we use our knowledge of the rates combinations, and which will probably strongly
and fitness costs of resistance development to design influence many future drug discovery and development
drugs with a low propensity for resistance development? programmes against pathogens.
A priori there are several predictions that could be made
regarding the characteristics of a low-propensity resist- Concluding remarks
ance mechanism: the rate of mutation or HGT should As discussed in this Review, resistance development
be low; fitness costs associated with resistance should be to toxic drugs in viruses, bacteria, fungi, parasites and
high; and the rate and efficiency of compensatory cancers shows both important similarities and differ-
evolution should be low. ences that allow us to make certain generalizations, but
Which resistance mutation or mechanisms would that also emphasize the need to sometimes describe and
be associated with high fitness costs? Drug targets with analyse resistance evolution in a manner that is specific
complex downstream effects — for example, RNA poly- to particular pathogens or resistance mechanisms. With
merase, the target of rifampins — are attractive because regard to similarities, it is striking that the mechanisms of
resistance mutations typically have pleiotropic effects resistance are often genetically and functionally similar
on pathogen physiology and reduce bacterial fitness. between these different organisms and cells. For exam-
However, evidence from both in vitro measurements and ple, resistance by mutational target alteration occurs in
clinical prevalence shows that compensatory second-site all systems, and upregulation of drug efflux systems is
mutations in RNA polymerase occur with a high fre- widespread, except in viruses. Furthermore, with regard
quency and restore function sufficiently so that resist- to the dynamics of resistance evolution, the effect of fac-
ance is widespread and established98,148. Accordingly, tors such as mutation supply rates and fitness effects of
fitness costs of resistance alone are not a good predictor the resistance mechanisms are very similar between
of subsequent clinical resistance development. these systems. Likewise, epistatic interactions between
A low rate of penetrance (the probability of a muta- resistance mechanisms and interactions between drugs
tion being expressed as a drug-resistance phenotype) seem to be shared and pervasive phenomena.
is expected if the target molecule is encoded by several However, there are also important differences, and
genes (for example, drugs that target ribosomal RNA one major difference concerns the extent of constraints
encoded by several rRNA operons in bacteria and where on resistance mechanisms with regard to their effects on
susceptibility is dominant). In bacteria, resistance to organism fitness and transmission. Cancer cells and
this type of targeting can be mediated by HGT of genes associated resistance mechanisms can be considered the
encoding enzymes that modify all of the rRNAs or that least constrained, as there is no selection for cancer cells
reduce the activity of the drug itself, but this type of tar- to transmit between different hosts, and evolution can
get could still be potentially useful in fungi and other be short-sighted and local. By contrast, the long-term
eukaryotic pathogens for which HGT is not a substantial evolutionary success of viruses, bacteria and parasites
issue. HGT events are hard to predict but depend on depends not only on survival and growth within the
the following four factors: first, the presence of a resist- infected host but also on the ability to transmit to new
Pleiotropic
ance gene in the total resistome; second, the ecological hosts. Furthermore, many bacteria and parasites spend
When one gene influences
multiple phenotypic traits. opportunity for HGT (frequency of pathogen–donor time outside the host in the natural environment, where
interaction); third, the efficiency of transfer versus they need to respond to different problems and selec-
Resistome genetic barriers (restriction systems or clustered regu- tion pressures, creating adaptive conflicts that must be
The collection of all of the larly interspaced short palindromic repeat (CRISPR) resolved. Another important difference between bacteria
antibiotic resistance genes
and their precursors in
systems); and fourth, the fitness effects of the resistance versus viruses, fungi, parasites and cancers is that the
both pathogenic and mechanism on the recipient. Currently, we have only a major resistance mechanisms in bacteria involve HGT
non-pathogenic bacteria. very limited knowledge of these factors. that has different characteristics and dynamics from
468 | AUGUST 2015 | VOLUME 16 www.nature.com/reviews/genetics
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
those of mutational mechanisms. HGT events are cur- natural products, to increase the probability of discov-
rently less predictable at the population level. Moreover, ering novel drugs. It is important that as far as possible
in contrast to mutational mechanisms, resistance to mul- all new drugs and targets should combine a propensity
tiple classes of drugs can be acquired in a single genetic for a low frequency of resistance selection, high fitness
event, suggesting that resistance evolution in bacteria costs associated with resistance and low probability of
may proceed in great leaps compared with more gradual fitness compensation. One of the major academic chal-
changes in other organisms. lenges that we face is to deepen our understanding of the
Looking to the future, what are the major challenges, resistome and the dynamics of HGT that constitute one
where do we next go to solve them, and are there lessons of the major causes of antibacterial drug resistance. A
to be learned from one system that can inform studies second academic challenge is to better understand drug
in any other system? The major practical challenge that structures and how their chemical properties relate to
we face is to discover, develop and bring into clinical combining efficacy with a low level of toxic liabilities
practice a new generation of drugs to regenerate effec- against the patient. The single most important lesson
tive therapy for each of these biological systems, and to from comparing different biological systems is that the
ensure that a continuous pipeline of drug discovery and use of drugs in combination should become standard
development is maintained. This will involve learning practice to help to minimize resistance development in
how to access new areas of chemical space, including all systems in which we use drug therapy.
1. World Health Organization. World Health Statistics 18. Dye, C. Doomsday postponed? Preventing and 35. Easwaran, H., Tsai, H. C. & Baylin, S. B.
2014 (WHO Press, 2014). reversing epidemics of drug-resistant tuberculosis. Cancer epigenetics: tumor heterogeneity, plasticity of
2. Abram, M. E., Ferris, A. L., Shao, W., Alvord, W. G. & Nat. Rev. Microbiol. 7, 81–87 (2009). stem-like states, and drug resistance. Mol. Cell 54,
Hughes, S. H. Nature, position, and frequency of 19. Andersson, D. I. & Hughes, D. Antibiotic resistance 716–727 (2014).
mutations made in a single cycle of HIV‑1 replication. and its cost: is it possible to reverse resistance? Nat. 36. Boutwell, C. L., Rowley, C. F. & Essex, M. Reduced viral
J. Virol. 84, 9864–9878 (2010). Rev. Microbiol. 8, 260–271 (2010). replication capacity of human immunodeficiency virus
3. Mansky, L. M. & Temin, H. M. Lower in vivo 20. Hoiby, N. et al. The clinical impact of bacterial type 1 subtype C caused by cytotoxic-T‑lymphocyte
mutation rate of human immunodeficiency virus biofilms. Int. J. Oral Sci. 3, 55–65 (2011). escape mutations in HLA‑B57 epitopes of capsid
type 1 than that predicted from the fidelity of 21. Mackinnon, M. J. & Read, A. F. Virulence in malaria: protein. J. Virol. 83, 2460–2468 (2009).
purified reverse transcriptase. J. Virol. 69, an evolutionary viewpoint. Phil. Trans. R. Soc. Lond. B 37. Armstrong, K. L., Lee, T. H. & Essex, M. Replicative
5087–5094 (1995). 359, 965–986 (2004). fitness costs of nonnucleoside reverse transcriptase
4. Chan, J. M., Carlsson, G. & Rabadan, R. Topology of 22. Muller, I. B. & Hyde, J. E. Antimalarial drugs: modes of inhibitor drug resistance mutations on HIV subtype C.
viral evolution. Proc. Natl Acad. Sci. USA 110, action and mechanisms of parasite resistance. Future Antimicrob. Agents Chemother. 55, 2146–2153 (2011).
18566–18571 (2013). Microbiol. 5, 1857–1873 (2010). 38. Cong, M. E., Heneine, W. & García-Lerma, J. G.
5. Sprenger, H. G., Bierman, W. F., van der Werf, T. S., 23. Shandilya, A., Chacko, S., Jayaram, B. & Ghosh, I. The fitness cost of mutations associated with human
Gisolf, E. H. & Richter, C. A systematic review of a A plausible mechanism for the antimalarial activity of immunodeficiency virus type 1 drug resistance is
single-class maintenance strategy with nucleoside/ artemisinin: a computational approach. Sci. Rep. 3, modulated by mutational interactions. J. Virol. 81,
nucleotide reverse transcriptase inhibitors in HIV/ 2513 (2013). 3037–3041 (2007).
AIDS. Antivir Ther. 19, 625–636 (2014). 24. Visser, B. J., van Vugt, M. & Grobusch, M. P. 39. Andersson, D. I. & Hughes, D. Persistence of antibiotic
6. Sharma, M. & Saravolatz, L. D. Rilpivirine: a new non- Malaria: an update on current chemotherapy. resistance in bacterial populations. FEMS Microbiol.
nucleoside reverse transcriptase inhibitor. Expert Opin. Pharmacother. 15, 2219–2254 Rev. 35, 901–911 (2011).
J. Antimicrob. Chemother. 68, 250–256 (2013). (2014). 40. Vogwill, T. & MacLean, R. C. The genetic basis of the
7. De Clercq, E. The nucleoside reverse transcriptase 25. Dondorp, A. M. et al. The threat of artemisinin- fitness costs of antimicrobial resistance: a meta-
inhibitors, nonnucleoside reverse transcriptase resistant malaria. N. Engl. J. Med. 365, 1073–1075 analysis approach. Evol. Appl. 8, 284–295 (2015).
inhibitors, and protease inhibitors in the treatment of (2011). 41. Sander, P. et al. Fitness cost of chromosomal drug
HIV infections (AIDS). Adv. Pharmacol. 67, 317–358 26. Noedl, H. et al. Evidence of artemisinin-resistant resistance-conferring mutations. Antimicrob. Agents
(2013). malaria in western Cambodia. N. Engl. J. Med. 359, Chemother. 46, 1204–1211 (2002).
8. Michaud, V. et al. The dual role of pharmacogenetics 2619–2620 (2008). 42. Bottger, E. C., Springer, B., Pletschette, M. &
in HIV treatment: mutations and polymorphisms First report of the worrying emergence of Sander, P. Fitness of antibiotic-resistant
regulating antiretroviral drug resistance and resistance to the most effective antimalarial drug microorganisms and compensatory mutations.
disposition. Pharmacol. Rev. 64, 803–833 (2012). therapy. Nat. Med. 4, 1343–1344 (1998).
9. Ridky, T. & Leis, J. Development of drug resistance 27. Takala-Harrison, S. et al. Genetic loci associated Provided the first clear evidence for the selection
to HIV‑1 protease inhibitors. J. Biol. Chem. 270, with delayed clearance of Plasmodium falciparum of low-cost antibiotic resistance mutations in a
29621–29623 (1995). following artemisinin treatment in Southeast Asia. clinical environment.
10. Thompson, M. A. et al. Antiretroviral treatment of Proc. Natl Acad. Sci. USA 110, 240–245 (2013). 43. Vincent, B. M., Lancaster, A. K., Scherz-Shouval, R.,
adult HIV infection: 2012 recommendations of the 28. Ariey, F. et al. A molecular marker of artemisinin- Whitesell, L. & Lindquist, S. Fitness trade-offs restrict
International Antiviral Society-USA panel. JAMA 308, resistant Plasmodium falciparum malaria. Nature the evolution of resistance to amphotericin B. PLoS
387–402 (2012). 505, 50–55 (2014). Biol. 11, e1001692 (2013).
11. Drake, J. W., Charlesworth, B., Charlesworth, D. & Identification of mutations in the K13 propellor as Experimental work showing how conflicting
Crow, J. F. Rates of spontaneous mutation. Genetics important determinants of artemisinin resistance selective pressures shape evolutionary trajectories
148, 1667–1686 (1998). and a molecular marker for surveillance. and suggesting a strategy for limiting the rapid
12. Komp Lindgren, P., Karlsson, Å. & Hughes, D. 29. Holohan, C., Van Schaeybroeck, S., Longley, D. B. & emergence of drug resistance.
Mutation rate and evolution of fluoroquinolone Johnston, P. G. Cancer drug resistance: an evolving 44. Rosenthal, P. J. The interplay between drug resistance
resistance in Escherichia coli isolates from patients paradigm. Nat. Rev. Cancer 13, 714–726 (2013). and fitness in malaria parasites. Mol. Microbiol. 89,
with urinary tract infections. Antimicrob. Agents 30. Duesberg, P., Stindl, R. & Hehlmann, R. Explaining the 1025–1038 (2013).
Chemother. 47, 3222–3232 (2003). high mutation rates of cancer cells to drug and 45. Gatenby, R. A. A change of strategy in the war on
13. Andersson, D. I. & Hughes, D. Gene amplification and multidrug resistance by chromosome reassortments cancer. Nature 459, 508–509 (2009).
adaptive evolution in bacteria. Annu. Rev. Genet. 43, that are catalyzed by aneuploidy. Proc. Natl Acad. Sci. 46. Schock, H. B., Garsky, V. M. & Kuo, L. C. Mutational
167–195 (2009). USA 97, 14295–14300 (2000). anatomy of an HIV‑1 protease variant conferring cross-
14. Sun, S., Berg, O. G., Roth, J. R. & Andersson, D. I. 31. Swanton, C. et al. Chromosomal instability determines resistance to protease inhibitors in clinical trials.
Contribution of gene amplification to evolution of taxane response. Proc. Natl Acad. Sci. USA 106, Compensatory modulations of binding and activity.
increased antibiotic resistance in Salmonella 8671–8676 (2009). J. Biol. Chem. 271, 31957–31963 (1996).
typhimurium. Genetics 182, 1183–1195 (2009). 32. Housman, G. et al. Drug resistance in cancer: an 47. Zhang, Y. M. et al. Drug resistance during indinavir
15. Anderson, J. B. Evolution of antifungal-drug overview. Cancers (Basel) 6, 1769–1792 (2014). therapy is caused by mutations in the protease gene
resistance: mechanisms and pathogen fitness. Nat. 33. McMillin, D. W., Negri, J. M. & Mitsiades, C. S. and in its Gag substrate cleavage sites. J. Virol. 71,
Rev. Microbiol. 3, 547–556 (2005). The role of tumour-stromal interactions in modifying 6662–6670 (1997).
16. Wright, G. D. The antibiotic resistome: the nexus of drug response: challenges and opportunities. Nat. 48. Bleiber, G., Munoz, M., Ciuffi, A., Meylan, P. &
chemical and genetic diversity. Nat. Rev. Microbiol. 5, Rev. Drug Discov. 12, 217–228 (2013). Telenti, A. Individual contributions of mutant protease
175–186 (2007). 34. Timp, W. & Feinberg, A. P. Cancer as a dysregulated and reverse transcriptase to viral infectivity,
17. Davies, J. & Davies, D. Origins and evolution of epigenome allowing cellular growth advantage at the replication, and protein maturation of antiretroviral
antibiotic resistance. Microbiol. Mol. Biol. Rev. 74, expense of the host. Nat. Rev. Cancer 13, 497–510 drug-resistant human immunodeficiency virus type 1.
417–433 (2010). (2013). J. Virol. 75, 3291–3300 (2001).
NATURE REVIEWS | GENETICS VOLUME 16 | AUGUST 2015 | 469
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
49. Kožišek, M. et al. Mutations in HIV‑1 gag and pol 74. Bastarache, S. M., Mesplede, T., Donahue, D. A., 93. Arjan, J. A. et al. Diminishing returns from mutation
compensate for the loss of viral fitness caused by a Sloan, R. D. & Wainberg, M. A. Fitness impaired supply rate in asexual populations. Science 283,
highly mutated protease. Antimicrob. Agents drug resistant HIV‑1 is not compromised in 404–406 (1999).
Chemother. 56, 4320–4330 (2012). cell‑to‑cell transmission or establishment of and Showed that the rate of evolutionary adaptation is
50. Koval, C. E., Dykes, C., Wang, J. & Demeter, L. M. reactivation from latency. Viruses 6, 3487–3499 proportional to mutation supply rate only in
Relative replication fitness of efavirenz-resistant (2014). particular circumstances of small or well-adapted
mutants of HIV‑1: correlation with frequency during 75. Butler, J. et al. Estimating the fitness advantage populations.
clinical therapy and evidence of compensation for the conferred by permissive neuraminidase mutations in 94. Kao, K. C. & Sherlock, G. Molecular characterization
reduced fitness of K103N + L100I by the nucleoside recent oseltamivir-resistant A(H1N1)pdm09 influenza of clonal interference during adaptive evolution in
resistance mutation L74V. Virology 353, 184–192 viruses. PLoS Pathog. 10, e1004065 (2014). asexual populations of Saccharomyces cerevisiae.
(2006). 76. Shcherbakov, D. et al. Directed mutagenesis of Nat. Genet. 40, 1499–1504 (2008).
51. Demeter, L. M. et al. Association of efavirenz Mycobacterium smegmatis 16S rRNA to reconstruct 95. Lang, G. I. et al. Pervasive genetic hitchhiking and
hypersusceptibility with virologic response in ACTG the in vivo evolution of aminoglycoside resistance in clonal interference in forty evolving yeast populations.
368, a randomized trial of abacavir (ABC) in Mycobacterium tuberculosis. Mol. Microbiol. 77, Nature 500, 571–574 (2013).
combination with efavirenz (EFV) and indinavir (IDV) in 830–840 (2010). A detailed analysis of the dynamics of evolutionary
HIV-infected subjects with prior nucleoside analog Reconstructed the resistance genotypes of clinical adaptation evaluating how this determines which
experience. HIV Clin. Trials 9, 11–25 (2008). strains in an isogenic background, revealing a mutations fix in a population and the
52. Schulz zur Wiesch, P., Engelstädter, J. & Bonhoeffer, S. pathway for resistance development that suggests reproducibility of evolution.
Compensation of fitness costs and reversibility of that compensatory evolution contributes to 96. Maisnier-Patin, S., Berg, O. G., Liljas, L. &
antibiotic resistance mutations. Antimicrob. Agents drug-resistant TB. Andersson, D. I. Compensatory adaptation to
Chemother. 54, 2085–2095 (2010). 77. O’Neill, A. J., Huovinen, T., Fishwick, C. W. & Chopra, I. the deleterious effect of antibiotic resistance
53. Soskine, M. & Tawfik, D. S. Mutational effects and the Molecular genetic and structural modeling studies of in Salmonella typhimurium. Mol. Microbiol. 46,
evolution of new protein functions. Nat. Rev. Genet. Staphylococcus aureus RNA polymerase and the 355–366 (2002).
11, 572–582 (2010). fitness of rifampin resistance genotypes in relation to 97. Brandis, G., Wrande, M., Liljas, L. & Hughes, D.
54. Schrag, S. J., Perrot, V. & Levin, B. R. Adaptation to clinical prevalence. Antimicrob. Agents Chemother. 50, Fitness-compensatory mutations in rifampicin-
the fitness costs of antibiotic resistance in Escherichia 298–309 (2006). resistant RNA polymerase. Mol. Microbiol. 85,
coli. Proc. Biol. Sci. 264, 1287–1291 (1997). 78. Brandis, G., Pietsch, F., Alemayehu, R. & Hughes, D. 142–151 (2012).
55. Bjorkman, J., Samuelsson, P., Andersson, D. I. & Comprehensive phenotypic characterization of 98. Brandis, G. & Hughes, D. Genetic characterization of
Hughes, D. Novel ribosomal mutations affecting rifampicin resistance mutations in Salmonella provides compensatory evolution in strains carrying rpoB
translational accuracy, antibiotic resistance and insight into the evolution of resistance in Ser531Leu, the rifampicin resistance mutation most
virulence of Salmonella typhimurium. Mol. Microbiol. Mycobacterium tuberculosis. J. Antimicrob. frequently found in clinical isolates. J. Antimicrob.
31, 53–58 (1999). Chemother. 70, 680–685 (2015). Chemother. 68, 2493–2497 (2013).
56. Kumpornsin, K. et al. Origin of robustness in 79. Mesplede, T. et al. Viral fitness cost prevents HIV‑1 99. Nagaev, I., Bjorkman, J., Andersson, D. I. &
generating drug-resistant malaria parasites. Mol. Biol. from evading dolutegravir drug pressure. Hughes, D. Biological cost and compensatory
Evol. 31, 1649–1660 (2014). Retrovirology 10, 22 (2013). evolution in fusidic acid-resistant Staphylococcus
57. McFarland, C. D., Mirny, L. A. & Korolev, K. S. 80. Gullberg, E. et al. Selection of resistant bacteria at aureus. Mol. Microbiol. 40, 433–439 (2001).
Tug‑of‑war between driver and passenger mutations in very low antibiotic concentrations. PLoS Pathog. 7, 100. Reynolds, M. G. Compensatory evolution in
cancer and other adaptive processes. Proc. Natl Acad. e1002158 (2011). rifampin-resistant Escherichia coli. Genetics 156,
Sci. USA 111, 15138–15143 (2014). Provided experimental evidence that sub-MIC 1471–1481 (2000).
58. Takebe, N. et al. Targeting Notch, Hedgehog, and Wnt levels of antibiotics select and enrich for resistant 101. Bjorkman, J., Hughes, D. & Andersson, D. I.
pathways in cancer stem cells: clinical update. Nat. mutants. Virulence of antibiotic-resistant Salmonella
Rev. Clin. Oncol. http://dx.doi.org/10.1038/ 81. Hughes, D. & Andersson, D. I. Selection of resistance typhimurium. Proc. Natl Acad. Sci. USA 95,
nrclinonc.2015.61 (2015). at lethal and non-lethal antibiotic concentrations. 3949–3953 (1998).
59. Worby, C. J., Lipsitch, M. & Hanage, W. P. Within-host Curr. Opin. Microbiol. 15, 555–560 (2012). 102. Levin, B. R., Perrot, V. & Walker, N. Compensatory
bacterial diversity hinders accurate reconstruction of 82. Gullberg, E., Albrecht, L. M., Karlsson, C., mutations, antibiotic resistance and the population
transmission networks from genomic distance data. Sandegren, L. & Andersson, D. I. Selection of a genetics of adaptive evolution in bacteria. Genetics
PLoS Comput. Biol. 10, e1003549 (2014). multidrug resistance plasmid by sublethal levels 154, 985–997 (2000).
60. Lynch, M. Evolution of the mutation rate. Trends of antibiotics and heavy metals. mBio 5, 103. Casali, N. et al. Evolution and transmission of
Genet. 26, 345–352 (2010). e01918-14 (2014). drug-resistant tuberculosis in a Russian population.
61. Foster, P. L. Methods for determining spontaneous 83. Andersson, D. I. & Hughes, D. Microbiological effects Nat. Genet. 46, 279–286 (2014).
mutation rates. Methods Enzymol. 409, 195–213 of sublethal levels of antibiotics. Nat. Rev. Microbiol. 104. Pingen, M., Nijhuis, M., de Bruijn, J. A., Boucher, C. A.
(2006). 12, 465–478 (2014). & Wensing, A. M. Evolutionary pathways of
62. Duffy, S., Shackelton, L. A. & Holmes, E. C. 84. Menéndez-Arias, L., Martinez, M. A., Quñones- transmitted drug-resistant HIV‑1. J. Antimicrob.
Rates of evolutionary change in viruses: patterns and Mateu, M. E. & Martinez-Picado, J. Fitness variations Chemother. 66, 1467–1480 (2011).
determinants. Nat. Rev. Genet. 9, 267–276 (2008). and their impact on the evolution of antiretroviral 105. Martinez-Picado, J. & Martínez, M. A. HIV‑1 reverse
63. Abdulkarim, F. & Hughes, D. Homologous drug resistance. Curr. Drug Targets Infect. Disord. 3, transcriptase inhibitor resistance mutations and
recombination between the tuf genes of Salmonella 355–371 (2003). fitness: a view from the clinic and ex vivo. Virus Res.
typhimurium. J. Mol. Biol. 260, 506–522 (1996). 85. Nijhuis, M., van Maarseveen, N. M. & Boucher, C. A. 134, 104–123 (2008).
64. Cabezón, E., Ripoll-Rozada, J., Peña, A., de la Cruz, F. Antiviral resistance and impact on viral replication 106. Wang, Y. et al. Co‑evolution of compensatory mutation
& Arechaga, I. Towards an integrated model of capacity: evolution of viruses under antiviral pressure K43E with mutation M41L in long-term HIV
bacterial conjugation. FEMS Microbiol. Rev. 39, occurs in three phases. Handb. Exp. Pharmacol. 189, antiretroviral treatment. Curr. HIV Res. 12, 22–31
81–95 (2014). 299–320 (2009). (2014).
65. Shaw, G. M. & Hunter, E. HIV transmission. 86. Mariam, S. H., Werngren, J., Aronsson, J., Hoffner, S. 107. de Visser, J. A. & Krug, J. Empirical fitness landscapes
Cold Spring Harb. Perspect. Med. 2, a006965 (2012). & Andersson, D. I. Dynamics of antibiotic resistant and the predictability of evolution. Nat. Rev. Genet.
66. Smith, M. R. & Wood, W. B. Jr. An experimental Mycobacterium tuberculosis during long-term 15, 480–490 (2014).
analysis of the curative action of penicillin in acute infection and antibiotic treatment. PLoS ONE 6, 108. Bedhomme, S., Hillung, J. & Elena, S. F.
bacterial infections. III. The effect of suppuration upon e21147 (2011). Emerging viruses: why they are not jack of all trades?
the antibacterial action of the drug. J. Exp. Med. 103, 87. Suerbaum, S. & Josenhans, C. Helicobacter pylori Curr. Opin. Virol. 10, 1–6 (2015).
509–522 (1956). evolution and phenotypic diversification in a 109. Kondrashov, D. A. & Kondrashov, F. A.
67. Del Monte, U. Does the cell number 109 still really fit changing host. Nat. Rev. Microbiol. 5, 441–452 Topological features of rugged fitness landscapes in
one gram of tumor tissue? Cell Cycle 8, 505–506 (2007). sequence space. Trends Genet. 31, 24–33 (2015).
(2009). 88. Markussen, T. et al. Environmental heterogeneity 110. Komp Lindgren, P., Marcusson, L. L., Sandvang, D.,
68. Carter, S. L. et al. Absolute quantification of somatic drives within-host diversification and evolution of Frimodt-Moller, N. & Hughes, D. Biological cost
DNA alterations in human cancer. Nat. Biotechnol. Pseudomonas aeruginosa. mBio 5, e01592-14 of single and multiple norfloxacin resistance
30, 413–421 (2012). (2014). mutations in Escherichia coli implicated in urinary
69. Andersson, D. I. & Levin, B. R. The biological cost 89. Gerrish, P. J. & Lenski, R. E. The fate of competing tract infections. Antimicrob. Agents Chemother. 49,
of antibiotic resistance. Curr. Opin. Microbiol. 2, beneficial mutations in an asexual population. 2343–2351 (2005).
489–493 (1999). Genetica 102–103, 127–144 (1998). 111. Marcusson, L. L., Frimodt-Moller, N. & Hughes, D.
70. Wiser, M. J., Ribeck, N. & Lenski, R. E. 90. Hughes, J. M. et al. The role of clonal interference in Interplay in the selection of fluoroquinolone resistance
Long-term dynamics of adaptation in asexual the evolutionary dynamics of plasmid–host and bacterial fitness. PLoS Pathog. 5, e1000541
populations. Science 342, 1364–1367 (2013). adaptation. mBio 3, e00077-12 (2012). (2009).
71. Lipsitch, M., Bergstrom, C. T. & Levin, B. R. 91. Gifford, D. R. & MacLean, R. C. Evolutionary reversals Illustrated how fitness costs incurred during
The epidemiology of antibiotic resistance in hospitals: of antibiotic resistance in experimental populations of resistance evolution can act as a driver for further
paradoxes and prescriptions. Proc. Natl Acad. Sci. Pseudomonas aeruginosa. Evolution 67, 2973–2981 resistance evolution.
USA 97, 1938–1943 (2000). (2013). 112. Trindade, S. et al. Positive epistasis drives the
72. Iyidogan, P. & Anderson, K. S. Current perspectives 92. Miralles, R., Gerrish, P. J., Moya, A. & Elena, S. F. acquisition of multidrug resistance. PLoS Genet. 5,
on HIV‑1 antiretroviral drug resistance. Viruses 6, Clonal interference and the evolution of RNA viruses. e1000578 (2009).
4095–4139 (2014). Science 285, 1745–1747 (1999). Examined epistasis between antibiotic resistance
73. Gotte, M. The distinct contributions of fitness and Measured the effects of clonal interference in an mutations that led to insights that suggested
genetic barrier to the development of antiviral drug asexual RNA virus and quantified the rates and reasons why multidrug-resistant bacteria are so
resistance. Curr. Opin. Virol. 2, 644–650 (2012). effects of beneficial mutations. prevalent.
470 | AUGUST 2015 | VOLUME 16 www.nature.com/reviews/genetics
© 2015 Macmillan Publishers Limited. All rights reserved
REVIEWS
113. Angst, D. C. & Hall, A. R. The cost of antibiotic 130. Oliveira, M., Mesplede, T., Quashie, P. K., Moisi, D. & 151. Woodman, Z. & Williamson, C. HIV molecular
resistance depends on evolutionary history in Wainberg, M. A. Resistance mutations against epidemiology: transmission and adaptation to human
Escherichia coli. BMC Evol. Biol. 13, 163 (2013). dolutegravir in HIV integrase impair the emergence of populations. Curr. Opin. HIV AIDS 4, 247–252 (2009).
114. Hall, A. R. & MacLean, R. C. Epistasis buffers the resistance against reverse transcriptase inhibitors. 152. Anastassopoulou, C. G. et al. Escape of HIV‑1 from a
fitness effects of rifampicin- resistance mutations in AIDS 28, 813–819 (2014). small molecule CCR5 inhibitor is not associated with a
Pseudomonas aeruginosa. Evolution 65, 2370–2379 131. Anderson, J. P., Daifuku, R. & Loeb, L. A. Viral error fitness loss. PLoS Pathog. 3, e79 (2007).
(2011). catastrophe by mutagenic nucleosides. Annu. Rev. 153. Andersson, D. I., Hughes, D. & Roth, J. R.
115. Salverda, M. L. et al. Initial mutations direct Microbiol. 58, 183–205 (2004). EcoSal-Escherichia coli and Salmonella: Cellular and
alternative pathways of protein evolution. PLoS Genet. 132. Clementi, M. Perspectives and opportunities for novel Molecular Biology (ASM, 2011).
7, e1001321 (2011). antiviral treatments targeting virus fitness. Clin. 154. Burch, C. L. & Chao, L. Evolvability of an RNA virus is
116. Weinreich, D. M., Delaney, N. F., Depristo, M. A. & Microbiol. Infect. 14, 629–631 (2008). determined by its mutational neighbourhood. Nature
Hartl, D. L. Darwinian evolution can follow only very 133. Crotty, S., Cameron, C. E. & Andino, R. RNA virus 406, 625–628 (2000).
few mutational paths to fitter proteins. Science 312, error catastrophe: direct molecular test by using 155. Domingo, E., Sheldon, J. & Perales, C. Viral
111–114 (2006). ribavirin. Proc. Natl Acad. Sci. USA 98, 6895–6900 quasispecies evolution. Microbiol. Mol. Biol. Rev. 76,
Analysis of the multistep evolution of high-level (2001). 159–216 (2012).
resistance to β-lactamases reveals that only a few Show experimentally that RNA virus mutagens can 156. Jabara, C. B., Jones, C. D., Roach, J., Anderson, J. A.
evolutionary trajectories are accessible and effectively cause a loss of viral viability and may & Swanstrom, R. Accurate sampling and deep
consequently that much of evolution may be represent a promising class of antiviral drugs. sequencing of the HIV‑1 protease gene using a Primer
reproducible and even predictable. 134. Crotty, S. et al. The broad-spectrum antiviral ID. Proc. Natl Acad. Sci. USA 108, 20166–20171
117. Palmer, A. C. & Kishony, R. Understanding, predicting ribonucleoside ribavirin is an RNA virus mutagen. (2011).
and manipulating the genotypic evolution of antibiotic Nat. Med. 6, 1375–1379 (2000). 157. Kinde, I., Wu, J., Papadopoulos, N., Kinzler, K. W. &
resistance. Nat. Rev. Genet. 14, 243–248 (2013). 135. Airaksinen, A., Pariente, N., Menéndez-Arias, L. & Vogelstein, B. Detection and quantification of rare
118. Szybalski, W. & Bryson, V. Genetic studies on Domingo, E. Curing of foot-and-mouth disease virus mutations with massively parallel sequencing. Proc.
microbial cross resistance to toxic agents. J. Bacteriol. from persistently infected cells by ribavirin involves Natl Acad. Sci. USA 108, 9530–9535 (2011).
64, 489–499 (1952). enhanced mutagenesis. Virology 311, 339–349 158. Schmitt, M. W. et al. Detection of ultra-rare mutations
119. Alekshun, M. N. & Levy, S. B. Molecular mechanisms (2003). by next-generation sequencing. Proc. Natl Acad. Sci.
of antibacterial multidrug resistance. Cell 128, 136. Clementi, M. & Lazzarin, A. Human immunodeficiency USA 109, 14508–14513 (2012).
1037–1050 (2007). virus type 1 fitness and tropism: concept, 159. Levy, S. F. et al. Quantitative evolutionary dynamics
120. Stephan, J., Mailaender, C., Etienne, G., Daffé, M. & quantification, and clinical relevance. Clin. Microbiol. using high-resolution lineage tracking. Nature 519,
Niederweis, M. Multidrug resistance of a porin deletion Infect. 16, 1532–1538 (2010). 181–186 (2015).
mutant of Mycobacterium smegmatis. Antimicrob. 137. Smith, R. A., Loeb, L. A. & Preston, B. D. Developed a sequence-based system to track
Agents Chemother. 48, 4163–4170 (2004). Lethal mutagenesis of HIV. Virus Res. 107, 215–228 500,000 yeast lineages, thus simultaneously
121. Garcia, L. G. et al. Antibiotic activity against (2005). revealing significant differences in early and later
small-colony variants of Staphylococcus aureus: 138. Pfeiffer, J. K. & Kirkegaard, K. A single mutation in evolutionary events.
review of in vitro, animal and clinical data. poliovirus RNA-dependent RNA polymerase confers 160. Qi, H. et al. A quantitative high-resolution genetic
J. Antimicrob. Chemother. 68, 1455–1464 (2013). resistance to mutagenic nucleotide analogs via profile rapidly identifies sequence determinants of
122. Perichon, B. & Courvalin, P. Synergism between increased fidelity. Proc. Natl Acad. Sci. USA 100, hepatitis C viral fitness and drug sensitivity. PLoS
β-lactams and glycopeptides against VanA-type 7289–7294 (2003). Pathog. 10, e1004064 (2014).
methicillin-resistant Staphylococcus aureus and 139. Pfeiffer, J. K. & Kirkegaard, K. Ribavirin resistance in 161. Ding, L., Raphael, B. J., Chen, F. & Wendl, M. C.
heterologous expression of the vanA operon. hepatitis C virus replicon-containing cell lines Advances for studying clonal evolution in cancer.
Antimicrob. Agents Chemother. 50, 3622–3630 conferred by changes in the cell line or mutations in Cancer Lett. 340, 212–219 (2013).
(2006). the replicon RNA. J. Virol. 79, 2346–2355 (2005). 162. Nik-Zainal, S. et al. The life history of 21 breast
Revealed and explained the basis for an 140. Sierra, M. et al. Foot-and-mouth disease virus mutant cancers. Cell 149, 994–1007 (2012).
unexpected and potentially useful synergy between with decreased sensitivity to ribavirin: implications for 163. Zhu, Y. O., Siegal, M. L., Hall, D. W. & Petrov, D. A.
unrelated antibiotics against MRSA. error catastrophe. J. Virol. 81, 2012–2024 (2007). Precise estimates of mutation rate and spectrum in
123. Macvanin, M. & Hughes, D. Hyper-susceptibility of a 141. Pfeiffer, J. K. & Kirkegaard, K. Increased fidelity yeast. Proc. Natl Acad. Sci. USA 111, E2310–E2318
fusidic acid-resistant mutant of Salmonella to different reduces poliovirus fitness and virulence under (2014).
classes of antibiotics. FEMS Microbiol. Lett. 247, selective pressure in mice. PLoS Pathog. 1, e11 164. Bopp, S. E. et al. Mitotic evolution of Plasmodium
215–220 (2005). (2005). falciparum shows a stable core genome but
124. Kim, S., Lieberman, T. D. & Kishony, R. Alternating 142. Perales, C., Agudo, R. & Domingo, E. Counteracting recombination in antigen families. PLoS Genet. 9,
antibiotic treatments constrain evolutionary paths to quasispecies adaptability: extinction of a ribavirin- e1003293 (2013).
multidrug resistance. Proc. Natl Acad. Sci. USA 111, resistant virus mutant by an alternative mutagenic 165. Haase, A. T. et al. Quantitative image analysis of HIV‑1
14494–14499 (2014). treatment. PLoS ONE 4, e5554 (2009). infection in lymphoid tissue. Science 274, 985–989
125. Imamovic, L. & Sommer, M. O. Use of collateral 143. Goldberg, D. E., Siliciano, R. F. & Jacobs, W. R. Jr. (1996).
sensitivity networks to design drug cycling protocols Outwitting evolution: fighting drug-resistant TB, 166. Sandegren, L., Lindqvist, A., Kahlmeter, G. &
that avoid resistance development. Sci. Transl Med. 5, malaria, and HIV. Cell 148, 1271–1283 (2012). Andersson, D. I. Nitrofurantoin resistance mechanism
204ra132 (2013). 144. Fischbach, M. A. Combination therapies for combating and fitness cost in Escherichia coli. J. Antimicrob.
Combined experimental evolution and genome antimicrobial resistance. Curr. Opin. Microbiol. 14, Chemother. 62, 495–503 (2008).
sequencing to map cross-resistance interactions 519–523 (2011). 167. White, S. J. et al. Self-regulation of Candida albicans
between antibiotics in E. coli and derive common 145. Piccolo, M. T., Menale, C. & Crispi, S. Combined population size during GI colonization. PLoS Pathog.
evolutionary principles. anticancer therapies: an overview of the latest 3, e184 (2007).
126. Lazar, V. et al. Genome-wide analysis captures the applications. Anticancer Agents Med. Chem. 15, 168. Miller, L. H., Ackerman, H. C., Su, X. Z. &
determinants of the antibiotic cross-resistance 408–422 (2015). Wellems, T. E. Malaria biology and disease
interaction network. Nat. Commun. 5, 4352 (2014). 146. Hill, J. A., O’Meara, T. R. & Cowen, L. E. pathogenesis: insights for new treatments. Nat. Med.
Experimentally showed the prevalence of collateral Fitness trade-offs associated with the evolution of 19, 156–167 (2013).
sensitivity, a potentially novel therapeutic paradigm resistance to antifungal drug combinations. Cell Rep. 169. Alix-Panabieres, C. & Pantel, K. Challenges in
for the cyclic use of drugs to treat infectious 10, 809–819 (2015). circulating tumour cell research. Nat. Rev. Cancer 14,
diseases and cancer. Identified evolutionary constraints that may 623–631 (2014).
127. Pena-Miller, R. et al. When the most potent minimize the evolution of resistance to
combination of antibiotics selects for the greatest combinations of antifungal drugs. Acknowledgements
bacterial load: the smile–frown transition. PLoS Biol. 147. Lazar, V. et al. Bacterial evolution of antibiotic D.H. and D.I.A. acknowledge funding from the Innovative
11, e1001540 (2013). hypersensitivity. Mol. Syst. Biol. 9, 700 (2013). Medicines Initiative Joint Undertaking under grant agree‑
128. Chait, R., Craney, A. & Kishony, R. Antibiotic 148. Comas, I. et al. Whole-genome sequencing of ment number 115583, resources of which are composed of
interactions that select against resistance. Nature rifampicin-resistant Mycobacterium tuberculosis financial contribution from the European Union’s Seventh
446, 668–671 (2007). strains identifies compensatory mutations in Framework Programme (FP7/2007‑2013) and EFPIA compa‑
A groundbreaking paper exploring the fitness RNA polymerase genes. Nat. Genet. 44, 106–110 nies’ in kind contribution. D.H. and D.I.A. also acknowledge
landscape for the evolution of resistance to (2012). support from Vetenskapsrådet (Swedish Science Council), SSF
multidrug combinations and revealing the trade-offs 149. Silver, L. L. Challenges of antibacterial discovery. Clin. (Swedish Strategic Science Foundation), Vinnova (Swedish
between drug potency and the selection that the Microbiol. Rev. 24, 71–109 (2011). Innovation Science), and the Knut and Alice Wallenberg
drugs impose on emerging resistant populations. 150. Rossolini, G. M., Mantengoli, E., Montagnani, F. & Foundation (RiboCore Project). D.I.A. acknowledges support
129. Hegreness, M., Shoresh, N., Damian, D., Hartl, D. & Pollini, S. Epidemiology and clinical relevance from the EU (EvoTar project).
Kishony, R. Accelerated evolution of resistance in of microbial resistance determinants versus anti-
multidrug environments. Proc. Natl Acad. Sci. USA Gram-positive agents. Curr. Opin. Microbiol. 13, Competing interests statement
105, 13977–13981 (2008). 582–588 (2010). The authors declare no competing interests.
NATURE REVIEWS | GENETICS VOLUME 16 | AUGUST 2015 | 471
© 2015 Macmillan Publishers Limited. All rights reserved
You might also like
- Seeking Wider Access To HIV Testing For Adolescents in Sub-Saharan AfricaDocument8 pagesSeeking Wider Access To HIV Testing For Adolescents in Sub-Saharan AfricaLuis ZabalaNo ratings yet
- Paediatric HIV Infection: The Potential For CureDocument13 pagesPaediatric HIV Infection: The Potential For CureLuis ZabalaNo ratings yet
- Hiv Infection: Prevention ManagementDocument1 pageHiv Infection: Prevention ManagementLuis ZabalaNo ratings yet
- Gut-homing Δ42PD1+Vδ2 T cells promote innate mucosal damage via TLR4 during acute HIV type 1 infectionDocument18 pagesGut-homing Δ42PD1+Vδ2 T cells promote innate mucosal damage via TLR4 during acute HIV type 1 infectionLuis ZabalaNo ratings yet
- Defining Total-Body AIDS-Virus Burden With Implications For Curative StrategiesDocument11 pagesDefining Total-Body AIDS-Virus Burden With Implications For Curative StrategiesLuis ZabalaNo ratings yet
- Integration Site Selection by Retroviruses and Transposable Elements in EukaryotesDocument17 pagesIntegration Site Selection by Retroviruses and Transposable Elements in EukaryotesLuis ZabalaNo ratings yet
- Hiv Infection: Prevention ManagementDocument1 pageHiv Infection: Prevention ManagementLuis ZabalaNo ratings yet
- Paediatric HIV Infection: The Potential For CureDocument13 pagesPaediatric HIV Infection: The Potential For CureLuis ZabalaNo ratings yet
- HIV Reservoirs: What, Where and How To Target ThemDocument6 pagesHIV Reservoirs: What, Where and How To Target ThemLuis ZabalaNo ratings yet
- Steven Deeks. HIV Infection PDFDocument22 pagesSteven Deeks. HIV Infection PDFLuis ZabalaNo ratings yet
- E Herrera-Carrillo, A Harwig and B Berkhout. Silencing of HIV-1 by AgoshRNA MoleculesDocument9 pagesE Herrera-Carrillo, A Harwig and B Berkhout. Silencing of HIV-1 by AgoshRNA MoleculesLuis ZabalaNo ratings yet
- RochaDocument13 pagesRochaLuis ZabalaNo ratings yet
- Vih PDFDocument10 pagesVih PDFdouglasvargas-1No ratings yet
- Pancera, M. Bylund, T. Druz, A. Lai, YT. Crystal Structures of Trimeric HIV Envelope With Entry Inhibitors BMS 378806 and BMS-626529Document10 pagesPancera, M. Bylund, T. Druz, A. Lai, YT. Crystal Structures of Trimeric HIV Envelope With Entry Inhibitors BMS 378806 and BMS-626529Luis ZabalaNo ratings yet
- Beryl A. Koblin, Walid Heneine 1970s and Patient 0' HIV-1 Genomes Illuminate Early HIVAIDS History in North AmericaDocument17 pagesBeryl A. Koblin, Walid Heneine 1970s and Patient 0' HIV-1 Genomes Illuminate Early HIVAIDS History in North AmericaLuis ZabalaNo ratings yet
- Z Huang, A Tomitaka. Current Application of CRISPR-Cas9 Gene-Editing Technique To Eradication of HIV-AIDSDocument8 pagesZ Huang, A Tomitaka. Current Application of CRISPR-Cas9 Gene-Editing Technique To Eradication of HIV-AIDSLuis ZabalaNo ratings yet
- E Herrera-Carrillo, A Harwig and B Berkhout. Silencing of HIV-1 by AgoshRNA MoleculesDocument9 pagesE Herrera-Carrillo, A Harwig and B Berkhout. Silencing of HIV-1 by AgoshRNA MoleculesLuis ZabalaNo ratings yet
- RochaDocument13 pagesRochaLuis ZabalaNo ratings yet
- 25 32Document288 pages25 32Mina MladenovicNo ratings yet
- Z Huang, A Tomitaka. Current Application of CRISPR-Cas9 Gene-Editing Technique To Eradication of HIV-AIDSDocument8 pagesZ Huang, A Tomitaka. Current Application of CRISPR-Cas9 Gene-Editing Technique To Eradication of HIV-AIDSLuis ZabalaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5782)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Wiper & Washer Circuit PDFDocument1 pageWiper & Washer Circuit PDFluis eduardo corzo enriquezNo ratings yet
- English Terms 1 Major Assessment Worksheet Answer KeyDocument29 pagesEnglish Terms 1 Major Assessment Worksheet Answer KeySamiNo ratings yet
- Hanoi 2023 Peoples Picks AwardsDocument113 pagesHanoi 2023 Peoples Picks AwardsNguyen Anh VuNo ratings yet
- Coyle Chapter 2 PowerPoint SlidesDocument33 pagesCoyle Chapter 2 PowerPoint SlidesKhaled Sheykh0% (1)
- Auto IntroductionDocument90 pagesAuto IntroductionShivanand ArwatNo ratings yet
- Civil Engineering Set 2Document13 pagesCivil Engineering Set 2Dev ThakurNo ratings yet
- Compression Molding of Gypsum Blocks Using Ecological Brick MachinesDocument11 pagesCompression Molding of Gypsum Blocks Using Ecological Brick Machinessami fanuaelNo ratings yet
- Explore the Precambrian EraDocument3 pagesExplore the Precambrian EraArjay CarolinoNo ratings yet
- Op-Amp Comparator: Astable (Or Free-Running) Multivibrators Monostable MultivibratorsDocument5 pagesOp-Amp Comparator: Astable (Or Free-Running) Multivibrators Monostable MultivibratorsYuvaraj ShanNo ratings yet
- House Service Connection NEW BSR 2020-1Document1 pageHouse Service Connection NEW BSR 2020-1Deshraj BairwaNo ratings yet
- Price List Grand I10 Nios DT 01.05.2022Document1 pagePrice List Grand I10 Nios DT 01.05.2022VijayNo ratings yet
- Sir ClanDocument109 pagesSir ClanJames AbendanNo ratings yet
- June 2023 BillingDocument10 pagesJune 2023 BillingEsther AkpanNo ratings yet
- Router ScriptDocument10 pagesRouter ScriptfahadNo ratings yet
- JAN LOHFELDT vs. NEDBANK LTD - Cape Town High Court Judge Goliath (24.02.2014) & Judge Zondi (25.02.2014)Document24 pagesJAN LOHFELDT vs. NEDBANK LTD - Cape Town High Court Judge Goliath (24.02.2014) & Judge Zondi (25.02.2014)willNo ratings yet
- Case CX210B Mine Crawler Excavator Tier 3 Parts Manual PDFDocument701 pagesCase CX210B Mine Crawler Excavator Tier 3 Parts Manual PDFJorge Martinez100% (3)
- Lab 7 Activities Sheet Winter 2020Document7 pagesLab 7 Activities Sheet Winter 2020Mareline MendietaNo ratings yet
- 2003 VW Jetta Wiring DiagramsDocument123 pages2003 VW Jetta Wiring DiagramsmikeNo ratings yet
- D-Glucitol (420i) Dextrose MonohydrateDocument3 pagesD-Glucitol (420i) Dextrose MonohydrateSilvia Melendez HNo ratings yet
- Energy Monitoring With Ultrasonic Flow MetersDocument35 pagesEnergy Monitoring With Ultrasonic Flow MetersViswa NathanNo ratings yet
- Captain Marvel (DC Comics) : Shazam! Navigation SearchDocument34 pagesCaptain Marvel (DC Comics) : Shazam! Navigation SearchAce Orense Cupid Uranus Ace Sphinx Galzu Acetr444 son of Multiverses Chaos Gaeia Eros ACETR444No ratings yet
- In Situ Combustion: Amit Kumar Singh R270307004 Integrated (Ape) +mba (Uam) Semester: VIIIDocument17 pagesIn Situ Combustion: Amit Kumar Singh R270307004 Integrated (Ape) +mba (Uam) Semester: VIIISmita SharmaNo ratings yet
- Land Rover Range Rover Owners Manual 2007Document358 pagesLand Rover Range Rover Owners Manual 2007PetreCaracaleanu0% (1)
- GadDocument1 pageGadFakhruddin DhilawalaNo ratings yet
- Turbofarmer P 34.7: AustraliaDocument2 pagesTurbofarmer P 34.7: AustraliaDenis OhmakNo ratings yet
- This Demonstration Covers The Usage of V-Ray Render Elements in Adobe PhotoshopDocument15 pagesThis Demonstration Covers The Usage of V-Ray Render Elements in Adobe PhotoshopBartek BanterNo ratings yet
- Aqua Mon 4000 PH Red Ox AnalyserDocument4 pagesAqua Mon 4000 PH Red Ox Analyserarvindgupta_2005No ratings yet
- Pic24fj256ga705 Family Data Sheet Ds30010118eDocument424 pagesPic24fj256ga705 Family Data Sheet Ds30010118eD GzHzNo ratings yet
- Carbozinc 859: Selection & Specification Data Substrates & Surface PreparationDocument2 pagesCarbozinc 859: Selection & Specification Data Substrates & Surface PreparationAmy JonesNo ratings yet