Professional Documents
Culture Documents
Cervical Epidural Pressure Measurement: Comparison in The Prone and Sitting Positions
Uploaded by
Gabriel PaezOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cervical Epidural Pressure Measurement: Comparison in The Prone and Sitting Positions
Uploaded by
Gabriel PaezCopyright:
Available Formats
PAIN MEDICINE Anesthesiology 2010; 113:666 –71
Copyright © 2010, the American Society of Anesthesiologists, Inc. Lippincott Williams & Wilkins
Cervical Epidural Pressure Measurement
Comparison in the Prone and Sitting Positions
Jee Y. Moon, M.D.,* Pyung-Bok Lee, M.D., Ph.D.,† Francis Sahngun Nahm, M.D.,‡
Yong-Chul Kim, M.D., Ph.D.,§ Jong-Bum Choi, M.D.㛳
ABSTRACT inappropriate for identifying the cervical epidural space in
Background: The hanging drop technique is used for iden- either the prone or sitting positions.
tifying the cervical epidural space, using its negative pressure.
However, it is doubtful whether the epidural space intrinsi-
What We Already Know about This Topic
cally exhibits a negative pressure. We designed this study to
test the hypothesis that the cervical epidural pressure (CEP) ❖ The hanging drop method to identify the cervical epidural
space assumes a negative pressure that may not occur in all
is significantly higher in the prone position than in the sitting patients and patient positions.
position. To evaluate this hypothesis, we measured and com-
pared 30 CEP values in the prone and sitting positions. What This Article Tells Us That Is New
Methods: We measured and compared 15 CEPs in the ❖ In 15 patients receiving cervical epidural injections in the prone
prone group and 15 in the sitting group using a closed pres- position, epidural pressure was positive in every case, and in
another 15 in the sitting position, it was not uniformly negative.
sure measurement system under fluoroscopic guidance.
❖ The hanging drop method may not identify the epidural space
Results: All CEPs in the prone group were consistently pos- in all patients, particularly when they are in the prone position.
itive (median, 10 mmHg; range, 4.8 –18.7; mean ⫾ SD,
10.5 ⫾ 4.4) in contrast to the sitting group (median, ⫺0.3
mmHg; range, ⫺2.4 –7.9; mean ⫾ SD, 0.5 ⫾ 2.8). CEPs in
the prone group were significantly higher than in the sitting C ERVICAL epidural steroid injections (CESIs) are used
worldwide for the conservative management of head,
neck, and upper extremity pain.1–3 When performing
group (P ⬍ 0.001).
Conclusion: CEP was found to be significantly higher in the CESIs, proper identification of the epidural space is impera-
prone position than in the sitting position. Furthermore, tive to minimize the risk of dural puncture, which is associ-
CEPs were not consistently negative even in the sitting posi- ated with potentially catastrophic complications, such as per-
manent spinal cord injury.4 –7
tion. These results suggest that the hanging drop technique is
To identify the cervical epidural space, practitioners oc-
casionally use the hanging drop (HD) technique,8 which
identifies the epidural space using its negative pressure.9
* Clinical Assistant Professor, Department of Anesthesiology and However, it is doubtful whether the epidural space intrinsi-
Pain Medicine, East and West Neo Medical Center, Kyung Hee Univer-
sity Medical School, Seoul, Republic of Korea. † Assistant Professor, cally exhibits a negative pressure. In previous studies, in
‡ Clinical Assistant Professor, Department of Anesthesiology and Pain which closed pressure measurement systems were used,10 –12
Medicine, Seoul National University Bundang Hospital, Seoul National epidural pressure (EP) was commonly found to be positive at the
University College of Medicine, Kyonggi-do, Republic of Korea. § Profes-
sor, Department of Anesthesiology and Pain Medicine, Seoul National thoracic level in the lateral decubitus position and to be consis-
University Hospital, Seoul National University College of Medicine, Seoul, tently negative only in the sitting position.10 These results sug-
Republic of Korea. 㛳 Clinical Assistant Professor, Department of Anesthe- gest that EP is influenced by body position, and that patients
siology and Pain Medicine, Gangnam Severance Hospital, Yonsei Univer-
sity College of Medicine, Seoul, Republic of Korea. should be seated when the HD technique is used. However, to
Received from the Department of Anesthesiology and Pain Med- our knowledge, no report or peer-reviewed article has been con-
icine, Seoul National University Bundang Hospital, Sungnam-si, ducted on the topic of cervical epidural pressure.
Kyonggi-do, Republic of Korea. Submitted for publication Decem- Accordingly, we designed this study to test the hypothesis
ber 11, 2009. Accepted for publication May 13, 2010. Support was
provided solely from institutional and/or departmental sources. that CEP is significantly higher in the prone position than in
Address correspondence to Dr. Lee: Department of Anesthesiol- the sitting position. To evaluate this hypothesis, we measured
ogy and Pain Medicine, Seoul National University Bundang Hospi-
tal, Seoul National University College of Medicine, 300 Kumi-dong,
Sungnam-si, Bundang-gu, Kyonggi-do, 463-707, Republic of Korea. 䉫 This article is featured in “This Month in Anesthesiology.”
painfree@snubh.org. This article may be accessed for personal use Please see this issue of ANESTHESIOLOGY page 9A.
at no charge through the Journal Web site, www.anesthesiology.org.
666 Anesthesiology, V 113 • No 3 • September 2010
Cervical Epidural Pressure Measurement
and compared CEPs in prone and sitting groups using a closed
pressure measurement system under fluoroscopic guidance.
Materials and Methods
We conducted an open-labeled, randomized, comparative
study. CEP measurements were taken in 30 patients sched-
uled for CESIs.
This study was approved by the Institutional Review
Board of Seoul National University Bundang Hospital
(Sungnam-si, Kyonggi-do, Republic of Korea) and was reg-
istered with Clinical Trials (Ref: NCT01009385). Assess-
ments and procedures were carried out at a university-based
pain clinic. All participants were given extensive written and
verbal information about the trial, and of its potential bene-
fits and risks, before they provided written consent.
The inclusion and exclusion criteria are listed in table 1
and patient selection and allocations to the prone and sitting
groups are described the flow diagram in figure 1. An inde-
pendent researcher performed the group allocations using a
computer-generated random list.
All epidural injections were performed by one pain clini- Fig. 1. Flow diagram showing enrollment, random allocation,
cian (J.M.), using the midline approach at the C6 –C7 level, follow-up, and analysis. The diagram shows the number of
where fluoroscopic lateral images showed no overlap with participants in each intervention group. CESI ⫽ cervical epi-
adjacent structures of the torso or arms in the prone or sitting dural steroid injection.
positions. During CESI, patients in both groups were asked
to place their heads on the table (a small headrest was placed gauge Tuohy needle with attachable wing (Tae-Chang In-
under the forehead) and to flex their necks fully, which max- dustrial Co., Kongju, Republic of Korea) was inserted in the
imally widens the C6 –C7 interlaminar space. After aseptic midline with a tunnel view parallel to the trajectory of the
preparation and skin infiltration with 1% lidocaine, a 20- spinous processes under fluoroscopic guidance using antero-
posterior images. When the needle was firmly grasped, a
Table 1. Inclusion and Exclusion Criteria lateral image was taken to ensure that the needle tip was
positioned in the C6 –C7 supraspinous or interspinous liga-
Inclusion criteria ment. EP measurements were then taken using a closed mea-
(1) Age 20 to 80 yr
(2) Cervical radicular pain caused by herniated surement system.12 In brief, a saline reservoir was placed at
nucleus pulposus, spinal stenosis, or other the level of the transducer (Autotransfuser®; Acemedical,
conditions, including herpes zoster-associated Kyonggi-do, Republic of Korea) to prevent saline from flow-
pain and sprain for more than 3 months ing into the epidural space. The zero level was set at the
(3) Axial cervical pain consisting of generalized needle insertion point using a laser-leveling device. After re-
neck symptoms, zygapophysial joint pain, or moving of the stylet in the Tuohy needle, the needle was
interscapular pain filled with saline and connected to the pressure monitoring
(4) Pain intensity ⱖ 5 of maximum 10 NRS
(5) Failure to improve with conservative treatment
system equipped with a disposable transducer via an 80-cm
(6) Cervical epidural location of needle confirmed long polyvinyl chloride tube also filled with saline. Maintain-
by the fluoroscopic images ing the same trajectory in the lateral plane, we advanced the
Exclusion criteria epidural needle very slowly holding the attachable wing in
(1) Acute infection place with our thumbs and index fingers under fluoroscope
(2) Patient refusal guidance using lateral images. The high pressure was ob-
(3) Previous cervical spine surgery
(4) Structural spinal deformities served during passage through the ligament flavum. The nee-
(5) Rapidly worsening pain, numbness, dle should not be advanced beyond the spinolaminar line. A
weakness, hyperreflexia, changes in bladder tactile sensation of give with a precipitous decrease in the
function, and other neurological symptoms that displayed pressure was noted just as the needle was entered
should prompt a reevaluation and surgical the epidural space. The bevel of the needle was considered to
evaluation have entered the epidural space when a typical waveform was
(6) Pregnancy observed, which consisted of small cardiac oscillations super-
(7) Allergy to contrast media or drugs to be used
in the procedure
imposed on greater respiratory oscillations. The needle was
then held immobile in the epidural space for 120 s to allow
NRS ⫽ numerical rating scale. the epidural pressure to stabilize, and CEP was measured.
Moon et al. Anesthesiology, V 113 • No 3 • September 2010 667
PAIN MEDICINE
Fig. 2. (A) Lateral fluoroscopic images of cervical epidural puncture performed at the C6 –C7 interspace. is the angle of the
needle with respect to the gravity. (B) The diagram shows that the vertical distance between the transducer and needle tip can
be calculated from the needle depth and angle against gravity. Distance ⫽ needle depth ⫻ cos(angle against gravity).
The greatest positive pressure generated during needle hydrochloride (Chirocaine®; Abbott Korea Ltd, Seoul, Re-
passage through the ligament flavum, the initial negative public of Korea), and 3.5 ml of normal saline (0.9% NaCl)
pressure measured on entering the epidural space, and mea- was then slowly infused under live fluoroscopy. After the
sured CEP were recorded by an anesthesiologist unaware of procedure, patients were observed for adverse effects, and a
study details. The same anesthesiologist then recorded needle neurologic examination was performed in a recovery room
depth and needle angle with respect to the gravity (fig. 2A). by a specially trained nurse in each case.
The measured CEP values were corrected to EP valued at the
needle tip (fig. 2B) using the following formula: Epidural Statistical Analysis
pressure ⫽ measured pressure ⫹ [needle depth ⫻ cos(measured The sample size calculations were based on the findings of a
needle angle) ⫻ 0.735], where 0.735 is a unit conversion factor previous study, which reported a mean EP at the T5–T6 level
(1 cm H2O ⫽ 0.735 mmHg). In addition, neck flexion angle of ⫺7.2 ⫾ 6.3 mmHg in the sitting position and ⫺5.1 ⫾ 4.4
was measured using a goniometer placed on the C7 spinous mmHg in the lateral decubitus position.10 Based on a type 1
process with respect to the line between the occiput and the error of 0.05, a type 2 error of 0.1, and a two-sided test, at
upper thoracic spinous process on lateral fluoroscopic image. least seven patients per group were required for the analysis,
Final needle positions were checked to ensure that the but because we were unaware of pressure ranges in the cervi-
needle was at or only slightly beyond the spinolaminar line in cal epidural space, we included 16 patients per group. An
the lateral fluoroscopic radiograph and midline in the antero- independent reviewer provided statistical analysis using SPSS
posterior radiograph. A syringe contained contrast medium version 15.0 (SPSS, Chicago, IL). Fisher exact test was used
(Omnipaque® 300 [iohexol, 300 mg of iodine per ml]; GE to compare frequency differences in the two groups; the
Healthcare, Piscataway, NJ) was attached to low-volume ex- Mann–Whitney U test was used to calculate statistical differ-
tension tubing and flushed. Before attaching the extension ences in continuous variables; and Spearman’s correlation
tubing, the Tuohy needle was disconnected from the pres- coefficients were used to examine the relationship between
sure monitoring system equipped with a disposable trans- CEP values and the measurements of the subjects. Analysis of
ducer, and a drop of contrast was placed in the needle to flush covariance, adjusted for neck flexion angle as a covariate, was
out any air. Then, under live fluoroscopy, contrast was in- used to compare CEPs in the two groups. P values of less than
jected evaluating for epidural flow and ensuring no vascular 0.05 were considered statistically significant.
pattern. If a venous pattern occured, the needle was with-
drawn and repositioned, but its CEP was excluded from the
data analysis. If an arterial pattern or a myelographic pattern Results
indicating subarachnoid injection occurred, CESIs were Thirty-six patients treated in October and November 2009
abandoned and their CEPs were excluded. If contrast was were enrolled; among them, 32 patients were randomly allo-
confirmed to flow epidurally along the spinolaminar line cated to the prone and sitting groups (fig. 1). However, two
creating a dorsal stripe, the needle was readjusted and a so- patients (one in each group) who showed a typical waveform
lution (5 ml) containing 10 mg triamcinolone acetonide sus- of the epidural space were excluded because the needle tip
pension (Tamcelon®; HanAll Pharmaceutical Co., Ltd., was found to be located in the subdural space on the lateral
Seoul, Republic of Korea), 1.5 ml of 0.75% levobupivacaine and anteroposterior fluoroscopic images. No CESI was per-
668 Anesthesiology, V 113 • No 3 • September 2010 Moon et al.
Cervical Epidural Pressure Measurement
Table 2. Demographics of Patients Table 3. Association between Cervical Epidural
Pressure and Covariates
Prone Sitting
Group Group ANCOVA
(n ⫽ 15) (n ⫽ 15)
Variables F Value P Value
Age, yr 57.5 ⫾ 15.8 46.3 ⫾ 15.3
Weight, kg 59.9 ⫾ 14.9 61.5 ⫾ 11.0 Neck Flexion Angle 0.689 0.415
Height, cm 159.4 ⫾ 9.9 163.7 ⫾ 10.4 Body Position 9.457 0.005
Male/Female 4/11 7/8 Neck Flexion Angle 0.041 0.841
Duration of Symptoms, 5.8 ⫾ 4.7 5.7 ⫾ 5.2 X Body Position
mo
F value shows the strength of association of body position and
Indications for CESI
cervical epidural pressure by analysis of covariance (ANCOVA)
Herniated Nucleus 4 3 regression analysis.
Pulposus
Spinal Stenosis 2 2
Herpes Zoster- 1 1 range, ⫺2.4 –7.9; mean ⫾ SD, 0.5 ⫾ 2.8) in the sitting group
associated Pain (fig. 3). Ten EPs in the sitting group were negative and five were
Sprain 8 9 positive. All 15 EPs in the prone group were positive. According
Neck Flexion Angle (°) 18.6 ⫾ 9.7* 9.3 ⫾ 4.7 to the Mann–Whitney U test, mean CEP in the prone group
was significantly higher than in the sitting group (P ⬍ 0.001).
Data are reported as mean ⫾ SD or number of patients.
* P ⬍ 0.05 vs. sitting group.
Furthermore, mean neck-flexion angles differed in the two
CESI ⫽ cervical epidural steroid injection. groups (P ⫽ 0.01). Spearman’s correlation analysis revealed a
moderate degree of correlation between CEP and neck flexion
formed in these two patients. No significant clinical or de- angle (r ⫽ 0.53, P ⫽ 0.004). Therefore, analysis of covariance
mographic differences were found between the two groups was used, adjusted for neck flexion angle as a covariate. Conse-
except for neck-flexion angle (table 2). quently, a significant difference was found between mean CEPs
Median EP was 10.0 mmHg (interquartile range, 6.4 – in the two groups (P ⫽ 0.005) (table 3).
13.6; range, 4.8 –18.7; mean ⫾ SD, 10.5 ⫾ 4.4) in the prone A high positive pressure (from ⫹35 mmHg to ⫹283
group and ⫺0.3 mmHg (interquartile range, ⫺1.3–2.0; mmHg) was observed during needle passage through the
Fig. 3. The difference in epidural pressure between the prone and sitting groups. Data are shown as box-and-whisker plots.
Cervical epidural pressure in the sitting group was lower than in the prone group (P ⫽ 0.005). Box boundaries show 25th to 75th
percentiles; lines within boxes indicate medians, whiskers above and below boxes indicate 10th to 90th percentiles, and a dot
shows the outlier.
Moon et al. Anesthesiology, V 113 • No 3 • September 2010 669
PAIN MEDICINE
ligamentum flavum. However, at the moment of epidural and that CEP in the sitting position was not always subat-
puncture, high negative pressures (range, ⫺27.0 to ⫺2.0 mospheric. The reasons for this difference can be speculated
mmHg) were observed for a few seconds in seven cases, as has upon. While performing a CESI, the cervical spine should be
been previously reported.12 However, in these patients, epi- flexed to open the interlaminar space as widely as possible.
dural pressure soon stabilized at ⫺2.4 to ⫹4.0 mmHg Previous studies have suggested that rapid, large increases in
within 120 s. EP could be produced by compression of the jugular vein18
Reported complications at follow-up examinations were or by neck flexion.19 Anatomically, the epidural veins are
minor and transitory: headache episodes, 2 of 30; facial flush- concentrated in the anterolateral portion of the epidural
ing, 2 of 30; and transient pain, 3 of 30. space,20 but in the presence of an obstruction to venous
run-off, the mid-posterior epidural space is likely to contain
large, distended, high-pressure veins, which would reduce
Discussion the volume of the entire posterior epidural space. Indeed, the
The present study is the first to report CEP values measured epidural space may play a role as a cushion and absorb pres-
using a closed pressure measurement system. In particular, sures generated by an over-distended epidural venous plexus.
CEP was found to be significantly higher in the prone posi- In the cervical region, the smaller cervical epidural space20
tion than in the sitting position. Furthermore, all CEPs in could reduce this cushioning effect compared with the epi-
the prone group were consistently positive, whereas in the dural space at the thoracic level. We believe that this is the
sitting group, median CEP was almost zero. reason why CEP was not found to be consistently negative in
Cervical epidural punctures are occasionally performed the sitting position.
using the HD technique,8,13 which depends on a negative EP Whether neck flexion increases CEP is debatable. In a
to draw saline into the needle hub. Furthermore, the subat- previous report,21 cranial spread of contrast medium was
mospheric nature of CEP has been suggested to be an excel- found to be significantly increased by neck flexion, and it has
lent, reliable indicator of epidural needle placement.13 How- been speculated that the decrease in EP observed after flexion
ever, we found that all 15 CEPs measured in the prone at the lumbar level22 could also occur after flexion at the
position and 5 of 15 in the sitting position were positive, cervical spine level.21 However, it has never been claimed
which implies that the HD technique is inappropriate for that neck-flexion angle affects contrast spread.23 In one
performing CESIs. study, it was suggested that an anterior shift of the posterior
Negative pressures are believed to be generated by either aspect of the dura during neck flexion probably results in a
tenting of the dura caused by an advancing blunt needle14 or transient negative pressure in the posterior spinal canal, and
to the retraction of the ligamentum flavum.15 Furthermore, consequently increases venous volume within the posterior
they have been suggested to be more important than absolute epidural venous plexus,24 which we believe could increase
pressures within the epidural space when the HD technique CEP.
is used.16 However, the ligamentum flavum in the cervical The present study could be criticized for a failure to con-
region is relatively thin and frequently is not fused at the trol neck-flexion angle in the two groups. However, a sup-
midline.17 Furthermore, we observed an initial negative pres- plementary study failed to reveal any change in neck-flexion
sure in only 7 of the 30 subjects. Despite the fact that we used angle after patient repositioning. Evidently, further study of
a less curved needle, which may have penetrated the ligamen- the relationship between CEP and neck-flexion angle is
tum flavum more smoothly and thereby may have induced needed.
fewer artifactual effects, such as dura tenting or ligamentum Several other study limitations warrant consideration.
flavum retraction,10 we believe that EP is often nonnegative First, differences between EPs in different body positions
in the cervical spine; thus, a negative CEP should not be may have been better analyzed by comparing among individ-
crucial for the HD technique. ual patients rather than between patient groups. However,
In a previous report, EP was found to be more negative in there are risks associated with changing the position of a
the sitting position than in the lateral decubitus position, and patient with a needle inserted in the cervical epidural space.
EPs in the sitting position were found to be consistently Second, the possible relations between pathologic conditions
subatmospheric.10 This suggests that EP differences in dif- at the C6 –C7 level and CEP were not investigated because
ferent patient positions are generated by gravity. That is to patient numbers were limited. Furthermore, in each case,
say, blood in the epidural plexus and cerebrospinal fluid in different amounts of contrast medium were injected to con-
the dural sac are redistributed on changing body positions, firm needle tip location in epidural space; thus, we could not
and the sitting position favors a negative EP. We presume evaluate whether contrast flow was affected by pressure re-
that this phenomenon is also applicable to CEP; thus, CEP cording. Accordingly, we suggest that additional investiga-
should be consistently negative, and theoretically more neg- tions be undertaken to examine relations between CEP and
ative than thoracic EP, at least in the sitting position. How- pathologic conditions at the C6 –C7 level and contrast flow
ever, we found that median CEP in the sitting position was rates.
greater than the median thoracic EP reported previously In summary, we found that CEP was significantly greater
(measured using a closed pressure measurement system),10 in the prone position than in the sitting position. Further-
670 Anesthesiology, V 113 • No 3 • September 2010 Moon et al.
Cervical Epidural Pressure Measurement
more, CEPs were not consistently negative even in the sitting 11. Visser WA, Gielen MJ, Giele JL, Scheffer GJ: A comparison of
epidural pressures and incidence of true subatmospheric epi-
position. These results suggest that the HD technique is in- dural pressure between the mid-thoracic and low-thoracic epi-
appropriate for identifying the cervical epidural space in the dural space. Anesth Analg 2006; 103:1318 –21
prone or sitting positions. 12. Okutomi T, Watanabe S, Goto F: Time course in thoracic
epidural pressure measurement. Can J Anaesth 1993; 40:
The authors are grateful to Jin-Hee Kim, M.D., Ph.D. (Associate 1044 – 8
Professor, Department of Anesthesiology and Pain Medicine, Seoul 13. Lirk P, Colvin J, Steger B, Colvin HP, Keller C, Rieder J,
National University Bundang Hospital, Kyonggi-do, Republic of Kolbitsch C, Moriggl B: Incidence of lower thoracic liga-
Korea), and Jin S. Yeom, M.D., Ph.D. (Associate Professor, Depart- mentum flavum midline gaps. Br J Anaesth 2005; 94:852–5
ment of Orthopedic Surgery, Seoul National University Bundang 14. Janzen E: Der negative Vorschlag bei Lumbalpunktion.
Hospital), for their supervision and guidance. Dtsch Z Nervenheilkd 1926; 94:280 –92
15. Zarzur E: Genesis of the ‘true’ negative pressure in the
lumbar epidural space. A new hypothesis. Anaesthesia
References 1984; 39:1101– 4
1. Strub WM, Brown TA, Ying J, Hoffmann M, Ernst RJ, Bulas 16. Hoffmann VL, Vercauteren MP, Vreugde JP, Hans GH,
RV: Translaminar cervical epidural steroid injection: Short- Coppejans HC, Adriaensen HA: Posterior epidural space
term results and factors influencing outcome. J Vasc Interv depth: Safety of the loss of resistance and hanging drop
Radiol 2007; 18:1151–5 techniques. Br J Anaesth 1999; 83:807–9
2. Stav A, Ovadia L, Sternberg A, Kaadan M, Weksler N: 17. Lirk P, Kolbitsch C, Putz G, Colvin J, Colvin HP, Lorenz I,
Cervical epidural steroid injection for cervicobrachialgia. Keller C, Kirchmair L, Rieder J, Moriggl B: Cervical and
Acta Anaesthesiol Scand 1993; 37:562– 6 high thoracic ligamentum flavum frequently fails to fuse in
3. Castagnera L, Maurette P, Pointillart V, Vital JM, Erny P, the midline. ANESTHESIOLOGY 2003; 99:1387–90
Sénégas J: Long-term results of cervical epidural steroid 18. Yokoyama T, Ushida T, Yamasaki F, Inoue S, Sluka KA:
injection with and without morphine in chronic cervical Epidural puncture can be confirmed by the Queckenstedt-
radicular pain. Pain 1994; 58:239 – 43 test procedure in patients with cervical spinal canal ste-
4. Stojanovic MP, Vu TN, Caneris O, Slezak J, Cohen SP, Sang nosis. Acta Anaesthesiol Scand 2008; 52:256 – 61
CN: The role of fluoroscopy in cervical epidural steroid 19. Usubiaga JE, Moya F, Usubiaga LE: Effect of thoracic and
injections: An analysis of contrast dispersal patterns. Spine abdominal pressure changes on the epidural space pres-
2002; 27:509 –14 sure. Br J Anaesth 1967; 39:612– 8
5. Hodges SD, Castleberg RL, Miller T, Ward R, Thornburg C: 20. Hogan QH: Epidural anatomy: New observations. Can J
Cervical epidural steroid injection with intrinsic spinal Anaesth 1998; 45:R40 – 8
cord damage. Two case reports. Spine 1998; 23:2137– 42
21. Lee CJ, Jeon Y, Lim YJ, Bahk JH, Kim YC, Lee SC, Kim CS:
6. Manchikanti L: Cervical epidural steroid injection with The influence of neck flexion and extension on the distri-
intrinsic spinal cord damage. Spine 1999; 24:1170 –2 bution of contrast medium in the high thoracic epidural
7. Abbasi A, Malhotra G, Malanga G, Elovic EP, Kahn S: space. Anesth Analg 2007; 104:1583– 6
Complications of interlaminar cervical epidural steroid in- 22. Takahashi K, Miyazaki T, Takino T, Matsui T, Tomita K:
jections: A review of the literature. Spine 2007; Epidural pressure measurements. Relationship between
32:2144 –51 epidural pressure and posture in patients with lumbar
8. Cluff R, Mehio AK, Cohen SP, Chang Y, Sang CN, Sto- spinal stenosis. Spine 1995; 20:650 –3
janovic MP: The technical aspects of epidural steroid in- 23. Goel A, Pollan JJ: Contrast flow characteristics in the
jections: A national survey. Anesth Analg 2002; 95:403– 8 cervical epidural space: An analysis of cervical epiduro-
9. Gutierrez A: Anesthesia metamerica peridural. Rev Circ B grams. Spine 2006; 31:1576 –9
Aires 1932; 12:665– 85 24. Patel TR, Chiocca EA, Freimer ML, Christoforidis GA: Lack
10. Gil NS, Lee JH, Yoon SZ, Jeon Y, Lim YJ, Bahk JH: Comparison of epidural pressure change with neck flexion in a patient
of thoracic epidural pressure in the sitting and lateral decubitus with Hirayama disease: Case report. Neurosurgery 2009;
positions. ANESTHESIOLOGY 2008; 109:67–71 64:E1196 –7
Moon et al. Anesthesiology, V 113 • No 3 • September 2010 671
You might also like
- Guide to Complex Interventional Endoscopic ProceduresFrom EverandGuide to Complex Interventional Endoscopic ProceduresKelly EspondaNo ratings yet
- Touhy y CateterDocument8 pagesTouhy y CateterhumildementeanestesiosNo ratings yet
- Comparison of Three Sitting Positions For Combined Spinal - Epidural Anesthesia: A Multicenter Randomized Controlled TrialDocument8 pagesComparison of Three Sitting Positions For Combined Spinal - Epidural Anesthesia: A Multicenter Randomized Controlled TrialFadhilNo ratings yet
- The Skin-To-Epidural Distance of Parturients by UlDocument5 pagesThe Skin-To-Epidural Distance of Parturients by UlzakyNo ratings yet
- Laryngoscopy and Tracheal Intubation in The.25 PDFDocument7 pagesLaryngoscopy and Tracheal Intubation in The.25 PDFFazaKhilwanAmnaNo ratings yet
- Apm 20072Document7 pagesApm 20072ida wahyuni mapsanNo ratings yet
- KJR 16 604Document9 pagesKJR 16 604Winna Eka PNo ratings yet
- Figure of 8Document6 pagesFigure of 8Muhammad Ichsan PrasetyaNo ratings yet
- Desseauve 2020Document6 pagesDesseauve 2020Raghad MimarNo ratings yet
- Pediatric Inguinal Hernia PDFDocument5 pagesPediatric Inguinal Hernia PDFade-djufrieNo ratings yet
- Gina TH 2017Document5 pagesGina TH 2017kiranNo ratings yet
- 2021 Article 1523Document9 pages2021 Article 1523Pratama RiyadNo ratings yet
- Intra-Articular Injection, Subacromial Injection, and Hydrodilatation For Primary Frozen Shoulder: A Randomized Clinical TrialDocument8 pagesIntra-Articular Injection, Subacromial Injection, and Hydrodilatation For Primary Frozen Shoulder: A Randomized Clinical TrialAbhishek JirelNo ratings yet
- Accuracy and Efficacy of Ultrasound-Guided Pes Anserinus Bursa InjectionDocument6 pagesAccuracy and Efficacy of Ultrasound-Guided Pes Anserinus Bursa Injectionthu hangNo ratings yet
- Meja Operasi Trakea Intubasi 2014Document7 pagesMeja Operasi Trakea Intubasi 2014Davira Azzahra FirjanantiNo ratings yet
- Use of eFAST in Patients With Injury To The Thorax or AbdomenDocument4 pagesUse of eFAST in Patients With Injury To The Thorax or Abdomenalejandro montesNo ratings yet
- Pediatric Anesthesia - 2021 - Luo - Effects of Erector Spinae Plane Block On Postoperative Pain in Children UndergoingDocument10 pagesPediatric Anesthesia - 2021 - Luo - Effects of Erector Spinae Plane Block On Postoperative Pain in Children UndergoingPablo Lukacs CarmonaNo ratings yet
- Aksu 2018Document2 pagesAksu 2018maurinmarceoiaNo ratings yet
- Characteristics of Cervical Position Sense in Subjects With Forward Head PostureDocument3 pagesCharacteristics of Cervical Position Sense in Subjects With Forward Head PostureA AZIZNo ratings yet
- Nuevo Método de Imagen para Evaluar La Biomecánica Del SDocument5 pagesNuevo Método de Imagen para Evaluar La Biomecánica Del SLargo FlacoNo ratings yet
- Lateral Oblique Superior To Lateral View CESI 2015Document14 pagesLateral Oblique Superior To Lateral View CESI 2015Michael HuntNo ratings yet
- Satoshi Dohi, Kiyotake Ichizuka, Ryu Matsuoka, Kohei Seo, Masaaki Nagatsuka, Akihiko SekizawaDocument6 pagesSatoshi Dohi, Kiyotake Ichizuka, Ryu Matsuoka, Kohei Seo, Masaaki Nagatsuka, Akihiko SekizawasandiNo ratings yet
- Out PDFDocument7 pagesOut PDFFayza RihastaraNo ratings yet
- JVP Dan CVPDocument8 pagesJVP Dan CVPHary SanjayaNo ratings yet
- Laryngoscopy and Tracheal Intubation in The Head-Elevated Position in Obese Patients: A Randomized, Controlled, Equivalence TrialDocument51 pagesLaryngoscopy and Tracheal Intubation in The Head-Elevated Position in Obese Patients: A Randomized, Controlled, Equivalence TrialanaeshklNo ratings yet
- Obstetrical Analgesia Word 2Document10 pagesObstetrical Analgesia Word 2Top MusicNo ratings yet
- Intrapartum Ultrasound Assessment of FetDocument8 pagesIntrapartum Ultrasound Assessment of FetXymon ZubietaNo ratings yet
- HSG Vs SonohysterographyDocument4 pagesHSG Vs Sonohysterography#15No ratings yet
- Youssef 2014Document7 pagesYoussef 2014Walter RizzatoNo ratings yet
- e507d2a9-15d1-4ffe-96d4-dccb4188b121Document12 pagese507d2a9-15d1-4ffe-96d4-dccb4188b121Julio AltamiranoNo ratings yet
- Diagnostic Values of Tests For Acromioclavicular Joint PainDocument6 pagesDiagnostic Values of Tests For Acromioclavicular Joint Painarum_negariNo ratings yet
- Ans 12950Document6 pagesAns 12950AYŞE GÜLŞAH ATASEVERNo ratings yet
- Revista Brasileira DE AnestesiologiaDocument7 pagesRevista Brasileira DE AnestesiologiaLuize KrulciferNo ratings yet
- Pre-Induction Translabial Ultrasound Measurements in Predicting Mode of Delivery Compared To Bishop Score: A Cross-Sectional StudyDocument7 pagesPre-Induction Translabial Ultrasound Measurements in Predicting Mode of Delivery Compared To Bishop Score: A Cross-Sectional StudydewiayuNo ratings yet
- Angle of Progression Measurements of Fetal Head at Term, A Systematic Comparison Between Open Magnetic Resonance Imaging and Transperineal UltrasoundDocument5 pagesAngle of Progression Measurements of Fetal Head at Term, A Systematic Comparison Between Open Magnetic Resonance Imaging and Transperineal UltrasoundNella SolanoNo ratings yet
- Propiocepcion Hombro Post CirugiaDocument6 pagesPropiocepcion Hombro Post Cirugiamarcelogascon.oNo ratings yet
- Assessment of Labor Progression by Intrapartum Ultrasonography Among Term Nulliparous WomenDocument5 pagesAssessment of Labor Progression by Intrapartum Ultrasonography Among Term Nulliparous WomenFrancesca Doreen VegaNo ratings yet
- Acup Utk TonsiltektomiDocument7 pagesAcup Utk Tonsiltektominewanda1112No ratings yet
- Minimizing Clearance Issues With Prone Breast Patients On Varian Linear Accelerators Through Isocenter PlacementDocument18 pagesMinimizing Clearance Issues With Prone Breast Patients On Varian Linear Accelerators Through Isocenter Placementapi-484763634No ratings yet
- 455 2014 Article 9580Document10 pages455 2014 Article 9580Ailin Vejar GaticaNo ratings yet
- Anae 12034Document8 pagesAnae 12034Gian Paolo SisonaNo ratings yet
- Vertical Expandable Prosthetic Titanium Rib Device Insertion: Does It Improve Pulmonary Function?Document4 pagesVertical Expandable Prosthetic Titanium Rib Device Insertion: Does It Improve Pulmonary Function?hayputriNo ratings yet
- Shockwave Therapy Plus Eccentric Exercises Versus Isolated Eccentric Exercisesfor Achilles Insertional TendinopathyDocument8 pagesShockwave Therapy Plus Eccentric Exercises Versus Isolated Eccentric Exercisesfor Achilles Insertional TendinopathySergi ArnauNo ratings yet
- The Effects of A Shoulder Roll During LaryngosDocument11 pagesThe Effects of A Shoulder Roll During LaryngospaulaNo ratings yet
- Accepted Manuscript: International Journal of Obstetric AnesthesiaDocument25 pagesAccepted Manuscript: International Journal of Obstetric AnesthesiaLissethe HernandezNo ratings yet
- 1 s2.0 S0165587622001008 MainDocument5 pages1 s2.0 S0165587622001008 MaintesteiroNo ratings yet
- Κουτσουρελάκης ΩΡΛDocument5 pagesΚουτσουρελάκης ΩΡΛΚουτσουρελακης ΩΡΛNo ratings yet
- Surgical Outcomes of Posterior Spinal Fusion Alone Using Cervical Pedicle ScrewDocument26 pagesSurgical Outcomes of Posterior Spinal Fusion Alone Using Cervical Pedicle ScrewprototyposNo ratings yet
- JOurnal Uro 2Document6 pagesJOurnal Uro 2Gladys AilingNo ratings yet
- C12 Comparison of Isometric Force of The Craniocervical Flexor and Extensor Muscles Between Women With and Without Forward Head PostureDocument6 pagesC12 Comparison of Isometric Force of The Craniocervical Flexor and Extensor Muscles Between Women With and Without Forward Head PostureChing HoNo ratings yet
- Research Article: Isolated Male Epispadias: Anatomic Functional Restoration Is The Primary GoalDocument4 pagesResearch Article: Isolated Male Epispadias: Anatomic Functional Restoration Is The Primary GoalsatriamarrantizaNo ratings yet
- Transvaginal Ultrasonography For Cervical Assessment For Induction of LaborDocument8 pagesTransvaginal Ultrasonography For Cervical Assessment For Induction of LaborGunther MirandaNo ratings yet
- 245-Article Text-456-1-10-20190606Document6 pages245-Article Text-456-1-10-20190606Oana RuxandraNo ratings yet
- Occlusal and Skeletal Effects of An Oral Appliance in The Treatment of Obstructive Sleep ApneaDocument7 pagesOcclusal and Skeletal Effects of An Oral Appliance in The Treatment of Obstructive Sleep Apnea陈延珑No ratings yet
- Ecg 1Document5 pagesEcg 1Hêny CarlênicNo ratings yet
- Quantitative Assessment of Inferior Oblique Muscle Overaction Using Photographs of The Cardinal Positions of GazeDocument9 pagesQuantitative Assessment of Inferior Oblique Muscle Overaction Using Photographs of The Cardinal Positions of GazenysNo ratings yet
- Son 2016Document4 pagesSon 2016Zaki RiciNo ratings yet
- 2010 Nihms Eus-UsDocument19 pages2010 Nihms Eus-UsVlad IchimNo ratings yet
- Primary Total Shoulder Arthroplasty Performed Entirely Thru The Rotator Interval - Technique and Minimum Two-Year OutcomesDocument10 pagesPrimary Total Shoulder Arthroplasty Performed Entirely Thru The Rotator Interval - Technique and Minimum Two-Year OutcomesmotohumeresNo ratings yet
- TAP Paper PublishedDocument8 pagesTAP Paper PublishedMotaz AbusabaaNo ratings yet
- Generative Shape DesignDocument195 pagesGenerative Shape DesignAdi Fiera100% (1)
- Statistics and Probability Module 3Document3 pagesStatistics and Probability Module 3Eftychia LeegleeNo ratings yet
- Guidelines For The Management of Brain InjuryDocument26 pagesGuidelines For The Management of Brain InjuryfathaNo ratings yet
- 40 RT-flex Control-System Rev01Document68 pages40 RT-flex Control-System Rev01Mayvon Botelho100% (2)
- Electrical Power System Device Function NumberDocument2 pagesElectrical Power System Device Function Numberdan_teegardenNo ratings yet
- ASCE Snow Loads On Solar-Paneled RoofsDocument61 pagesASCE Snow Loads On Solar-Paneled RoofsBen100% (1)
- Pref - 2 - Grammar 1.2 - Revisión Del IntentoDocument2 pagesPref - 2 - Grammar 1.2 - Revisión Del IntentoJuan M. Suarez ArevaloNo ratings yet
- Spectroscopy (L-26 To 29)Document81 pagesSpectroscopy (L-26 To 29)Vashistha GargNo ratings yet
- ZhentarimDocument4 pagesZhentarimLeonartNo ratings yet
- Efficient Rice Based Cropping SystemDocument24 pagesEfficient Rice Based Cropping Systemsenthilnathan100% (1)
- Binet Kamat Test For General Mental AbilitiesDocument54 pagesBinet Kamat Test For General Mental AbilitiesSana Siddiq100% (14)
- SP 73Document105 pagesSP 73Rodrigo Vilanova100% (3)
- Adaptive Cruise ControlDocument5 pagesAdaptive Cruise ControlIJIRSTNo ratings yet
- Method Statement For Cable Trays & Cable Ladders InstallationDocument7 pagesMethod Statement For Cable Trays & Cable Ladders InstallationJamal Budeiri0% (1)
- Chemistry Notes: SUBJECT: Leaving Cert Chemistry Level: TEACHER: Tara LyonsDocument5 pagesChemistry Notes: SUBJECT: Leaving Cert Chemistry Level: TEACHER: Tara LyonsSevinc NuriyevaNo ratings yet
- Cac de Luyen ThiDocument18 pagesCac de Luyen ThiVinh Dao CongNo ratings yet
- Leadership Games and ActivitiesDocument38 pagesLeadership Games and ActivitiesWilliam Oliss100% (1)
- Abnormalities of Placenta, Amniotic Fluid and Cord: Prepared By, B. Ezhilarasi, Nursing TutorDocument21 pagesAbnormalities of Placenta, Amniotic Fluid and Cord: Prepared By, B. Ezhilarasi, Nursing TutorGopala KrishnanNo ratings yet
- LJ-V7080 DatasheetDocument2 pagesLJ-V7080 DatasheetOrhan DenizliNo ratings yet
- Killer Kohler Part I IDocument17 pagesKiller Kohler Part I Irusyn100% (1)
- Propert 447-445Document11 pagesPropert 447-445LUNA100% (1)
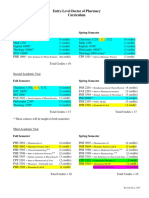
- Pharmd CurriculumDocument18 pagesPharmd Curriculum5377773No ratings yet
- 1.1 The Prescription of Blood ComponentsDocument9 pages1.1 The Prescription of Blood ComponentsagurtovicNo ratings yet
- Ii 2015 1Document266 pagesIi 2015 1tuni santeNo ratings yet
- BS746 2014Document22 pagesBS746 2014marco SimonelliNo ratings yet
- Five Star Hotel and ResortDocument9 pagesFive Star Hotel and ResortAISHNo ratings yet
- Upaam 1135891 202105060749199700Document18 pagesUpaam 1135891 202105060749199700Kartik KapoorNo ratings yet
- Bio (RocessDocument14 pagesBio (RocessVijay SansanwalNo ratings yet
- 1ST SUMMATIVE TEST FOR G10finalDocument2 pages1ST SUMMATIVE TEST FOR G10finalcherish austriaNo ratings yet
- The Dry Bulk Management StandardDocument18 pagesThe Dry Bulk Management Standardamu_more44100% (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (24)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (58)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingFrom EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingRating: 4 out of 5 stars4/5 (1138)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsFrom EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsRating: 4.5 out of 5 stars4.5/5 (6)