Professional Documents
Culture Documents
JMWatt Consulting Firm's Report To TOMA On The Proposed MD School at UNTHSC
Uploaded by
Tây SơnOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
JMWatt Consulting Firm's Report To TOMA On The Proposed MD School at UNTHSC
Uploaded by
Tây SơnCopyright:
Available Formats
JMWatt Consulting
JMWatt Consulting Phone (415) 499-7619
1178 Idylberry Road FAX (415) 499-8769
San Rafael, CA 94903 Mobile (415) 987-3210
Report to the Texas
Osteopathic Medical
Association
Development of an Allopathic Medical School
at the
University of North Texas
Health Science Center
February 7, 2011
David F. Altman, MD, MBA
J. Michael Watt, MBA
JMWatt Consulting ● Altman
REPORT TO THE TEXAS OSTEOPATHIC MEDICAL
ASSOCIATION ON DEVELOPMENT OF AN ALLOPATHIC
MEDICAL SCHOOL AT THE UNIVERSITY OF
NORTH TEXAS HEALTH SCIENCE CENTER
Executive Summary
At the request of the Texas Osteopathic Medical Association (TOMA), we have reviewed
The “Academic and Business Plan for the Development of a Proposed MD Program”
(“the Plan”) that the Regents of the University of North Texas (UNT) approved in
October 2010 to develop a new school of allopathic medicine (UNTMD) in Fort Worth.
This Plan was said to be in response to a growing perception that there is a looming crisis
in the availability of physicians, particularly in primary care. In addition, and perhaps
paradoxically in view of the primary care crisis, it is based on the idea that there would be
advantages, both for residency training programs now being developed by local hospitals
and for clinical practice in general, for there to be an expansion of allopathically trained
graduates instead of a further increase in the number of osteopathic-trained graduates
through the Texas College of Osteopathic Medicine (TCOM). Allopathic graduates are
more likely to pursue residency training in one of the specialties of medicine, while
TCOM graduates have a greater orientation toward primary care.
On review of the Plan, several issues have been recognized:
The shortage of physicians, both locally and nationally, will not be resolved
rapidly by training more medical students. A more immediate solution would be
to develop additional graduate medical education (GME) positions, which is
where the “bottleneck” in the training pipeline is most acute. This is especially
true in Texas, where there are more medical school graduates today than there are
entry-level residency training positions, thus forcing Texas medical school
graduates to leave the state for residency training and reducing the likelihood that
they will return to Texas for their medical careers. In addition, TCOM is a highly
regarded school, turning out students who acquit themselves well in osteopathic
and allopathic residencies and on the licensing examinations and most of whom
embark on careers in Texas.
The Plan’s program and timeline appear to have been given considerable thought,
with attention paid to accreditation requirements and processes. However, it
appears to us highly unlikely that a UNTMD program could bring all of the pieces
together to achieve accreditation and recruit and select students so that a first-year
class could commence medical studies in 2013. For example, early recruitment of
senior leadership is critical. Unless all are internal candidates, recruitment will be
time-consuming, likely more than allowed in UNTMD’s aggressive timetable. If
the senior leadership are internal candidates, however, their transfer to UNTMD
will impact the existing programs of UNTHSC and TCOM.
JMWatt Consulting ● Altman
Report to TOMA: Development of an Allopathic Medical School at UNTHSC February 7, 2011
The Plan’s financial projections also present a highly optimistic view of the
economies that can be achieved by establishing a new school on UNTHSC’s
existing campus. Faculty and administrative costs may be underestimated and the
projections assume that existing UNT staff will take on significantly more
responsibility at no direct cost to UNTMD. State per capita support and tuition
revenues are projected to provide nearly $11 million to support the proposed
school’s $16.8 million in direct operating cost in the first two years of the
program, but are dependent on recruiting the full maximum class of 100 students
in the first year – unusual and extremely difficult given the projected timing of
accreditation and infrastructure development. Over the first eight years of
UNTMD’s operation, the Plan projects it will require and receive State payments
of $105.8 million. Further, the pledges made by hospitals toward starting a new
school may be tenuous, given the deficits in federal and state budgets that finance
Medicare and Medicaid, two major sources of hospital funds. Finally, while
building a new school on an established campus can yield some economies, the
track record of other medical schools that have been recently developed indicates
that their costs have been in the range of four times the amount set forth in the
plan for UNTMD.
Commitments to maintain the integrity of TCOM as the new allopathic school
develops are part of the Plan. However, while initial commitments were made to
obtain support for the Plan from the osteopathic profession, both the American
Osteopathic Association and TOMA passed resolutions in opposition prior to the
UNT Regents’ consideration of the proposal in August 2010. The enforceability
of the promises made concerning TCOM is unclear at best, and regardless of the
effort to ensure cooperation between the schools there inevitably will be
competition for existing and potential new resources between TCOM and a new
allopathic school that will only be heightened if the initial projections for
UNTMD prove, as we expect, to be overly optimistic.
Given these realities, our recommendation would be for TOMA not to endorse the
proposed new medical school. Instead we would advise working with the local and state-
wide leadership in medical education to develop new or expanded programs at the GME
level, which is the priority identified by the Texas Higher Education Coordinating Board
(THECB) and the Texas Medical Education and Physician Workforce Consensus Group.
For GME expansion, an MD-granting medical school is not required. Providing more
opportunities for the medical students already graduating from Texas medical schools
(educated in part at State expense) to stay in the Metroplex for their residencies will
achieve more directly and quickly the benefits the UNTMD Plan seeks to achieve.
JMWatt Consulting ● Altman ii
REPORT TO THE TEXAS OSTEOPATHIC MEDICAL
ASSOCIATION ON DEVELOPMENT OF AN ALLOPATHIC
MEDICAL SCHOOL AT THE UNIVERSITY OF
NORTH TEXAS HEALTH SCIENCE CENTER
Background and Questions for this Review
The Texas College of Osteopathic Medicine (TCOM) is a well-established and highly
regarded osteopathic medical school in Fort Worth. It is accredited by the Commission on
Osteopathic College Accreditation (COCA), the organization recognized by the U.S.
Department of Education for accreditation of osteopathic medical education programs,
and is a part of the University of North Texas Health Science Center (UNTHSC). Its
programs have educated many of the primary care practitioners in the Fort Worth area
and beyond. Given the growing awareness of a physician shortage, especially in the
primary care and generalist disciplines, UNT’s and TCOM’s strategic goals over the next
several years include expanding TCOM’s enrollment to 230 students per year. There also
has been discussion over the past several years about whether there is a further need to
develop an allopathic medical school in Fort Worth and whether such a development
would have advantages for UNT, area providers, and the Fort Worth community more
generally. Leaders at UNT and in the Fort Worth community have developed a proposal
for creating a separate new allopathic medical school – “UNTMD” – to educate an
additional 100 students per year beginning in 2013 in conjunction with and running
parallel to TCOM.
The “Academic and Business Plan for the Development of a Proposed MD Program”
(“the Plan”) has been approved by the UNT Regents for further development and
implementation 1 but requires a range of approvals and actions before moving forward. In
particular, the Plan is built around the elements necessary for accreditation by the Liaison
Committee for Medical Education (LCME). This organization, jointly managed by the
American Medical Association (AMA) and the Association of American Medical
Colleges (AAMC), establishes strict standards for the curriculum, facilities, faculty, and
finances that are the infrastructure for allopathic medical education programs. More
generally, the Plan describes elements of distinctiveness of the proposed UNTMD
program as a rationale for developing a separate allopathic medical school within a
general framework of maximizing sharing of faculty, facilities, and infrastructure on the
UNTHSC campus to reduce the costs of developing and operating the proposed school.
The tension between the argument for the distinctiveness of the proposed school and the
plans for maximum sharing of resources is evident throughout the Plan: If UNTMD is
developed to be distinctive and meet the LCME’s accreditation requirements, can it meet
the goals for development speed and budget frugality it has set without prejudice to
1
Action at the UNT Regents meeting of August 19, 2010.
JMWatt Consulting ● Altman
Report to TOMA: Development of an Allopathic Medical School at UNTHSC February 7, 2011
TCOM? If it meets its goals for development speed and budget frugality, can it achieve
its goals for distinctiveness, which are important to its rationale for why it should be
developed as a parallel school, for recruiting faculty and students, and for meeting
accreditation requirements?
This Report
This report examines UNT’s Plan, focusing on two distinct but overlapping sets of issues:
1. The adequacy of the planned organization, facilities, faculty, and curriculum of
the new allopathic school and its development timeline, especially in comparison
to the accreditation standards established by the LCME; and
2. Financial projections for the development, start-up, and operation of a new school
of medicine, in light of UNT’s business plan, the opportunities and difficulties of
sharing resources, and the very recent experience in Texas and elsewhere with the
development of several new medical schools.
In preparing it, we have reviewed the Plan and accompanying August 2010 “High-Level
Costing Model” in depth in light of our collective 50 years of experience 2 in developing
and implementing plans for undergraduate and graduate medical education programs in
Texas, California, and at the national level as well as in conducting accreditation reviews.
We also have interviewed knowledgeable individuals from the DFW Metroplex and
beyond, most of whom were at least somewhat familiar with the UNTMD plan.
After a brief summary of trends in allopathic and osteopathic medical education
nationally and in Texas and the LCME accreditation process that provide a context for
UNTHSC’s Plan, we discuss key elements of the academic program, facilities, and
financial elements of the Plan.
Medical Education in Texas
Medical Schools in the United States, Allopathic and Osteopathic
There currently are 133 accredited allopathic medical schools awarding the M.D. degree
in the United States, including seven that are “in development” having been granted
“Preliminary Accreditation” status. (See further discussion in the section on LCME
below.) They are in 45 states and in Puerto Rico. Texas has eight schools, including the
Paul Foster School at Texas Tech University in El Paso, which is on Preliminary
Accreditation status. Seven other schools nationally, but none in Texas, are in the initial
“Applicant” status in the accreditation process. One additional school is a “Candidate”
school – the stage preceding Preliminary Accreditation.
2
See author biographies, Appendix A.
JMWatt Consulting ● Altman 2
Report to TOMA: Development of an Allopathic Medical School at UNTHSC February 7, 2011
There currently are 26 colleges of osteopathic medicine awarding the D.O. degree,
offering instruction at 34 locations in 25 states. The University of North Texas Health
Science Center Texas College of Osteopathic Medicine in Fort Worth is the only
osteopathic medical school in the State.
As discussed in the UNTMD Plan, with the current perception that there either is or will
be a shortage of physicians in the U.S., particularly those in the generalist or primary care
disciplines, there has been pressure to increase enrollment in medical schools, both by
expanding class size in existing schools and by expanding the number of schools. The
Association of American Medical Colleges (AAMC), for example, has called for a 30%
increase in the number of graduates (currently around 16,000 per year in the U.S. from
allopathic schools) by 2020, and the American Association of Osteopathic Colleges of
Medicine (AACOM) projects a roughly parallel growth in number of graduates, which
given the smaller number of osteopathic than allopathic schools yields a significantly
higher rate of growth.
Several challenges stand between achieving this growth in medical school enrollment and
achieving its intended effects. One challenge is to orient students toward primary care, as
only about 25% of allopathic medical school graduates wind up in these disciplines after
finishing their training. It would seem paradoxical that the Plan actually calls for students
from UNTMD to follow the example of MD graduates elsewhere and favor training in
one of the subspecialty services, not primary care, which is where the shortage is most
acute. A recently reported study showed that Texas in 2008 had the second lowest ratio of
primary care providers to population in the nation – 30% lower than the average of the 50
states. 3 A second challenge is to induce these graduates to practice in currently
underserved areas – most of them rural or inner city communities. Third, and underlying
the previous two, is the tremendous debt load with which students graduate, not
uncommonly exceeding $200,000. Fourth, and most pressing in Texas, is the limited
number of residency positions available to medical school graduates, which has not been
increasing commensurate with the increasing number of graduating medical students and
is limited by caps on federal support for graduate medical education. (See below.)
There has been growing convergence between allopathic and osteopathic medical
education, so that the educational programs are looking increasingly similar. For
example, research expansion has been an important priority at TCOM. Allopathic and
osteopathic graduates are accepted into residency programs, research grants are available
to both, and public and private insurance plans make no distinction between physicians
who are graduates of osteopathic versus allopathic medical schools. A distinct philosophy
of medicine is at osteopathy’s roots, one that emphasizes care for the whole individual in
his/her social environment and other elements particularly important in primary care, as
well as the techniques of osteopathic manipulation. While calls for further coming
together have been published in medical journals including Academic Medicine
3
Leighton Ku, et.al., “The States’ Next Challenge – Securing Primary Care for Expanded
Medicaid Populations.” New England Journal of Medicine Online First, 10.1056/NEJMp1011623
downloaded from nejm.org January 27, 2011, Table A.1
JMWatt Consulting ● Altman 3
Report to TOMA: Development of an Allopathic Medical School at UNTHSC February 7, 2011
(published by the AAMC), differences between the two modes of education have been
cited, including by the leadership both of the LCME and the osteopathic profession, as
reasons to maintain parallel tracks.
The LCME Accreditation Process
Accreditation of allopathic medical schools in the United States is under authority
granted by the U.S. Department of Education to the Liaison Committee on Medical
Education (LCME). The LCME is an organization jointly managed by the American
Medical Association and the Association of American Medical Colleges. Each of those
organizations appoints a senior staff person as Secretary of the LCME, and the Secretariat
alternates each year between the two LCME Secretaries.
The LCME publishes the standards for medical school accreditation as The Structure and
Functions of a Medical School, a well-organized document but one that is also
challenging to understand and interpret. However, the LCME Secretaries in general are
very helpful both to established and proposed schools in interpreting the intent of the
standards. The standards also undergo regular review and revision.
The LCME emphasizes that it accredits “programs," not schools. In reading through the
documents, it is clear that the principal intent is for there to be a well-designed and well-
executed program that supports student education in a scholarly environment.
A separate document issued by the LCME, Guidelines for New and Developing Medical
Schools, outlines the standards and process for starting a new school of medicine. New
schools face challenging standards that must be in place prior to the initial application for
accreditation. Personnel and agreements must be in place and initial documentation
submitted for a proposed school to move from Applicant to Candidate status. Under the
LCME standards, new schools may not advertise for applicants in any manner while in
either Applicant or Candidate status. Moving from Candidate to Preliminary
Accreditation status requires submission of extensive documentation of the program’s
infrastructure and curricular plans, the so-called Self Study, followed by a site visit
scheduled according to LCME’s calendar. The LCME holds two-day meetings three
times a year, usually in October, February, and June, to make decisions concerning
accreditation and re-accreditation. The information gathered through the self-study and
site visit is reviewed by the LCME and Preliminary Accreditation possibly granted. Only
then may a first class of students be recruited, selected, and matriculate – a process that
itself requires nearly a year after the LCME grants Preliminary Accreditation. A second
set of detailed materials, site visit, and LCME action is required at the mid-point of the
charter class’ second year in order to continue Preliminary Accreditation and allow the
students to continue into the clinical years of their MD training. Programs subsequently
are reviewed at the time that the first class enters their fourth year, and if the program is
deemed worthy the LCME grants full accreditation.
JMWatt Consulting ● Altman 4
Report to TOMA: Development of an Allopathic Medical School at UNTHSC February 7, 2011
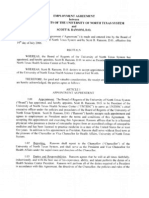
A chart comparing the LCME standards, based on the most recent (2010) revision of the
Structure and Functions document, with the UNTMD Plan for its medical school is
included as Appendix B. Exhibit 1 highlights those requirements that would be especially
challenging to complete in the short time frame suggested in the Plan.
Exhibit 1
MAJOR LCME REQUIREMENTS NOT ADDRESSED IN THE UNTMD PLAN
LCME
Section Requirement Comment
IS-8 Appointment of the This cannot officially begin prior to legislative approval of the
medical school dean MD program. Recruiting someone, especially if from the
outside, may take six months or more.
IS-11 Appointment of Also likely to take significant time -- after the dean is in place.
Associate Deans, Dept. Also, recruitment of academic leaders and senior faculty can
be very expensive.
Chairs, etc.
IS-12 Establish clinical While not required with the initial class, the time needed for
settings with GME and new GME program approval may be up to two years.
CME
ED-1 Faculty defines overall This must be the role of the UNTMD faculty (recruited and
objectives for the appointed after the Dean and other UNTMD academic
leaders), not the TCOM faculty.
educational program
ED-24 Residents must be Not required with the initial class, but of critical importance.
familiar with educational The UNTMD academic program as outlined depends
heavily on new residency programs, leaving much doubt
objectives and prepared about the rapidity of realizing it.
as teachers
MS-23 Effective financial aid Not clear where this will “live.” Assigned to Director of
and debt management Financial Aid but this position is not budgeted for the initial
application year.
counseling
FA-2 Sufficient numbers of See notes for IS-11 above. The Plan for clinical education
faculty to meet the depends heavily on part-time community faculty physicians
whose commitment to UNTMD is not documented in the
needs of the educational Plan and an unknown proportion of whom currently may
program have responsibilities educating TCOM students.
ER-2 Adequate present and As noted elsewhere, there are questions about the adequacy
anticipated financial of the financial models presented.
resources
ER-6 Appropriate resources The plan depends on using both existing and new hospital
for clinical instruction settings with existing or new residency programs. There is
already a mismatch between the number of medical school
graduates and entry GME positions in Texas, which would
be made worse by adding of UNTMD.
As can be seen, numerous essential activities must take place prior to the development of an
application for preliminary accreditation that are not addressed in the Plan or will require significant
time to undertake if the Legislature gives UNT authority to develop UNTMD. The appointment of
JMWatt Consulting ● Altman 5
Report to TOMA: Development of an Allopathic Medical School at UNTHSC February 7, 2011
a medical school dean, especially from outside of UNT and especially if the candidate is a savvy
negotiator, could take months to complete. The development of clinical sites, with respect to
facilities, clinical teachers and residents, is another major challenge given the timeline necessary for
development and accreditation of a GME program where none exists today as well as the
contemporary pressures placed on medical faculty in the clinical departments that necessarily limit
their commitment to medical education.
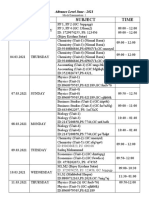
Schools in Development, and the LCME Accreditation Timetable
Moving from Applicant to Candidate to Preliminary Accreditation status has been a
lengthy process for most schools currently in development, as shown in Exhibit 2.
Exhibit 2
Medical School Development Proposals in the LCME Accreditation Pipeline 2008-10
Applicant Institution Location June 2008 January 2010 October 2010
Scripps SoM La Jolla, CA Applicant School Withdrawn?? Withdrawn*
Oakland University William Beaumont SoM Rochester, MI Applicant School Candidate School Preliminary Accreditation
Touro University CoM Hackensack, NJ Applicant School Applicant School Withdrawn**
Hofstra University SoM Hempstead, NY Applicant School Applicant School Preliminary Accreditation
Virginia Tech Carilion SoM Roanoke, VA Applicant School Preliminary Accreditation Preliminary Accreditation
The Commonwealth Medical College Scranton, PA Candidate School Preliminary Accreditation Preliminary Accreditation
Florida International University CoM Miami, FL Preliminary Accreditation Preliminary Accreditation Preliminary Accreditation
University of Central Florida CoM Orlando, FL Preliminary Accreditation Preliminary Accreditation Preliminary Accreditation
Paul L. Foster SoM - Texas Tech University El Paso, TX Preliminary Accreditation Preliminary Accreditation Preliminary Accreditation
Thunder Bay / To be surveyed 2011-12 for To be surveyed 2011-12 for
Northern Ontario SoM Sudbury, ONT Provisional Accreditation Full Accreditation Full Accreditation
University of California, Riverside SoM Riverside, CA Applicant School Applicant School
Central Michigan University SoM Mount Pleasant, MI Applicant School Applicant School***
Cooper Medical School of Rowan University Camden, NJ Applicant School Applicant School
Quinnipiac University SoM North Haven, CT Applicant School
Palm Beach Medical College Palm Beach, FL Applicant School
Western Michigan University SoM Kalamazoo, MI Applicant School
University of South Carolina SOM, Greenville Greenville, SC Applicant School
Florida Atlantic University CoM Boca Raton, FL Candidate School
* December 2010: The Scripps Research Institute will affiliate with Florida Atlantic University's Medical School, which has separated from University of Miami
** Touro College now completing affiliation with New York Medical College; Touro will appoint NYMC Board of Trustees.
*** Central Michigan University press release, 12-15-2010 (Not yet shown on LCME website
Sources: LCME and Institution websites.
Site visits are a central part of the accreditation process; they require the LCME to
assemble accreditation staff from a range of disciplines. In many cases site visit
scheduling has required from three to six months’ lead time following submission and
review of the required self-study material. Additional time is required for the visitors to
develop and agree on their report, for the Secretariat to review it and schedule its review
by the full LCME, and for the LCME to grant the approval.
As noted in UNT’s Plan, in Texas two factors beyond the LCME timing affect its ability
to achieve the timetable it has set for developing UNTMD and matriculating a first class
of 100 students in August 2013.
The first is critical to the beginning of the process. The University of North Texas Board
of Regents currently is prohibited in Texas state law from offering programs leading to
JMWatt Consulting ● Altman 6
Report to TOMA: Development of an Allopathic Medical School at UNTHSC February 7, 2011
the MD degree. Providing that authority will require an act by the Texas Legislature
during its current session, before May 2011. The Texas Higher Education Coordinating
Board (THECB) would be requested to comment on the proposed bill as a part of the
legislative process. THECB’s analyses show that development of additional residency
programs and positions would be the most important actions for increasing the supply of
new physicians practicing in Texas. A two-thirds legislative majority is required for laws
to take effect immediately on the Governor’s signature; otherwise they become effective
90 days later or on the first day of September. As of the date of this report, no legislation
had been introduced to remove the prohibition, and THECB has not been requested for
comment.
The second factor is the timetable for applications to medical schools in Texas through
the Texas Medical and Dental Schools Application Service (TMDSAS), in which all
Texas medical schools participate. The process begins in May of the year before the year
in which applicants are accepted and matriculate. For UNTMD to participate fully in the
TMDSAS process and matriculate students in August 2013, it would need approval to
recruit its first class before May of 2012 – not possible according to the LCME timetable
as described above and in the Plan. As projected in the Plan, a June LCME approval
would require a special TMDSAS alert to students who already may have begun the
application process, who could revise their applications to include UNTMD. Due to the
LCME’s prohibition of any recruitment of students before the accreditation decision,
however, UNTMD would have little time to advertise widely information about the new
school or do any outreach for that purpose. For any later LCME approval, UNTMD
would need to follow a separate application process. Time for candidate interviews would
be tightly compressed. While possible, in either case the timing of the application process
would make it very difficult for UNTMD to matriculate a first class of 100 from among
the most highly qualified candidates.
Summary Observations and Conclusions – Medical Education, the Plan, and LCME Accreditation
The LCME accreditation process is long and tortuous. It is not possible to accelerate
it, and patience and great attention to detail is required.
Much of the program leadership has to be in place before an application for
accreditation can be submitted. This includes the Dean, senior staff, and core faculty.
Unless all are internal candidates, recruitment is likely to be time-consuming, perhaps
more than allowed in UNTMD’s aggressive timetable, and more expensive than
planned. If the senior leadership are internal candidates, their transfer to UNTMD will
impact the existing programs of UNTHSC and TCOM.
Much thought has gone into the UNTMD proposal, and it is likely that the planners
have received some advice and guidance from the LCME. However, as shown in
Exhibit 1 and Appendix B, much work needs to be done to bring the plans to the point
that they can be submitted as an application for Preliminary Accreditation. Given the
history of other schools in development, submitting the application within six months
of the arrival of a dean is highly aggressive, and the lead times for LCME action to
JMWatt Consulting ● Altman 7
Report to TOMA: Development of an Allopathic Medical School at UNTHSC February 7, 2011
review the material and grant the initial site visit and then to act on the site visit report
and grant Preliminary Accreditation also are compressed. To achieve all of this so
that a new class can matriculate in the fall of 2013 would seem highly unlikely.
Medical Schools and GME
Graduate Medical Education (GME) is the training that takes place after graduation from
medical school and that focuses on clinical training in one of the specialties of medicine.
This is also known as residency and fellowship training, and it lasts from three to seven
years. The Accreditation Council for Graduate Medical Education (ACGME) accredits
allopathic GME programs; osteopathic internships and residencies are accredited by the
American Osteopathic Association (AOA). Some programs, including ones in Fort
Worth, are dually accredited, and ACGME-accredited programs are open to osteopathic
medical graduates.
GME programs generally are sponsored by hospitals or health systems, and residents
serve in both inpatient and outpatient settings. GME is largely financed by hospital
revenues, which are supplemented and largely underwritten by payments from the federal
Medicare program. Medicare spent approximately $11 billion in 2010 under specific
programs that support GME activities in residencies accredited by either the ACGME or
AOA. Historically, Medicaid programs also contributed to the support of GME as part of
their payments for patient care. However, Texas eliminated GME funding through its
Medicaid program several years ago. In addition, in recent years there has been a cap on
how many positions the Medicare program will support, and new GME programs or
positions have been difficult if not impossible to fund in this way.
Both the ACGME and the LCME cite the requirement in their standards that residents
serve as teachers. The LCME specifically requires that students have a component of
their education and training in the presence of residents.
In Texas, there are more medical school graduates than first year residency positions. In
2010 there were 1,404 graduates of the State’s medical schools (including TCOM) and
1,390 entry-level residency positions. The Texas Higher Education Coordinating Board
(THECB), the Medical Education and Physician Workforce Consensus Group (in which
TCOM and the other medical schools in Texas participated) and other groups have
documented this situation and the costs and loss of direct benefits that result, and have
recommended expansion of GME as the highest medical education priority in the State.
As one medical school leader told us, “We are losing our medical school graduates to
California” – after state funds have contributed about $200,000 to the education of each
student who must go out of state for residency. This poses significant problems for
Texas, since residency location is a stronger predictor of where physicians wind up in
practice than either their state of origin or the location of their medical school training. A
shortage of physicians in a state or region will not be solved rapidly by the creation of a
new medical school, the entering class of which will enter practice no earlier than seven
years later. Developing residency programs to allow graduates of existing medical
JMWatt Consulting ● Altman 8
Report to TOMA: Development of an Allopathic Medical School at UNTHSC February 7, 2011
schools to stay in state and attracting medical school graduates from other states has a
quicker “payoff.”
Summary Observations and Conclusions – The Plan and Texas’ Need for GME
GME is an essential ingredient in the stew that is a medical school. The current hospital
sites used by TCOM for medical student clinical education and that have residency
programs may not be able or willing to take on a substantial increment of allopathic
medical students. As one hospital’s GME official told us, “If we have to take more
medical students for clerkship rotations, we will have to cut back the number of students
we train in other areas.” In addition, the sites mentioned in the Plan that currently are
expressing interest in new GME programs may well get cold feet due to both the
challenge of obtaining accreditation and the uncertainty, to say the least, of receiving any
public funding for the significant costs they would incur in sponsoring and operating
GME programs.
Additionally, the Plan seems to contain a logic that is difficult to understand: that there is
currently a challenge in obtaining residency positions for TCOM graduates, and therefore
there is a need for more GME positions in the region, but the development of GME
programs by hospitals can only happen if there is an MD-granting school as their
academic partner. First, there is no basis in the standards of accreditation or otherwise
for this last assertion. Second, from the comments we heard from hospital leaders, the
decisions by these hospitals concerning their development of new or expanded residency
programs would appear only loosely linked to the development of UNTMD.
Finally, if the “problem to be solved” by development of UNTMD is Texas’ need for
physicians, development of GME programs rather than development of a second medical
school in Fort Worth would appear to be the near-term priority.
JMWatt Consulting ● Altman 9
Report to TOMA: Development of an Allopathic Medical School at UNTHSC February 7, 2011
The UNT Plan for UNTMD
Academic Program
The plan set forth in the program description addresses both the basic science and the
clinical portion of the medical school curriculum, although the document provides greater
detail for some critical aspects of the program than others. Some highlights include the
following:
Faculty are to be shared in the two schools. The proposed allopathic medical school for
the University of North Texas (UNTMD) is basing much of its program on maintaining
very close ties with the osteopathic medical school that already exists and with the
Graduate School of Biological Sciences, whose faculty now provide basic science
instruction for TCOM students. Specifically, the academic program that we have seen
documented indicates that "to every extent possible the DO and MD schools should
utilize the same organizational structure and personnel…" This includes faculty and
administrators, and even a Joint Curriculum Committee (not apparently with final
approval authority).
The Plan calls for a "single medical faculty" for the two schools. Yet there also would be
separate Promotions and Tenure committees, separate faculty by-laws, and other
structures. For the basic science faculty the plan looks for "economies of scale" in
combining the faculty. Meanwhile the Plan calls for the addition of 12 FTE (estimated at
about 28 new faculty members, many of them part-time) to accommodate the increased
teaching demands from medical student education. Clinical faculty will initially be
hospital- and community-based. Approximately 14 new FTE will be approved (70
individual faculty with partial support) across the disciplines. However, the mechanics of
allocation of the FTEs to departments, both clinical and basic science, is not apparent.
The clinical faculty plan does not specify whether the additional clinical faculty would be
a mix of physicians new to teaching who would need training on educational methods
and evaluation, versus additional time for current TCOM faculty members, which would
likely take away time from their clinical practices and potentially from their availability
to TCOM students. While the Plan presents evidence of interest from hospitals, it does
not have a parallel section documenting the willingness of community physicians to teach
in the UNTMD program.
Curriculum. TCOM's Problem-Focused Curriculum is proposed to serve as the model -
first year students will receive the bulk of direct teaching in a large-group format. The
Plan suggests that "economies of scale" can be gained by combining the DO and MD
students.
The "Problem Focused Application" module will be core. This follows the Problem-
Focused Curriculum and involves case presentations and analysis and is done in small
groups. While this teaching is the same for MD and DO students, its class-size limitations
lead to requiring more faculty participation. In the DO program, small group discussion
JMWatt Consulting ● Altman 10
Report to TOMA: Development of an Allopathic Medical School at UNTHSC February 7, 2011
sessions supplement the large-group lectures. No similar provision is made in the Plan
for additional MD or PhD faculty to lead similar sessions for the MD students.
The pledge that UNT has made that TCOM and UNTMD students would receive clinical
training in the same settings through a common faculty also could raise dilemmas for
individual faculty members: to the extent that the curricular goals and student evaluation
requirements of UNTMD differ from those of TCOM, individual faculty may be pulled in
two ways in providing clinical instruction. On the other hand, if the curricular goals and
evaluation schemas are identical between UNTMD and TCOM, the distinctiveness and
need for UNTMD is less clear.
Research. There are suggestions throughout the proposal that there will be curricular
offerings, especially in the basic sciences, which will advance a research emphasis for
medical students, and that this will be a distinguishing characteristic of UNTMD versus
TCOM. The specifics on how this would be done are not provided. In addition, a research
faculty is required if there is to be credible mentoring of medical students with research
interests. Research faculty depend largely on extramural, i.e. grant, support, with the
National Institutes of Health (NIH) being the most recognized and honored source of
such funds. Extramural support can be elusive, and it is very difficult for institutions to
compete with institutions like Johns Hopkins and UT Southwestern that are already well
funded, but UNTHSC has doubled its research revenues in the last several years from a
variety of sources and operates the nation’s only federally funded center for osteopathic
research. An ambition to grow research programs exists, but the financial plan set forth
in the UNTMD proposal includes no faculty positions fully dedicated to research (versus
teaching) and little of the required infrastructure for a sustained research enterprise.
UNTHSC has submitted a legislative appropriation request (LAR) for funding
development of a research building on the UNTHSC campus in the upcoming biennium,
but does not stipulate that the request is contingent on approval of development of
UNTMD. If the request has been sized based on the projected needs of TCOM and
Graduate School of Biological Sciences faculty, if UNTMD is approved the proposed
building either will need to be expanded, or the expansion plans of existing UNTHSC
units will be constrained by recruitment of UNTMD researchers.
Information Sciences. "Informatics" is an area given special attention in the Plan and
would be taught via the library with limited additional staff.
Clinical Training. Clinical training also calls for joint activities between the two schools.
There is heavy dependency on hospitals to provide clinical training for students and to
provide the faculty for that training. There remains a need to develop a formal curriculum
for the "core" clinical areas (family medicine, internal medicine, pediatrics, surgery,
psychiatry, obstetrics & gynecology) and agreements for faculty and facilities that would
provide for the more than 40% increase in the number of students who would require
clinical training in local facilities if UNTMD is developed according to the Plan.
JMWatt Consulting ● Altman 11
Report to TOMA: Development of an Allopathic Medical School at UNTHSC February 7, 2011
Summary Observations and Conclusions – Academic Program
Clearly there has been much thought given to the development of the program proposal
for a new school of allopathic medicine at UNT. The academic program has most
certainly been tailored to attempt to meet the LCME standards and to be different from
the program at TCOM in sufficient particulars to justify its separate development and
accreditation while being as frugal as possible. Many details have been necessarily left
out. However our review of the UNTMD Plan suggests concerns about several of its
elements:
The joint faculty arrangement prescribed may generate “economies of scale” but may
also run afoul of the LCME requirements for independence and autonomy of the
medical school faculty.
The community-based model of clinical education has worked well for some schools
of medicine, but the challenges in gaining and especially sustaining success in such
an arrangement are substantial, especially around guaranteeing quality instruction.
This approach to clinical education requires recruiting sufficient numbers of
voluntary faculty who donate their time or receive some stipend support. Recruiting
community faculty and assuring educational quality is made even more challenging
by the increasing pressures on practicing physicians for productivity in the face of
declining reimbursement and the increasing requirements for direct supervision of
trainees, both medical students and residents, in the clinical setting.
The role of GME in medical student education has been under-emphasized, as has the
difficulty in developing new residency programs in hospitals currently without GME
activities. This is the case related to both the sources of revenues to support GME
and the difficulty faced with gaining GME program accreditation.
The difficulty and expense of developing a robust research enterprise is not
sufficiently acknowledged. The cost of recruiting a single senior investigator and his
or her entourage can easily be well beyond $1 million versus the $750,000 projected
in the Plan.
The overarching issue of whether there is now a need for a new medical school in the
Dallas-Fort Worth Metroplex has also been called into question by some of those we
have interviewed. As one individual in the region who has for a number of years
been in senior positions in medical education told us, “We really do not need this
medical school here, not at a time when state funds are limited and serious budget
reductions are threatened.” With the development of a UNTMD in the Metroplex,
along with the expanded enrollment of TCOM and the highly regarded, research
intensive University of Texas Southwestern Medical School, the Metroplex would be
the area with the highest concentration of medical students in public medical schools
in Texas. As the December 2008 report of the Texas Health Policy Council showed,
medical schools in Texas enroll more first-year medical students who are from the
Metroplex than from any other region in Texas. But the Metroplex has less than half
JMWatt Consulting ● Altman 12
Report to TOMA: Development of an Allopathic Medical School at UNTHSC February 7, 2011
as many first-year residency positions as the Gulf Coast (Houston/Galveston) region.4
As discussed above, if the fundamental goal is to educate physicians who will meet
the future needs of the Metroplex, the focus should be on GME.
Infrastructure and Facilities Plan
The Plan proposes to accommodate a 43% increase in medical student numbers on
campus without any new building. Renovation of 22,200 square feet of space in facilities
vacated by TCOM is planned to provide the lounge space and most, but not all, of the
lecture and classroom space required for the UNTMD students, and $1.6 million for these
renovations has been included in the financial plan – as an “HSC-wide expense” and
therefore not included in the $21.5 million figure the Plan cites as the costs of developing
UNTMD. Library and study space in the Lewis Library on campus (which recently added
an open floor of study space), along with other buildings on campus, is projected to be
capable of handling the large increase in students.
The Plan, however, does not address in detail how it would provide for a number of the
other critical facilities required for the new school and its incremental staff. It discusses
gross anatomy laboratory and related space, and concludes it is adequate. However, while
the staffing plan anticipates that 5 of the 12 FTE additional basic science faculty
members will be research faculty and the financial plan projects the recruiting packages
for those faculty members will include $250,000 each for lab renovations, the Plan does
not discuss where in the existing buildings on campus those labs would be housed.
UNTHSC’s planned research building, for which it is seeking legislative funding
approval during this session but not mentioned in the Plan, may be sized sufficiently to
accommodate an increase in researchers and research-related administrative functions,
but the space and cost are not included in the Plan, and accommodating the additional
research faculty would be contingent on Legislative authority to construct that additional
space.
More generally, the Plan does not discuss where space would be provided for the
additional faculty who need to be recruited for UNTMD, who could range upward from
26 FTE to as many as 100 (individual headcount). While individual offices need not be
required for all of them and some of the clinical faculty in particular presumably would
have space at the hospitals, additional space on campus likely will be needed. Similarly,
the Plan does not provide space for the Dean’s office or administrative functions of
UNTMD, other than to suggest that they potentially could be located in space built for
TCOM and other existing campus programs, which would cramp the potential future
expansion of the programs for which the building was built and create pressure for
additional building on campus after UNTMD was developed that is not included in the
Plan. The Plan’s financial analysis does not include any portion of the development costs
of these additional spaces either as up-front costs (as it does treat renovation of the
building that TCOM will vacate and UNTMD will use) or show any separate line item
for costs of occupancy of the buildings over the eight-year projection period.
4
Texas Health Policy Council, Physician Workforce and Graduate Medical Education in Texas,
December, 2008, figures 10 and 13, pps 19 and 21.
JMWatt Consulting ● Altman 13
Report to TOMA: Development of an Allopathic Medical School at UNTHSC February 7, 2011
Summary Observations and Conclusions – Infrastructure and Facilities Plan
The planned space assumes significant sharing, which makes direct comparisons difficult,
but appears to leave out provision for school functions that are included in the space
inventories of other medical schools in Texas.
Financial Plan
The Plan includes as an appendix the “High-Level Costing Model” developed in August
2010, which provides significant detail to support the projected revenues and costs
associated with development and operation of UNTMD. The analysis appropriately is
presented on a marginal cost basis – attempting to project only the incremental costs and
revenues attributable to developing UNTMD. It is clear that economies are possible by
developing a new program that would share resources on an existing campus. However,
the size of the new program – projected to be a 43% increase in the medical students
trained through UNTHSC – raises many issues of “relevant range” in the estimate of
incremental activity that could be undertaken by existing campus units without additional
cost.
The projected budget of the Dean’s office presents one example. Staffing during the
planning period appears especially lean, given the extent of agreements that need to be
put into place and documentation that needs to be developed for the LCME accreditation
process. Despite the large number of affiliation contracts and program agreements that
will need to be put into place to govern the students’ experience in clinical rotations,
there is no provision for General Counsel, either as direct staffing or as a specifically
allocated expense. Similarly, there is no provision for staff or allocated cost for
Operations (human resources, controller, public relations, etc.) all of which will have
significant up-front, unique demands on their time to establish the new school. Despite
the Plan’s reliance on community physicians as clinical faculty, there is no provision for
a director of faculty development to recruit faculty and assure their development as
teachers. While the summary financial plan does include UNTHSC’s standard assessment
of 35% of UNTMD revenues as “infrastructure costs,” there is no assessment during the
planning period when school-specific marginal demands on UNT infrastructure will be
highest.
As discussed above, it is likely that significant facility-related costs also are not included
in the Plan.
Thus, while we agree that UNTMD may be able to be developed at a cost less than the
$100 million estimated by THECB as the cost of developing a new medical school, the
net $21.5 million figure cited as the costs of developing and operating UNTMD from
inception to “full build out” with 400 students substantially understates the financial
commitment that would be required.
The revenue side of the financial Plan demonstrates that UNTMD would not be
“costless” to the State general fund: the Plan assumes state funding for the increased
number of students, without reduction in statewide per student funding formula that
JMWatt Consulting ● Altman 14
Report to TOMA: Development of an Allopathic Medical School at UNTHSC February 7, 2011
might be required by the Legislature in the face of State budget shortfalls as the number
of students increases at UNTHSC and at other schools statewide.
The projected state payments in the financial Plan also demonstrate the importance of
enrolling the full first 100 UNTMD students in 2013: state formula funding is provided
during a biennium based on the number of students enrolled at the end of the prior
biennium. If UNTMD’s first class is delayed to 2014, it would not receive the $10.6
million in state payments projected for 2014 and 2015. This $10.6 million in revenue is
assumed to be received by UNTMD in those years – and without it the net cost of
developing UNTMD would rise to $32.1 million, greater than the pledges of private
support UNTHSC reports it has received. Similarly, if UNTMD is unable to fill its first
class due to a later than projected accreditation decision by LCME, it would receive state
payments, but a lower amount than projected. UNTMD’s Plan is unusual in projecting
the full 100 students expected to be the maximum size of its future classes are recruited in
its first year. Many other schools in development recruit smaller initial classes and
expand later ones as the infrastructure for the school develops, procedures become more
routine, etc. Tuition revenue also is important to the financial viability of the Plan, and
dependent on UNTMD’s ability to reach its target number of students in each year.
Finally, we note that other schools in operation in Texas and elsewhere seek philanthropy
and other sources to meet operating as well as capital needs. Against that background it
is hard to imagine a UNTMD revenue/cost structure that would produce, as projected in
the financial Plan, annual reserves for additional investment without requiring
philanthropy.
Summary Observations and Conclusions – Financial Plan
The Plan presents detailed financial projections, appropriately constructed on a marginal
cost basis. However, costs that would appropriately be directly allocated to UNTMD
appear to be left out of the calculations, and the revenue projections assume a timing and
level of success in recruitment of students that appears highly unlikely. The estimated net
$21.5 million cost for development of UNTMD depends on its receiving $10.6 in State
funds in 2014 and 2015, which itself depends on the School’s ability to recruit a full class
of 100 to matriculate in 2013.
JMWatt Consulting ● Altman 15
Report to TOMA: Development of an Allopathic Medical School at UNTHSC February 7, 2011
Conclusions and Recommendations
The University of North Texas has set forth an ambitious plan to develop and open a new
allopathic medical school matriculating 100 students per year beginning in 2013. This
new school would be linked to the existing, well-regarded Texas College of Osteopathic
Medicine. The UNT Regents have approved the Plan, as well as specific provisions that
are meant to protect the interests of the osteopathic school, although these provisions
have not satisfied the concerns of the osteopathic profession nor are they clearly
enforceable. Much thought has gone into the program plan, with attention to the broad
issues of medical education in a setting that nurtures students, addresses both primary
care and specialty careers, and supports research.
However, the Plan includes timelines and financial and facility plans that we believe are
at best challenging and may be unrealistic. This begins with the permissions that need to
be granted by the Texas Legislature and the Texas Higher Education Coordinating Board
before anything else of substance can done, and goes through the process of receiving
accreditation by the LCME, the recruitment of deans, other leaders, and core faculty, and
the application process for admitting new students. While some economies are generated
through the sharing of faculty and space, the overall financial plan is priced well below
what recent experience with building such an enterprise in Texas has been.
Given that at least to date no legislation has yet been proposed that would give UNT
permission to develop a program leading to the M.D. degree, there is likely to be a
significant delay in realizing the Plan that the Regents approved.
There are three major conclusions we would draw from our review:
1. There is no immediate need for an allopathic medical school in Fort Worth,
given the greater need for graduate medical education positions and the
opportunity to expand the output of TCOM, both of which would do more and
more quickly to answer Texas’ need for primary care physicians.
2. The time course for development of a new school has been substantially
underestimated. Given the time needed for the administrative and other
arrangements that take precedence over admitting students, it may require an
additional one-to-three years for the first class to matriculate if the University
were to go forward with the plan for an allopathic medical school.
3. The financial plan is underfunded. Even with the economies that could be
realized due to shared physical and personnel resources, it is difficult to see how a
new medical school could be developed at this cost, which is but a quarter of the
estimates made by the Higher Education Coordinating Board and which has been
the experience elsewhere in Texas. With the State of Texas already facing a
$27 billion deficit in its current legislative biennium, a funding shortfall in the
plan for UNTMD would be difficult to make up from public sources and could
severely compromise the viability and quality of the education program.
JMWatt Consulting ● Altman 16
Report to TOMA: Development of an Allopathic Medical School at UNTHSC February 7, 2011
These conclusions apply now and into the foreseeable future. For them to change, we
believe the following conditions would be required:
The priorities for medical education set forth by the THECB and others for GME
development and for schools in other regions of the state would have been met.
The Texas legislature would be able to commit to ongoing support to funding
additional student positions without a commensurate decrease in formula funding
for current positions.
The availability of primary care physicians in shortage areas had been adequately
addressed.
Based on these findings, we would make the following recommendations:
1. The Texas Osteopathic Medical Association (TOMA) should not endorse the
plan approved by the University of North Texas Regents to develop a new
allopathic medical school.
2. TOMA should work with the TCOM and UNT leadership, as well as with the
leadership of teaching hospitals in the Metroplex, the University of Texas
health leadership, and the legislature, to expand opportunities in graduate
medical education programs. This would include both increasing available
residency positions for osteopathic school graduates and increasing the overall
GME enterprise in the region and the state, especially those GME programs that
prepare trainees for primary care practice.
JMWatt Consulting ● Altman 17
Report to TOMA: Development of an Allopathic Medical School at UNTHSC February 7, 2011
Appendix A
Author Biographical Information
David Altman, MD, MBA. is a medical executive with over 30 years’ experience as a chief
medical officer in public teaching hospitals, dean of a geographically separated medical school
campus, health policy and management consultant, practitioner, medical educator and LCME
accreditation site visit member. Dr. Altman received his residency training in internal
medicine and gastroenterology at the University of California Medical Center in San
Francisco. While a member of the faculty at UCSF, he also served for ten years as the school's
Associate Dean and attained the rank of Professor of Clinical Medicine. In 1989, he was
appointed as Associate Dean and Director of the University's Medical Education Program in
California’s Central San Joaquin Valley, overseeing medical training programs which were
aimed at addressing the chronic shortage of primary care physicians in the state’s rural areas.
In this capacity he worked closely with many of the community hospitals in the region and
maintained an active clinical practice at UCSF. In 1992-93 he was a Robert Wood Johnson
Health Policy Fellow and under the auspices of this program served on the legislative staff of
Senator John D. Rockefeller IV of West Virginia. He was also a member of working groups
of the White House Task Force on Health Care Reform in 1993. As Associate Vice President
for Medical Education, from 1994-1996 Dr. Altman launched the AAMC’s Generalist
Physician Initiative. From 1996 through 2000 Dr. Altman was a vice president at The Lewin
Group, where he led projects related to strategic planning, hospital and academic medical
center consolidations, physician compensation arrangements, physician-hospital relations, and
graduate medical education. He directed the project to develop the Harlingen proposal for the
RAHC. From 2001 through 2004 he led clinical and academic programs as Chief Medical
Officer at the Los Angeles County-USC Healthcare Network, a 1350-bed academic hospital
system. From 2004 through 2008 Dr. Altman was Chief Medical Officer at Alameda County
Medical Center, an integrated health care system that is Oakland, California’s leading trauma
center. He currently serves as Regional Medical Director for the Central California Alliance
for Health, the Medicaid managed care organization serving 200,000 residents of Santa Cruz,
Monterey, and Merced counties.
J. Michael Watt, MBA is President of JMWatt Consulting, an independent consulting
practice he established in May 1999 that specializes in planning, financial analysis and
management assistance for healthcare institutions. Over the last 30 years, his consulting
practice has focused on strategic planning and inter-institutional relations projects for the top
management and boards of health care institutions and medical schools. He recently led
development of a report outlining a multi-year plan for developing the University of Texas-
San Antonio’s Regional Academic Health Center into a four-year medical school and Health
Science Center. Previously, with Dr. Altman, he assisted the community of Harlingen, Texas,
Valley Baptist Medical Center and Su Clinica Familiar in developing the proposal that led to
the development of the RAHC in the Lower Rio Grande Valley and subsequently assisted in
developing the affiliation agreement between the UTHSCSA and VBMC, the ACGME-
accredited internal medicine residency program, and proposals for state and Medicare funding
for RAHC programs. In projects for the Santa Clara Valley Health and Hospital System since
2000, he led development of strategic business plans; facilitated planning for expansion of
JMWatt Consulting ● Altman A.1
Report to TOMA: Development of an Allopathic Medical School at UNTHSC February 7, 2011
SCVHHS’ system of community based primary care clinics and incorporating medical home
principles into their organization and operations; and assisted in development of plans for
replacement of inpatient facilities to meet California seismic safety requirements. He also has
assisted a number of federally qualified health centers in a variety of planning projects. Before
establishing JMWatt Consulting for 12 years he directed projects as a Vice President of The
Lewin Group, a national health policy research and management consulting firm. He led
strategic planning studies for academic health science centers, urban public hospitals,
community hospital systems and research institutes. In projects focused on medical education,
he led Lewin’s studies of geographically separated medical school campuses and the costs of
limits on resident work hours, and facilitated development of GME consortia in Phoenix and
Fort Worth. Subsequently, the Phoenix GME Consortium became part of the University of
Arizona’s two-year geographically separated medical school clinical education program in
Phoenix, which recently enrolled its first class as the University of Arizona College of
Medicine at Phoenix, now a full, four-year medical school.
JMWatt Consulting ● Altman A.2
Appendix B February 7, 2011
APPENDIX B
LCME REQUIREMENTS FOR ACCREDITATION OF A FOUR-YEAR SCHOOL OF MEDICINE
ASSESSMENT OF THE PROPOSAL FOR A NEW SCHOOL OF MEDICINE AT THE UNIVERSITY OF NORTH TEXAS
ELEMENT REQUIREMENT1 m/s2 UNTMD PLAN vs. LCME Requirement
I. Institutional Setting
A. Governance and
Administration
Part of an accredited (m), not-for-profit (s) m/s relationship with UNT fulfills standard
institution with formal delineation of the
relationship
By-laws govern faculty, executives, and m relationship with UNT fulfills standard
governing board
A qualified dean with access and clear lines m to be recruited
of authority
Appropriate associate and assistant deans, s to be recruited and relationships with TCOM determined.
department chairs, other leaders, and staff Proposal suggests some parallel positions, some unified
Charter key committees m to be completed
B. Academic Environment
Component of a university offering other s planned, contingent on authorization by Legislature and
graduate and professional degrees approval by THECB
Clinical settings with GME and CME s not yet completed, although commitments supposedly
have been made by various clinical entities in Fort Worth
area; few GME programs currently accredited and in
operation. Hospital interest in expanding GME described
as their primary interest in UNTMD proposal.
An environment of a "community of scholars" m to be developed
1
from LCME, Functions and Structure of a Medical School, 2010 (bold=requirements for LCME consideration of new medical schools)
2
m="must" s="should"
JMWatt Consulting ● Altman Page B.1
Appendix B February 7, 2011
1 2 UNTMD PLAN vs. LCME Requirement
ELEMENT REQUIREMENT m/s
Opportunities for students in research, other s to be developed; scholarly activities, research at UNTHSC
scholarly activities, service-learning are centered in the Graduate School of Biological
Sciences. Current activities in the osteopathic medical
school are less than at many allopathic schools
Policies and practices to achieve diversity: m Mission statement commits to diverse student population
students, faculty, staff mirroring that of Ft. Worth, and Plan calls for a Director of
Diversity Programs. But no such position is identified in
the 8-year table of staffing in financial model.
II. Educational Program for
the M.D. Degree
A. Educational Objectives
Faculty defines overall objectives for the m not clear in plans
educational program
A working plan for the curriculum as a m exists, but relationship to TCOM's existing curriculum not
whole clear.
Objectives stated in outcome-based terms that m to be done
allow assessment of developing competencies
A system of central oversight of the program m to be done. Relationship with existing TCOM systems and
and settings and faculty monitoring of student staff a critical & unclear factor.
progress
Objectives known to all involved in or m to be done. Relationship with existing TCOM systems and
responsible for student education staff a critical & unclear factor. E.g., proposed shared
clerkships will be difficult for supervising faculty if learning
objectives are different
1. General Design
At least 130 weeks of instruction m to be done
Program includes:
active learning and independent study m not addressed
current concepts in basic & clinical science m in plan
fundamental principles of medicine m in plan
JMWatt Consulting ● Altman Page B.2
Appendix B February 7, 2011
1 2 UNTMD PLAN vs. LCME Requirement
ELEMENT REQUIREMENT m/s
Comparable educational experiences and m addressed In program plan as a goal
methods of evaluation across sites
2. Content While the proposal addresses many of the issues that are
important for accreditation, the level of detail is not that
which is required for accreditation.
Includes behavioral and socioeconomic m in plan
content
Full spectrum of basic sciences (m), including m/s in plan
laboratory experience (s)
Clinical instruction in all organ systems; m in plan
experience in primary care; experience in both
outpatient and inpatient settings
Clinical experience across array of core s in plan
disciplines
Multidisciplinary content areas (e.g., ER, m in plan
Geriatrics)
Basic principles of clinical and translational m in plan
research
Instruction in communication skills, medical m in plan
consequences of common societal problems,
cultural diversity, gender and cultural biases,
medical ethics
C. Teaching and Evaluation
Residents familiar with educational objectives m limited current GME programs, and no discussion of the
and prepared as teachers planning and budget needed to develop them.
Faculty supervise learning experiences and m Plan for supervision and evaluation to be developed. See
have a system of evaluation across comments above about plan assumptions about shared
knowledge, skills, behaviors, and attitudes TCOM/UNTMD supervision
Evaluation of problem solving, clinical m not addressed
reasoning, and communication skills
Course and clerkship directors have system of m not addressed
JMWatt Consulting ● Altman Page B.3
Appendix B February 7, 2011
1 2 UNTMD PLAN vs. LCME Requirement
ELEMENT REQUIREMENT m/s
Students evaluated early enough to allow for s not addressed
remediation
Evaluations include narrative component s not addressed
D. Curriculum Management
1. Roles and Responsibilities
Integrated institutional responsibility for m in plan, but relationship to TCOM to be developed .
overall design, management, and Staffing plan does not provide an Assoc Dean for Med Ed
evaluation of curriculum
Chief Academic Officer with resources and m in plan
authority
Faculty committee monitors courses, works m in plan
with course leaders and administration re time
in courses and total required hours
2. Geographically Separated
Programs
Chief Academic Officer responsible for m N/A
program at all sites; site director responsible to
medical school's Chief Academic Officer
Single standard for promotion and graduation m N/A
of students
School responsible for assignment of students s/m N/A
(s); students provided with a process to
request alternative site (m)
E. Evaluation of Program
Effectiveness
School uses variety of measures including m not addressed
student evaluation of courses, to assess
degree to which objectives are being met
III. Medical Students
A. Admissions
1. Premed Requirements
Broad course of study with limited required s not clear in plan
courses
JMWatt Consulting ● Altman Page B.4
Appendix B February 7, 2011
1 2 UNTMD PLAN vs. LCME Requirement
ELEMENT REQUIREMENT m/s
2. Selection
Faculty committee with responsibility, m acknowledged, however questions about whether
clearly defined policies and selection proposed staff adequate to process expected applications
criteria / interviews. Note that TCOM faculty are expected to
conduct some UNTMD interviews.
Sufficient pool of applicants m assumed
No political of financial factors in admissions m acknowledged
Programs for diversity, standards for m to be done
admission of disabled students
Informational materials describe programs and m to be done
school's criteria for selection
3. Visiting and Transfer
Students
Have comparable experience and m n/a
achievement to current students
Verify credentials of visiting students s n/a
Visiting students possess comparable m n/a
qualifications to current students
B. Student Services
1. Academic and Career
Counseling
Systems for academic advising and for m spin-off from TCOM
career choice assistance
Residency application not disruptive of s n/a
education
2. Financial Aid Counseling
and Resources
Effective financial aid and debt m Assigned to Director of Financial Aid (new position).
management counseling Staffing plan doesn't have position in place during initial
application year.
JMWatt Consulting ● Altman Page B.5
Appendix B February 7, 2011
1 2 UNTMD PLAN vs. LCME Requirement
ELEMENT REQUIREMENT m/s
Programs for minimizing effect of educational s not in plan
expenses on debt
Policies for tuition and fee refunds m not in plan
3. Health Services and
Personal Counseling
Effective programs for counseling, well- m Assigned to Director of Medical Education (new position)
being Not in staffing plan
Access to preventive, diagnostic, and m not in plan
therapeutic health services, health
insurance, disability insurance
Those providing psychiatric care not involved m not in plan
in academic evaluation
Follow guidelines for immunization of students s not in plan
Policies for student exposure to infectious and m not in plan
environmental hazards
C. The Learning Environment
No discrimination based on gender, sexual m plan needs to be written
orientation, age, race, creed, or national origin
Ensure that the environment promotes m plan needs to be written
development of explicit and appropriate
professional attributes
Define and publicize standards of conduct m plan needs to be written
for teachers, learners and the teacher-
learner relationship and policies for
resolution
Publicize to all faculty and students m plan needs to be written
standards and procedures for evaluation,
advancement, graduation, disciplinary
action
JMWatt Consulting ● Altman Page B.6
Appendix B February 7, 2011
1 2 UNTMD PLAN vs. LCME Requirement
ELEMENT REQUIREMENT m/s
Due process for students subject to adverse m plan needs to be written
action
Student records kept confidential, available to m plan needs to be written
faculty on "need to know" basis
Assure adequate study space, lounge areas, s lounge area from old TCOM building made available;
lockers, secure storage needs to be renovated. Library/study space adequate for
proposed class size.
IV. Faculty
A. Number, Qualifications,
and Functions
Sufficient numbers to meet the needs of the m Proposal calls for the two medical schools to share a
educational program common faculty , with 12 FTE added the Basic Science
faculty and 14 FTE added to the faculty in the clinical
departments to accommodate the larger student body.
Faculty in the clinical departments is primarily part-time
from affiliated hospitals and other organizations; support
would be through a combination of medical school
stipends and clinical practice. A faculty practice plan is
not proposed.
Faculty with capability and commitment as m Faculty recruitment is proposed as a departmental
effective teachers function; separate but overlapping recruitment functions
proposed , with oversight by a Promotions and Tenure
Committee
Commitment to scholarly productivity s not in proposal
Faculty make decisions on student m not in proposal
admissions, promotion, and graduation,
provide career and academic counseling
B. Personnel Policies
Clear policies for faculty appointment, m/s Promotion and Tenure Committee to be appointed; would
promotion, tenure, and dismissal (m), be responsible for policy development
conflict of interest (s)
JMWatt Consulting ● Altman Page B.7
Appendix B February 7, 2011
1 2 UNTMD PLAN vs. LCME Requirement
ELEMENT REQUIREMENT m/s
Faculty receive written information about terms s not in current proposal
of appointment, responsibility, privileges,
benefits, regularly scheduled evaluations of
performance
C. Governance
Dean and committee of faculty determine s as proposed
medical school policies
Full faculty meets regularly to discuss medical s not in current proposal. Schools heavily reliant on
school policies and procedures community clinical faculty have difficulty in making this
happen effectively.
V. Educational Resources
LCME notified of changes in enrollment or m n/a for now
resources
A. Finances
Adequate present and anticipated financial m May be underestimated in proposal; current thinking
resources for the educational program and bases cost estimates on assumptions re: cost savings
achievement of institutional goals from shared faculty, facilities. Also may overstate funds
available from tuition and state resources.
B General Facilities
Buildings and equipment appropriate m Plan depends on MD school taking over space vacated by
the DO school, which is moving to new desirable space;
the adequacy of that space is subject of a separate
section of this report.
Appropriate security systems at all sites s not in current proposal
JMWatt Consulting ● Altman Page B.8
Appendix B February 7, 2011
1 2 UNTMD PLAN vs. LCME Requirement
ELEMENT REQUIREMENT m/s
C. Clinical Teaching Facilities
Appropriate resources for clinical m UNTHSC has developed an expanded clinical simulation
instruction facility. Other clinical instruction resources depend on
hospital affiliates.
Hospital that is major teaching site with m Affiliation with hospitals already engaged in GME is being
appropriate instructional facilities and counted on for instructional facilities as well as faculty.
information resources Programs in new hospital affiliates without current GME
have not been developed.
Required clerkships in settings where there are s needs development; it is not clear where the hospitals
residents in accredited GME programs, without currently accredited residency programs are in the
residents teaching under faculty supervision. process with the ACGME. Those with approved programs
do not have the capacity to accommodate all the new
students, especially given the provision in paragraph 13 of
Appendix A of the Plan, which promises equal access of
MD and DO students to clinical training sites.
Written and signed affiliation agreements m Proposal says they are present, but none is specified.
Students at affiliate sites remain under control m Current status not clear. Staffing proposal does not
of the faculty provide a General Counsel resource to develop affiliation
agreements.
D. Information Resources
and Library Services
Access to well-maintained library and m This seems adequate. Staffing plan provides 4 additional
information facilities of sufficient size and FTE for informatics and library.
breadth, information technology
Library and information services m ditto
responsive to needs of faculty, residents,
students
JMWatt Consulting ● Altman Page B.9
You might also like
- UNT System Contract With Scott Ransom, DO As President of UNTHSC From 2006-2015Document28 pagesUNT System Contract With Scott Ransom, DO As President of UNTHSC From 2006-2015Tây SơnNo ratings yet
- Report On Evaluation of The Proposed Merger of UNTDocument33 pagesReport On Evaluation of The Proposed Merger of UNTTây SơnNo ratings yet
- Paris Peace Accords 1973Document16 pagesParis Peace Accords 1973Tây SơnNo ratings yet
- The National Flag of VNDocument16 pagesThe National Flag of VNTây SơnNo ratings yet
- Letter of Appreciation From A Patient's DaughterDocument3 pagesLetter of Appreciation From A Patient's DaughterTây SơnNo ratings yet
- UNT System Firing Letter To UNTHSC President Scott RansomDocument4 pagesUNT System Firing Letter To UNTHSC President Scott RansomTây SơnNo ratings yet
- President Ransom's Presentation To Board of RegentsDocument4 pagesPresident Ransom's Presentation To Board of RegentsTây SơnNo ratings yet
- The Law of Sea of VietnamDocument24 pagesThe Law of Sea of VietnamTây SơnNo ratings yet
- Letter of Chairman of Board of VisitorsDocument2 pagesLetter of Chairman of Board of VisitorsTây SơnNo ratings yet
- Sovereignty of Vietnam Over Spratly and Paracel IslandsDocument11 pagesSovereignty of Vietnam Over Spratly and Paracel IslandsTây SơnNo ratings yet
- Blind AmbitionDocument3 pagesBlind AmbitionTây SơnNo ratings yet
- The Right Eye Care For YouDocument3 pagesThe Right Eye Care For YouTây SơnNo ratings yet
- China's Erroneous Juridical Title Claims in Paracel and Spratly IslandsDocument13 pagesChina's Erroneous Juridical Title Claims in Paracel and Spratly IslandsTây SơnNo ratings yet
- Examine China's Claim Over SpratlysDocument3 pagesExamine China's Claim Over SpratlysTây Sơn0% (1)
- The Historical and Juridical Title of Vietnam After 1884Document10 pagesThe Historical and Juridical Title of Vietnam After 1884Tây SơnNo ratings yet
- Historical Title of China Concerning The XishaDocument6 pagesHistorical Title of China Concerning The XishaTây SơnNo ratings yet
- Analyzing The Diplomatic Note of Pham Van DongDocument4 pagesAnalyzing The Diplomatic Note of Pham Van DongTây SơnNo ratings yet
- Chapter III-5 Subsequent Development of The TitleDocument3 pagesChapter III-5 Subsequent Development of The TitleTây SơnNo ratings yet
- The Spratlys ResurfaceDocument3 pagesThe Spratlys ResurfaceTây SơnNo ratings yet
- Chapter II-Acquisition of The Original TitleDocument6 pagesChapter II-Acquisition of The Original TitleTây SơnNo ratings yet
- The Historical and Juridical Title of VietnamDocument13 pagesThe Historical and Juridical Title of VietnamTây SơnNo ratings yet
- International Claims in Spratly and Oil ClaimsDocument4 pagesInternational Claims in Spratly and Oil ClaimsTây SơnNo ratings yet
- Chapter III-6 Subsequent Development of TitleDocument7 pagesChapter III-6 Subsequent Development of TitleTây SơnNo ratings yet
- Chapter IV-Conclusions and Bases For A Settlement of The DisputeDocument8 pagesChapter IV-Conclusions and Bases For A Settlement of The DisputeTây SơnNo ratings yet
- Chapter III-5 Subsequent Development of The TitleDocument3 pagesChapter III-5 Subsequent Development of The TitleTây SơnNo ratings yet
- Chapter III-4 Subsequent Development of The TitleDocument11 pagesChapter III-4 Subsequent Development of The TitleTây SơnNo ratings yet
- Chapter III-7 Subsequent Development of The TitleDocument8 pagesChapter III-7 Subsequent Development of The TitleTây SơnNo ratings yet
- Chapter III-3 Subsequent Development of TitleDocument3 pagesChapter III-3 Subsequent Development of TitleTây SơnNo ratings yet
- Chapter III-1 Subsequent Development of TitleDocument6 pagesChapter III-1 Subsequent Development of TitleTây SơnNo ratings yet
- Chapter III-2 Subsequent Development of TitleDocument5 pagesChapter III-2 Subsequent Development of TitleTây SơnNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Mock Examination Routine A 2021 NewDocument2 pagesMock Examination Routine A 2021 Newmufrad muhtasibNo ratings yet
- Sing A Like CompetitionDocument3 pagesSing A Like CompetitionLajo HeroNo ratings yet
- Timeline of Sikolohiyang Pilipino in <40Document2 pagesTimeline of Sikolohiyang Pilipino in <40Ces0% (1)
- Both Texts Discuss The Topic of Technological Changes That Museums Have Undergone Over The Last DecadeDocument2 pagesBoth Texts Discuss The Topic of Technological Changes That Museums Have Undergone Over The Last DecadefonderoNo ratings yet
- Work Immersion Action Plan 2020-2021Document10 pagesWork Immersion Action Plan 2020-2021francisco macatugobNo ratings yet
- State Common Entrance Test Cell, Maharashtra State, MumbaiDocument50 pagesState Common Entrance Test Cell, Maharashtra State, MumbaiDinesh GadkariNo ratings yet
- Data and Graphs Project Advanced MathDocument8 pagesData and Graphs Project Advanced Mathapi-169858360No ratings yet
- AFMC MBBS Information Brochure 2019Document27 pagesAFMC MBBS Information Brochure 2019riteshNo ratings yet
- 13.2.3a Practicing Good SpeakingDocument9 pages13.2.3a Practicing Good SpeakingNieyfa RisyaNo ratings yet
- COmmonwealthDocument7 pagesCOmmonwealthCle Ford DhyNo ratings yet
- P.E 7 Lesson PlanDocument3 pagesP.E 7 Lesson PlanRazel Atamosa CodinaNo ratings yet
- 08 Amber B11 Llgas Jeric B.Document1 page08 Amber B11 Llgas Jeric B.Loriene SorianoNo ratings yet
- CAV JanuaryCOADocument58 pagesCAV JanuaryCOAGina GarciaNo ratings yet
- E-3 Start Invitation Paying-RevisedDocument5 pagesE-3 Start Invitation Paying-Revisedmario navalezNo ratings yet
- Sally-Mangan SADocument30 pagesSally-Mangan SAAlex NichollsNo ratings yet
- 08:05 Fan ShenDocument9 pages08:05 Fan ShenFlavia StoianNo ratings yet
- Radical Innovation Liberating The Potential of TOC in Mining 2019-05-15 Arrie V NiekerkDocument45 pagesRadical Innovation Liberating The Potential of TOC in Mining 2019-05-15 Arrie V NiekerkJelena FedurkoNo ratings yet
- 15 - Unit Test 1Document1 page15 - Unit Test 1gildae219100% (1)
- A Resource Book For The Beginning Physics Teacher: DraftDocument6 pagesA Resource Book For The Beginning Physics Teacher: DraftAnirudh KhannaNo ratings yet
- Gurugram University, Gurugram: Revised Last Date of Online Application For The Ph.D. ProgrammeDocument2 pagesGurugram University, Gurugram: Revised Last Date of Online Application For The Ph.D. ProgrammeNikhil KumarNo ratings yet
- Unit 2: Language Test B: GrammarDocument2 pagesUnit 2: Language Test B: GrammarBelen GarciaNo ratings yet
- AggressionDocument54 pagesAggressionادیبہ اشفاقNo ratings yet
- Business English CorrespondenceDocument6 pagesBusiness English CorrespondenceCandra Pirngadie100% (2)
- The Sport Education ModelDocument2 pagesThe Sport Education ModelZul AizamNo ratings yet
- Brussels Tribunal - Assassination of Iraqi AcademicsDocument109 pagesBrussels Tribunal - Assassination of Iraqi AcademicsOmar :)No ratings yet
- Recuitment & SelectionDocument39 pagesRecuitment & SelectionYogesh SangleNo ratings yet
- Guidelines For Critical Review Form Qualitative StudiesDocument12 pagesGuidelines For Critical Review Form Qualitative StudiesTopo SusiloNo ratings yet
- Sidneys ResumeDocument3 pagesSidneys Resumeapi-355088892No ratings yet
- Methods of Generating Ideas: Focus Groups, Brainstorming & MoreDocument21 pagesMethods of Generating Ideas: Focus Groups, Brainstorming & MoreAd QasimNo ratings yet
- SIM Grade 7 1stDocument14 pagesSIM Grade 7 1stSarah EvaristoNo ratings yet