Professional Documents
Culture Documents
Chron's Disease 2
Uploaded by
TarantadoOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chron's Disease 2
Uploaded by
TarantadoCopyright:
Available Formats
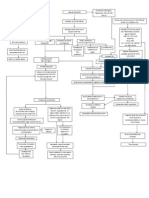
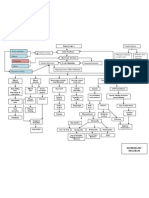
Pathophysiology:
Predisposing Factor:
Age – 15 and 30 years Precipitating Factor:
of age; 50 to 70 years of Pesticides, food
age additives, tobacco,
Women and men tend to radiation, and NSAIDs
be affected equally
Family history
Etiology:
Idiopathi
c
The disease process begins
Edema and
thickening of the
mucosa
These lesions are not
in continuous contact Ulcers begin to
with one another and appear on the
are separated by inflamed mucosa
normal tissue
Fistulas, fissures Granulomas
and abscesses occur in 50% of
These clusters of form as the patients
ulcers tend to take on inflammation
a classic “cobblestone” extends into the
appearance
As the disease
advances
The bowel wall
thickens and
becomes fibrotic
Intestinal lumen
narrows
Diseased bowel loops
sometimes adhere to other loops
surrounding them
Assessment:
Cramplike and colicky pain after meals
Diarrhea (semisolid); may contain mucus and pus
Dehydration
Electrolyte imbalances
Fever
A proctosigmoidoscopic examination is usually performed initially to determine
whether the rectosigmoid area is inflamed.
A stool examination is also performed; the result may be positive for occult
blood and steatorrhea (ie, excessive fat in the feces).
The most conclusive diagnostic aid for regional enteritis is a barium study of the
upper GI tract that shows the classic “string sign” on an x-ray film of the
terminal ileum, indicating the constriction of a segment of intestine.
Endoscopy and intestinal biopsy may be used for confirmation of the diagnosis.
A barium enema may show ulcerations (the cobblestone appearance
described earlier), fissures, and fistulas.
A CT scan may show bowel wall thickening and fistula tracts.
A complete blood cell count is performed to assess hematocrit and hemoglobin
levels (usually decreased) and the white blood cell count (may be elevated).
The sedimentation rate is usually elevated. Albumin and protein levels may
be decreased, indicating malnutrition.
Nsg Interventions:
Acute phase: maintain NPO status, administer IV’s and electrolytes, or total
parenteral nutrition (TPN), as prescribed.
Restrict the client’s activity, to reduce intestinal activity.
Monitor bowel sounds and for abdominal tenderness and cramping.
Monitor stools, noting color, consistency , and the presence or absence of
blood.
Monitor for perforation, peritonitis, and hemorrhage.
Following the acute phase, the fiet progresses from clear liquids to low
residue as tolerated.
You might also like
- Essential Newborn Care: The DOH/WHO ProtocolDocument21 pagesEssential Newborn Care: The DOH/WHO ProtocolfelicitycherubNo ratings yet
- Medstar Obgyn 1st EditionDocument320 pagesMedstar Obgyn 1st Editionfetene82% (11)
- Gouty Arthritissss PathophyDocument2 pagesGouty Arthritissss Pathophybilliam123No ratings yet
- Pathophysiology of DMDocument4 pagesPathophysiology of DMNicole Louise N. VillanuevaNo ratings yet
- Case Pre.. Cushing SyndromeDocument11 pagesCase Pre.. Cushing Syndromedee_day_8No ratings yet
- Cholecystitis Pathophysiology Schematic DiagramDocument2 pagesCholecystitis Pathophysiology Schematic DiagramChristyl CalizoNo ratings yet
- Pathophysiology of Acute Gastroenteritis: Causes, Symptoms & TreatmentDocument1 pagePathophysiology of Acute Gastroenteritis: Causes, Symptoms & TreatmentZhenmeiNo ratings yet
- Teen 2 Teen Entire Curriculum Guide For PresentersDocument113 pagesTeen 2 Teen Entire Curriculum Guide For PresentersElena Rusu50% (2)
- Pathophysiology of PneumoniaDocument2 pagesPathophysiology of PneumoniaMaria Cristina100% (1)
- Group 8: Parik Rabasto Patel, D Patel, J Raghuwanshi Regis Moleta Moreno NaromalDocument35 pagesGroup 8: Parik Rabasto Patel, D Patel, J Raghuwanshi Regis Moleta Moreno NaromalDominique RabastoNo ratings yet
- CholelithiasisDocument5 pagesCholelithiasisrgflores1979100% (2)
- CROHNSDocument2 pagesCROHNSAlvin Germo Pasuquin100% (1)
- Sources of Drug InformationDocument36 pagesSources of Drug InformationCristine ChubiboNo ratings yet
- Case Study Castillo H MoleDocument52 pagesCase Study Castillo H MoleGodfrey Bag-ao100% (1)
- 74-Year-Old Male with PneumoniaDocument5 pages74-Year-Old Male with PneumoniaBeverlyNo ratings yet
- Pathophysiology of Hyperthyroidism and Thyroid StormDocument3 pagesPathophysiology of Hyperthyroidism and Thyroid StormPen MontanteNo ratings yet
- Step 2-3-Clinical Checklist: Behavioral Science (8 Videos 2 Hours 9 Minutes)Document14 pagesStep 2-3-Clinical Checklist: Behavioral Science (8 Videos 2 Hours 9 Minutes)MILTHON DAVID DIAZ PUENTES67% (3)
- Cholecystitis Case PresDocument103 pagesCholecystitis Case PresAnton LaurencianaNo ratings yet
- Patho UGIBDocument3 pagesPatho UGIBKristineBungcagNo ratings yet
- FINAL CHOLE,,,Sa Wakas TpozDocument64 pagesFINAL CHOLE,,,Sa Wakas TpozakatzkiNo ratings yet
- Group 3 Pathophysiology-of-BREAST-CANCERDocument1 pageGroup 3 Pathophysiology-of-BREAST-CANCERArisa VijungcoNo ratings yet
- PathophysiologyDocument4 pagesPathophysiologyAngelou Joefred Congreso100% (1)
- NURSE Board Exam November 2008 ResultsDocument790 pagesNURSE Board Exam November 2008 ResultsstuffednurseNo ratings yet
- Pre EclampsiaDocument39 pagesPre EclampsiaStanly Elliemo100% (1)
- Ex LapDocument42 pagesEx LapOmar Khalif Amad PendatunNo ratings yet
- Dengue PoathoDocument6 pagesDengue PoathoCleobebs Agustin100% (1)
- Diabetes Mellitus: Hyperglycemia (304 MG/DL, 13.2 MG/DL)Document3 pagesDiabetes Mellitus: Hyperglycemia (304 MG/DL, 13.2 MG/DL)John Henry ValenciaNo ratings yet
- Weaknes S/ Fatigue Polyphag IaDocument5 pagesWeaknes S/ Fatigue Polyphag IaEwert Hesketh Nillama PaquinganNo ratings yet
- A Grand Case UgibDocument84 pagesA Grand Case UgibAdrianne Kricia100% (2)
- Pathophysiology (Client Base) :: Predisposing Factors: Precipitating FactorsDocument1 pagePathophysiology (Client Base) :: Predisposing Factors: Precipitating Factorsleslie_macasaetNo ratings yet
- Pathophysiology of Colon Cancer 1Document3 pagesPathophysiology of Colon Cancer 1Katherine Clarisse Carvajal Lavarias100% (1)
- Liver Cancer Pathophysiology: Predisposing FactorDocument3 pagesLiver Cancer Pathophysiology: Predisposing FactorTarantado100% (2)
- Abdominal Stab Wound Case StudyDocument36 pagesAbdominal Stab Wound Case StudyMean Elepaño80% (5)
- Pathophysiology of IBDDocument11 pagesPathophysiology of IBDOktarina Heni SunandarNo ratings yet
- CHOLANGITISDocument1 pageCHOLANGITISKirk Torregosa PañaresNo ratings yet
- OUR LADY OF FATIMA UNIVERSITY Case Study on Post Streptococcal GlomerulonephritisDocument20 pagesOUR LADY OF FATIMA UNIVERSITY Case Study on Post Streptococcal GlomerulonephritisMikaCasimiroBalunanNo ratings yet
- Managing Upper GI Bleeding in a Male PatientDocument19 pagesManaging Upper GI Bleeding in a Male PatientMary Ann Garcia100% (1)
- Pa Tho PhysiologyDocument3 pagesPa Tho Physiologyaprilkow07No ratings yet
- Pathophysiology of Septic Shock Secondary To PyelonephritisDocument2 pagesPathophysiology of Septic Shock Secondary To PyelonephritisShirlyn100% (1)
- Thromboangiitis Obliterans (Buerger's Disease): A Case PresentationDocument16 pagesThromboangiitis Obliterans (Buerger's Disease): A Case PresentationYan VencerNo ratings yet
- Case Analysis and Interventions Pyschopathology: Predisposing Factor Precipitating FactorDocument1 pageCase Analysis and Interventions Pyschopathology: Predisposing Factor Precipitating FactorSydelle GravadorNo ratings yet
- Cervical Cancer Patho.2Document2 pagesCervical Cancer Patho.2Verni Dela CruzNo ratings yet
- Pathophysiology: Bipolar DisorderDocument3 pagesPathophysiology: Bipolar DisorderPae EdejerNo ratings yet
- Pa Tho Irritable Bowel SyndromeDocument1 pagePa Tho Irritable Bowel Syndromekaye0403No ratings yet
- Psychopathology of Schizophrenia (Client)Document1 pagePsychopathology of Schizophrenia (Client)Robert Joseph Sison67% (3)
- Acute Gastroenteritis Pathophysiology ExplainedDocument2 pagesAcute Gastroenteritis Pathophysiology ExplainedMareeze Hatta100% (1)
- Cancer of The ColonDocument8 pagesCancer of The Colonnot your medz duranNo ratings yet
- Pathophysiology Cholelithiasis 2Document2 pagesPathophysiology Cholelithiasis 2Jamie HaravataNo ratings yet
- Cancer Pathophysiology To Be EditedDocument5 pagesCancer Pathophysiology To Be EditedEyySiEffVeeNo ratings yet
- Diabetes Mellitus Type 2 Schematic DiagramDocument1 pageDiabetes Mellitus Type 2 Schematic DiagramChristelle GarciaNo ratings yet
- Cellular AberrationDocument6 pagesCellular AberrationCheysser FerolinoNo ratings yet
- Colon Cancer: Causes, Symptoms, Stages & TreatmentDocument17 pagesColon Cancer: Causes, Symptoms, Stages & TreatmentYaska MusaNo ratings yet
- SLE PathophysiologyDocument3 pagesSLE PathophysiologyyasiraNo ratings yet
- Gastritis Types, Causes, Symptoms and TreatmentDocument17 pagesGastritis Types, Causes, Symptoms and TreatmentSri Wahyuni HarliNo ratings yet
- Pre Eclampsia of Severe FeaturesDocument3 pagesPre Eclampsia of Severe FeaturesPrincess Diane S. VillegasNo ratings yet
- Tarlac State University College of Nursing case study on choledocholithiasisDocument53 pagesTarlac State University College of Nursing case study on choledocholithiasisCzarina ManinangNo ratings yet
- Path o PhysiologyDocument9 pagesPath o PhysiologyKyle Ü D. CunanersNo ratings yet
- Neonatal Pneumonia Case StudyDocument2 pagesNeonatal Pneumonia Case StudyAngel Villamor0% (1)
- Gordon's Functional HealthDocument2 pagesGordon's Functional HealthReina ArabelleNo ratings yet
- Chronic Calculous CholecystitisDocument35 pagesChronic Calculous CholecystitisJoshua AgawinNo ratings yet
- Pathophysiology of Rheumatic Heart Disease to CardiomegalyDocument2 pagesPathophysiology of Rheumatic Heart Disease to CardiomegalyRj Avila100% (1)
- Pathophysiology of Gastric UlcerDocument4 pagesPathophysiology of Gastric UlcerNielArmstrongNo ratings yet
- Concept MapDocument2 pagesConcept Mapantherchio100% (2)
- Pathophysiology HPN CvaDocument1 pagePathophysiology HPN Cvatresdos09No ratings yet
- Inflammatory Bowel Disease Intestinal Obstruction and PolypsDocument55 pagesInflammatory Bowel Disease Intestinal Obstruction and PolypsLiza Marie IgnacioNo ratings yet
- Inflammatory Bowel Disease (IBD) Epidemiology and Clinical ManifestationsDocument5 pagesInflammatory Bowel Disease (IBD) Epidemiology and Clinical ManifestationsMaryam AzizNo ratings yet
- Valentina Miacci VI Anno 2018/2019Document20 pagesValentina Miacci VI Anno 2018/2019valentina miacciNo ratings yet
- University of Jordan Pathology Lecture on Inflammatory Bowel DiseaseDocument19 pagesUniversity of Jordan Pathology Lecture on Inflammatory Bowel DiseasejwanaNo ratings yet
- Pathophysiology of PudDocument3 pagesPathophysiology of PudAngel-Jeh De Guzman100% (1)
- Liver CancerDocument1 pageLiver CancerTarantado67% (3)
- Top Performing Schools in November 2008 NLEDocument19 pagesTop Performing Schools in November 2008 NLETarantadoNo ratings yet
- 2.3 Ferry Indriasmoko - CCA Overview Jogja 8AUG19Document12 pages2.3 Ferry Indriasmoko - CCA Overview Jogja 8AUG19Netty HerawatiNo ratings yet
- Kemampuan Clinical Reasoning Pada Ujian Osce Mahasiswa Kedokteran Tahun KetigaDocument9 pagesKemampuan Clinical Reasoning Pada Ujian Osce Mahasiswa Kedokteran Tahun Ketigabelahan jiwaNo ratings yet
- The Value of Early Intraoral Incisions in Patiens With Perimandibular Odontogenic Maxillofacial Abscess 2015Document4 pagesThe Value of Early Intraoral Incisions in Patiens With Perimandibular Odontogenic Maxillofacial Abscess 2015kaarlaamendezNo ratings yet
- Gynecological Specimen Collection Principle: Page 1 of 7Document7 pagesGynecological Specimen Collection Principle: Page 1 of 7Katrina Nadonga JarabejoNo ratings yet
- 108846HIV Rapid Test Kit Assembly Machine Poll of The DayDocument3 pages108846HIV Rapid Test Kit Assembly Machine Poll of The DaysandurigklNo ratings yet
- Case PresentationDocument35 pagesCase Presentationapi-498720485No ratings yet
- Final DraftDocument5 pagesFinal Draftapi-451064930No ratings yet
- Homeopathic Management of Ring WormDocument3 pagesHomeopathic Management of Ring WormEditor IJTSRDNo ratings yet
- Knowledge, Attitude and Practice of Cancer Screening Among Health Care Professionals in A Central Hospital in NepalDocument8 pagesKnowledge, Attitude and Practice of Cancer Screening Among Health Care Professionals in A Central Hospital in NepalBruce LennyNo ratings yet
- Bwdi DR, Chemist&Stp Final ListDocument226 pagesBwdi DR, Chemist&Stp Final ListzaheerbcNo ratings yet
- Guidelines For Toxicity/safety Profile Evaluation of Ayurved & Siddha, Plant DrugsDocument5 pagesGuidelines For Toxicity/safety Profile Evaluation of Ayurved & Siddha, Plant DrugsPRAKASH DESHPANDENo ratings yet
- Health 6 Quarter 1 Module5Document15 pagesHealth 6 Quarter 1 Module5Cindy EsperanzateNo ratings yet
- The Psychiatric Review of Symptoms - A Screening Tool For Family Physicians - American Family PhysicianDocument7 pagesThe Psychiatric Review of Symptoms - A Screening Tool For Family Physicians - American Family PhysicianTimothy TurscakNo ratings yet
- Research Proposal CapsuleDocument12 pagesResearch Proposal CapsuleClaire GonoNo ratings yet
- Capstone OutlineDocument3 pagesCapstone Outlineapi-395468231No ratings yet
- COVID-19 Vaccine Mechanisms and ImmunityDocument1 pageCOVID-19 Vaccine Mechanisms and ImmunityAvinash KumbharNo ratings yet
- JHSPH Prospectus WebDocument76 pagesJHSPH Prospectus WebAyodeji SamuelsNo ratings yet
- Prelim ProgrammeDocument7 pagesPrelim Programmeasalizwa ludlalaNo ratings yet
- Maternal 8Document15 pagesMaternal 8shanikaNo ratings yet
- Repositioning Family Planning in Mali: A BaselineDocument50 pagesRepositioning Family Planning in Mali: A BaselineFuturesGroup1No ratings yet
- Virclia Lotus en Pme095-0722Document6 pagesVirclia Lotus en Pme095-0722MohammedNo ratings yet
- Pharmaceutical Medical Sales Representative in Houston TX Resume Jennifer MillerDocument1 pagePharmaceutical Medical Sales Representative in Houston TX Resume Jennifer MillerJenniferMiller1No ratings yet
- CSL AssignmentDocument2 pagesCSL AssignmentMuhammad QubaisNo ratings yet
- PANR Part 1Document2 pagesPANR Part 1Jastine SabornidoNo ratings yet