Professional Documents
Culture Documents
Acute Ankle Injuries
Uploaded by
A C De GuzmanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acute Ankle Injuries
Uploaded by
A C De GuzmanCopyright:
Available Formats
orthopaedics
Peer Reviewed
Office Management of
Acute Ankle Injuries:
Soft Tissue Injuries
John G Aronen, MD; James G Garrick, MD
Roughly 85% of all acute ankle injuries are sprains; most are uncomplicated and involve
only the lateral ligaments. However, three types of soft tissue injury are considered
significant because of the long-term physical limitations that can result, especially when
the injuries are not initially identified and treated appropriately. These injuries involve
the retinacular sheath of the peroneal tendons, the Achilles tendon, and the tendon of
the tibialis posterior muscle. By the time the patient with a significant soft tissue ankle
injury is evaluated in the office, the findings are usually not as discrete to the area of
injury as they are when the ankle is examined immediately after the injury. However,
even if soft tissue swelling prevents a definitive diagnosis by examination alone, a
history that reveals the typical mechanism of injury, symptoms experienced, and level
of disability at the time of the injury, is usually enough to warrant early orthopaedic
referral.
A
ll acute ankle injuries result in soft
tissue trauma and swelling. Associated
with these findings is loss of motion,
which presents as stiffness, increased
generalized discomfort, and an increased level
of disability.
The time frame between an acute ankle
injury and the initial evaluation is usually suf-
ficient for significant soft tissue swelling, and
the physical and functional changes, to occur.
This increased level of disability noted initially
can lead to the assumption that the severity
of the injury is greater than it is. Thus, during
the history taking, it is important to obtain the
All acute ankle injuries result in soft tissue trauma and swelling. level of disability at the time of the injury and
shortly after.
Medical Progress July 2010 317
orthopaedics
In the June issue, we discussed
the five ankle fractures that must be
Box I
considered in the evaluation. In this A systematic guide for the examination of acute ankle injuries
article, we focus on the evaluation and
management of the three significant With the patient sitting, knees extended and feet off the examination table:
soft tissue injuries that must be 1. Perform a gross observation. Note any soft tissue swelling or ecchymosis.
considered in the evaluation of acute a. Is the extent of disability more significant than the swelling, ecchymosis, etc? The severity
ankle injuries. We also provide a of the injury is directly related to the extent of disability at the time of the injury and shortly
systematic guide for the examination after. If the extent of disability was not that significant, then the injury is not severe.
of acute ankle injuries. 2. Palpate the base of the fifth metatarsal to detect an avulsion fracture.
3. Palpate the proximal shaft of the fifth metatarsal to detect a Jones fracture.
Acute Ankle Injuries
4. If the patient is an adolescent, palpate the lateral malleolus with emphasis on the growth plate
to detect a physeal (growth plate) fracture.
Roughly 85% of all acute ankle injuries
are sprains,1 of which about 85% 5. Palpate the distal third of the fibula to detect an isolated vertical fracture.
are uncomplicated, ie, that involve 6. Palpate the area posterior and superior to the lateral malleolus for tenderness of the peroneal
the lateral ligaments only.2 When tendon retinacular sheath and the proximal peroneal tendons.
the examination findings are incom- 7. Palpate the Achilles tendon 2½ to 3 inches above its insertion site for tenderness or a defect.
patible with a fracture or tendon injury 8. Palpate the area posterior and inferior to the medial malleolus for tenderness of the tibialis
(Box I), results of diagnostic studies posterior tendon.
are negative, and the primary area of a. Evaluate both ankles for inversion motion and strength. If a difference in motion and strength
tenderness is anteroinferior to the is noted, have the patient stand up and observe for variances in the longitudinal arch of the
lateral malleolus over the anterior talo- injured foot compared with the unaffected foot.
fibular and calcaneofibular ligaments 9. Palpate the area over the navicular bone on the dorsomedial aspect of the foot.
(Figure 1), the diagnosis is that of an
10. Palpate the area of the anterior talofibular and calcaneofibular ligament.
uncomplicated lateral ankle sprain.
With the patient prone, knees extended and feet off the examination table:
Significant Soft Tissue Ankle 11. Evaluate the Achilles tendon for a visible or palpable defect and discrete tenderness 2½ to
Injuries 3 inches above its insertion site.
a. If any of the above signs are present, perform the Thompson test (Figure 4).
Of all the soft tissue ankle injuries, 12. Based on the history and examination findings, determine whether diagnostic studies are
three types are considered significant warranted.2,3 If findings are incompatible with a fracture or a significant soft tissue injury,
because of the long-term physical diagnostic studies are negative, and the primary area of tenderness is anteroinferior to the
limitations that can result, especially lateral malleolus over the anterior talofibular and calcaneofibular ligaments, the diagnosis is
when the injuries are not initially that of an uncomplicated lateral ankle sprain.
identified and treated appropriately.
These injuries involve the following
anatomical areas and corresponding muscle—located posterior to the in the office, the findings on exami-
soft tissue structures: medial malleoli and runs a course nation are usually not as discrete to
• Lateral aspect of the ankle: the inferior and anterior to the medial the area of injury as they are when the
retinacular sheath of the peroneal malleolus to its insertion onto the ankle is examined immediately after
tendons—responsible for retaining navicular bone. the injury. However, even if soft tissue
the peroneal tendons posterior to the Because of the potential for swelling prevents a definitive diagnosis
lateral malleoli long-term disability after injury to by examination alone, a history that
• Posterior aspect of ankle: the each of these structures, their exami- reveals the typical mechanism of
Achilles tendon—the tendon of the nation during the acute ankle injury injury, symptoms experienced, and
gastrocnemius and soleus muscles evaluation must be emphasized. By level of disability at the time of the
• Medial aspect of the ankle: the time the patient with a significant injury, is usually enough to warrant
the tendon of the tibialis posterior soft tissue ankle injury is evaluated early orthopaedic referral.
318 Medical Progress July 2010
orthopaedics
Figure 1.
”Of all the soft tissue
ankle injuries, three types
are considered significant
because of the long-term
physical limitations that
can result“
The primary area of tenderness in an uncomplicated lateral ankle sprain is anteroinferior to the lateral malleolus
over the anterior talofibular and calcaneofibular ligaments.
Peroneal Tendon Dislocation Figure 2.
Mechanism of Injury
Dislocation of the peroneal tendons
occurs only when the stress placed on
the peroneal tendon retinacular sheath
is sufficient enough to cause it to either
rupture or avulse from the posterolateral
aspect of the lateral malleolus. When
the ankle is forced into dorsiflexion
with or without inversion during an A B
acute ankle injury, the integrity or the
retinacular sheath—the ability to retain
the peroneal tendons posterior to the
malleoli—is challenged. If the stress
is sufficient, the peroneal tendons can
dislocate anteriorly. When the ankle is
taken out of dorsiflexion, the peroneal
tendons spontaneously reduce to their
normal location posterior to the lateral
malleoli (Figure 2). C D
The mechanism of a typical
In plantar flexion, the line of pull of the proximal peroneal muscles along the peroneal tendons onto the
uncomplicated lateral ankle sprain—
distal insertion sites is practically linear (A). In forced dorsiflexion, the line of pull becomes angular (B). With
inversion with the ankle in plantar a contraction of the peroneal muscles, the stress placed on the retinacular sheath may be sufficient to allow
flexion—does not cause the peroneal the peroneal tendons to dislocate anteriorly, as depicted by the dotted line (C). When the ankle is taken out of
tendons to place stress on their dorsiflexion, the peroneal tendons spontaneously reduce (D).
retinacular sheath.
Medical Progress July 2010 319
orthopaedics
Symptoms Typically Experienced
Patients commonly say that they felt Figure 3. Figure 4.
something quickly slip or pop forward
over the bone on their outer ankle and
then quickly slip or pop back.
Extent of Disability
The disability is typically significant.
Patients frequently hobble on the ball
of their foot to keep the ankle in
plantar flexion (this prevents them
from feeling that the peroneal tendons
may re-dislocate). Some patients may
be able to walk or limp on the foot
but have persistent, often intense, pain
at the site of the injured retinacular
sheath.
The Achilles tendon ruptures about 2 ½ to 3 inches
The Thompson test, used to determine the
above its insertion into the calcaneus (marked).
Examination Findings integrity of the Achilles tendon, is performed with
This is referred to as the "watershed area." This
Because the peroneal tendons spontan- area of the tendon has a tenuous blood supply,
the patient lying prone with his or her knees
eously reduce when the foot is out of extended and feet off the table. If the Achilles
which makes it susceptible to rupture.
tendon is intact, the amount of plantar flexion of
the forced dorsiflexed position, distinct
both feet will be equal when the gastrocnemius
tenderness is limited to the area poste- muscles are simultaneously squeezed. The test is
rolateral to the lateral malleoli (where suspected or confirmed by the history considered positive when the amount of plantar
the peroneal tendon retinacular sheath and examination. Definitive treatment flexion on the involved side is diminished or
is located). Patients may also have gen- (usually operative) by the orthopaedic absent.
eralized pain of the peroneal tendons. specialist is necessary to regain the
The generalized tenderness of peroneal integrity of the retinacular sheath.
tendon dislocation differs from that Unless the integrity of the sheath is Symptoms Typically Experienced
of a typical lateral ankle sprain in that regained, painful dislocations of the Patients usually feel a sharp pain and/
it more closely follows the course of peroneal tendons can recur and severely or pop in the back of the ankle at the
the tendons posterior to the lateral limit the patient's activity. time of the rupture.
malleoli. With an uncomplicated lateral
ankle sprain, there is no pain over the Achilles Tendon Rupture Extent of Disability
peroneal tendons or sheath. The extent of disability is significant,
Mechanism of Injury although the pain following the acute
Radiographic Findings Achilles tendon rupture may result painful rupture may be minimal. The
In most cases, radiographs are unre- from an acute episode of ballistic patient can usually walk or limp on the
markable; however, a small avulsion stress that is placed on the tendon injured ankle, but walks flatfooted with
fracture of the posterior lateral during a physical activity, such as bas- the foot externally rotated to eliminate
malleolus may infrequently occur. This ketball, or from sudden, unexpected the toe-off phase of the gait, which
fragment is seen on the anterior views dorsiflexion of the ankle that occurs requires an intact Achilles tendon
of the ankle only, and confirms the with a seemingly benign action, complex.
diagnosis. such as stepping off an unseen curb.
Although usually considered an injury Examination Findings
Management of the younger athlete, Achilles tendon Achilles tendon ruptures occur 2 ½ to
Immobilization and referral to an rupture is common in both athletic 3 inches above the tendon's insertion
orthopaedic specialist is warranted and non-athletic persons 35 years and into the calcaneus (Figure 3). If there is
when the diagnosis is either strongly older. no soft tissue swelling, a defect in the
320 Medical Progress July 2010
orthopaedics
tendon may be visible and/or palpable
in this area. This defect is associated Figure 5.
with discrete tenderness. Although
the presence of soft tissue swelling
may obscure this defect, discrete ten-
derness will still be noted in this area
of the Achilles tendon—2½ to 3 inches
above the tendon's insertion into the
calcaneus. The Thompson test can be
used to evaluate the integrity of the
Achilles tendon. With the patient lying
prone with knees extended and feet
hanging over the end of the exami-
nation table, the examiner squeezes the
gastrocnemius muscles. The normal
response is a slight plantar flexion of
both ankles. The test is considered Patients who have chronic inflammation of the tibialis posterior tendon present with discomfort with or without
swelling posterior to the medial malleolus. Management is directed at prevention of rupture on the inflamed
positive for an Achilles tendon rupture
tendon.
when the amount of plantar flexion
of the affected foot is diminished or
absent compared with that in a normal Management Extent of Disability
foot (Figure 4). Immobilization and an orthopaedic The extent of disability is significant.
referral are warranted when the Patients are able to walk or limp on the
Radiographic Findings diagnosis is either strongly suspected injured ankle; however, they have an
No radiographic findings are associated or confirmed by the history and exami- altered gait as a result of the functional
with this injury. nation. For a successful outcome, loss of the contributions of the tibialis
definitive treatment, typically surgical posterior muscle to the sophisticated
repair, should be done within 5 to 10 motions of the ankle with ambulation.
days of the injury.
Examination Findings
Tibialis Posterior Tendon Patients may have discrete tenderness
Rupture
”The Thompson test is with or without swelling over the area
posterior and inferior to the medial
considered positive for an Mechanism of Injury
malleolus (Figure 5). The tibialis
A rupture of the tibialis posterior
Achilles tendon rupture tendon is the end result of attritional
posterior muscle, which is primarily
responsible for inversion of the foot, is
changes from chronic tendon inflam-
when the amount of mation. The rupture most commonly also an accessory plantar flexor of the
foot, and is one of the key structures
plantar flexion of the occurs with a seemingly benign activity.
that help maintain the foot arch. When
For unknown reasons, this injury is
affected foot is diminished seen primarily in women 45 years and the tibialis posterior tendon ruptures,
older. the patient's ability to actively invert the
or absent compared with plantar flexed foot and hold the foot in
inversion against manual resistance, is
that in a normal foot“ Symptoms Typically Experienced
The discomfort the patient feels at the greatly diminished on the affected side.
time of the rupture is minimal. In some With the patient standing, loss of the
cases, this discomfort is so minimal longitudinal arch of the involved foot
that loss of arch support is the patient's compared with the non-involved foot
chief complaint. is commonly detected.
Medical Progress July 2010 321
orthopaedics
Radiographic Findings.
No radiographic findings are associated By the time the patient with a significant soft tissue ankle injury is evaluated
with this injury. in the office, the findings are usually not as discrete to the area of injury as
they are when the ankle is examined immediately after the injury.
Management
Immobilization and orthopaedic
referral are warranted when the
diagnosis is either strongly suspected
or confirmed by the history and exami-
nation. Because of tendon attrition and
chronic inflammation, surgical repair
of tibialis posterior tendon rupture is
usually difficult, and the results of both
non-surgical treatment and surgery are
either very poor or poor in most cases.
Thus, the ideal management is pre-
vention of recurrence.
Preventive treatment includes rest,
anti-inflammatory medication, calf-
stretching exercises,1 and sometimes
immobilization, if all other conser-
vative measures fail to resolve tendon
tenderness. If the patient has pes
planus, the use of an over-the-counter
semi-rigid arch support (orthotic) may
be beneficial. Advise patients to refrain
from all activities until they have no
swelling or discomfort in the area and
have achieved adequate flexibility of
the calf muscles. Patients should be The mechanism of injury is resisted References
educated about the attritional changes inversion or forced eversion of the 1. Aronen JG, Garrick JG. Sports-induced inflammation in the
that occur when the inflammation is ankle. Patients feel a sharp pain and/ lower extremities. Hosp Pract (Milmeap). 1999;34:51–67.
not appropriately treated before their or pop in the area of the navicular on 2. Stiell IG, Greenberg GH, McKnight RD, et al. A study to
return to activities, and how these the superior mid-portion of the arch develop clinical decision rules for the use of radiology in
changes compromise the effectiveness at the time of the injury. The extent of acute ankle injuries. Ann Emerg Med. 1992;21:384–390.
of treatment. the disability is significant. Patients are A complete list of references can be obtained upon
forced to hobble or limp dramatically request from the editor.
Other Tibialis Posterior Tendon because of the pain. The examination
Injuries reveals discrete pain over the area of © 2009 CMP Healthcare Media LLC. Initially
Avulsion fractures of the tendon's the navicular, coupled with a decreased published in Consultant Dec 2009;49(12):734–
insertion site onto the navicular bone, ability to invert the plantar flexed foot 740.
and ruptures of the extreme distal and to resist manual eversion of the
portion of the tendon, have both been plantar flexed foot.
About the Authors
reported in younger athletes with a Treatment is immobilization and Dr Aronen is a consultant at the Center for Sports
previously healthy ankle. Both of these early orthopaedic referral for surgical Medicine at Saint Francis Memorial Hospital in San
injuries are described as infrequent; intervention. The surgical outcome Francisco. Dr Garrick is director at the Center for
however, health care providers should is excellent if these injuries are rec- Sports Medicine at Saint Francis Memorial Hospital.
be aware of them. ognized early.
322 Medical Progress July 2010
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Ashley Jones RN ResumeDocument1 pageAshley Jones RN Resumeapi-299649525100% (1)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Anamnesis & PemfisDocument81 pagesAnamnesis & PemfisFikriYTNo ratings yet
- At The DOCTOR Dialogues and Vocabulary ListDocument12 pagesAt The DOCTOR Dialogues and Vocabulary ListMax Tapia CastilloNo ratings yet
- Stress: Dr. Jayesh PatidarDocument56 pagesStress: Dr. Jayesh PatidarDr. Jayesh Patidar100% (2)
- Philippine Diabetes Prevention ProgramDocument19 pagesPhilippine Diabetes Prevention Programkoala100% (1)
- Enteral Feeding Nursing Care PlanDocument2 pagesEnteral Feeding Nursing Care PlanChebz Zy0% (1)
- Dialysis in Older PatientsDocument220 pagesDialysis in Older PatientsMiguel Angel Molinero100% (1)
- HSS Sotw 2017-18 ArDocument98 pagesHSS Sotw 2017-18 Arlf515No ratings yet
- Project Management HealthcareDocument29 pagesProject Management Healthcareiyad.alsabiNo ratings yet
- Communicating With Patients From Different Cultural BackgroundDocument24 pagesCommunicating With Patients From Different Cultural BackgroundRiska Aprilia100% (1)
- IDS Inmediate Dentin Sealing For Tooth Preparations... Magne 2014Document2 pagesIDS Inmediate Dentin Sealing For Tooth Preparations... Magne 2014Angie HernándezNo ratings yet
- AXR PresentationDocument30 pagesAXR PresentationLalit KumarNo ratings yet
- IVMS ICM-Heart MurmursDocument22 pagesIVMS ICM-Heart MurmursMarc Imhotep Cray, M.D.No ratings yet
- Nerve Entrapment - UpdateDocument17 pagesNerve Entrapment - UpdatealobrienNo ratings yet
- A Soft-Tissue Cephalometric Analysis and Its Use in Orthodontic Treatment Planning. Part IDocument28 pagesA Soft-Tissue Cephalometric Analysis and Its Use in Orthodontic Treatment Planning. Part IJorge Ramírez100% (1)
- Gastritis Treatment PlanDocument2 pagesGastritis Treatment PlanSuresh ThanneruNo ratings yet
- Practice Test On NutritionDocument6 pagesPractice Test On NutritionIvy Yvonne Quinico Malubag100% (1)
- HCW NigeriaDocument12 pagesHCW NigeriaFrancis Njihia KaburuNo ratings yet
- Diabetes - Oral KnowledgeDocument19 pagesDiabetes - Oral KnowledgeKSeegurNo ratings yet
- Rationale: Most Patients Prescribed To Receive Platelet Transfusions Exhibit Moderate ToDocument2 pagesRationale: Most Patients Prescribed To Receive Platelet Transfusions Exhibit Moderate TojoanneNo ratings yet
- Rhopalurus Junceus: and The Treatment of CancerDocument17 pagesRhopalurus Junceus: and The Treatment of CancerAmalia Tri UtamiNo ratings yet
- A Clinical Decision Support Framework ForDocument5 pagesA Clinical Decision Support Framework FordineshshaNo ratings yet
- TTM As5000brochureDocument12 pagesTTM As5000brochureAphichetNo ratings yet
- Toxi TestDocument4 pagesToxi TestFrank NobodNo ratings yet
- Using Lean Six Sigma Techniques To Improve Efficiency in Outpatient Ophthalmology ClinicsDocument9 pagesUsing Lean Six Sigma Techniques To Improve Efficiency in Outpatient Ophthalmology ClinicsMinh Nguyễn Phương HồngNo ratings yet
- Lung Cancer Types & TreatmentsDocument45 pagesLung Cancer Types & TreatmentsHowell Thomas Montilla AlamoNo ratings yet
- Improving Patient Safety in Radiotherapy by Learning From Near Misses, Incidents and ErrorsDocument5 pagesImproving Patient Safety in Radiotherapy by Learning From Near Misses, Incidents and ErrorsrosanaNo ratings yet
- 0315 DVTDocument28 pages0315 DVTEloisa TardioNo ratings yet
- Coombs Test FreddyDocument11 pagesCoombs Test FreddyFreddy Vallejo LeonNo ratings yet
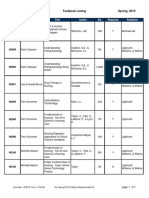
- BFLSON Course Textbook ListingDocument7 pagesBFLSON Course Textbook ListingWina ViqaNo ratings yet