Professional Documents
Culture Documents
Pathophysiology of Ketoacidosis in Type 2 Diabetes Mellitus
Uploaded by
Heredia A. MarcoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pathophysiology of Ketoacidosis in Type 2 Diabetes Mellitus
Uploaded by
Heredia A. MarcoCopyright:
Available Formats
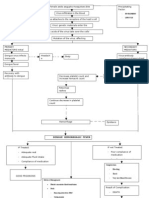
Pathophysiology of ketoacidosis in Type 2
Pathophysiology
Original article
Oxford, UK
Diabetic
DME
Blackwell
0742-3071
22 Article
Medicineof ketoacidosis
Publishing, Ltd.
2005 in Type 2 diabetes P. Linfoot et al.
diabetes mellitus
P. Linfoot, C. Bergstrom and E. Ipp
Abstract
Department of Medicine, Los Angeles Biomedical Aims Despite an increasing number of reports of ketoacidosis in populations
Research Institute at Harbor-UCLA Medical Center, with Type 2 diabetes mellitus, the pathophysiology of the ketoacidosis in these
Torrance, CA, USA
patients is unclear. We therefore tested the roles of three possible mechanisms:
Accepted 19 December 2005 elevated stress hormones, increased free fatty acids (FFA), and suppressed insulin
secretion.
Methods Forty-six patients who presented to the Emergency Department with
decompensated diabetes (serum glucose > 22.2 mmol /l and /or ketoacid concen-
trations ≥ 5 mmol /l), had blood sampled prior to insulin therapy. Three groups
of subjects were studied: ketosis-prone Type 2 diabetes (KPDM2, n = 13) with
ketoacidosis, non-ketosis-prone subjects with Type 2 diabetes (DM2, n = 15),
and ketotic Type 1 diabetes (n = 18).
Results All three groups had similar mean plasma glucose concentrations. The
degree of ketoacidosis (plasma ketoacids, bicarbonate and anion gap) in Type 1
and 2 subjects was similar. Mean levels of counterregulatory hormones (glucagon,
growth hormone, cortisol, epinephrine, norepinephrine), and FFA were not sig-
nificantly different in DM2 and KPDM2 patients. In contrast, plasma C-peptide
concentrations were approximately three-fold lower in KPDM2 vs. non-ketotic
DM2 subjects (P = 0.0001). Type 1 ketotic subjects had significantly higher
growth hormone (P = 0.024) and FFA (P < 0.002) and lower glucagon levels
(P < 0.02) than DM2.
Conclusions At the time of hospital presentation, the predominant mechanism
for ketosis in KPDM2 is likely to be greater insulinopenia.
Diabet. Med. 22, 1414–1419 (2005)
Keywords C-peptide, insulin, ketoacidosis, Type 2 diabetes
Abbreviations BMI, body mass index; FFA, free fatty acid; ICA, islet cell
antibody; KPDM2, ketosis-prone Type 2 diabetes; OHA, oral hypoglycaemic agent
findings that characterize the state of ketoacidosis: availability
Introduction of substrate (free fatty acids) and a ketogenic set of the liver
Ketoacidosis is a key clinical feature of Type 1 diabetes. The that is dependent in large part upon elevation of circulating
mechanisms have been extensively studied and are known to counterregulatory hormones [1–3]. However, it has become
be a result of the severe insulin deficiency that underlies this evident that ketoacidosis is no longer seen exclusively in Type 1
disease. Two other factors complete a triad of pathophysiological diabetes. A similar syndrome in Type 2 diabetes has now
been reported in numerous populations. Winter [4] first
described ketoacidosis in an inherited form of adolescent-onset
Correspondence to: Eli Ipp MD, Harbor-UCLA Medical Center, 1000 W. Carson Type 2 diabetes in African-Americans. In many of these
Street, Box 16, Torrance, CA 90509-2910, USA. E-mail: ipp@labiomed.org patients, insulin was discontinued later and their course
1414 © 2005 Diabetes UK. Diabetic Medicine, 22, 1414–1419
Original article 1415
was otherwise fairly typical Type 2 diabetes. Banerji [5] also Type 1 diabetes was also included in order to provide addition-
described ketoacidosis in black patients at onset or during the al comparative data in patients with a classical clinical presen-
course of Type 2 diabetes. Since then, this phenomenon has tation. However, we did not study patients with decompensated
been described in other ethnic groups by centres in the USA Type 1 diabetes any further after screening if they were not
[6–10] and world-wide [11– 16]. ketotic on biochemical analysis.
Subjects were placed into the Type 2 diabetic group if they
The pathogenic mechanisms identified in Type 1 diabetes
were islet antibody negative and in addition were treated with
have not been tested during ketoacidosis in Type 2 diabetes,
diet or oral hypoglycaemic agent (OHA) therapy prior to pres-
although subjects studied after resolution of ketoacidosis are entation. If diabetes was previously undiagnosed, subjects were
reported to be relatively insulin deficient [5,6,17]. An addi- classified as Type 2 if they met three criteria: islet cell antibody
tional explanation commonly provided for ketoacidosis in (ICA) negative, late-onset diabetes (age of onset ≥ 40 years or
Type 2 diabetes is increased severity of concomitant illnesses, > 35 years in Hispanics) and / or were overweight [body mass
with stress-induced elevation of counterregulatory hormones index (BMI) > 27 kg / m2]. Where possible, measurement of
proposed as a contributory factor [18]. We therefore set out to glucagon-stimulated C-peptide secretion at least 3 months after
evaluate the pathogenic triad in subjects with Type 2 diabetes presentation, or evidence for the absence of insulin dependency
and ketoacidosis. We tested whether counterregulatory (i.e. treatment with diet or OHAs) were obtained. Subjects were
hormone and/ or free fatty acid concentrations are higher in classified as Type 1 diabetes only if they fitted typical clinical
criteria of leanness, young age of onset of diabetes and insulin
patients at initial presentation with ketoacidosis in Type 2
use since diagnosis. This resulted in a group consistent with the
diabetes, compared with Type 2 patients and decompen-
Type 1 phenotype, with mean age of onset 26.0 ± 2.3 years and
sated diabetes who were not ketotic. In addition, we evaluated BMI 21.5 ± 0.7 kg / m2, respectively (Table 1). Antibodies were
insulin secretion during ketoacidosis in all subjects. Our not measured in this group.
results suggest that the pathophysiology of ketoacidosis The total patient population consisted of 30 men and 18
in Type 2 diabetes is associated primarily with severe insulin women. Ages at the time of presentation ranged from 21 to
deficiency. 90 years. Prior informed consent was obtained in the Emergen-
cy Department from all patients who participated in this study,
which was approved by the institution’s human subjects review
Materials and methods committee. All patients had routine admission laboratory
studies and were managed by the admitting medicine service in
Enrolment criteria an intensive care unit setting.
Any patient with serum glucose > 22.2 mmol / l and / or serum
ketones ≥ 1+ was eligible for enrolment. Subjects gave a complete Procedures
history and underwent full physical examination, and were
questioned about the time of their last meal and last use of Prior to starting insulin infusion (usually after initiation of fluid
alcohol. Clinical ketoacidosis for screening purposes was defined therapy), blood was sampled for estimation of C-peptide, glu-
by the presence of a metabolic acidosis with anion gap > 16 cagon, cortisol, growth hormone, epinephrine, norepinephrine,
mEq/l and serum ketones > 2+, measured semiquantitatively acetoacetate, β-hydroxybutyrate, lactate, pyruvate, and FFAs.
using the nitroprusside method. Ketosis was subsequently Where possible, ketotic subjects had a glucagon stimulation test
confirmed biochemically using quantitative radioenzymatic to assess β-cell secretory function after at least 3 months of out-
assays. Ketoacidosis was considered to be present if total patient treatment. Following an overnight fast, 1 mg of glucagon
serum ketones (acetoacetate and β-hydroxybutyrate) exceeded was injected intravenously. A plasma C-peptide concentration
5.0 mmol /l. > 0.6 nmol/l at 6 min post injection was defined as a Type 2
response [9,19].
Patients groups
Analytical methods
A non-consecutive, convenience sample was obtained of
patients who presented to the Harbor-UCLA Medical Center C-peptide, glucagon, cortisol, and growth hormone were meas-
Emergency Department with acutely decompensated diabetes ured by radioimmunoassay as previously described [20,21].
mellitus. We studied three groups of subjects. The primary Epinephrine and norepinephrine were measured by radioenzy-
study group consisted of patients with ketoacidosis who matic assays as described [20]. Acetoacetate, β-hydroxybutyrate,
appeared to have Type 2 diabetes (ketosis-prone Type 2 diabetes, lactate, and pyruvate were measured by enzymatic assays also
KPDM2). There were two control groups. The primary control previously described [22]. FFAs were measured using the color-
group consisted of subjects with typical Type 2 diabetes who imetric method of Falholt [23]. ICAs and insulin autoantibodies
presented to hospital with decompensated diabetes, but who were measured as described by Neufeld [24].
did not develop ketosis (DM2). Comparison between the two Statistical analyses were carried out using the Statview
groups of Type 2 diabetes allowed us to test which of the patho- program. ANOVA or χ2 analysis was used depending on whether
physiological triad—insulin deficiency, increased free fatty continuous or categorical data were used; post hoc analyses
acids (FFA) and / or counterregulatory excess— could account for were performed using Fisher’s PLSD test. Data are presented as
ketoacidosis. A second control group with ketoacidosis and mean ± SEM, unless otherwise indicated.
© 2005 Diabetes UK. Diabetic Medicine, 22, 1414–1419
1416 Pathophysiology of ketoacidosis in Type 2 diabetes • P. Linfoot et al.
Table 1 Clinical characteristics of study subjects
Age Prior Age of Duration BMI
DM type (years) therapy onset (years) (years) (kg/m2) Precipitant
Type 2 non-ketotic
1 52 None 52 0 33.2 None found
2 77 OHA 60 17 44.1 None found
3 52 OHA 36 16 25.2 Cellulitis
4 38 None 38 0 36.6 None found
5 62 OHA 58 4 25.4 UTI
5 39 None 39 0 34.2 None found
7 44 OHA 41 3 27.3 Non-compliance
8 60 None 60 0 22.6 Pneumonia
9 90 OHA 89 1 — Pneumonia
10 62 OHA 47 15 32.0 Non-compliance
11 41 None 41 0 32.4 None found
12 73 OHA — — — Urosepsis
13 71 Diet 50 21 22.3 Obstructive uropathy
14 53 None 53 0 46.0 Pyelonephritis
15 40 OHA 40 2 — Foot ulcer, non-compliance
Mean ± SEM 57 ± 4.1 50 ± 3.7 5.5 ± 2.1 31.8 ± 2.2
(N = 15)
Type 2 ketotic
16 36 None 36 0 — Sepsis (died)
17 38 None 38 0 32.7 None found
18 42 OHA 41 1 23.0 Cholecystitis
19 50 None 50 0 20.1 None found
20 21 OHA 21 0.25 32.1 Non-compliance
21 23 OHA 22 1 — Exudative pharyngitis
22 42 Insulin 38 4 24.4 Non-compliance
23 53 None 53 0 40.4 Buttock abscess
24 36 OHA 35 1 24.8 Non-compliance
25 48 OHA 45 3 22.0 Non-compliance
26 58 Insulin 48 10 24.8 Non-compliance
27 68 Diet 63 5 25.4 Cellulitis
28 25 None 25 0 43.1 None found
Mean ± SEM 41 ± 3.9a 39 ± 3.4b 1.9 ± 0.8 28.4 ± 2.3
(N = 13)
Type 1 ketotic
Mean ± SEM 35 ± 2.3c None or 26 ± 2.3d,e 9.3 ± 2.0f 21.5 ± 0.7g,h
(n = 18) insulin
a
P = 0.0036 and bP < 0.0247 vs. Type 2 non-ketotic. cP = 0.0247, eP < 0.0001 and gP < 0.0001 vs. Type 2 non-ketotic. dP < 0.0001, fP = 0.0076 and
h
P = 0.0061 vs. Type 2 ketotic.
BMI, Body mass index; OHA, oral hypoglycaemic agent; UTI, urinary tract infection.
as an out-patient. All of the remaining nine KPDM2 subjects
Results tested were ICA–. All subsequent statistical comparisons were
made between the following three groups: KPDM2, n = 13;
Classification of patients
DM2, n = 15; Type 1 ketotic, n = 18.
Of 48 patients entered into the study, the data from 46 were
analysed (Table 1). Two subjects first classified as non-ketotic
Clinical and demographic features
Type 2 diabetes were found to be ICA+, placing them in the
non-ketotic Type 1 category, and were excluded. ICAs were For the most part, the clinical characteristics of KPDM2
measured in all non-ketotic Type 2 and nine of 13 ketotic Type subjects were similar to those without ketosis (Table 1). Only
2 subjects. The four subjects in whom ICAs were not obtained the mean age of onset of diabetes was significantly lower in the
were retained in the KPDM2 group because they were success- ketotic subjects (P = 0.0247), though not as low as in the Type 1
fully managed subsequently with an OHA or, if they continued group (P = 0.0001). Duration of diabetes and the BMI were not
to be treated with insulin, were found to maintain adequate significantly different between the two Type 2 groups, though BMI
C-peptide secretory response to glucagon after several months was higher in both than in the Type 1 group (P < 0.0065).
© 2005 Diabetes UK. Diabetic Medicine, 22, 1414–1419
Original article 1417
Precipitating causes of metabolic decompensation were sim- from each other (Table 2). Ketoacids were predominantly
ilar in the two Type 2 groups (Table 1; note that more than one in the form of β-hydroxybutyrate (acetoacetate not shown).
cause was assigned to some subjects). The most common pre- Lactate (Table 2) and pyruvate (not shown) were similarly,
cipitant was infection in 7/ 15 of DM2 patients and 5 /13 of the mildly elevated in all three groups.
KPDM2 patients. Six patients had newly diagnosed diabetes in Mean concentrations of counterregulatory hormones and
the DM2 group and five in the KPDM2 group. In five DM2 FFA (Table 3) were not significantly different in KPDM2
and four KPDM2 subjects, no precipitating event could be and DM2, respectively. Epinephrine (661 ± 317 vs. 437 ± 164
found—in both groups, in most of these this was the first pres- pmol/ l), norepinephrine (7482 ± 1442 vs. 4716 ± 1093 pmol / l),
entation of diabetes. Non-compliance with medication may cortisol (772 ± 193 vs. 634 ± 110 nmol / l) and growth hormone
have been a factor in the decompensated diabetes of two DM2 (84 ± 42 vs. 60 ± 19 pmol/ l) were elevated, but not significantly,
subjects and five of the KPDM2 subjects. in the KPDM2 group. Plasma glucagon concentrations were
The demographic characteristics of the three groups were lower in the KPDM2 group (118 ± 15 vs. 200 ± 60 pmol/ l),
not similar. The Type 1 and DM2 patients were roughly evenly but also not significantly different from DM2. FFA levels upon
distributed between men and women; Type 1 ketotic (7 F/11 presentation were also not significantly different (673 ± 85 vs.
M) and DM2 (8 F /7 M). However, KPDM2 subjects were pre- 410 ± 42 µEq/ l, respectively). Type 1 ketotic patients showed
dominantly males (2 F/11 M). Type 1 diabetes occurred more some differences from the other two groups. Growth hormone
often in caucasians (10 C/ 5 AA/ 3 H), DM2 in Hispanics (8 H / concentrations were higher in Type 1 DM than in either of the
4 AA /3 C) and KPDM2 in African-American and Hispanic Type 2 groups (P = 0.0135 vs. DM2, P = 0.0240 vs. KPDM2).
subjects (6 AA / 5 H/ 2 C). In Type 1 patients, FFA concentrations (972 ± 190) were also
significantly higher ( P = 0.0017), and glucagon (74 ± 15),
significantly lower (P = 0.0189) than in the DM2 group; the
Metabolic and hormonal features
ketotic Type 1 and 2 subjects were not different.
The biochemical characteristics of the three groups are shown Plasma C-peptide concentrations at the time of presentation
in Table 2. All three groups had a similar degree of hypergly- are shown in Table 3. Type 1 ketotic patients had the lowest
caemia. The two ketotic groups had a similar decrease in plasma level of endogenous insulin secretion (0.118 ± 0.07 nmol/ l).
bicarbonate and comparable anion gap acidosis. pH in the KPDM2 patients had intermediate (0.463 ± 0.08 nmol/ l) and
KPDM2 was less than in the DM2 group, but not as low as in DM2 patients the highest C-peptide concentrations (1.245 ±
the Type 1 ketotic group. Levels of total plasma ketoacids were 0.184 nmol/ l). Mean C-peptide concentrations in KPDM2
elevated in both ketotic groups, and not significantly different subjects were almost three times less than in DM2 patients. Both
ketotic groups had mean C-peptide levels that were significantly
Table 2 Metabolic characteristics of subjects upon presentation to different from the non-ketotic DM2 group (P = 0.0001).
emergency room
Type 2 Type 2 Type 1 Discussion
DM type ketotic non-ketotic ketotic
The pathophysiology of ketoacidosis has been well described
Glucose (mmol/l) 31.2 ± 4.1 33.2 ± 4.1 31.3 ± 2.3 in Type 1 diabetes [1 – 3]. However, there is little information
Bicarbonate (mEq/l) 17 ± 0.8 22 ± 1.4 19.4 ± 1.5 on the pathophysiology of this metabolic state in Type 2
Anion gap (mEq/l) 16 ± 1.4 14.1 ± 1.5 19.9 ± 1.8 diabetes. This study provides a broad biochemical and hormonal
pH 7.30 ± 0.02 7.36 ± 0.04 7.22 ± 0.03
profile of ketoacidosis in patients with Type 2 diabetes, includ-
Total ketones (mmol/l) 9.0 ± 1.1 2.3 ± 0.4 11.8 ± 1.4
Lactate (mmol/l) 1.7 ± 0.4 1.4 ± 0.3 1.8 ± 0.3 ing FFAs, lactate, pyruvate and counterregulatory hormones
at presentation, and differs from previous studies of Type 2
Mean ± standard error of mean. ketoacidosis in a number of ways. First, previous studies of the
Table 3 Hormonal and free fatty acid (FFA)
values during presentation with ketoacidosis Type 2 Type 2 Type 1
ketotic non-ketotic ketotic
Epinephrine (pmol/l) 661 ± 317 437 ± 164 531 ± 208
Norepinephrine (pmol/l) 7482 ± 1442 4716 ± 1093 7454 ± 2134
Cortisol (nmol /l) 772 ± 193 634 ± 110 966 ± 193
Growth hormone (pmol/l) 84 ± 42 60 ± 19 567 ± 205a,b
Glucagon (pmol /l) 118 ± 15 200 ± 60 74 ± 15b
FFA (µEq/l) 673 ± 85 410 ± 42 972 ± 190c
C-peptide (nmol/l) 0.463 ± 0.08c 1.245 ± 0.184 0.118 ± 0.07c
Mean ± standard error of mean.
a
P = 0.024 vs. Type 2 ketotic. bP < 0.02 vs. Type 2 non-ketotic. cP < 0.002 vs. Type 2 non-ketotic.
© 2005 Diabetes UK. Diabetic Medicine, 22, 1414–1419
1418 Pathophysiology of ketoacidosis in Type 2 diabetes • P. Linfoot et al.
pathogenesis of ketoacidosis in Type 2 diabetes reported found to be similar in another group of similar patients that we
C-peptide only [6,17]. Second, those studies were carried out have since studied (J. Canales, personal communication)]; (ii)
after ketoacidosis had cleared [6,17]. Third, earlier compara- hypokalaemia can impair insulin secretion [28]; however,
tive studies of metabolic and hormonal pathogenesis such as potassium levels were similar in ketotic and non-ketotic
this did not distinguish between Type 1 and Type 2 DM; a subjects; (iii) prolonged fasting increases the rate of ketosis in
ketoacidosis group was compared with the hyperosmolar non- Type 1 subjects [29] and may decrease insulin secretion, but
ketotic state [2,25]. Thus, specific data on the pathogenesis of the number of subjects who had fasted for longer than 12 h did
Type 2 ketoacidosis are lacking, and the paucity of data in this not differ between the two groups (data not shown).
area of investigation was acknowledged in a recent technical Other factors that may have contributed to ketosis were
review [2]. considered. No evidence for increased stress [18] was found;
Comparison of our two groups with Type 2 diabetes reveals both Type 2 groups were similar with respect to: (i) precipitat-
that despite similar degrees of deterioration in glucose control, ing causes (Table 1), (ii) degree of elevation of counterregula-
ketotic patients displayed a clear-cut ketoacidosis distinct from tory hormones and (iii) severity of illness, evaluated indirectly
non-ketotic control subjects, and similar to Type 1 patients by measurement of serum osmolality and a blood urea nitrogen /
recruited in the same period. Because both Type 2 groups were creatinine ratio (data not shown). Alcohol may cause ketoaci-
otherwise comparable with respect to their clinical presenta- dosis, but does not explain insulinopenia [30]. Nor was there
tion, we were able to evaluate the respective contribution of a difference in the number of subjects reporting recent use of
the major mechanisms for ketoacidosis. The primary patho- alcohol in the Type 2 groups. Half of the KPDM2 subjects
physiological triad tested include (i) an excess of circulating denied prior use of alcohol at any time. Thus, although other
counterregulatory hormones; (ii) increased delivery of the pri- environmental factors cannot be ruled out, it is possible that
mary substrate for ketogenesis, i.e. FFAs; and (iii) diminished the insulinopenia observed in the KPDM2 subjects has a
insulin secretion [1–3]. This study demonstrates that, of these unique constitutional or genetic basis.
three factors, diminished insulin secretion (measured as Limitations of this study include the fact that we sampled at
C-peptide) during ketoacidosis best differentiates between the only one time point in the evolution of ketoacidosis in these
two groups with Type 2 diabetes. Mean C-peptide levels were patients. Prior to entry into the study, counterregulatory hor-
three-fold lower in the KPDM2 group. In contrast, plasma mone and FFA concentrations may have been different from those
concentrations of the counterregulatory hormones and FFAs observed, particularly if one takes into account the known
were not significantly different in the two groups with Type 2 pulsatility of many counterregulatory hormones [20]. Also,
diabetes. This suggests that increased substrate availability classification of patients as Type 1 or Type 2 diabetes is imper-
or hormonal stress do not explain increased ketogenesis in fect; in an attempt to deal with this problem, Maldonado et al.
Type 2 diabetes. However, it should be noted that the relatively [9] suggested that patients with ketoacidosis be classified into
small size of the groups studied precludes a definitive statement four groups, based upon the presence or absence of autoanti-
with respect to FFA and some (e.g. norepinephrine) but not bodies and / or evidence of residual insulin secretion subsequent
other (e.g. glucagon) counterregulatory hormones. Of note, to the episode of ketoacidosis. We recognize that some among
KPDM2 was associated with growth hormone levels similar to the four subjects in the Type 2 group with ketoacidosis in whom
DM2 patients, not the much higher concentrations seen in autoantibodies were not obtained could theoretically fall into
Type 1 ketoacidosis (Table 3). This suggests that high growth the Maldonado A+β+ group (antibody+; insulin secretion+),
hormone levels seen in Type 1 ketoacidosis [25] may be and therefore technically have Type 1 diabetes. Since even
enhanced by younger age or lower BMI, rather than ketoaci- in that study [9] this was a relatively rare occurrence (10% of
dosis per se [25]. In this study, C-peptide concentrations in the patients with ketoacidosis), it is unlikely that subjects of this
KPDM2 subjects were not significantly different from those in type would be of significant number in our KPDM2 group.
Type 1 diabetic patients. In summary, we evaluated the metabolic pathophysiology
Diminished insulin secretion is clearly the initial event in during ketoacidosis in patients with Type 2 diabetes. Our find-
ketoacidosis of Type 1 diabetes and thus is a logical mecha- ings indicate that β-cell dysfunction manifesting as severe insulin
nism for the syndrome seen in KPDM2. This is consistent with insufficiency is the most likely proximate cause for ketoacidosis
other studies that measured insulin or C-peptide long after res- in this setting.
olution of ketoacidosis [5]. The cause of severe insulinopenia
in Type 2 patients with ketoacidosis remains uncertain. In
many patients, insulin can be discontinued at a later date (e.g.
Competing interests
[5,15,16]), suggesting that severe insulin deficiency seen dur- None declared.
ing ketoacidosis later resolves in some cases. We therefore con-
sidered some of the possible transient causes of insulinopenia
Acknowledgements
in this clinical setting: (i) glucotoxicity impairs β-cell function
[26, 27]; yet ketotic and non-ketotic Type 2 subjects had We are indebted to Dr Noel Maclaren who performed the ICA
similar levels of hyperglycaemia at presentation [and HbA1c was measurements. We acknowledge the expert assistance of the
© 2005 Diabetes UK. Diabetic Medicine, 22, 1414–1419
Original article 1419
nursing and laboratory staff of the GCRC at Harbor-UCLA 15 Yu E, Guo H, Wu T. Factors associated with discontinuing insulin
Medical Center and we thank the subjects who agreed to therapy after diabetic ketoacidosis in adult diabetic patients. Diabet
Med 2001; 18: 895–899.
participate. These studies were supported in part by a grant
16 Sobngwi E, Vexiau P, Levy V, Lepage V, Mauvais-Jarvis F, Leblanc H
from the NIH to the GCRC at Harbor-UCLA Medical. et al. Metabolic and immunogenetic prediction of long-term insulin
Center (MO1-RR00425). remission in African patients with atypical diabetes. Diabet Med
2002; 19: 832–835.
17 Umpierrez GE, Woo W, Hagopian WA, Isaacs SD, Palmer JP,
References Gaur LK et al. Immunogenetic analysis suggests different pathogen-
esis for obese and lean African-Americans with diabetic ketoacidosis.
1 Ipp E, Westhoff T. Diabetes mellitus and the critically ill patient. In Diabetes Care 1999; 22: 1517–1523.
Bongard S ed. Current Diagnosis and Treatment in Critical Care, 2nd 18 Goldman L, Bennett JC. Cecil Textbook of Medicine, 21st edn.
edition. New York: Lange and McGraw Hill, 2002. Philadelphia: W.B. Saunders, 2000: 1263.
2 Kitabchi AE, Umpierrez GE, Murphy MB, Barrett EJ, Kreisberg RA, 19 Hother-Nielsen O, Faber O, Sorensen NS, Beck-Nielsen H. Classifi-
Malone JI et al. Management of hyperglycemic crises in patients with cation of newly diagnosed diabetic patients as insulin-requiring or
diabetes. Diabetes Care 2001; 24: 131–153. non-insulin-requiring based on clinical and biochemical variables.
3 McGarry JD, Foster DW. Regulation of hepatic fatty acid oxidation Diabetes Care 1988; 11: 531–537.
and ketone body production. Ann Rev Biochem 1980; 49: 395–420. 20 Genter P, Berman N, Jacob M, Ipp E. Counterregulatory hormones
4 Winter WE, Maclaren NK, Riley WJ, Clarke DW, Kappy MS, oscillate during steady state hypoglycemia. Am J Physiol 1998; 275:
Spillar RP. Maturity-onset diabetes of youth in black Americans. E821–829.
N Engl J Med 1987; 316: 285–291. 21 Ipp E, Sinai Y, Forster B, Cortez C, Baroz B, Nesher R et al. A glucose
5 Banerji MA, Chaiken RL, Huey H, Tuomi T, Norin AJ, Mackay IR reduction challenge in the differential diagnosis of fasting hypoglyc-
et al. GAD antibody negative NIDDM in adult black subjects with emia: a two center study. J Clin Endocrinol Metab 1990; 70: 711–
diabetic ketoacidosis and increased frequency of human leukocyte 717.
antigen DR3 and DR4. Diabetes 1994; 43: 741–745. 22 Cooper DM, Barstow TJ, Lee W-NP. Blood glucose turnover during
6 Umpierrez GE, Casals MM, Gebhart SP, Mixon PS, Clark WS, high and low intensity exercise. Am J Physiol 1989; 257: E405–
Phillips LS. Diabetic ketoacidosis in obese African-Americans. E412.
Diabetes 1995; 44: 790–795. 23 Falholt K, Lund B, Falholt W. An easy colorimetric micromethod for
7 Wilson C, Krakoff J, Gohdes D. Ketoacidosis in Apache Indians with routine determination of free fatty acids in plasma. Clin Chim Acta
non-insulin-dependent diabetes mellitus. Arch Intern Med 1997; 1973; 46: 105–111.
157: 2098–2101. 24 Neufeld M, Maclaren NK, Riley WJ, Lezotte D, McLaughlin JV,
8 Balasubramanyam A, Zern JW, Hyman DJ, Pavlik V. New profiles of Silverstein J et al. Islet cell and other organ-specific antibodies in U.S.
diabetic ketoacidosis: type 1 vs. type 2 diabetes and the effect of Caucasians and Blacks with insulin-dependent diabetes mellitus.
ethnicity. Arch Intern Med 1999; 159: 2317–2322. Diabetes 1980; 29: 589–592.
9 Maldonado M, Hampe CS, Gaur LK, D’Amico S, Iyer D, Hammerle LP 25 Chupin M, Charbonnel B, Chupin F. C-peptide blood levels in
et al. Ketosis-prone diabetes: dissection of a heterogeneous syndrome ketoacidosis and in hyperosmolar non-ketotic diabetic coma. Acta
using an immunogenetic and β-cell functional classification, prospec- Diabet Lat 1981; 18: 123–128.
tive analysis and clinical outcomes. J Clin Endocrinol Metab 2003; 26 Unger RH, Grundy S. Hyperglycemia as an inducer as well as a con-
88: 5090–5098. sequence of impaired islet cell function and insulin resistance:
10 Linfoot PA, Ipp E. Ketoacidosis in Type 2 diabetes mellitus: presence implications for management of diabetes. Diabetologia 1985; 28:
of insulin deficiency. Proceedings of the Endocrine Society Meeting 119–121.
1993. 27 Leahy JR, Cooper HE, Deal DA, Weir GC. Chronic hyperglycemia is
11 Aizawa T, Katakura M, Taguchi N, Kobayashi H, Aoyagi E, associated with impaired glucose influence on insulin secretion: a
Hashizume K et al. Ketoacidosis-onset noninsulin dependent study in normal rats using chronic in vivo glucose infusions. J Clin
diabetes in Japanese subjects. Am J Med Sci 1995; 310: 198–201. Invest 1986; 77: 908–915.
12 Zouvanis M, Pieterse AC, Seftel HC, Joffe BI. Clinical characteristics 28 Plavinik FL, Rodrigues CIS, Zanella MT, Ribiero AB. Hypokalemia,
and outcome of hyperglycaemic emergencies in Johannesburg Africans. glucose intolerance, and hyperinsulinemia during diuretic therapy.
Diabet Med 1997; 14: 603–606. Hypertension 1992; 19 (Suppl. II): 26–29.
13 Tan KC, Mackay IR, Zimmet PZ, Hawkins BR, Lam KS. Metabolic 29 Burge MR, Hardy KJ, Schade DS. Short-term fasting is a mechanism
and immunologic features of Chinese patients with atypical diabetes for the development of euglycemic ketoacidosis during periods
mellitus. Diabetes Care 2000; 23: 335–338. of insulin deficiency. J Clin Endocrinol Metab 1993; 76: 1192–
14 Pitteloud N, Philippe J. Characteristics of Caucasian type 2 diabetic 1198.
patients during ketoacidosis and at follow-up. Schweiz Med 30 Fulop M. Alcoholic ketoacidosis. Endocrinol Metab Clinics 1993;
Wochenschr 2000; 130: 576–582. 22: 209–219.
© 2005 Diabetes UK. Diabetic Medicine, 22, 1414–1419
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Position PaperDocument16 pagesPosition PaperMathew McCarthyNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Cir 0000000000000628Document101 pagesCir 0000000000000628Diana AngelesNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Cir 0000000000000628Document101 pagesCir 0000000000000628Diana AngelesNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Cir 0000000000000628Document101 pagesCir 0000000000000628Diana AngelesNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Cir 0000000000000628Document101 pagesCir 0000000000000628Diana AngelesNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Thalassemias and Hemolytic AnemiasDocument43 pagesThe Thalassemias and Hemolytic AnemiasAnonymous elq7jZiSNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- MRCP Recalls May 2014Document15 pagesMRCP Recalls May 2014sohailsu100% (1)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Past Paper Questions and AnswersDocument61 pagesPast Paper Questions and AnswerssophiaNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- MCQ For University Exam Chapter-Wise: For More Join Us On TelegramDocument6 pagesMCQ For University Exam Chapter-Wise: For More Join Us On TelegramDrug ViralNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Integumentary 2Document13 pagesIntegumentary 2api-302885118No ratings yet
- Blood GroupDocument12 pagesBlood Groupalive computerNo ratings yet
- Cancer Detection by GraphologyDocument5 pagesCancer Detection by GraphologyEndy Mulio100% (1)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Protein Structure Powerpoint Presentation Newest Pink and PurpleDocument21 pagesProtein Structure Powerpoint Presentation Newest Pink and Purpleapi-281150432No ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- PCR 5 Lab SetupDocument22 pagesPCR 5 Lab Setupptz1965No ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- 1.1 Fields and Careers in BiologyDocument5 pages1.1 Fields and Careers in BiologyFHATIN AMIRA BINTI MUSA MoeNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Krizia Joy Borromeo-Galve, MD: Bulacan Medical Center, Department of PediatricsDocument84 pagesKrizia Joy Borromeo-Galve, MD: Bulacan Medical Center, Department of PediatricsTara Oliveros Dela CruzNo ratings yet
- Your Health Today Choices in A Changing Society 5th Edition Teague Test BankDocument29 pagesYour Health Today Choices in A Changing Society 5th Edition Teague Test Banktaylorruiznqfpogxske100% (17)
- Tumor Markers in Common UseDocument10 pagesTumor Markers in Common Usethoai doan vanNo ratings yet
- Calbiochem InhibitorsDocument124 pagesCalbiochem InhibitorsChazMarloweNo ratings yet
- Spatial Transcriptomics Reveals Distinct and Conserved Tumor Core and Edge Architectures That Predict Survival and Targeted Therapy ResponseDocument61 pagesSpatial Transcriptomics Reveals Distinct and Conserved Tumor Core and Edge Architectures That Predict Survival and Targeted Therapy Response戴义宾No ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Seizure Disorders: Musupila.M DCM, Adgm, BSC Cs (Unza) 6 November 2019Document26 pagesSeizure Disorders: Musupila.M DCM, Adgm, BSC Cs (Unza) 6 November 2019Emmanuel MukukaNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Excretion and HomeostasisDocument31 pagesExcretion and HomeostasiscsamarinaNo ratings yet
- PHILIPPINES Asthma Consensus Guidelines 2009Document134 pagesPHILIPPINES Asthma Consensus Guidelines 2009Sirias_black50% (2)
- Cells of The Immune SystemDocument38 pagesCells of The Immune SystemprabuNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- About The Measure Domain MeasureDocument3 pagesAbout The Measure Domain MeasureMaríaA.SerranoNo ratings yet
- Epidemiological Trends in Skin Mycoses Worldwide: Blanka Havlickova, Viktor A. Czaika and Markus FriedrichDocument14 pagesEpidemiological Trends in Skin Mycoses Worldwide: Blanka Havlickova, Viktor A. Czaika and Markus FriedrichRS Tk IV PekanbaruNo ratings yet
- Improving Eyesight With Red Light TherapyDocument23 pagesImproving Eyesight With Red Light TherapyMark Sloan100% (8)
- Efflux-Mediated Antimicrobial Resistance in Bacteria - Mechanisms, Regulation and Clinical Implications-ADIS (2016)Document850 pagesEfflux-Mediated Antimicrobial Resistance in Bacteria - Mechanisms, Regulation and Clinical Implications-ADIS (2016)jenny joseNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- 6101 01 MSC 20080611Document17 pages6101 01 MSC 20080611sg noteNo ratings yet
- In2Med HaematologyDocument30 pagesIn2Med Haematologye148659No ratings yet
- Rheumatoid ArthritisDocument38 pagesRheumatoid ArthritisOlga GoryachevaNo ratings yet
- Hepatitis C Virus Encoded Antigen DetectionDocument25 pagesHepatitis C Virus Encoded Antigen DetectionPrasanth GovindanNo ratings yet
- Causes of MiscarriageDocument7 pagesCauses of MiscarriageClaire Nimor VentulanNo ratings yet
- Pathophysio DHF EDITEDDocument3 pagesPathophysio DHF EDITEDricmichael100% (1)
- Pancreas Anatomy and PhysiologyDocument34 pagesPancreas Anatomy and PhysiologySourabh MishraNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)