Professional Documents
Culture Documents
Differential Diagnosis of The Diseases With Systolic Murmurs
Uploaded by
Xiang Yun Tan0 ratings0% found this document useful (0 votes)
282 views2 pagesThe document discusses the differential diagnosis of diseases that cause systolic murmurs. It describes the characteristics of various types of systolic murmurs including midsystolic ejection murmurs, holosystolic (pansystolic) murmurs, and early and late systolic murmurs. Causes of these murmurs include valvular diseases like mitral regurgitation and tricuspid regurgitation, ventricular septal defects, and obstructions of the semilunar valves. The document provides details on the locations, timings, and other clinical findings that help distinguish between murmurs from different underlying diseases.
Original Description:
Original Title
Differential diagnosis of the diseases with systolic murmurs
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe document discusses the differential diagnosis of diseases that cause systolic murmurs. It describes the characteristics of various types of systolic murmurs including midsystolic ejection murmurs, holosystolic (pansystolic) murmurs, and early and late systolic murmurs. Causes of these murmurs include valvular diseases like mitral regurgitation and tricuspid regurgitation, ventricular septal defects, and obstructions of the semilunar valves. The document provides details on the locations, timings, and other clinical findings that help distinguish between murmurs from different underlying diseases.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
282 views2 pagesDifferential Diagnosis of The Diseases With Systolic Murmurs
Uploaded by
Xiang Yun TanThe document discusses the differential diagnosis of diseases that cause systolic murmurs. It describes the characteristics of various types of systolic murmurs including midsystolic ejection murmurs, holosystolic (pansystolic) murmurs, and early and late systolic murmurs. Causes of these murmurs include valvular diseases like mitral regurgitation and tricuspid regurgitation, ventricular septal defects, and obstructions of the semilunar valves. The document provides details on the locations, timings, and other clinical findings that help distinguish between murmurs from different underlying diseases.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 2
Differential diagnosis of the diseases with which is normal in VSD but it is widely split in
systolic murmurs pulmonary stenosis.
However, VSD is almost always pansystolic where
In answering this question, we have to first get to know the murmur of pulmonary stenosis is diamond-
the types of systolic murmurs and associated diseases. shaped and ends clearly before S2.
Many innocent murmurs also arise from this location
Systolic murmurs start at or after S1 and end before or but S1 and S2 must split normally.
at S2.
There are a few types of systolic murmurs
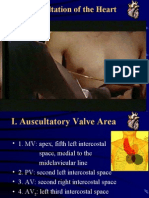
1.Midsystolic ejection murmurs Dilation of aortic root or pulmonary artery
– Mid-systolic murmurs begin after S1, have a Produces an ejection sound, with a short ejection
crescendo-decrescendo shape, and end before S2. systolic murmur and a relatively wide split S2. There is
Brief gaps are audible between the murmurs and no hemodynamic abnormality. This is similar to
the normal heart tones. The gap before S2 is often pulmonary hypertension except the latter has
easier to discern and usually confirms the murmurs hemodynamic instabilities.
as midsystolic. Midsystolic murmurs are often
related to the blood flow across the semilunar Increased semilunar blood flow
valves. This can occur in situations such as anemia,
pregnancy, or thyrotoxicosis.
– Midsystolic ejection murmurs are due to blood flow
through the semilunar valves. They occur at the
Aortic valve sclerosis
start of blood ejection, which start after S1, and
This is due to degenerative thickening of the roots of
end with the cessation of the blood flow, which is
the aortic cusps but produces no obstruction and no
before S2. Therefore, the onset of a midsystolic
hemodynamic instability and thus should be
ejection murmur is separated from S1 by the
differentiated from aortic stenosis. It is heard over right
isovolumic contraction phase; the cessation of the
second intercostals space with a normal carotid pulse
murmur and the S2 interval is the aortic or
and normal S2.
pulmonary hangout time. The resultant
configuration of this murmur is a crescendo-
Innocent midsystolic murmurs
decrescendo murmur.
These murmurs are not accompanied by other
– Causes of midsystolic ejection murmurs include abnormal findings. One example is Still's murmur in
outflow obstruction, increased flow through normal children.
semilunar valves, dilation of aortic root or
pulmonary trunk, or structural changes in the
1.Holosystolic (pansystolic) murmurs
semilunar valves without obstruction.
Usually due to regurgitation in cases such as mitral
regurgitation, tricuspid regurgitation, or ventricular
Aortic outflow obstruction
septal defect (VSD)
Murmurs can be due to aortic valve stenosis or
These murmurs start at S1 and extend up to S2
hypertrophic cardiomyopathy (HCM), with a harsh and
rough quality
Mitral regurgitation
Valvular aortic stenosis can produce a harsh or even In the presence of incompetent mitral valve, the
pressure in the L ventricle becomes greater than that
a musical murmur over the right second intercostals
in the L atrium at the onset of isovolumic contraction,
space which radiates into the neck over the two
which corresponds to the closing of the mitral valve
carotid arteries. The most common cause of AS
(S1). This explains why the murmur in MR starts at
(Aortic Stenosis) is calcified valves due to aging
the same time as S1. This difference in pressure
followed by congenital bicuspid aortic valves (normal
extends throughout systole and can even continue
valve is tricuspid). The distinguishing feature
after aortic valve has closed, explaining how it can
between these two causes is that bicuspid AS has
sometimes drown the sound of S2.
little or no radiation. It can be confirmed if it also has
an aortic ejection sound, a short early diastolic
The murmur in MR is high pitched and best heard at
the apex with diaphragm of the stethoscope with
murmur, and normal carotid pulse. The murmur in
patient in the lateral decubitus position.
valvular AS decreases with standing and straining
with Valsalva maneuver. Left ventricular function can be assessed by
determining the apical impulse. A normal or
hyperdynamic apical impulse suggests good ejection
Supravalvular aortic stenosis is loudest at a point
fraction and primary MR. A displaced and sustained
slightly higher than in that of valvular AS and may
apical impulse suggests decreased ejection fraction
radiate more to the right carotid artery.
and chronic and severe MR.
Subvalvular aortic stenosis is usually due to Tricuspid insufficiency
hypertrophic cardiomyopathy (HCM), with murmur
loudest over the left sternal border or the apex. The
Can be best heard over the fourth left sternal border.
murmur in HCM increases in intensity with a standing The intensity can be accentuated following
position as well as straining with Valsalva maneuver. inspiration (Carvallo's sign) due to increased
regurgitant flow in right ventricular volume.
Pulmonic outflow obstruction Tricuspid regurgitation is most often secondary to
A harsh murmur usually on left second intercostals pulmonary hypertension.
space radiating to left neck and accompanied by Primary tricuspid regurgitation is less common and
palpable thrill. It can be distinguished from a VSD can be due to bacterial endocarditis following IV drug
(Ventricular Septal Defect) by listening to the S2,
use, Ebstein's anomaly, carcinoid disease, or prior (Main answer for this question is DDx for diseases
right ventricular infarction. causing aortic stenosis, so can refer to question no. 29)
Ventricular septal defect
VSD is a defect in the ventricular wall, producing a
shunt between the left and right ventricles.
Since the L ventricle has a higher pressure than the
R ventricle, flow during systole occurs from the L to R
ventricle, producing the holosystolic murmur. It can
be best heard over the left third and fourth
intercostals spaces and along the sternal border.
It is associated with normal pulmonary artery
pressure and thus S2 is normal. This fact can be used
to distinguish from pulmonary stenosis, which has a
wide splitting S2.
If the shunt becomes reversed in the Eisenmenger
complex because the L ventricle becomes too "tired",
the murmur may be absent and S2 can become
markedly accentuated and single.
1.Early systolic murmur
– Early systolic murmurs begin with S1, decrescendo,
and end well before S2
– These murmurs are almost identical to holosystolic
murmurs, which start at S1 but ends before S2. It is
also associated with MR, TR, or VSD. The reason an
early systolic murmur is heard rather than a
holosystolic murmur is because the condition is
more acute and more severe.
1. Late systolic murmurs
– Late systolic murmurs begin in mid to late systole,
crescendo, and end at S2. An example of a late
systolic murmur would be the murmur of a
prolapsed mitral valve.
– Late systolic murmurs start after S1 and, if left
sided, extend up to S2, usually in a crescendo
manner.
– Causes include mitral valve prolapse, tricuspid
valve prolapse, and papillary muscle dysfunction.
Mitral valve prolapse
This is the most common cause of late systolic
murmurs.
It can be heard best over the apex of the heart,
usually preceded by clicks.
The most common cause of mitral valve prolapse is
"floppy" valve (Barlow's) syndrome.
If the prolapse becomes severe enough, mitral
regurgitation may occur.
Any maneuver that decreases left ventricular
volume, such as standing, sitting, Valsalva
maneuver, and amyl nitrate inhalation, can produce
earlier onset of clicks, longer murmur duration, and
decreased murmur intensity.
Any maneuver that increases left ventricular volume,
such as squatting, elevation of legs, hand grip, and
phenylephrine, can delay the onset of clicks, shorten
murmur duration, and increase murmur intensity.
Tricuspid valve prolapse
Uncommon without concomitant mitral valve
prolapse.
Best heard over left lower sternal border.
Papillary muscle dysfunction
Usually due to acute myocardial infarction or
ischemia which causes mild mitral regurgitation.
You might also like
- Heart Sounds: Mitral Regurgitation Congestive Heart FailureDocument6 pagesHeart Sounds: Mitral Regurgitation Congestive Heart FailurecindyNo ratings yet
- Cardiovascular Examination: Andi Wahjono Adi, MD, FihaDocument34 pagesCardiovascular Examination: Andi Wahjono Adi, MD, FihaAmira FRNo ratings yet
- Heart MurmursDocument18 pagesHeart MurmursRobby Wiranata WijayaNo ratings yet
- 01 Interview FormDocument7 pages01 Interview FormSavage SkylenNo ratings yet
- Cardiology Arteritis ChartDocument3 pagesCardiology Arteritis ChartM PatelNo ratings yet
- STEP 1 ChecklistDocument11 pagesSTEP 1 ChecklistHasan Khan RoudbaryNo ratings yet
- Cardiology ConsultsDocument2 pagesCardiology ConsultsjuweriyNo ratings yet
- Ebp HandoutDocument2 pagesEbp Handoutapi-543558169No ratings yet
- Cardiovascular Nursing: Study Online atDocument7 pagesCardiovascular Nursing: Study Online atLilly DayeNo ratings yet
- Auscultation of HeartDocument92 pagesAuscultation of Heartsanjivdas100% (1)
- History and Physical Examination Outline (See Pediatric Supplement For Patients Under Age 18)Document2 pagesHistory and Physical Examination Outline (See Pediatric Supplement For Patients Under Age 18)Isaac SuNo ratings yet
- Chief Complaint FormatDocument3 pagesChief Complaint Formatkazniels100% (1)
- Weekly Clinical Prep Packet 12 REVISEDDocument12 pagesWeekly Clinical Prep Packet 12 REVISEDMei SarteNo ratings yet
- Advanced 12-Lead InterpretationDocument30 pagesAdvanced 12-Lead InterpretationRohini SelvarajahNo ratings yet
- Mo Intern Handbook - FinalDocument37 pagesMo Intern Handbook - FinalGideon K. MutaiNo ratings yet
- Anaesthesia and Atrial FibrillationDocument15 pagesAnaesthesia and Atrial FibrillationNaresh Dhawan100% (1)
- Musculoskeletal System: Dr. Dipti RamaniDocument30 pagesMusculoskeletal System: Dr. Dipti Ramaniaarti HingeNo ratings yet
- LV RV FailureDocument118 pagesLV RV FailureMirza Thaariq HapsitoNo ratings yet
- Ekg FastlaneDocument10 pagesEkg FastlaneAida UzunovicNo ratings yet
- Right Side EcgDocument4 pagesRight Side EcgDragos CirsteaNo ratings yet
- Format of History and PEDocument2 pagesFormat of History and PEJill Eizavel BertisNo ratings yet
- IMD - Step-Up To USMLE Step 3 - Chapter 1 - CardiologyDocument124 pagesIMD - Step-Up To USMLE Step 3 - Chapter 1 - CardiologyAly SherifNo ratings yet
- Cvs PracticalDocument63 pagesCvs PracticalSreedeep TejaNo ratings yet
- Internal Medicine Topic List 2015Document3 pagesInternal Medicine Topic List 2015Krystal Mae LopezNo ratings yet
- Classification of MurmursDocument2 pagesClassification of MurmursNazneen SiddiquiNo ratings yet
- USMLE Step 2 CK 6 Months Study Plan For 240Document1 pageUSMLE Step 2 CK 6 Months Study Plan For 240DhritisdiaryNo ratings yet
- HEENT Cheat SheetDocument22 pagesHEENT Cheat SheetKatrina FeriNo ratings yet
- CVS NotesDocument26 pagesCVS NotesKelly YeowNo ratings yet
- Heart SoundsDocument56 pagesHeart SoundsBetsy Babilonia100% (1)
- Epithelial TissueDocument7 pagesEpithelial TissueJoan PaulineNo ratings yet
- Pathophys ComplicationsOfPregnancy 2020 21Document11 pagesPathophys ComplicationsOfPregnancy 2020 21JohnNo ratings yet
- 20 Lower Urinary Tract and Male Reproductive DisordersDocument23 pages20 Lower Urinary Tract and Male Reproductive Disordersndnplaya712No ratings yet
- ECG Interpretation in One PageDocument2 pagesECG Interpretation in One PageRyan AycockNo ratings yet
- Pharm Fall Cardiovascular Pharmacology Study Guide-106Document47 pagesPharm Fall Cardiovascular Pharmacology Study Guide-106sean liyanageNo ratings yet
- CVS Examination 3rd MBDocument30 pagesCVS Examination 3rd MBsnowlover boyNo ratings yet
- Outline For History TakingDocument2 pagesOutline For History TakingBlancheNo ratings yet
- Trusted Evidence For Confident Clinical Decisions: Resources For Medication, Disease, and ToxicologyDocument10 pagesTrusted Evidence For Confident Clinical Decisions: Resources For Medication, Disease, and ToxicologyCurcubeuAuroraNo ratings yet
- Cardiac Murmurs - 1p Cheat Sheet PDFDocument1 pageCardiac Murmurs - 1p Cheat Sheet PDFPkernNo ratings yet
- Heart SoundsDocument4 pagesHeart SoundsAthieNo ratings yet
- Approach To The Cardiovascular Examination567 160120085414 PDFDocument22 pagesApproach To The Cardiovascular Examination567 160120085414 PDFHNINNo ratings yet
- Cerebral Blood FlowDocument39 pagesCerebral Blood FlowRajat ThakurNo ratings yet
- Associations USMLEDocument99 pagesAssociations USMLEnu.bombinaNo ratings yet
- Post-Cardiac Arrest Therapeutic Hypothermia Targeted Temperature Manangement (TTM) Quick SheetDocument3 pagesPost-Cardiac Arrest Therapeutic Hypothermia Targeted Temperature Manangement (TTM) Quick SheetkimberlyNo ratings yet
- Intern Survival Guide 2014-2015Document145 pagesIntern Survival Guide 2014-2015Katie Kroll BradyNo ratings yet
- Taking A History NotesDocument3 pagesTaking A History NotesMarkNo ratings yet
- Medical Mnemonic BookletDocument14 pagesMedical Mnemonic Bookletahmed abd elazizNo ratings yet
- Week 10 - Hypertension, Atherosclerosis, ArrhythmiaDocument14 pagesWeek 10 - Hypertension, Atherosclerosis, Arrhythmiashivani patel100% (1)
- Cardiac Pacing: Terms You Will Become Familiar With in This Section of TheDocument21 pagesCardiac Pacing: Terms You Will Become Familiar With in This Section of TheClt Miskeen100% (1)
- (MED II) 1.05 Emergencies in Cancer PatientsDocument17 pages(MED II) 1.05 Emergencies in Cancer PatientsJearwin AngelesNo ratings yet
- PE by PositionDocument8 pagesPE by PositionaznpianodreamNo ratings yet
- Patterns of RespirationDocument67 pagesPatterns of Respirationsteven hkNo ratings yet
- Heart SoundsDocument2 pagesHeart Soundsdanny_awwadNo ratings yet
- Valvular Heart Disease: Presented by DR Mirjana Milutinovic Professor, SJSMDocument69 pagesValvular Heart Disease: Presented by DR Mirjana Milutinovic Professor, SJSMAbanoub AwadallaNo ratings yet
- PE, Tamponade, Constrictive PericarditisDocument1 pagePE, Tamponade, Constrictive PericarditisKaylee HvezdaNo ratings yet
- Guidelines For The Diagnosis and Treatment of Chronic Heart FailureDocument26 pagesGuidelines For The Diagnosis and Treatment of Chronic Heart FailurecubewormNo ratings yet
- Mid-Systolic Ejection: Time Condition DescriptionDocument3 pagesMid-Systolic Ejection: Time Condition DescriptionZahrosofi AhmadahNo ratings yet
- IVMS Heart and Lung Auscultation Sounds NotesDocument7 pagesIVMS Heart and Lung Auscultation Sounds NotesMarc Imhotep Cray, M.D.No ratings yet
- Heart Murmurs Topic Review - From Description To AuscultationDocument15 pagesHeart Murmurs Topic Review - From Description To AuscultationRapmle PrasadNo ratings yet
- Gangguan Bunyi JantungDocument3 pagesGangguan Bunyi JantungDewiDwipayantiGiriNo ratings yet
- Gangguan Bunyi JantungDocument3 pagesGangguan Bunyi JantungDewiDwipayantiGiriNo ratings yet
- Efficacy of Nerve Flossing Technique On Improving Sciatic Nerve Function in Patients With Sciatica - A Randomized Controlled TrialDocument10 pagesEfficacy of Nerve Flossing Technique On Improving Sciatic Nerve Function in Patients With Sciatica - A Randomized Controlled Trialsphadungkit100% (1)
- CHAPTER 11: The History and Physical Examination: An Evidence Based ApproachDocument5 pagesCHAPTER 11: The History and Physical Examination: An Evidence Based ApproachReda SoNo ratings yet
- Multiple SclerosisDocument96 pagesMultiple SclerosisDrGasnasNo ratings yet
- Acid Base WorkshopDocument71 pagesAcid Base WorkshopLSU Nephrology Transplant Dialysis AccessNo ratings yet
- Performance Checklist Enema NOT DoneDocument1 pagePerformance Checklist Enema NOT DoneMhel MG100% (1)
- Osnove FarmakokinetikeDocument46 pagesOsnove Farmakokinetikeapi-3814389No ratings yet
- Scalar Wave Morphogenetic Field Mechanic PDFDocument135 pagesScalar Wave Morphogenetic Field Mechanic PDFMokhtar Mohd100% (7)
- European Pharmacopoeia 7 0 PDFDocument1 pageEuropean Pharmacopoeia 7 0 PDFMercedesNo ratings yet
- (Final Proposal) 20181220 Beauttah Migiro Akuma - Research Proposal - Right To Health - Version 1.0Document14 pages(Final Proposal) 20181220 Beauttah Migiro Akuma - Research Proposal - Right To Health - Version 1.0Brian BeauttahNo ratings yet
- Daftar ObatDocument1 pageDaftar ObatPramukadua DepokNo ratings yet
- R7 US CatalogDocument476 pagesR7 US CatalogmatzoneNo ratings yet
- VA DoD Management of Concussion Mild Traumatic Brain InjuryDocument112 pagesVA DoD Management of Concussion Mild Traumatic Brain InjurycirtestNo ratings yet
- Textbook of Medical Parasitology Protozoology HelmDocument2 pagesTextbook of Medical Parasitology Protozoology HelmAnge OuedraogoNo ratings yet
- Genetic Engineering Applications in Animal BreedingDocument6 pagesGenetic Engineering Applications in Animal BreedingFadilla HadiwijayaNo ratings yet
- BIS A2000 - Operating ManualDocument102 pagesBIS A2000 - Operating Manualgabygg06No ratings yet
- Laboratory Test Report: Test Name Result Biological Reference Interval Fasting Plasma Glucose: 102Document3 pagesLaboratory Test Report: Test Name Result Biological Reference Interval Fasting Plasma Glucose: 102Ramesh KumarNo ratings yet
- Republic of Kenya: Application For Registration of A Health InstitutionDocument13 pagesRepublic of Kenya: Application For Registration of A Health InstitutionianNo ratings yet
- Research Journal of Pharmaceutical, Biological and Chemical SciencesDocument9 pagesResearch Journal of Pharmaceutical, Biological and Chemical SciencesAtraoNo ratings yet
- TLX Technique GuideDocument28 pagesTLX Technique Guidejerry rice100% (2)
- Format N Assessment Isb533Document9 pagesFormat N Assessment Isb533Anis HayatiNo ratings yet
- Project Hospital Fin All Business SummaryDocument32 pagesProject Hospital Fin All Business Summarykanchoo100% (1)
- Communication Boards in Critical CareDocument9 pagesCommunication Boards in Critical CareSeresolNo ratings yet
- Greater Political ParticipationDocument12 pagesGreater Political ParticipationBe-COOL State Of MindNo ratings yet
- GBSDocument19 pagesGBSRahma ArsellaNo ratings yet
- Migraine Patient HandoutDocument14 pagesMigraine Patient HandoutthiautamiNo ratings yet
- Instructor Clinical Evaluation ToolsDocument11 pagesInstructor Clinical Evaluation ToolsJoric MagusaraNo ratings yet
- Advise Patients Not To Exceed The Recommended Dose or Frequency of AdministrationDocument3 pagesAdvise Patients Not To Exceed The Recommended Dose or Frequency of AdministrationPrincess M Viznar BalolotNo ratings yet
- Dental AssistantDocument2 pagesDental Assistantapi-78993102No ratings yet
- List of Instruments For 2nd Year BDSDocument17 pagesList of Instruments For 2nd Year BDSMohammad ShoebNo ratings yet
- Prevencion DeliriumDocument13 pagesPrevencion DeliriumCarlos Hutarra DiazNo ratings yet