Professional Documents
Culture Documents
Recommended Childhood and Adolescent Immunization Schedule: United States - 2005
Uploaded by
rizki_rahayuningsihOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Recommended Childhood and Adolescent Immunization Schedule: United States - 2005
Uploaded by
rizki_rahayuningsihCopyright:
Available Formats
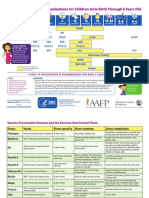
Recommended Childhood and Adolescent Immunization Schedule UNITED STATES • 2005
Age
Birth 1 2 4 6 12 15 18 24 4–6 11–12 13–18
Vaccine month months months months months months months months years years years
HepB #1
Hepatitis B1 HepB #3 HepB Series
HepB #2
Diphtheria, DTaP DTaP DTaP DTaP DTaP Td Td
Tetanus, Pertussis2
Haemophilus Hib Hib Hib Hib
influenzae type b3
Inactivated Poliovirus IPV IPV IPV IPV
Measles, Mumps, MMR #1 MMR #2 MMR #2
Rubella4
Varicella5 Varicella Varicella
PCV
Pneumococcal6 PCV PCV PCV PCV PPV
Influenza7 Influenza (Yearly) Influenza (Yearly)
Va c c i n e s b e l o w r e d l i n e a r e f o r s e l e c t e d p o p u l a t i o n s
8
Hepatitis A Hepatitis A Series
This schedule indicates the recommended ages for routine administration of currently contraindicated. Providers should consult the manufacturers' package inserts for
licensed childhood vaccines, as of December 1, 2004, for children through age detailed recommendations. Clinically significant adverse events that follow
18 years. Any dose not given at the recommended age should be given at any immunization should be reported to the Vaccine Adverse Event Reporting System
subsequent visit when indicated and feasible. (VAERS). Guidance about how to obtain and complete a VAERS form can be found on
Indicates age groups that warrant special effort to administer those vaccines the Internet: www.vaers.org or by calling 800-822-7967.
not previously given. Additional vaccines may be licensed and recommended during Range of recommended ages Only if mother HBsAg(–)
the year. Licensed combination vaccines may be used whenever any components of
the combination are indicated and the vaccine’s other components are not Preadolescent assessment Catch-up immunization
The Childhood and Adolescent Immunization Schedule is approved by:
Department of Health and Human Services Advisory Committee on Immunization Practices www.cdc.gov/nip/acip
Centers for Disease Control and Prevention American Academy of Pediatrics www.aap.org
American Academy of Family Physicians www.aafp.org
Footnotes
Recommended Childhood and Adolescent Immunization Schedule
UNITED STATES • 2005
1. Hepatitis B (HepB) vaccine. All infants should receive the first dose of 4. Measles, mumps, and rubella vaccine (MMR). The second dose of MMR
hepatitis B vaccine soon after birth and before hospital discharge; the first dose is recommended routinely at age 4–6 years but may be administered during any
may also be given by age 2 months if the infant’s mother is hepatitis B surface visit, provided at least 4 weeks have elapsed since the first dose and both doses
antigen (HBsAg) negative. Only monovalent HepB can be used for the birth dose. are administered beginning at or after age 12 months. Those who have not
Monovalent or combination vaccine containing HepB may be used to complete the previously received the second dose should complete the schedule by the visit at
series. Four doses of vaccine may be administered when a birth dose is given. The age 11–12 years.
second dose should be given at least 4 weeks after the first dose, except for
combination vaccines which cannot be administered before age 6 weeks. The third 5. Varicella vaccine. Varicella vaccine is recommended at any visit at or after age
dose should be given at least 16 weeks after the first dose and at least 8 weeks 12 months for susceptible children (i.e., those who lack a reliable history of
after the second dose. The last dose in the vaccination series (third or fourth dose) chickenpox). Susceptible persons aged ≥13 years should receive 2 doses, given at
should not be administered before age 24 weeks. least 4 weeks apart.
Infants born to HBsAg-positive mothers should receive HepB and 0.5 mL of 6. Pneumococcal vaccine. The heptavalent pneumococcal conjugate
Hepatitis B Immune Globulin (HBIG) within 12 hours of birth at separate sites. The vaccine (PCV) is recommended for all children aged 2–23 months. It is also
second dose is recommended at age 1–2 months. The last dose in the recommended for certain children aged 24–59 months. The final dose in the series
immunization series should not be administered before age 24 weeks. These should be given at age ≥12 months. Pneumococcal polysaccharide
infants should be tested for HBsAg and antibody to HBsAg (anti-HBs) at age 9–15 vaccine (PPV) is recommended in addition to PCV for certain high-risk groups.
months. See MMWR 2000;49(RR-9):1-35.
Infants born to mothers whose HBsAg status is unknown should receive the 7. Influenza vaccine. Influenza vaccine is recommended annually for children
first dose of the HepB series within 12 hours of birth. Maternal blood should be aged ≥6 months with certain risk factors (including but not limited to asthma,
drawn as soon as possible to determine the mother's HBsAg status; if the HBsAg cardiac disease, sickle cell disease, HIV, and diabetes), healthcare workers, and
test is positive, the infant should receive HBIG as soon as possible (no later than other persons (including household members) in close contact with persons in
age 1 week). The second dose is recommended at age 1–2 months. The last dose groups at high risk (see MMWR 2004;53[RR-6]:1-40) and can be administered to
in the immunization series should not be administered before age 24 weeks. all others wishing to obtain immunity. In addition, healthy children aged 6–23
months and close contacts of healthy children aged 0–23 months are
2. Diphtheria and tetanus toxoids and acellular pertussis (DTaP) recommended to receive influenza vaccine, because children in this age group are
vaccine. The fourth dose of DTaP may be administered as early as age at substantially increased risk for influenza-related hospitalizations. For healthy
12 months, provided 6 months have elapsed since the third dose and the child is persons aged 5–49 years, the intranasally administered live, attenuated influenza
unlikely to return at age 15–18 months. The final dose in the series should be given vaccine (LAIV) is an acceptable alternative to the intramuscular trivalent inactivated
at age ≥4 years. Tetanus and diphtheria toxoids (Td) is recommended at influenza vaccine (TIV). See MMWR 2004;53(RR-6):1-40. Children receiving TIV
age 11–12 years if at least 5 years have elapsed since the last dose of tetanus and should be administered a dosage appropriate for their age (0.25 mL if 6–35 months
diphtheria toxoid-containing vaccine. Subsequent routine Td boosters are or 0.5 mL if ≥3 years). Children aged ≤8 years who are receiving influenza
recommended every 10 years. vaccine for the first time should receive 2 doses (separated by at least 4 weeks for
TIV and at least 6 weeks for LAIV).
3. Haemophilus influenzae type b (Hib) conjugate vaccine. Three Hib
conjugate vaccines are licensed for infant use. If PRP-OMP (PedvaxHIB or ComVax 8. Hepatitis A vaccine. Hepatitis A vaccine is recommended for children and
[Merck]) is administered at ages 2 and 4 months, a dose at age 6 months is not adolescents in selected states and regions and for certain high-risk groups; consult
required. DTaP/Hib combination products should not be used for primary your local public health authority. Children and adolescents in these states, regions,
immunization in infants at ages 2, 4 or 6 months but can be used as boosters and high-risk groups who have not been immunized against hepatitis A can begin
following any Hib vaccine. The final dose in the series should be given at age the hepatitis A immunization series during any visit. The 2 doses in the series
≥12 months. should be administered at least 6 months apart. See MMWR 1999;48(RR-12):1-37.
Recommended Immunization Schedule
for Children and Adolescents Who Start Late or Who Are More Than 1 Month Behind
UNITED STATES • 2005
The tables below give catch-up schedules and minimum intervals between doses for children who have delayed immunizations.
There is no need to restart a vaccine series regardless of the time that has elapsed between doses. Use the chart appropriate for the child’s age.
CATCH-UP SCHEDULE FOR CHILDREN AGED 4 MONTHS THROUGH 6 YEARS
Minimum Minimum Interval Between Doses
Vaccine Age for
Dose 1 Dose 1 to Dose 2 Dose 2 to Dose 3 Dose 3 to Dose 4 Dose 4 to Dose 5
Diphtheria, 6 wks 4 weeks 4 weeks 6 months 6 months1
Tetanus, Pertussis
Inactivated 6 wks 4 weeks 4 weeks 4 weeks2
Poliovirus
Hepatitis B3 Birth 4 weeks 8 weeks
(and 16 weeks after first dose)
Measles, Mumps,
Rubella 12 mo 4 weeks4
Varicella 12 mo
4 weeks 4 weeks6 8 weeks (as final dose)
if first dose given at age <12 months if current age <12 months This dose only necessary for
children aged 12 months–5 years
Haemophilus 8 weeks (as final dose) 8 weeks (as final dose) 6
who received 3 doses before age
5 6 wks
influenzae type b if first dose given at age 12-14 months if current age ≥12 months and 12 months
second dose given at age <15 months
No further doses needed
if first dose given at age ≥15 months No further doses needed
if previous dose given at age ≥15 mo
4 weeks 4 weeks 8 weeks (as final dose)
if first dose given at age <12 months if current age <12 months This dose only necessary for
and current age <24 months children aged 12 months–5 years
8 weeks (as final dose) who received 3 doses before age
8 weeks (as final dose) if current age ≥12 months 12 months
Pneumococcal7 6 wks if first dose given at age ≥12 months
or current age 24–59 months No further doses needed
for healthy children if previous dose
No further doses needed given at age ≥24 months
for healthy children if first dose given
at age ≥24 months
CATCH-UP SCHEDULE FOR CHILDREN AGED 7 YEARS THROUGH 18 YEARS
Minimum Interval Between Doses
Vaccine
Dose 1 to Dose 2 Dose 2 to Dose 3 Dose 3 to Booster Dose
6 months8
if first dose given at age <12 months and current age
<11 years
Tetanus, 5 years8
Diphtheria 4 weeks 6 months if first dose given at age ≥12 months and third dose
given at age <7 years and current age ≥11 years
10 years8
if third dose given at age ≥7 years
Inactivated 4 weeks 4 weeks IPV2,9
Poliovirus9
Hepatitis B 4 weeks 8 weeks
(and 16 weeks after first dose)
Measles, 4 weeks
Mumps, Rubella
Varicella10 4 weeks
Footnotes
Children and Adolescents Catch-up Schedules UNITED STATES • 2005
1. DTaP. The fifth dose is not necessary if the fourth dose was given after the 5. Hib. Vaccine is not generally recommended for children aged ≥5 years.
fourth birthday.
6. Hib. If current age <12 months and the first 2 doses were PRP-OMP
2. IPV. For children who received an all-IPV or all-oral poliovirus (OPV) series, a (PedvaxHIB or ComVax [Merck]), the third (and final) dose should be given at age
fourth dose is not necessary if third dose was given at age ≥4 years. If both OPV 12–15 months and at least 8 weeks after the second dose.
and IPV were given as part of a series, a total of 4 doses should be given,
regardless of the child’s current age. 7. PCV. Vaccine is not generally recommended for children aged ≥5 years.
3. HepB. All children and adolescents who have not been immunized against hepatitis 8. Td. For children aged 7–10 years, the interval between the third and booster dose
B should begin the HepB immunization series during any visit. Providers should make is determined by the age when the first dose was given. For adolescents aged
special efforts to immunize children who were born in, or whose parents were born in, 11–18 years, the interval is determined by the age when the third dose was given.
areas of the world where hepatitis B virus infection is moderately or highly endemic.
9. IPV. Vaccine is not generally recommended for persons aged ≥18 years.
4. MMR. The second dose of MMR is recommended routinely at age 4–6 years but
may be given earlier if desired. 10. Varicella. Give 2-dose series to all susceptible adolescents aged ≥13 years.
Report adverse reactions to vaccines through the federal Vaccine Adverse For additional information about vaccines, including precautions and
Event Reporting System. For information on reporting reactions following contraindications for immunization and vaccine shortages, please visit the
immunization, please visit www.vaers.org or call the 24-hour national National Immunization Program Web site at www.cdc.gov/nip or call the
toll-free information line 800-822-7967. Report suspected cases of National Immunization Information Hotline at
vaccine-preventable diseases to your state or local health department. 800-232-2522 (English) or 800-232-0233 (Spanish).
You might also like
- APhA Immunization Participant - Case - WorksheetsDocument11 pagesAPhA Immunization Participant - Case - WorksheetsGerald Gamboa100% (2)
- USMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsFrom EverandUSMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsRating: 5 out of 5 stars5/5 (9)
- Clinical Management Review 2023-2024: Volume 1: USMLE Step 3 and COMLEX-USA Level 3From EverandClinical Management Review 2023-2024: Volume 1: USMLE Step 3 and COMLEX-USA Level 3Rating: 5 out of 5 stars5/5 (1)
- 0 6 Yrs Immunization ScheduleDocument1 page0 6 Yrs Immunization ScheduleAira ReyesNo ratings yet
- For Those Who Fall Behind or Start Late, See The Catch-Up ScheduleDocument4 pagesFor Those Who Fall Behind or Start Late, See The Catch-Up ScheduleTony MichelNo ratings yet
- Recommended Immunization Schedule For Persons Aged 0 Through 6 YearsDocument1 pageRecommended Immunization Schedule For Persons Aged 0 Through 6 YearshendergmNo ratings yet
- 7-18yr Schedule For Immunizations, CDC 2008Document1 page7-18yr Schedule For Immunizations, CDC 2008Tracy100% (1)
- ImmunizationDocument39 pagesImmunizationhhh11599No ratings yet
- VACCINES Eng Spa 0 To 6 Years ScheduleDocument4 pagesVACCINES Eng Spa 0 To 6 Years ScheduleMaría del Mar OrtizNo ratings yet
- Parent Ver SCH 0 6yrsDocument2 pagesParent Ver SCH 0 6yrsMatri SearchNo ratings yet
- 07 Childschd 6x4.5 1-Page PRDocument2 pages07 Childschd 6x4.5 1-Page PRSteluta GalbenusNo ratings yet
- Immunisation 2013 PDFDocument1 pageImmunisation 2013 PDFjuniorebindaNo ratings yet
- Recommended Immunization Schedule For Persons Aged 0-6 YearsDocument3 pagesRecommended Immunization Schedule For Persons Aged 0-6 YearsAlvaro FloresNo ratings yet
- PEDIA Immunizations 2018Document4 pagesPEDIA Immunizations 2018Mary Christine IlangaNo ratings yet
- 0 - 18yrs Schedule of VaccineDocument4 pages0 - 18yrs Schedule of VaccineEmanGamalAlbazNo ratings yet
- Parent Ver SCH 0 6yrsDocument2 pagesParent Ver SCH 0 6yrsSrinivasamurthy KamarthiNo ratings yet
- HepB Provider Tipsheet 508Document2 pagesHepB Provider Tipsheet 508Jamshaid AhmedNo ratings yet
- 0 18yrs ScheduleDocument4 pages0 18yrs Schedulekar_ind4u5636No ratings yet
- Haemophilus Influenzae Type: RD ND STDocument4 pagesHaemophilus Influenzae Type: RD ND STnickyboreNo ratings yet
- Immunization ScheduleDocument18 pagesImmunization Scheduledr parveen bathlaNo ratings yet
- Binational Schedule Immunization USA MEXICODocument2 pagesBinational Schedule Immunization USA MEXICOfernando_morales_15No ratings yet
- Recommend Ations: S GK, SS, S M, K C, S A, S K D, S V, A KS, S S, S K, H K P, SB, B JP, GVB, P GDocument11 pagesRecommend Ations: S GK, SS, S M, K C, S A, S K D, S V, A KS, S S, S K, H K P, SB, B JP, GVB, P Ga hNo ratings yet
- Immunization StatusDocument21 pagesImmunization StatusAubery RongNo ratings yet
- Indian Academy of Pediatrics (IAP) Recommended Immunization Schedule For Children Aged 0 Through 18 Years - India, 2014 and Updates On ImmunizationDocument16 pagesIndian Academy of Pediatrics (IAP) Recommended Immunization Schedule For Children Aged 0 Through 18 Years - India, 2014 and Updates On Immunizationkrishna615No ratings yet
- Adult Immunization Schedule by Vaccine and Age Group - CDCDocument17 pagesAdult Immunization Schedule by Vaccine and Age Group - CDCCamacaro Arevalo JoseNo ratings yet
- Adult Combined ScheduleDocument6 pagesAdult Combined ScheduleAstrid Elaine RosalesNo ratings yet
- IZSchedule0 6yrsDocument1 pageIZSchedule0 6yrsKaty ForemanNo ratings yet
- Childhood Immunization RecordDocument4 pagesChildhood Immunization RecordJoseph Edward DimayugaNo ratings yet
- Alexander - Peters VaccinationSchedule 04Document1 pageAlexander - Peters VaccinationSchedule 04Alex PetersNo ratings yet
- Iap Guide Book On Immunization Immunization in Special Situations PDFDocument8 pagesIap Guide Book On Immunization Immunization in Special Situations PDFGirdhari Lal Saini100% (1)
- The Routine Immunisation ScheduleDocument10 pagesThe Routine Immunisation ScheduleJamesWaitonNo ratings yet
- Baby Shots EngDocument2 pagesBaby Shots Engsunmo8217No ratings yet
- Adult Combined Schedule VaccineDocument33 pagesAdult Combined Schedule VaccinehatsuneNo ratings yet
- Parent Ver SCH 0 6yrsDocument2 pagesParent Ver SCH 0 6yrsunmundoextranopodcastNo ratings yet
- 0 18yrs ScheduleDocument4 pages0 18yrs ScheduleprashantNo ratings yet
- Iap Vaccination RecentDocument7 pagesIap Vaccination RecentDrNavya K UmeshNo ratings yet
- Infant ImmunisationDocument1 pageInfant ImmunisationPaul GallagherNo ratings yet
- TVCC Vaccination Presentation-1Document57 pagesTVCC Vaccination Presentation-1Gagandeep Singh DhamiNo ratings yet
- Parent Ver SCH 0 6yrs AafpDocument2 pagesParent Ver SCH 0 6yrs AafpcicitNo ratings yet
- ScheduleDocument2 pagesScheduleapi-286634335No ratings yet
- Rec Iz BabiesDocument1 pageRec Iz Babiesmaverick2748No ratings yet
- Vaccine Project - FinalDocument2 pagesVaccine Project - Finalchelsea garzaNo ratings yet
- 0 18yrs Child Combined ScheduleDocument14 pages0 18yrs Child Combined ScheduleEphrem LemmaNo ratings yet
- General Principles For ImmunizationsDocument29 pagesGeneral Principles For ImmunizationsKevin AnindytaNo ratings yet
- Combination VaccinesDocument19 pagesCombination VaccinesNorbaytiNo ratings yet
- Expanded Program On ImmunizationDocument9 pagesExpanded Program On ImmunizationJesena Salve100% (1)
- Vaccines: General Medical Conditions - PediatricsDocument21 pagesVaccines: General Medical Conditions - PediatricsSarah AlyssaNo ratings yet
- Vaccines For Your ChildDocument4 pagesVaccines For Your ChildIftekhar SaikatNo ratings yet
- Vaccinations For Preteens and Teens, Age 11-19 Years: Vaccine Do You Need It?Document1 pageVaccinations For Preteens and Teens, Age 11-19 Years: Vaccine Do You Need It?Phan303No ratings yet
- Peds Vaccination ScheduleDocument4 pagesPeds Vaccination Schedulekman0722No ratings yet
- Immunisation and Under 5 CardDocument31 pagesImmunisation and Under 5 CardStephen AngelNo ratings yet
- EPI Vaccines Revised Oct 2010Document18 pagesEPI Vaccines Revised Oct 2010Jei JayNo ratings yet
- Immunization ScheduleDocument2 pagesImmunization ScheduleTracy100% (1)
- Immunisation ScheduleDocument3 pagesImmunisation SchedulejegathesmsjsNo ratings yet
- Catchup Schedule PRDocument1 pageCatchup Schedule PRJesus A. Pineda GarciaNo ratings yet
- IMMUNIZATION ScheduleDocument2 pagesIMMUNIZATION Schedulejhonny100% (1)
- IMUNISASI2Document29 pagesIMUNISASI2RatnaSuryatiNo ratings yet
- 0 6yrs Schedule BWDocument1 page0 6yrs Schedule BWRyan ArdyantoNo ratings yet
- Immunizations For Babies: A Guide For Parents These Are The Vaccinations Your Baby Needs!Document1 pageImmunizations For Babies: A Guide For Parents These Are The Vaccinations Your Baby Needs!Lisa ManggadNo ratings yet
- Hep BDocument47 pagesHep BMia Mia MiaNo ratings yet
- General EssaysDocument75 pagesGeneral EssaysGanesh BabuNo ratings yet
- Strong BonesDocument9 pagesStrong BonesGanesh Babu100% (1)
- Cowboy MoviesDocument10 pagesCowboy MoviesGanesh BabuNo ratings yet
- C Programming Examples: Prof. Gustavo Alonso Computer Science Department ETH Zürich Alonso@inf - Ethz.chDocument12 pagesC Programming Examples: Prof. Gustavo Alonso Computer Science Department ETH Zürich Alonso@inf - Ethz.chmohit20singhNo ratings yet
- Edhs MapsDocument25 pagesEdhs MapsGanesh Babu100% (1)
- Batch File ABCsDocument4 pagesBatch File ABCsGanesh Babu100% (3)
- Breathing ExercisesDocument4 pagesBreathing ExercisesGanesh BabuNo ratings yet
- Tai Chi Breathing ExercisesDocument17 pagesTai Chi Breathing ExercisesGanesh Babu100% (15)
- Yoga and PainDocument29 pagesYoga and PainGanesh Babu100% (1)
- Stretching ExerciesDocument2 pagesStretching ExerciesGanesh Babu100% (1)
- Intro RobDocument16 pagesIntro RobGanesh Babu100% (1)
- AathichudiDocument16 pagesAathichudiமுரளி கிருஷ்ணன் alias முகி100% (9)
- Scripting ReferenceDocument1,130 pagesScripting ReferenceGanesh Babu100% (1)
- Gettingstarted DirectorDocument84 pagesGettingstarted Directormohammed.saboor100% (2)
- Living With PainDocument84 pagesLiving With PainGanesh Babu100% (11)
- Gettingstarted DirectorDocument84 pagesGettingstarted Directormohammed.saboor100% (2)
- MS Windows RegistryDocument9 pagesMS Windows RegistryGanesh Babu100% (2)
- Thirukural (TamilEnglish)Document167 pagesThirukural (TamilEnglish)arunprasad.vit100% (5)