Professional Documents
Culture Documents
Anaesthetic Management Supra Ten To Rial Intracranial Tumours
Uploaded by
mohamed_abdulrazikOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anaesthetic Management Supra Ten To Rial Intracranial Tumours
Uploaded by
mohamed_abdulrazikCopyright:
Available Formats
The Indian Anaesthetists’ Forum – (www.theiaforum.
org) Online ISSN 0973-0311
October 2005(2)
ANAESTHETIC MANAGEMENT OF
SUPRATENTORIAL INTRACRANIAL TUMOURS
G.S. Umamaheswara Rao
Professor
Department of Neuroanaesthesia
National Institute of Mental Health and Neurosciences
Bangalore 560 029
Brain tumours constitute the majority of neurosurgical conditions that
present for elective operations. The nature of the lesions varies from benign
tumours like meningiomas and schwannomas to highly malignant tumours like
glioblatomas. About 80% of the tumors are located in the supratentorial
compartment and about 20% in the posterior fossa.
The anaesthetic and perioperative care of patients with brain tumours
requires an understanding the following aspects:
1. Intracranial pathophysiology of the tumors
2. Effects of anaesthetics on brain
3. Measures to decrease the brain bulk at surgery
4. Intraoperative monitoring requirements
5. Implications of fluid therapy
6. Perioperative haemodynamic management
7. Implications of surgical position
8. Implications of concurrent medications
PATHOPHYSIOLOGIC CONSIDERATIONS
Intracranial Pressure
Normal intracranial pressure (ICP) is about 10-15 mmHg. Raised ICP is a
common feature of intracranial tumours. Intracranial hypertension, in these
cases, results from the mass lesion itself, oedema of the surrounding brain or
hydrocephalus in case of III ventricular or infratentorial tumors. Natural
mechanisms such as displacement of intracranial blood volume and
cerebrospinal fluid (CSF) and increased reabsorption of CSF tend to limit the
increase in ICP as the tumor increases in size. When these mechanisms are
exhausted, ICP increases steeply. Such steep increase in ICP leads to rapid
neurological deterioration. The important consequences of raised ICP are:
a) Cerebral ischemia due to reduction of cerebral perfusion pressure (CPP) and
b) Brain shifts. Significant gradients of ICP within various compartments of
intracranial cavity lead to herniation of brain structures. The most common forms
of herniation are herniation of the uncus of the temporal lobe through the hiatus
in the tentorium cerebelli, herniation of the cingulate gyrus under the falx cerebri,
and herniation of the cerebellar tonsils through formen magnum.
Umamaheswara Rao G. S.: Anaesthetic Management of Supratentorial Intracranial Tumours 1
The Indian Anaesthetists’ Forum – (www.theiaforum.org) Online ISSN 0973-0311
October 2005(2)
Clinical Signs of Raised ICP
Headache vomiting and papilloedema are the three cardinal signs of
raised ICP. Conscious patients with raised ICP complain of generalised or frontal
headache. They may also have nausea and vomiting. Vomiting is generally
projectile in nature. Impairment of consciousness occurs when the ICP is very
high; it may vary from somnolence to stupor and deep coma. Hypertension and
bradycardia represent an attempt at restoration cerebral blood flow (CBF) in the
face of grossly elevated ICP. Presence of retinal haemorrhage, indicates very
high ICP. A variety of abnormal breathing patterns have been observed in
patients with severe increase in ICP. Periodic, irregular, deep, shallow or typical
Cheyne-stokes patterns have been reported. Increase of respiratory rate is
usually an initial sign of elevated ICP followed by irregularity or depression of the
respiration and finally periods of apnoea and respiratory arrest.
Diagnostic studies for Raised ICP
Skull Radiography: Plain X-ray of the skull shows "beaten-silver" appearance and
demineralisation of sella tursica in patients with chronic elevation of ICP.
Angiography: Slowing of the circulation may be evident on angiography.
Angiography may also show diffuse narrowing of intracerebral arteries.
CT Scan: Focal or diffuse oedema is seen as hypodensity of brain parenchyma,
usually in the white matter. Diffuse brain oedema is accompanied by obliteration
of the basal cisterns and cerebral sulci and collapse of ventricles. Focal or
perilesional oedema in cerebral hemispheres manifests with compression of
ipsilateral ventricle and midline shift. Significant shift of brain structures may
occur without increase in the measured global ICP. Most often, CT scan provides
a better indication of the status of ICP dynamics than direct measurement of ICP.
ICP Monitoring: The indications for ICP monitoring in patients with brain tumours
are not clearly defined. With easy accessibility to CT scanning, continuous ICP
monitoring in patients with brain tumours has become less frequent. However,
postoperative ICP monitoring may be employed in patients with massive
intraoperative brain swelling requiring aggressive treatments such as mechanical
ventilation, barbiturate therapy etc. ICP monitoring is also helpful in patients at
enhanced risk of postoperative haematoma (e.g., intraventricular tumours).
Cerebral Blood Flow Changes
Normal CBF is 40-45 ml/100g/min. Cortical blood flow (70 mL/100g/min) is
much higher than subcortical flow (20 ml/100g/min). In health, CBF is regulated
by important mechanisms such as autoregulation and cerebral blood flow-
metabolism coupling. Brain tumors may cause an increase or decrease in the
CBF depending on the nature of the tumour. Changes in CBF autoregulation,
vascular response to CO2 and CBF-CMR coupling also occur in these patients.
Umamaheswara Rao G. S.: Anaesthetic Management of Supratentorial Intracranial Tumours 2
The Indian Anaesthetists’ Forum – (www.theiaforum.org) Online ISSN 0973-0311
October 2005(2)
Tolerance to arterial hypotension is reduced if the autoregulation is impaired.
Loss of vascular response to CO2 may limit the usefulness of hyperventilation in
decreasing the ICP. Loss of CBF-CMR coupling may result in luxury perfusion in
the peritumoral zones.
Implications of Cerebral Effects of Anaesthetics
Anaesthetics may exert their effects on various facets of cerebral function
such as CMRO2, CBF, cerebral blood flow-metabolism coupling, ICP,
autoregulation, vascular response to CO2 and brain electrical activity. The net
result of all these effects of the anaesthetic agents combined with their systemic
effects may prove beneficial or detrimental to an already diseased brain.
All anaesthetics, in general, decrease cerebral oxygen consumption
(CMRO2) in a dose-dependent manner, but their potency varies with individual
agents. Intravenous induction agents (barbiturate, propofol) are the most potent
depressants of cerebral metabolism (CMR) followed by inhalational agents
(isoflurane, sevoflurane, desflurane), benzodiazepines (midazolam) and
narcotics (fantanyl, alfentanil, sufentanil). All intravenous agents with the
exception of ketamine decrease ICP. All inhalational agents increase ICP, though
individual agents vary in the magnitude of this effect. Intravenous agents
preserve autoregulation, while inhalational agents impair it to varying degrees.
Agents that cause significant impairment of autoregulation are likely to cause
higher degrees of reduction of cerebral perfusion in the event of perioperative
hypotension. Anaesthetic agents that produce an isoelectric
electroencephalogram in clinically useful concentrations (isoflurane, sevoflurane,
desflurane) are likely to play a cerebral protective role in the intraoperative period
though convincing clinical evidence is lacking.
Opioids have been the mainstay of neuroanaesthesia for a number of
years. The earlier belief that synthetic short-acting opioids agents lack any
significant effect on ICP and CPP was challenged by studies that documented a
small increase in CSF pressure, significant decrease in mean arterial pressure
(MAP) and thus a substantial change in CPP1. Based on studies that reported
EEG seizure activity with high doses of fentanyl in animals and humans2,3,
cerebral activation with corresponding increase in CBF has been proposed as
the possible mechanism of this increase in ICP. A more plausible explanation
came from a study in head injured patients4 that demonstrated a close
relationship between opioid-induced hypotension and an increase in ICP.
Effective prevention of such hypotension prevented the increase in ICP. This
observation led to the hypothesis that the ICP increase is related to the
autoregulatory cerebral vasodilation in response to the hypotension caused by
the opioids.
Remifentanil seems to be particularly suitable for neurosurgery because of
its rapid onset and rapid offset of action and minimal effect on ICP. In a human
study of patients undergoing supratentorial craniotomy, remifentanil, alfentanil
Umamaheswara Rao G. S.: Anaesthetic Management of Supratentorial Intracranial Tumours 3
The Indian Anaesthetists’ Forum – (www.theiaforum.org) Online ISSN 0973-0311
October 2005(2)
and placebo caused similar changes in ICP5. Most of the later studies in
neurosurgical patients showed an overall efficacy and safety profile that is similar
to, if not better than, fentanyl. The important difference between remifentanil and
other opioids is its rapid offset of action that facilitates early response to verbal
commands and rapid tracheal extubation. Patients receiving remifentanil are
more likely to have immediate postoperative pain and therefore, may require a
transitional analgesia6,7. Rapid titratability makes it a promising agent for awake
craniotomy for brain tumors.
During the maintenance phase of anaesthesia, rapid changes in the depth
of anaesthesia can be effected with sevoflurane. Rapid emergence from
sevoflurane anaesthesia facilitates early neurological examination. Smooth
emergence without coughing prevents increase in cerebral venous pressure and
the possibility of haematoma formation.
Propofol offers a number of pharmacological advantages for total
intravenous anaesthesia (TIVA) in neurosurgical patients. It decreases CBF, and
CMRO2 and increases cerebrovascular resistance (CVR). Cerebral
autoregulation and vascular response to carbon dioxide remain unaltered. Its
effects on neuronal activity are similar to those of thiopentone. Therefore, it was
proposed that, like thiopentone, it could offer cerebral protection. The protection
offered by propofol seems to be a result of a decrease in CMRO2, maintenance
or redistribution of CBF and prevention of large increases in blood glucose, which
generally accompanies and worsens cerebral ischemia8. Despite these
theoretical considerations, till date, there is no convincing evidence to use
propofol as a cerebral protective agent in clinical situations.
Management of Fluid and Electrolyte Balance
The volume and composition of the fluid transfused have major
implications in patients with cerebral pathology. While hypervolemia increases
brain oedema, excessive dehydration decreases CBF.
Plan of Intraoperative Fluid Management
Intraoperative fluid therapy in patients with brain tumors should take into
account the maintenance requirements and excessive urine losses due to
diuretics. Third space losses may be considered negligible in these patients.
Fluid deficit due to preoperative fasting may be ignored in adult patients. The
goal of intraoperative fluid management in adult patients is to achieve a mild
negative balance of the order of 500-1000 mL. More meticulous calculations are
required in children to ensure that there is neither a positive nor a negative
balance at the end of surgery.
Glucose containing solutions are preferably avoided during the first four
hours of surgery. In prolonged surgeries glucose containing solutions are
administered in moderation. Our own approach in this regard has been to
administer alternate units of glucose-containing and non-glucose containing
Umamaheswara Rao G. S.: Anaesthetic Management of Supratentorial Intracranial Tumours 4
The Indian Anaesthetists’ Forum – (www.theiaforum.org) Online ISSN 0973-0311
October 2005(2)
solutions for maintenance requirements. Faster infusion requirements caused by
excessive diuresis or blood loss are met with by non-glucose containing
solutions.
Composition of the Fluid: Maintenance of mild hyperosmolality of plasma is
desirable in the intraoperative period. Therefore, hypotonic fluids like 5%
Dextrose in water, 1/2 N saline, 1/5 N Saline, Isolyte-M must be avoided in the
intraoperative period. Isotonic solutions such as 0.9% normal saline or Ringer's
lactate are the fluids of choice. Depending on the necessity (children, diabetic
patients), 5% dextrose may be added to these solutions. When there is a need
for large volume of fluid infusion, even Ringer's lactate is not advisable as it is
mildly hypotonic with reference to plasma. While these recommendations are
applicable to patients without any major preoperative electrolyte disturbances, in
patients with preoperative electrolyte disturbances, the choice of the fluid is
determined by the nature of disturbance involved.
Mannitol: Mannitol is the commonest hypertonic solution used to provide lax
brain at surgery. While causing cerebral dehydration and decreasing the ICP,
mannitol has the potential to cause adverse effects such as dehydration,
hyponatremia, hypokalemia, renal failure, transient increase in ICP before the
diuresis sets in and exaggeration of brain shifts in patients with unilateral mass
lesions. Dose recommendations for intraoperative use of mannitol vary from 0.25
- 2 g/kg as a bolus. Some centres use mannitol as a routine in all cases of
cerebral tumors; the rationale for such practice is that mannitol, by reducing the
brain bulk, provides easy access to the surgical lesion even when the ICP is not
very high. In some centres mannitol is used only in situations where the brain is
expected to be tense based on the preoperative CT scan. When indicated, it
must be administered as a bolus over 15-20 min before opening the dura. Urine
output, serum osmolality and serum electrolytes must be monitored to avoid
complications related to intravascular volume and electrolyte disturbances.
Implications of Surgical Position
Surgery on intracranial tumours may require various positions, which
include supine, prone, lateral and sitting positions. Haemodynamic and
respiratory complications and nerve injuries associated with these positions need
to be taken into account while positioning the patients for surgery.
Sitting position has fallen to disrepute in recent years because of life
threatening complications such as venous air-embolism and severe hypotension.
Surgical access to the operative lesion may demand acute flexion of the neck
that may cause airway obstruction and obstruction to cerebral venous outflow,
resulting in intraoperative brain swelling. Elevation of the head above the heart
level facilitates cerebral venous drainage; however, it may be fraught with the risk
of venous air embolism from open veins if the gradient between the vein and the
right atrium is sufficiently high.
Umamaheswara Rao G. S.: Anaesthetic Management of Supratentorial Intracranial Tumours 5
The Indian Anaesthetists’ Forum – (www.theiaforum.org) Online ISSN 0973-0311
October 2005(2)
Nociceptive stimulation during the three-pin holder application must be
prevented by administration of additional doses of fentanyl or infiltration of the
scalp with a local anesthetic agent.
Perioperative Haemodynamic Management
Optimal blood pressure management plays an important role in preventing
major intraoperative and postoperative complications. In conditions associated
with impaired autoregulation, CBF is pressure-dependent; hypotension
decreases CBF and hypertension increases CBF and ICP. Intraoperatively, blood
pressure must be maintained at preoperative values of the patient. Control of
systemic hypertension prior to surgery or control of intraoperative episodes of
hypertension requires consideration of the effect of such treatment on intracranial
pathology and cardiovascular function. Acute normalisation of blood pressure in
a patient with hypertension due to raised ICP may cause worsening of
neurological deficits.
Induced hypotension, which was a popular technique for reduction of
intraoperative blood loss, is not received with same enthusiasm at present. There
is substantial evidence to show that neurological morbidity of induced
hypotension is significantly high while the observed benefits are marginal.
Choice of antihypertensives to control hypertension - when indicated -
depends on the effects of these agents on cerebral circulation and ICP. Direct
vasodilators such as sodium nitroprusside, nitroglycerine and calcium
antagonists are to be discouraged as they are likely to increase CBF and ICP.
Beta-adrenergic blocking agents and angiotensin converting enzyme inhibitors
are preferred.
Implications of Concurrent Medications
Anticonvulsants, and steroids are some of the common medications that
these patients are likely to be receiving at the time of surgery. The patient's drug
schedule should be noted so that the relevant drugs can be administered when
the repeat doses are due in the intraoperative period. Drug interactions can occur
between the preoperative and intraoperative medications. Anticonvulsant agent,
phenytoin may decrease the duration of action of nondepolarising muscle
relaxants. Adrenocortical suppression due to prolonged steroid therapy may
cause unexpected hypotension intraoperatively.
ANAESTHETIC MANAGEMENT
Premedication
In patients with raised ICP, sedative premedication carries the risk of
depression of consciousness, airway obstruction, hypoxia and hypercapnia and
hence avoided. In patients without evidence of raised ICP, small doses of
benzodiazepines may be given orally on the day of surgery to allay anxiety.
Narcotics may be administered after establishment of IV access, during the
Umamaheswara Rao G. S.: Anaesthetic Management of Supratentorial Intracranial Tumours 6
The Indian Anaesthetists’ Forum – (www.theiaforum.org) Online ISSN 0973-0311
October 2005(2)
placement of monitoring devices. The patient must be carefully monitored and
should not be left unattended. Other concurrent medications such as
corticosteroids, anticonvulsants, antacids and medications for coincidental
diseases must be continued up to the day of surgery.
Intraoperative Monitoring
Routine monitoring during brain tumour surgery should include ECG,
invasive and noninvasive blood pressure, pulse oximetry, capnography,
nasopharyngeal temperature and urine output.
Anaesthetic Technique
Patients who are symptomatic for raised ICP, tend to pose problems of
“tight brain” or “massive intraoperative brain swelling” at surgery. The majority of
these patients would have received steroids for sometime that might have
brought the ICP under reasonable control when they present themselves for
surgical intervention. Preoperative CT evidence of large tumour, excessive
peritumoral oedema, gross midline shift, obliterated or effaced lateral ventricles
and subarachnoid cisterns and obliterated cortical sulci suggests high ICP.
Induction and intubation may aggravate intracranial hypertension. Liberal
doses of thiopentone or propofol combined with narcotics to achieve adequate
depth of anaesthesia, mild to moderate hyperventilation with mask before
intubation, intravenous lignocaine bolus and avoidance of nitrous oxide and
inhalational anaesthetics until such time as moderate hypocapnia is established,
are some of the measures that prevent dangerous increases in ICP. Total
intravenous anaesthesia may provide better operating conditions than
inhalational anaesthesia; this issue however, remains controversial in the light of
a few studies that showed no significant difference between inhalational and
intravenous anaesthesia in terms of short-term outcome measures. There are no
studies on the impact of anaesthetic technique on the long-term neurological
outcome of the patients.
Intraoperative ICP Reduction
Slack brain facilitates easy surgical access and adequate excision of the
tumour. Inability to achieve adequate brain laxity is fraught with serious
complications such as herniation of brain through craniotomy and excessive
retractor pressure leading to retractor anaemia.
Prevention of tense brain at surgery requires attention to a number of
details. These include smooth and unhurried induction, mild head elevation, and
avoiding neck kink and pressure on the neck veins. Intubation in light planes of
anaesthesia must be avoided. This would require higher than normal doses of
induction agents, adequate muscle relaxation and administration of IV lignocaine
prior to intubation. A small bolus of the IV induction agent may be repeated prior
to intubation.
Umamaheswara Rao G. S.: Anaesthetic Management of Supratentorial Intracranial Tumours 7
The Indian Anaesthetists’ Forum – (www.theiaforum.org) Online ISSN 0973-0311
October 2005(2)
Definitive measures used for decreasing the brain bulk include
hyperventilation, mannitol, continuous infusion of anaesthetic agents like
thiopentone or propofol, and CSF diversion through a ventriculostomy catheter in
patients with hydrocephalus. Moderate hypothermia may be employed in
extreme conditions of massive brain swelling resistant to conventional measures.
Role of Hyperventilation
Hyperventilation, which has been in clinical use for many years for
reduction of ICP, has been subjected to more critical analysis in the recent years.
Hypocapnia decreases CBF by 2-3% for each mmHg fall in PaCO2 upto 20
mmHg. Normal cerebral blood volume (CBV), which is 3-4 ml/100g, is reduced
by 0.049 ml/100g/mmHg change in PaCO2. If hyperventilation is sustained, CBF
and CBV return to baseline over about 4 h.
For many decades, it has been a practice to lower PaCO2 to improve
operating conditions during craniotomy. Recently, there is some evidence to
suggest that preoperative signs of raised ICP and condition of brain at
craniotomy are poorly correlated and the value of routine hyperventilation to
improve operating conditions remains questionable9. Secondly, the value of
hyperventilation in decreasing the brain volume seems to depend on the
background anaesthetic. A recent study demonstrated diminished
responsiveness of CBF and CBV to hypocapnia during propofol anaesthesia10.
Benefit of hyperventilation is probably limited to reversal of inhalational
anaesthetic induced cerebral vasodilation and consequent increase in CBV.
Emergence from Anaesthesia
Aims during emergence from anaesthesia are maintenance of stable
blood pressure and ICP, thereby adequate CPP, optimal oxygenation, normal
PaCO2, and normothermia. Hypertension, coughing, and asynchrony with the
ventilator increase the chances of postoperative haematoma and oedema. The
patient must be fully awake at the time of extubation so that neurological
examination can be performed. The advantages of early versus delayed
extubation are a subject of debate. The potential benefits of early awakening are
feasibility of early neurological examination, and low cost. Advantages of
delaying the extubation by a few hours have been reported recently. The
potential benefits of delaying extubation are reduced risk of hypoxemia, better
respiratory and haemodynamic control, and lower incidence of postoperative
haematoma formation. Obtunded consciousness and inadequate airway
preoperatively, intraoperative brain swelling, problems with haemostasis during
surgery, and major postoperative homeostatic disturbances warrant delaying
extubation.
Causes of delayed emergence: Unplanned delayed emergence is not an
infrequent event after surgery for brain tumors. Some of the potential causes for
such delay are seizure, intracranial haematoma, brain oedema or swelling, and
tension pneumocephalus. Hypothermia, metabolic acidosis and hyponatremia
Umamaheswara Rao G. S.: Anaesthetic Management of Supratentorial Intracranial Tumours 8
The Indian Anaesthetists’ Forum – (www.theiaforum.org) Online ISSN 0973-0311
October 2005(2)
are some of the systemic causes of delayed emergence. A CT or MRI and serum
biochemistry including blood gas analysis will help the differential diagnosis.
References
1) Marx W, Shah N, Long C, et al: Sufentanil, alfentanil, and fentanyl: Impact on
cerebrospinal fluid pressure in patients with brain tumors. J Neurosurg Anesth
1989; 1:3-7
2) de Castro J, Van de Water A, Wouters L, et al: Comparative study of
cardiovascular neurological, and metabolic side effects of eight narcotics in
dogs. Acta Anaesthesiol Belg 1979; 30:5-99
3) Tempelhoff R, Modica PA, Bernardo KL, et al: Fentanyl-induced
electrocorticographic seizures in patients with complex partial epilepsy. J
Neurosurg 1992; 77:201-8
4) Werner C, Kochs E, Bause H, et al: Effects of sufentanil on cerebral
hemodynamics and intracranial pressure in patients with brain injury.
Anesthesiology 1995; 83:721-6
5) Egan T, Minto C, Hermann D, et al: Remifentanil versus alfentanil:
Comparative pharmacokinetics and pharmacodynamics in healthy adult male
volunteers. Anesth Analg 1996; 82:821-33
6) Balakrishnan G, Raudzens P, Samra SK, et al: Safety and efficacy of
remifentanil versus fentanyl in patients undergoing surgery for intracranial
mass lesions. Anesth Analg 2000; 91:163-9
7) Crawford MW, Leman J, Saldivia V, Carmichael FJ, Hemodynamic and organ
blood flow responses to halothane and sevoflurane anaesthesia during
spontaneous ventilation. Anesth Analg 1992; 75:1000-6.
8) Milde LN. Brain protection . In Cucchiara RF, Michenfelder JD (Eds) : Clinical
neuroanaesthesia : New York, 1990, Churchill – Livingstone, pp:188
9) Cenic A, Craen RA, Howard-Lech VL, et al: Cerebral blood volume and blood
flow at varying arterial carbon dioxide tension levels in rabbits during propofol
anesthesia. Anesth Analg 2000; 90:1376-83.
10) Turner CR, Losasso TJ, Muzzi DA, et al: Brain relaxation and cerebrospinal
fluid pressure during craniotomy for resection of supratentorial mass lesions.
J Neurosurg Anesthesiol 1996;8:126-32.
Umamaheswara Rao G. S.: Anaesthetic Management of Supratentorial Intracranial Tumours 9
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 7cc003 Assignment DetailsDocument3 pages7cc003 Assignment Detailsgeek 6489No ratings yet
- Site Master S113C, S114C, S331C, S332C, Antenna, Cable and Spectrum AnalyzerDocument95 pagesSite Master S113C, S114C, S331C, S332C, Antenna, Cable and Spectrum AnalyzerKodhamagulla SudheerNo ratings yet
- EIS Summary NotsDocument62 pagesEIS Summary NotsKESHAV DroliaNo ratings yet
- Favis vs. Mun. of SabanganDocument5 pagesFavis vs. Mun. of SabanganAyra CadigalNo ratings yet
- Mathematics Trial SPM 2015 P2 Bahagian BDocument2 pagesMathematics Trial SPM 2015 P2 Bahagian BPauling ChiaNo ratings yet
- ĐỀ THI DỰ ĐOÁN 9Document4 pagesĐỀ THI DỰ ĐOÁN 9tranvananh2041985No ratings yet
- Dark Witch Education 101Document55 pagesDark Witch Education 101Wizard Luxas100% (2)
- Configuration Steps - Settlement Management in S - 4 HANA - SAP BlogsDocument30 pagesConfiguration Steps - Settlement Management in S - 4 HANA - SAP Blogsenza100% (4)
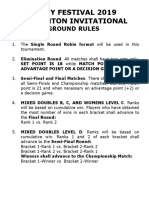
- Ground Rules 2019Document3 pagesGround Rules 2019Jeremiah Miko LepasanaNo ratings yet
- 10-C# Forms InteractionDocument22 pages10-C# Forms InteractionMaria Anndrea MendozaNo ratings yet
- Binary SearchDocument13 pagesBinary SearchASasSNo ratings yet
- Isolated Flyback Switching Regulator W - 9V OutputDocument16 pagesIsolated Flyback Switching Regulator W - 9V OutputCasey DialNo ratings yet
- S - BlockDocument21 pagesS - BlockRakshit Gupta100% (2)
- Em - 1110 1 1005Document498 pagesEm - 1110 1 1005Sajid arNo ratings yet
- Simple Past TenselDocument3 pagesSimple Past TenselPutra ViskellaNo ratings yet
- Psc720-Comparative Politics 005 Political CultureDocument19 pagesPsc720-Comparative Politics 005 Political CultureGeorge ForcoșNo ratings yet
- From Jest To Earnest by Roe, Edward Payson, 1838-1888Document277 pagesFrom Jest To Earnest by Roe, Edward Payson, 1838-1888Gutenberg.org100% (1)
- Storage Emulated 0 Android Data Com - Cv.docscanner Cache How-China-Engages-South-Asia-Themes-Partners-and-ToolsDocument140 pagesStorage Emulated 0 Android Data Com - Cv.docscanner Cache How-China-Engages-South-Asia-Themes-Partners-and-Toolsrahul kumarNo ratings yet
- Update UI Components With NavigationUIDocument21 pagesUpdate UI Components With NavigationUISanjay PatelNo ratings yet
- ASME-Y14.5.1M 1994 Mathematical Definition of Dimensioning and Tolerancing Principles PDFDocument89 pagesASME-Y14.5.1M 1994 Mathematical Definition of Dimensioning and Tolerancing Principles PDFwulfgang66No ratings yet
- Ottley Sandra 2009Document285 pagesOttley Sandra 2009Lucas Fariña AlheirosNo ratings yet
- Level 5 - LFH 6-10 SepDocument14 pagesLevel 5 - LFH 6-10 SepJanna GunioNo ratings yet
- Diabetes & Metabolic Syndrome: Clinical Research & ReviewsDocument3 pagesDiabetes & Metabolic Syndrome: Clinical Research & ReviewspotatoNo ratings yet
- Ib Physics SL - Unit 4 ReviewDocument46 pagesIb Physics SL - Unit 4 ReviewMax HudgenesNo ratings yet
- WHAT - IS - SOCIOLOGY (1) (Repaired)Document23 pagesWHAT - IS - SOCIOLOGY (1) (Repaired)Sarthika Singhal Sarthika SinghalNo ratings yet
- The Handmaid's Tale - Chapter 2.2Document1 pageThe Handmaid's Tale - Chapter 2.2amber_straussNo ratings yet
- Music 20 Century: What You Need To Know?Document8 pagesMusic 20 Century: What You Need To Know?Reinrick MejicoNo ratings yet
- Introduction To PTC Windchill PDM Essentials 11.1 For Light UsersDocument6 pagesIntroduction To PTC Windchill PDM Essentials 11.1 For Light UsersJYNo ratings yet
- Roofing Shingles in KeralaDocument13 pagesRoofing Shingles in KeralaCertainteed Roofing tilesNo ratings yet
- Oldham Rules V3Document12 pagesOldham Rules V3DarthFooNo ratings yet