Professional Documents
Culture Documents
005 Performance Evaluation of The Sysmex XT-2000i
Uploaded by
blanket_thOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
005 Performance Evaluation of The Sysmex XT-2000i
Uploaded by
blanket_thCopyright:
Available Formats
ISLH
Laboratory Hematology 9:29-37 2003 Carden Jennings Publishing Co., Ltd.
Official Publication
Performance Evaluation of the Sysmex XT-2000i Automated Hematology Analyzer
K. LANGFORD, L. LUCHTMAN-JONES, R. MILLER, D. WALCK
Saint Louis Childrens Hospital Core Laboratory/Hematology, St. Louis, Missouri, USA
Received October 2, 2002; received in revised form January 13, 2003; accepted January 17, 2003
ABSTRACT
The Sysmex XT-2000i automated hematology analyzer was evaluated at Saint Louis Childrens Hospital (SLCH), St. Louis, MO, USA. Complete blood count results from the Sysmex XT-2000i were compared to results from the Sysmex XE-2100 for 114 pediatric and adult patient samples. Manual differentials were performed on each specimen by 2 experienced medical technologists using guidelines established in the National Committee for Clinical Laboratory Standards (NCCLS) document H20-A. Carryover, precision, linearity, correlation, stability, and mixing-test studies were also performed. The XT-2000i results showed excellent correlation with the results from the XE-2100 for the following parameters: white blood cells; red blood cells; hemoglobin; hematocrit; mean corpuscular volume; mean corpuscular hemoglobin; mean corpuscular hemoglobin concentration; red blood cell distribution width by standard deviation; red blood cell distribution width by coefcient of variation; mean platelet volume; platelets; percent neutrophils, lymphocytes, monocytes, eosinophils, and basophils; and reticulocyte percent and number. In our evaluation of the XT-2000i the correlation coefcients for all complete blood counts and differential parameters compared well with those of the XE-2100. We concluded that the XT-2000i demonstrated comparable analytical performance to its predecessor, the XE-2100. Lab Hematol.
2003;9:29-37.
KEY WORDS: Performance evaluation Automated hematology analyzer XT-2000i INTRODUCTION
The Sysmex XT-2000i is a new fully automated hematology analyzer that performs a complete blood count (CBC) with a 16-parameter hemogram, a 5-part white blood cell (WBC) differential, and reticulocyte (RET) analysis that includes the immature RET fraction (IRF) and a uorescent optical platelet count (PLT-O). The analyzer is designed for high-volume output in the clinical laboratory with a throughput of 80 samples per hour, but the instruments compact size allows it to fit in a physicians ofce lab. The aspirated sample volume required is 85 L of whole blood for the manual mode and 150 L for the closed mode [1]. The XT-2000i uses the newest in applications, including an Internet access line, flat-screen monitor, and easy-tonavigate software. This instrument uses the current technology of uorescent ow cytometry with a semiconductor laser to provide the differential, RET, and fluorescent optical PLT information. The purpose of this study was to evaluate the performance of the XT-2000i and compare its accuracy and precision to those of an already established hematology analyzer, the XE-2100. The performance of the XT-2000i was evaluated at the laboratory of Saint Louis Childrens Hospital (SLCH), the oldest pediatric hospital west of the Mississippi River. SLCH has 235 beds, including a 26-bed pediatric intensive care unit, a 52-bed neonatal intensive care unit, and a 5-bed pediatric bone marrow transplantation unit. The dedicated pediatric laboratories process specimens for hos29
Correspondence and reprint requests: Keith Langford, Saint Louis Childrens Hospital Core Laboratory/Hematology, One Childrens Place, St. Louis, MO 63110-1077, USA; 1-314-454-4268; fax: 1-314454-4156 (e-mail: kxl6966@bjc.org).
30
K. Langford et al
pitalized patients, subspecialty clinics, and outpatient clinics in the St. Louis area. The hematology laboratory of Barnes Jewish Christian Hospital (BJC), which provided the adult samples, processes specimens from patients admitted to this tertiary hospital as well as from the subspecialty clinics and various ambulatory care centers in the community.
MATERIALS AND METHODS Specimens Residual peripheral venous blood samples collected in K2EDTA and K3EDTA tubes were used in the comparison testing. These blood samples were sent to SLCH and BJC laboratories for routine CBC testing. The specimens were analyzed on the XE-2100 (Sysmex Corporation of America, Long Grove, Illinois, USA) and the XT-2000i (Sysmex) within 8 hours of collection. A few exceptions were made for very unusual CBC results because they were received in the evening and night shifts. These specimens were stored until the next morning in a refrigerator at 2C to 8C and analyzed within 24 hours. The specimens used in the study consisted of 50 samples with CBC results that fell within normal ranges according to SLCH/BJC parameters and 64 samples that were classied as abnormal. The 64 abnormal specimens were obtained from patients with various clinical diagnoses including leukemias, sickle cell disease, multiple myeloma, viral infections, idiopathic thrombocytopenic purpura, sepsis, pancytopenia, and iron deficiency. Samples were obtained from preterm and term sick and healthy infants and from patients in critical care units, including the bone marrow transplantation unit. These specimens were used to determine whether unusual CBC ndings could be evaluated appropriately on the XT2000i. Furthermore, the types of suspect and user-dened flags generated for each abnormality were evaluated. The variety of abnormal cells and cell parameters encountered included nucleated red blood cells (NRBCs), sickle cells, blasts, immature granulocytes, atypical lymphocytes, plasma cells, large PLTs, low PLT counts, high WBC counts, PLT clumps, and RBC fragments. Duplicate peripheral blood smear slides were made and stained with a Wright-Giemsa stain. A slide from each sample was given to each of 2 technologists, who performed blind manual differentials of 200 cells each. These differentials were performed according to the National Committee for Clinical Laboratory Standards (NCCLS) document H20-A [2]. The results from both smears were then averaged. If the difference in results varied signicantly between the technologists, then another technologist read a referee slide. The laboratory used the following criteria to determine if the differential was abnormal: >10 bands; >5 atypical lymphocytes; presence of any metamyelocyte, myelocyte, promyelocyte, or blast; and presence of any NRBCs.
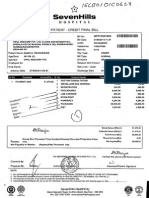
Instruments The XT-2000i is a new hematology analyzer capable of providing a 16-parameter hemogram, a 5-part differential, and RET analysis including IRF information. The XT2000i stores 10,000 samples in a Windows 2000 package using a at-screen monitor and user-friendly software. Figure 1 is an example of a NEGATIVE XT-2000i screen print including the scattergrams and histograms. Figure 2 is an example of a POSITIVE XT-2000i screen print. The term POSITIVE indicates that the CBC was interpreted as abnormal and the XT-2000i alerted the operator of the suspect ags, which resulted because of the unusual ndings. The following is a list of suspect ags/interpreted messages generated with the presence of unusual measurements: immature granulocytes, left shift, blasts, abnormal lymphocyte/L-blasts, atypical lymphocytes, NRBCs, RBC fragments, RBC lyse resistance, RBC agglutination, dimorphic RBC population, turbidity/HGB interference, iron deciency, HGB defects, PLT clumps, and WBC, RET, and PLT abnormal scattergrams. User-defined flags are defined by each institution to identify abnormal numerical results within the population being tested. Examples of user-dened ags are neutrophilia, monocytosis, anisocytosis, macrocytosis, and leukocytopenia. The WBC count is determined by ow cytometry using forward-scattered and side-scattered light. The differential uses a specic nucleic acid dye to measure the cells by sideuorescent light and side-scattered light. The RBC and PLT impedance (I) are measured using direct-current detection. The hematocrit (HCT) is simultaneously determined using the RBC pulse-height detection method. RETs are analyzed using ow cytometry and a nucleic acid uorescent dye. The measurement uses both forward-scattered light and side uorescent information to determine the RET count, percentage, and immature RET information. The PLT-O is also performed in this channel. The following parameters are calculated from directly measured data: mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), mean corpuscular hemoglobin concentration (MCHC), RBC distribution width by standard deviation (RDW-SD), RDW by coefcient of variation (RDW-CV), platelet distribution width (PDW), mean platelet volume (MPV), platelet large cell ratio (P-LCR), IRF, low uorescence ratio (LFR), middle uorescence ratio (MFR), and high uorescence ratio (HFR). The Sysmex XE-2100 was used for the comparison study. This analyzer is used daily in the laboratory at SLCH. A CBC with a 5-part differential and an RET count was performed on both analyzers. Calibration At the time of its arrival, the XT-2000i was calibrated by Sysmex Corporation service engineers according to the manufacturers guidelines using the Sysmex recommended
Performance Evaluation of the Sysmex XT-2000i
31
FIGURE 1. Example of negative XT-2000i screen print. WBC indicates white blood cells; RBC, red blood cells; HGB, hemoglobin; HCT, hematocrit; MCV, mean corpuscular volume; MCH, mean corpuscular hemoglobin; MCHC, MCH concentration; PLT, platelets; RDW-SD, RBC distribution width by standard deviation; RDW-CV, RDW by coefcient of variation; MPV, mean platelet volume; RET#, reticulocyte count; IRF, immature RET fraction; NEUT#, neutrophil count; LYMPH#, lymphocyte count; MONO#, monocyte count; EO#, eosinophil count; BASO#, basophil count.
FIGURE 2. Example of positive XT-2000i screen print. See Figure 1 legend for abbreviation denitions.
32
K. Langford et al
TABLE 1. Reagent Comparison*
Reagent CellPack Cell Sheath Sulfolyser Stromatolyser-FB Stromatolyser-DL/4DS Stromatolyser-IM Stromatolyser-NR Ret Search II Description Red blood cell/platelet and hemoglobin diluent that is used as the main rinse of the instrument. Diluent used as a sheath for cells owing through the aperture. Sodium lauryl sulfate hemoglobin measuring reagent. Basophil diluent and lyse. Lyses all cells except basophils. Differential reagents used to lyse red blood cells and dilute and stain white blood cells. Used to lyse red blood cells and white blood cell cytoplasm for detection of immature granulocyte information. Used as a lyse in the detection of nucleated red blood cells. Dilutes and stains reticulocytes and platelets for analysis XT-2100i X X X X X XE-2100 X X X X X X X X
*X indicates reagent is used on the system; , reagent is not used.
calibrator product. Three levels of quality control material e-Check were used (levels 1, 2, and 3) throughout the comparison study. Each day before specimen analysis shutdown and startup were performed with close attention to background counts. All instruments in the study had the same user-defined flag settings for flagging evaluation, thus ensuring that all conditions such as leukopenia, neutrophilia, and microcytosis would trigger the appropriate ag on both analyzers.
XE-2100. Table 1 lists the reagents required for both the XT2000i and XE-2100.
Precision Precision for both the closed mode (automated aspiration via cap-piercing) and manual open mode aspiration was evaluated by the performance of 10 consecutive measurements on fresh donor blood samples. Carryover Carryover was performed using the International Committee for Standardization in Hematology (ICSH) procedure for the following parameters: WBC, RBC, HGB, HCT, PLT, and numbers of RETs, neutrophils, lymphocytes, monocytes, eosinophils, and basophils. Carryover was assessed by 3 consecutive analyses of a patient sample with high analyte con-
Reagents By way of comparison, the XT-2000i and the XE-2100 use a common reagent system. The XT-2000i uses 3 fewer reagents than the XE-2100. The footprint of the XT-2000i is smaller because it does not use Cell Sheath, NRBC diluent and dye, or Stromatolyser IM, reagents that are unique to the
TABLE 2A. PrecisionOpen-Tube Analysis of the XT-2000i *
Open-Tube Analysis Mean SD CV% RBC, 106/L 5.15 0.03 0.6 HGB, g/dL 15.9 0.11 0.7 HCT, % 47.5 0.31 0.7 MCV, fL 92.3 0.3 0.3
PLT, 103/L 638 5.2 0.8
WBC, 103/L 12.22 0.19 1.6
NEUT, 103/L 6.41 .10 1.6
LYM, 103/L 4.36 0.08 1.9
MONO, 103/L 0.89 0.03 3.5
RET, 106/L 0.13 0.01 4.9
*RBC indicates red blood cells; HGB, hemoglobin; HCT, hematocrit; MCV, mean corpuscular volume; PLT, platelets;WBC, white blood cells; NEUT, neutrophils; LYM, lymphocytes; MONO, monocytes; RET, reticulocytes; CV, coefcient of variation.
TABLE 2B. PrecisionClosed-Tube Analysis of the XT-2000i *
Closed-Tube Analysis Mean SD CV% RBC, 106/L 4.35 0.02 0.6 HGB, g/dL 13.4 0.06 0.4 HCT, % 40.4 0.30 0.7 MCV, fL 92.9 0.28 0.3 PLT, 103/L 305 6.1 2.0 WBC, 103/L 8.54 0.10 1.1 NEUT, 103/L 4.46 0.07 1.5 LYM, 103/L 3.14 0.09 2.9 MONO, 103/L 0.60 0.03 4.8 RET, 106/L 0.08 0.01 6.3
*See Table 2A footnote for abbreviation denitions.
Performance Evaluation of the Sysmex XT-2000i
33
centration (H1, H2, H3) followed by 3 consecutive analyses of a patient sample with low analyte concentration (L1, L2, L3). The percentage of carryover for each parameter was calculated from the formula [3]: Carryover (%) = L1 L3 100. H3 L3
TABLE 4. Carryover of High Platelet and White Blood Cell Counts
Carryover Low 1 Low 2 Low 3 High 1 High 2 High 3 Carryover, % Platelet Count 60 57 52 6561 6558 6597 0.12 White Blood Cell Count 23.24 23.78 23.37 109.50 106.37 105.18 0.16
Linearity To assure the linearity of WBC, RBC, HGB, HCT, PLT, and RET results, blood samples were serially diluted to challenge the reportable range of the instrument. Data from these analyses were compared graphically using the actual values obtained plotted against values projected from the undiluted sample. High PLT-I linearity was evaluated using a single-donor pheresis product that had been volume reduced; the resulting platelet-rich product was added to a venous blood tube. High WBC linearity was established by using a specimen from a patient with chronic myeloid leukemia who had presented with a WBC count of 410 103/L. The following criteria were used for linear performance testing: the data must t a linearity regression line for which the coefcient of determination (R 2) must be >0.95; a minimum of 5 dilutions distributed throughout the linearity range must be used; the dilutions must cover the reportable range for the parameter; and each dilution result must be the mean value of duplicate or more measurements on the same range. Mixing Studies The XT-2000i mixes each tube 10 times by inversion in the automode prior to blood aspiration. The effectiveness of the 10-inversion mixing was validated by performance of 3 analyses of 14 samples in the automode and averaging of the RBC value. This value was used as the baseline comparison. The 14 samples were then allowed to sit undisturbed for 4 hours at room temperature. After 4 hours, the samples were placed on the analyzer without any manual mixing and analyzed in the automode. The specimens were then mixed well by hand and reanalyzed in the automode. Both of the
TABLE 3. Carryover*
WBC H1 H2 H3 L1 L2 L3 Carryover, % 12.05 12.18 12.07 3.73 3.57 3.66 0.83 RBC 5.11 5.07 5.15 1.52 1.53 1.52 0 HGB 15.8 15.8 15.8 4.7 4.7 4.7 0 HCT 47.6 47.2 47.8 14.5 14.5 14.4 0.30 PLT 645 638 638 131 134 129 0.39 RET# 0.1298 0.1278 0.1344 0.019 0.0252 0.0228 3.41
RBC obtained values were then compared to the baseline values and had to agree within 1.5% of the baseline.
Comparison Studies As discussed previously, a total of 114 venous blood samples were selected and analyzed on the Sysmex XT-2000i and the Sysmex XE-2100. For all specimens, 2 blood lms were prepared for a 400-cell manual differential that was performed by 2 technologists. The CBC and differential data were evaluated. RESULTS Precision Results from replicate open-tube and closed-tube analysis are shown in Tables 2A and 2B, respectively. The precision attained surpassed manufacturer specications for all parameters. RBC parameters showed exceptional precision, with coefcients of variation (CVs) less than 1.0%. The WBC and PLT parameters showed CVs of 2.0% or less. Precision of differentials for the primary cell typesneutrophils, lymphocytes, and monocytesalso was excellent, with CVs less than 5%. Carryover Carryover data are presented in Table 3 for total WBC, RBC, HGB, HCT, PLT, and RET number. Carryover on the XT-2000i for all parameters was of minimal magnitude. The results of high-to-low carryover testing were less than 1% for all determinations. Carryover was also performed on a manipulated singledonor pheresis PLT product and a specimen with a high WBC count to test the XT-2100i, and the results showed no signicant carryover even with extremely high parameters (Table 4).
TABLE 5. Linearity
Parameter White blood cell count Platelet count High platelet count Lowest Highest Correlation Value Value Coefcient Slope Intercept 0.39 2 102 401.83 1474 6560 1.00 1.00 1.00 1.00 1.01 1.00 1.11 4.23 100
*See Figure 1 legend for abbreviation denitions.
34
K. Langford et al
TABLE 6. Mixing Studies*
RBC 1 Run 1 Run 2 Run 3 Average 4 h unmixed 4 h premixed Change unmixed, % Change premixed, % 1.5% 4.1 4.12 4.11 4.11 4.09 4.13 0.49 0.49 OK RBC 2 4.45 4.47 4.46 4.46 4.44 4.41 0.45 1.12 OK RBC 3 2.23 2.26 2.25 2.25 2.25 2.28 0.15 1.48 OK RBC 4 4.88 4.87 4.88 4.88 4.89 4.9 0.27 0.48 OK RBC 5 5.7 5.69 5.67 5.69 5.73 5.72 0.76 0.59 OK RBC 6 5.49 5.49 5.45 5.48 5.48 5.46 0.06 0.30 OK RBC 7 2.97 2.98 2.98 2.98 2.97 2.94 0.22 1.23 OK RBC 8 4.49 4.51 4.49 4.50 4.49 4.51 0.15 0.30 OK RBC 9 2.79 2.82 2.8 2.80 2.84 2.78 1.31 0.83 OK RBC 10 RBC 11 RBC 12 RBC 13 RBC 14 4.86 4.86 4.83 4.85 4.79 4.84 1.24 0.21 OK 4.13 4.11 4.09 4.11 4.12 4.11 0.24 0.00 OK 4.63 4.61 4.62 4.62 4.62 4.62 0.00 0.00 OK 3.92 3.95 3.96 3.94 3.97 3.97 0.68 0.68 OK 4.45 4.45 4.44 4.45 4.48 4.43 0.75 0.37 OK
*RBC indicates red blood cell.
Linearity The linearity results looked very good on all parameters, with special attention given to the WBC and PLT counts. Table 5 shows the WBC linearity with an upper reportable range veried at 410 103/L and the upper reportable PLT value of 1474 103/L. A specimen was obtained from a single-donorpheresis PLT product, and the volume was reduced to yield a very high PLT count of 6560 103/L. Table 5 also shows the results of this high linearity. Mixing Studies The data from the mixing studies indicated that even after 4 hours of sitting undisturbed, the samples were adequately mixed on the XT-2000i and showed no signicant difference from those specimens that were mixed thoroughly before
TABLE 7. Comparison of XT-2000i and XE-2100 Complete Blood
Count and Differential*
Parameter WBC RBC HGB HCT MCV MCH MCHC RDW-SD RDW-CV PLT NEUT# LYMPH# MONO# EO# BASO# RET% RET# IRF% Correlation Coefcient 1.00 1.00 1.00 0.99 0.98 0.99 0.86 0.99 1.00 0.98 1.00 0.98 0.98 0.99 0.99 0.99 0.99 0.97 Slope 1.12 1.03 1.02 1.00 0.99 1.03 0.84 0.92 0.99 1.04 1.01 0.96 1.10 1.02 1.09 1.22 1.20 1.19 Intercept 0.63 0.12 0.16 0.43 0.51 0.33 5.93 2.72 0.22 4.55 0.01 0.04 0.05 0.01 0.01 0.22 0.01 1.22 N 114 114 114 114 114 114 114 114 114 114 114 114 114 114 114 114 114 114
being analyzed. All changes in the RBC count were less than 1.5%. The data are displayed in Table 6.
Comparison Studies As shown in Table 7, overall correlation between the XT2000i and the XE-2100 for all measured parameters was excellent, with R2 values for all parameters >0.92. The only exception was the MCHC, which showed an R2 value of 0.8552. Only 64 of the 114 specimens used in the comparison testing were abnormal. These specimens with unusual measurements were selectively picked to challenge the linearity of the analyzer and its capability to categorize the cells in the automated differential. See Figure 3 for graphic display of key parameters. Comparison of XT-2000i with the Manual Differential Reference Method The correlation coefficients, slope, intercept point, and number of comparison results are shown in Table 8. Experienced technologists performed the two 200-cell reference manual differentials. The autodifferential results obtained on the XT-2000i compared very well with the manual differential results. More than half of the specimens used in the comparison had abnormal differential ndings, and excellent correlation between the 2 instruments was demonstrated. See Figure 4 for graphic display. Morphologic Abnormality Flagging Efciency The results of the reference 400-cell differential indicated that immature or morphologically abnormal cells were present in 48 of the 114 samples. The XT-2000i generated a morphologic flag on 46 of these samples. Two samples, both showing NRBCs present at very low levels (less than 1/100 WBCs) were not agged. Both of these samples had WBC counts less than 1.8 103/L. No immature or morphologically abnormal cells were found by the manual differential on the remaining 66 samples, although distributional abnormalities were present in some cases. The XT-2000i correctly identied 60 of these samples. The remaining 6 samples had false-positive ags; 1 had a left shift ag, 1 had an
*See Figure 1 legend for abbreviation denitions.
Performance Evaluation of the Sysmex XT-2000i
35
FIGURE 3. Comparison graphs of results for white blood cells (WBC), red blood cells (RBC), and hemoglobin (HGB) obtained on
the XT-2000i and those obtained on the XE-2100.
36
K. Langford et al
TABLE 8. Comparison Results of XT-2000i to the Manual Differential
Reference Method
Parameter Neutrophils Lymphocytes Monocytes Eosinophils Basophils Correlation Coefcient (r) 0.95 0.96 0.90 0.94 0.76 Slope 0.95 0.85 1.37 0.87 0.48 Intercept 3.38 1.67 1.89 0.04 0.24 N 114 114 114 114 114
immature granulocyte flag, 3 had abnormal lymphocyte ags, and 1 had multiple abnormal/immature ags. The XT2000i agging sensitivity and specicity are shown in Table 9. The XT-2000i showed very good agging efciency for both adult and pediatric samples. Separate analysis of the NRBC and blast ags also showed good efciency. Blasts were identied on 9 of the manual dif-
ferentials. The XT-2000i agged 6 of these samples as having blasts present. The 3 samples not agged by the XT-2000i all had a manual blast count of <1.0%. All 3 of these samples had other ags that would have prompted a manual review. On these 3 samples, a rare blast was reported by only 1 of the 2 technologists doing a 200-cell differential. On further review, the referee could not positively determine whether the cells were blasts without performing cytochemical stains. According to the referee, the cells appeared to be abnormal immature lymphocytes with only a rare blast. Detection of a blast cell during a manual review of 100 cells is an extremely rare occurrence. An additional 3 samples had generated a false-positive blast ag; however, all 3 samples had signicant numbers of pathologically abnormal lymphocytes. The blast flag alone had a negative clinical accuracy of 97% and an efciency of 94.7%. NRBCs were identied on 24 of the samples in a range of 0.25 to 84/100 WBCs. The XT-2000i generated an NRBC ag on 20 of these samples. The 4 samples not agged all had NRBCs present at less than 1/100 WBCs.
FIGURE 4. Comparison graphs of results obtained on the XT-2000i and those obtained with the manual differential reference method.
Performance Evaluation of the Sysmex XT-2000i TABLE 9. Flagging Efciency
Positive Manual differential XT-2000i Sensitivity Specicity Positive clinical accuracy Negative clinical accuracy Efciency 48 52 95.8% 90.9% 88.5% 96.8% 92.9% Negative 66 62
37
A false-positive NRBC ag was generated on 6 of the 114 samples. The NRBC flag alone showed a negative clinical accuracy of 95.5% and an efciency of 91.2%.
DISCUSSION AND CONCLUSION
Our evaluation has shown that the XE-2100 and the XT2000i have excellent correlation statistics for all CBC, RET, and differential values. Because the technology is very similar in both analyzers, this result is not surprising. The use of uorescent ow cytometry for the CBC differential gives very good correlation with the manual reference method. By challenging the linearity of the instrument with extremely high- and low-count samples, we validated the linearity of the XT-2000i for WBC counts up to 410 103/L and PLT counts up to 6560 103/L. This extended linearity could eliminate the labor-intensive and error-prone manual dilutions required when dealing with specimens with drastically increased values. The condence that comes from knowing that PLT counts can be measured accurately
by the uorescent optical method also reduces the need for the technologist to perform a manual microscopic PLT count to verify results on a specimen that contains enlarged PLTs or RBC fragments, both of which interfere with the impedance PLT methodology. PLT testing is of great importance in the pediatric population because the majority of capillary specimens received have a higher incidence of PLT clotting or clumping. The technical comparison performed resulted in outstanding statistical results indicating that the XT-2000i is a very precise and accurate hematology analyzer that would perform well in any clinical setting. Our laboratory personnel were impressed that the XT-2000i uses the already proven Sysmex methodologies from the XE-2100 [4] and improves on them, resulting in an instrument that is more user friendly and a little more compact without sacricing any technical reliability.
REFERENCES
1. XT-2000i Product Brochure. Long Grove, Ill: Sysmex Corporation of America; 2002. 2. National Committee for Clinical Laboratory Standards. Reference leukocyte differential count (proportional) and evaluation of instrument method. Villanova, Pa: NCCLS; 1992. Approved standard, NCCLS Document H20-A. 3. International Committee for Standardization in Hematology. Protocol for evaluation of automated hematology analyzer. ICSH. 1984:;6:69. 4. Gould N, Connell B, Dyer K, Richmond T. Performance evaluation of the Sysmex XE-2100, automated hematology analyzer. Sysmex J Int. 1999;9:120-125.
You might also like
- Performance Evaluation of The Sysmex XT-2000i Automated Hematology AnalyzerDocument10 pagesPerformance Evaluation of The Sysmex XT-2000i Automated Hematology AnalyzerMaysaaNo ratings yet
- Performance Evaluation of The Sysmex XT-2000i AutoDocument10 pagesPerformance Evaluation of The Sysmex XT-2000i AutoMahmoud AhmedNo ratings yet
- Evaluation of RDW-CV RDW-SD Math 1sd 2013Document8 pagesEvaluation of RDW-CV RDW-SD Math 1sd 2013Gregorio De Las CasasNo ratings yet
- Jcla 22392Document8 pagesJcla 22392Ajish joNo ratings yet
- Platelet Counting by The Coulter LH 750, Sysmex XE 2100Document7 pagesPlatelet Counting by The Coulter LH 750, Sysmex XE 2100blanket_thNo ratings yet
- Evaluation of The Abbott CELL-DYN 4000 HematologyDocument10 pagesEvaluation of The Abbott CELL-DYN 4000 Hematologypasamuco473No ratings yet
- Dacosta 2015Document36 pagesDacosta 2015JE SimianNo ratings yet
- DR Preeti Mansukhani - CBC 5 Parts - 2017Document56 pagesDR Preeti Mansukhani - CBC 5 Parts - 2017Silence T-jmNo ratings yet
- Vol30 1 02Document7 pagesVol30 1 02dhia.yNo ratings yet
- Flags in Sysmex Xe 5000Document8 pagesFlags in Sysmex Xe 5000Prosenjit Roy ChoudhuryNo ratings yet
- Evaluation of The Performance of The Sysmex XT-200Document11 pagesEvaluation of The Performance of The Sysmex XT-200Игорь БеняNo ratings yet
- Reticulocyte Counting in ThalasemiaDocument6 pagesReticulocyte Counting in ThalasemiaSutjipto WijonoNo ratings yet
- Hedley 2010Document12 pagesHedley 2010my accountNo ratings yet
- Evaluation and Comparison of The New Mindray BC-6200 Hematology Analyzer With ADVIA 2120iDocument8 pagesEvaluation and Comparison of The New Mindray BC-6200 Hematology Analyzer With ADVIA 2120iGABRIELA HERRERANo ratings yet
- Sismex ManualDocument11 pagesSismex ManualDigo SomengNo ratings yet
- Evaluation of The Performance of Sysmex XN-3100 Automated Hematology Analyzer Regarding The Sysmex XE-2100 and Microscopic ExaminationDocument9 pagesEvaluation of The Performance of Sysmex XN-3100 Automated Hematology Analyzer Regarding The Sysmex XE-2100 and Microscopic ExaminationbalkisNo ratings yet
- Lmy 030Document7 pagesLmy 030Tuan NguyenNo ratings yet
- Automated Counters3Document14 pagesAutomated Counters3Jacky SharmaNo ratings yet
- Sysmex ScattergramsDocument7 pagesSysmex ScattergramsRuxandra Mesaros100% (1)
- BC-5300 Brochure EnglishDocument1 pageBC-5300 Brochure EnglishAngelica R BernalNo ratings yet
- Bruegel 2015Document15 pagesBruegel 2015my accountNo ratings yet
- Ceelie 2007Document9 pagesCeelie 2007alecoletoNo ratings yet
- Evaluation of RDW-CV, RDW-SD, and MATH-1SD For The Detection of Erythrocyte Anisocytosis Observed by Optical MicrosDocument8 pagesEvaluation of RDW-CV, RDW-SD, and MATH-1SD For The Detection of Erythrocyte Anisocytosis Observed by Optical MicrosAlhasn AlmerabyNo ratings yet
- White Paper CPD Sepsis AJCP 2005Document5 pagesWhite Paper CPD Sepsis AJCP 2005jtmchughNo ratings yet
- Peripheral Blood Smear and HistologyDocument26 pagesPeripheral Blood Smear and Histologystudent2013No ratings yet
- SG 8 CH 15 InstrumentationDocument5 pagesSG 8 CH 15 InstrumentationwerfsdsfNo ratings yet
- 2 Ijmpsapr20172Document6 pages2 Ijmpsapr20172TJPRC PublicationsNo ratings yet
- Immature GranulocytesDocument10 pagesImmature Granulocytespieterinpretoria391No ratings yet
- 10 0000@www Jrheum Org@32@5@828Document5 pages10 0000@www Jrheum Org@32@5@828Yasser AlghrafyNo ratings yet
- FlagsDocument6 pagesFlagsjonathan andre mora quimbayoNo ratings yet
- 3minute Blood Film EvaluationsDocument16 pages3minute Blood Film EvaluationsSanthi Swetha100% (1)
- Comparison of The Leukocyte Differentiation PDFDocument8 pagesComparison of The Leukocyte Differentiation PDFDyah LaksmiNo ratings yet
- Ok 2Document7 pagesOk 2cydolusNo ratings yet
- Original Article: Study of RBC Histogram in Various AnemiasDocument14 pagesOriginal Article: Study of RBC Histogram in Various AnemiasSirishaNo ratings yet
- Digital Microscopy As A Screening Tool For The Diagnosis of Hereditary Hemolytic AnemiaDocument10 pagesDigital Microscopy As A Screening Tool For The Diagnosis of Hereditary Hemolytic AnemiaRanhie Pen'ned CendhirhieNo ratings yet
- Potential of Cell Tracking Velocimetry As An Economical and Portable Hematology Analyzer.Document13 pagesPotential of Cell Tracking Velocimetry As An Economical and Portable Hematology Analyzer.Lizet SantacruzNo ratings yet
- 023 Evaluation of The Sysmex UF-100 AutomatedDocument4 pages023 Evaluation of The Sysmex UF-100 Automatedblanket_thNo ratings yet
- Performance Evaluation of The Sysmex XS PDFDocument7 pagesPerformance Evaluation of The Sysmex XS PDFZaza KvantalianiNo ratings yet
- New QuantitiesDocument6 pagesNew Quantities20100117 Bùi Thùy VyNo ratings yet
- CSF, UF 1000i, 2015Document11 pagesCSF, UF 1000i, 2015balkisNo ratings yet
- Clinical Biochemistry: E. Schapkaitz, S. RaburabuDocument7 pagesClinical Biochemistry: E. Schapkaitz, S. RaburabuMunawwar SaukaniNo ratings yet
- An Artificial Intelligence-Assisted Diagnostic PlaDocument11 pagesAn Artificial Intelligence-Assisted Diagnostic Plahanrong912No ratings yet
- Briggs 2009Document13 pagesBriggs 2009anggaririnNo ratings yet
- CQ HematoDocument8 pagesCQ HematoRizky Pratama NurhakimNo ratings yet
- Utility - of - Scatterplot - Patterns - of - Automated - Hematology Analysers 2020Document6 pagesUtility - of - Scatterplot - Patterns - of - Automated - Hematology Analysers 2020tufis02No ratings yet
- HarrisADVIA2120methods LabHema2005 11 47-61 PDFDocument16 pagesHarrisADVIA2120methods LabHema2005 11 47-61 PDFedu_14cNo ratings yet
- Performance Evaluation of The Sysmex XP-300 in An Oncology Setting: Evaluation and Comparison of Hematological Parameters With The Sysmex XN-3000Document7 pagesPerformance Evaluation of The Sysmex XP-300 in An Oncology Setting: Evaluation and Comparison of Hematological Parameters With The Sysmex XN-3000Yojan Leo Irakurri PuenteNo ratings yet
- 012 Analysis of Reticulocyte Parameters On The Sysmex XEDocument8 pages012 Analysis of Reticulocyte Parameters On The Sysmex XEblanket_thNo ratings yet
- Erroneous Automated Optical Platelet Counts PDFDocument8 pagesErroneous Automated Optical Platelet Counts PDFfar faraNo ratings yet
- Comparison of ABX PENTRA 120 Retic, Sysmex R-2000, Flow Cytometry, and Manual CountsDocument10 pagesComparison of ABX PENTRA 120 Retic, Sysmex R-2000, Flow Cytometry, and Manual CountsdayanaNo ratings yet
- XE-2100 Automated Hematology System: Fast, Accurate, DependableDocument8 pagesXE-2100 Automated Hematology System: Fast, Accurate, Dependablehery_140978No ratings yet
- Validation of The Body FL Uid Module On The New Sysmex XN-1000 For Counting Blood Cells in Cerebrospinal FL Uid and Other Body FL UidsDocument8 pagesValidation of The Body FL Uid Module On The New Sysmex XN-1000 For Counting Blood Cells in Cerebrospinal FL Uid and Other Body FL UidsbalkisNo ratings yet
- Hematology BasicDocument4 pagesHematology BasicAjay DataniyaNo ratings yet
- Hema I Ass 4 GenericDocument1 pageHema I Ass 4 GenericTilahun TesemaNo ratings yet
- Science: Assessment of The Reliability of The Sysmex XE-5000 Analyzer To Detect Platelet ClumpsDocument6 pagesScience: Assessment of The Reliability of The Sysmex XE-5000 Analyzer To Detect Platelet ClumpsnivmastNo ratings yet
- Equ28-01 Sysmex XE2100 Op SOPDocument16 pagesEqu28-01 Sysmex XE2100 Op SOPWasim AkramNo ratings yet
- eJHaem - 2022 - Linko Parvinen - HemoScreen Hematology Analyzer Compared To Sysmex XN For Complete Blood Count White BloodDocument9 pageseJHaem - 2022 - Linko Parvinen - HemoScreen Hematology Analyzer Compared To Sysmex XN For Complete Blood Count White Bloodrince noveliaNo ratings yet
- Optimization of Laboratory Workflow in Clinical Hematology Laboratory With Reduced Manual Slide Review: Comparison Between Sysmex XE-2100 and ABX Pentra DX120Document8 pagesOptimization of Laboratory Workflow in Clinical Hematology Laboratory With Reduced Manual Slide Review: Comparison Between Sysmex XE-2100 and ABX Pentra DX120Marice Ferrufino SchmidtNo ratings yet
- 023 Evaluation of The Sysmex UF-100 AutomatedDocument4 pages023 Evaluation of The Sysmex UF-100 Automatedblanket_thNo ratings yet
- 022 Leucocyte Differentiation With The XT-SeriesDocument6 pages022 Leucocyte Differentiation With The XT-Seriesblanket_thNo ratings yet
- 012 Analysis of Reticulocyte Parameters On The Sysmex XEDocument8 pages012 Analysis of Reticulocyte Parameters On The Sysmex XEblanket_thNo ratings yet
- 011 Evaluation of The Automated Immature Granulocyte CountDocument1 page011 Evaluation of The Automated Immature Granulocyte Countblanket_thNo ratings yet
- Precision and Accuracy of The Leukocyte DifferentialDocument14 pagesPrecision and Accuracy of The Leukocyte Differentialblanket_thNo ratings yet
- 008the Technology of ReagentsDocument7 pages008the Technology of Reagentsblanket_thNo ratings yet
- Doctors Order LoveDocument4 pagesDoctors Order LoveAubrey Unique EvangelistaNo ratings yet
- Test Bank For Surgical Technology Principles and Practice 6th Edition by Fuller DownloadDocument11 pagesTest Bank For Surgical Technology Principles and Practice 6th Edition by Fuller DownloadCrystalDavisibng100% (17)
- Hematology 2015-2016 CM 299Document36 pagesHematology 2015-2016 CM 299Nadejda DoroseviciNo ratings yet
- Price List For 2020 (Februari) Asa LabDocument64 pagesPrice List For 2020 (Februari) Asa LabBintang Rejeki AlkesindoNo ratings yet
- ABG, CBC, BONE Marrow BiopsyDocument34 pagesABG, CBC, BONE Marrow Biopsymarthonsilva123No ratings yet
- XS-1000i Operators Instructions PDFDocument238 pagesXS-1000i Operators Instructions PDFNicoleta Roxana Calcan Rizea80% (10)
- Quality Assessment Schemes ProgramDocument24 pagesQuality Assessment Schemes ProgramShahrizad Mad SariffNo ratings yet
- Approach To The Adult Patient With Anemia - UpToDateDocument23 pagesApproach To The Adult Patient With Anemia - UpToDateNicole SierraNo ratings yet
- Science & Beyond Science Final1Document25 pagesScience & Beyond Science Final1Veeresh M Honnihal100% (2)
- BC-5300 - Service Manual - V5.0 - EN PDFDocument228 pagesBC-5300 - Service Manual - V5.0 - EN PDFalexandre xarebava0% (1)
- HematopoieticDocument1 pageHematopoieticborsk8674No ratings yet
- Haematology: DR - Abhilash Kumar JainDocument1 pageHaematology: DR - Abhilash Kumar Jainseds5anuragNo ratings yet
- Complete Blood CountDocument5 pagesComplete Blood Counttharaka100% (1)
- Maternal Anemia and Birth Weight: A Prospective Cohort StudyDocument14 pagesMaternal Anemia and Birth Weight: A Prospective Cohort StudyHumairah AnandaNo ratings yet
- 25 Yr(s) Sex:Male 13190414867 26 Apr 2019 15:15 26 Apr 2019 18:48Document1 page25 Yr(s) Sex:Male 13190414867 26 Apr 2019 15:15 26 Apr 2019 18:48arpan mukherjeeNo ratings yet
- Zainab Muhammad T.RDocument31 pagesZainab Muhammad T.RAdam AbubakarNo ratings yet
- Ygeia Medical Center - Manila, PhilippinesDocument3 pagesYgeia Medical Center - Manila, PhilippinesKratos de GuzmanNo ratings yet
- Mispa Count Plus 1Document2 pagesMispa Count Plus 1Tony DanartoNo ratings yet
- Biochemistry Hematology RequisitionDocument1 pageBiochemistry Hematology RequisitionRhodjane Dela CruzNo ratings yet
- Module 4 Soap NoteDocument5 pagesModule 4 Soap Noteapi-539434803No ratings yet
- 16CB01OIC0628Document38 pages16CB01OIC0628Satish GuptaNo ratings yet
- NCM 417 - Midterm Exam 2015Document5 pagesNCM 417 - Midterm Exam 2015Mae DacerNo ratings yet
- Leukopenia and Neutropenia As A Predictors of Neonatal SepsisDocument8 pagesLeukopenia and Neutropenia As A Predictors of Neonatal SepsisYandiNo ratings yet
- Diagnostic Report: FinalDocument2 pagesDiagnostic Report: FinalPRIYANSHU NAMANNo ratings yet
- Evaluation of Pallor in ChildrenDocument23 pagesEvaluation of Pallor in ChildrenFlorie Lei BulosNo ratings yet
- Chemotherapy For PatientsDocument8 pagesChemotherapy For PatientsAlwin PrasetyaNo ratings yet
- Fully Automated Analyzers For The Determination of The Erythrocyte Sedimentation RateDocument8 pagesFully Automated Analyzers For The Determination of The Erythrocyte Sedimentation RateFelipe SarmentoNo ratings yet
- Dacie and Lewis Practical Haematology 12Th Edition Barbara J Bain Full ChapterDocument67 pagesDacie and Lewis Practical Haematology 12Th Edition Barbara J Bain Full Chapterwilliam.darrell229100% (4)
- DXH 500 Series CasebookDocument46 pagesDXH 500 Series CasebookphisantelaboratoryNo ratings yet
- Arif ReportsDocument3 pagesArif ReportsAinaNo ratings yet