Professional Documents
Culture Documents
PREECLAMPSIA
Uploaded by
Daly L. NacionalOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PREECLAMPSIA
Uploaded by
Daly L. NacionalCopyright:
Available Formats
Pre eclampsia Page |1
O
Presentors will be able to:
B J E C T I V E S
Explain briefly the disease process: its causes, effects, management, treatment, and possible preventions.
Determine the pathophysiology of the condition with their rationale for occurrence of each manifestation. Determine why certain management and medications are given and provided for the condition.
Explain briefly how and why certain diagnostic tests are done for the condition.
Review the concepts about the anatomy and physiology with regards to the condition. Provide health teachings to the patient about certain interventions in the maintenance of health care.
Discuss options for surgical management for Preeclampsia.
Students or audience will be able :
To recognize the cause and risk factors of Preeclampsia.
To develop a comprehensive assessment for the disease process.
To understand the anatomy and physiology of the Renal/Urinary System, Cardiovascular System, Vascular System, and Female Reproductive
System. Clinical Instructors will be:
Able to give recommendations or suggestions necessary for the improvement of the case sharing.
Able to ask questions regarding the case for further understandings.
Group2
Pre eclampsia Page |2
Able to evaluate the presentation with utmost fairness.
I N T R O D U C T I O N
Preeclampsia, also referred to as toxemia, is a medical condition where hypertension arises in pregnancy (pregnancy-induced hypertension) in association with significant amounts of protein in the urine. It refers to a set of symptoms rather than any causative factor. Preeclampsia has been described as a disease of theories, because the cause is unknown. Preeclampsia is a condition that typically starts after the 20th week of pregnancy and is related to increased blood pressure and protein in the mother's urine (as a result of kidney problems). It is the most common of the dangerous pregnancy complications; it may affect both the mother and the unborn child. Pre-eclampsia affects the placenta, and it can affect the mother's kidney, liver, and brain. When preeclampsia causes seizures, the condition is known as eclampsia-the second leading cause of maternal death in the U.S. Preeclampsia is also a leading cause of fetal complications, which include low birth weight, premature birth, and stillbirth. Preeclampsia may develop from 20 weeks gestation (it is considered early onset before 32 weeks, which is associated with increased morbidity). Its progress differs among patients; most cases are diagnosed pre-term. Preeclampsia may also occur up to six weeks post-partum. Preeclampsia is classified into mild and severe. Preeclampsia is mild in 75% of cases and severe in 25% of them. In its extreme, the disease may lead to liver and renal failure, disseminated intravascular coagulopathy (DIC), and central nervous system (CNS) abnormalities. If preeclampsiaassociated seizures develop, the disorder has developed into the condition called eclampsia. Mild preeclampsia is defined as the presence of hypertension (BP 140/90 mm Hg) on 2 occasions, at least 6 hours apart, but without evidence of end-organ damage in the patient.
Group2
Pre eclampsia Page |3
Severe preeclampsia is defined as the presence of 1 of the following symptoms or signs in the presence of preeclampsia:
SBP of 160 mm Hg or higher or DBP of 110 mm Hg or higher on 2 occasions at least 6 hours apart Proteinuria of more than 5 g in a 24-hour collection or more than 3+ on 2 random urine samples collected at least 4 hours apart Pulmonary edema or cyanosis Oliguria (< 400 mL in 24 h) Persistent headaches Epigastric pain and/or impaired liver function Thrombocytopenia Oligohydramnios, decreased fetal growth, or placental abruption The incidence of preeclampsia in the United States is estimated to range from 2% to 6% in healthy, nulliparous women. Among all cases of
the preeclampsia, 10% occur in pregnancies of less than 34 weeks' gestation. The global incidence of preeclampsia has been estimated at 5-14% of all pregnancies. In the Philippines, according to the Department of Health, Maternal Mortality Rate (MMR) is 162 out of 10,000 live births (Family Planning Survey, 2006). Maternal deaths account for 14% of deaths among women. For the past five years all of the causes of maternal deaths exhibited an upward trend. Preeclampsia showed an increasing trend of 6.89%; 20%; and 40%;. Ten women die every day in the Philippines from pregnancy and childbirth related causes but for every mother who dies, roughly 20 more suffer serious disease and disability. The only known treatments for eclampsia or advancing preeclampsia are abortion or delivery, either by labor induction or Caesarean section. Magnesium sulphate is the first-line treatment of prevention of primary and recurrent eclamptic seizures. The mother and the family deserve a careful teaching regarding the problem, its observation, and its treatment. Regular, adequate prenatal care is the best insurance for control of the complication.
Group2 A B G L N P P Q R Y
Pre eclampsia Page |4
Arteries - Arteries are strong, elastic vessels adapted for carrying blood away from the heart at relatively high pumping pressure. Bladder - a triangle-shaped, hollow organ located in the lower abdomen. Blood pressure - Blood pressure measures the force of blood against the walls of the blood vessels. Extra fluid in the body increases the amount of fluid in blood vessels and makes blood pressure higher. Narrow, stiff, or clogged blood vessels also raise blood pressure. Capillaries - The arterioles branch into the microscopic capillaries, or capillary beds, which lie bathed in interstitial fluid, or lymph, produced by the lymphatic system. Eclampsia - seizures that cannot be attributable to other causes, in a woman with preeclampsia. Endothelium - is the thin layer of cells that lines the interior surface of blood vessels, forming an interface between circulating blood in the lumen and the rest of the vessel wall. Filtration - The first step in formation of urine is filtration. Filtration is the process by which the blood that passes through the glomerulus is filtered out, so that only certain structures pass through into the proximal convoluted tubule. Glumerular filtration rate (GFR) the total volume of renal filtrate that the kidneys form in 1 minute; average is 100-125 mL/minute. Hyperreflexia - defined as overactive or over responsive reflexes.
Group2
Pre eclampsia Page |5
Hypoxia - inadequate oxygen tension at the cellular level, characterized by tachycardia, hypertension, peripheral vasoconstriction, dizziness, and mental confusion. Intrauterine Growth Retardation (IUGR) failure to grow at the expected rate in utero. Oncotic pressure is a form of osmotic pressure exerted by proteins in blood plasma that usually tends to pull water into the circulatory system. Oligohydramnios - amniotic fluid volume that is less than expected for gestational age. It is typically diagnosed by ultrasound examination and may be described qualitatively (eg, mild, moderate, or severe oligohydramnios) or quantitatively (eg, amniotic fluid index [AFI] <5). Peripheral resistance - this term refers to the resistance the vessels offer to the flow of blood. Proteinuria - The presence of abnormal quantities of protein in the urine, which may indicate damage to the kidneys. Prostacyclin - is a prostaglandin with vasodilator properties. Selective Reabsorption - This step is known as selective reabsorption because only some elements are reabsorbed back into the body. Scotomata - A partial loss of vision or a blind spot in an otherwise normal visual field. Thrombocytopenia - refers to lowering of the platelets, the blood cells that prevent us from bleeding. The medical term for a platelet is Thrombocyte. Thrombo stems from Greek word "Thrombos" which means clot. Term Penia stems from Latin and means reduction. Toxemia - an abnormal condition of pregnancy characterized by hypertension and edema and protein in the urine. Two kidneys - a pair of purplish-brown organs located below the ribs toward the middle of the back.
Group2
Pre eclampsia Page |6
Two ureters - narrow tubes that carry urine from the kidneys to the bladder. Thromboxane - is a prostaglandin with vasoconstrictor properties. Vasospasm - a condition in which blood vessels spasm, leading to vasoconstriction. Veins - Blood leaving the capillary beds flows into a series of progressively larger vessels, called venules, which in turn unite to form veins.
Group2
Pre eclampsia Page |7
H Y S I C A L
S S E S S M E N T
&
E V I E W
Y S Y T E M
An accurate physical assessment requires an organized and systematic approach using the techniques of inspection, palpation, percussion, and auscultation. It also requires a trusting relationship and rapport between the nurse and the patient to decrease the stress the patient may have from being physically exposed and vulnerable. The patient will be much more relaxed and cooperative if the nurse explains what will be done and the reason for doing it. While the findings of a nursing assessment do sometimes contribute to the identification of a medical diagnosis, the unique focus of a nursing assessment is on the patient's responses to actual or potential problems. The purposes for a physical assessment are: To obtain baseline physical and mental data on the patient. To supplement, confirm, or question data obtained in the nursing history. To obtain data that will help the nurse establish nursing diagnoses and plan patient care. To evaluate the appropriateness of the nursing interventions in resolving the patient's identified pathophysiology problems.
Group2
Pre eclampsia Page |8
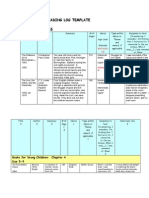
Systems General Appearance
Mild Preeclampsia Weight gain 2 lbs/week in 2nd trimester and 1lb/wk in 3rd trimester Mild edema none none none none
Severe Preeclampsia Weight gain of 3 or more lbs/wk in 2nd or 3rd trimester Headache Edema in the Face, Blurred vision none none Shortness of Breath (use of accessory muscle) Pulmonary Edema none none 160/110 mm Hg Thrombocytopenia
Review of Systems Patient may verbalize body weakness Patient may report headache or dizziness. Patient may report blurring of vision none none Patient may verbalize difficulty in breathing none none Patient may report chest pain and fatigue
Problem Identified Fluid volume excess
Head/Hair/Face EENT Mouth and Pharynx Neck Thorax/Lungs
Ineffective tissue perfusion Volume Excess Risk for injury, Altered Sensory perception No problem identified No problem identified Bradypnea, Ineffective breathing pattern No problem identified No problem identified Decreased cardiac output
Back Breast and Axilla
none none
Cardiovascular/Peripheral 140/90 mmHg taken at Vascular least 6 hours.
Group2
Pre eclampsia Page |9
Lymphatic GIT
none Nausea
none Excessive Vomiting, nausea, Severe Epigastic Pain RUQ Proteinuria (3- 5 g on a 24 hr. sample) Elevated serum creatinine as lab test revealed Oliguria (500mL less than in 24 hrs) Fatigue Extensive edema Puffiness in hands Altered consciousness, Seizure/Brain damage none
none Patient may report epigastric discomfort Patient may verbalize decreased urine output
No problem identified Risk Fluid volume deficit Acute pain Altered Comfort Less urine output
GUT
Oliguria Proteinuria of 1-2+ on a random sample
Musculoskeletal Integumentary Neurologic Endocrine
none none Headache, dizziness none
Patient may verbalize fatigue Patient may verbalize body weakness Patient may verbalize severe headache, dizziness none
Fatigue Ineffective Tissue perfusion Risk for injury Acute Pain No problem identified
Group2
P r e e c l a m p s i a P a g e | 10
I A G N O S T I C
E S T
Group2
P r e e c l a m p s i a P a g e | 11
Diagnostic Test Serum Creatinine
Purpose
Normal Values
Results and interpretation
Nursing responsibilities
-To assess glomerular In men: 0.8to Elevated levels generally indicate renal filtration 1.2 mg/dL disease that has seriously damage 50% -to screen for renal damage In women: 0.6 or more of the nephrons. to 0.9 mg/dL
Pre test: -Explain to the patient that the test evaluates kidney function. -Tell the patient that the test requires a blood sample. Explain who will perform the venipunture and when. -Explain to the patient that he may experience slight discomfort from the tourniquet and needle puncture. -Instruct the patient that he need not restrict food and fluids. -Notify the laboratory and physician of drugs he patient is taking that may affect test results it may be necessary to restrict them. Post test: -Apply direct pressure to the venipuncture site until bleeding stops. -Inform the patient that he may resume his usual medications discontinued before the test.
Group2
P r e e c l a m p s i a P a g e | 12
Diagnostic Test
Purpose
Normal Values
Results and interpretation
Nursing responsibilities
Blood Urea Nitrogen
To evaluate Kidney function and aid in the diagnosis of renal disease and to aid in the assessment of hydration.
8-20mg/dL
. Elevated levels: Renal disease. Reduced renal blood flow(caused by dehydration, for example) urinary tract obstruction and increased protein catabolisms (such as burns)
Pre test: Tell the patient that this test is used to evaluate kidney function. Inform the patient that he need not to restrict food and fluids but should avoid a diet high in meat.
Lower levels: Severe hepatic damage, Tell the patient that the test malnutrition, and over hydration. requires a blood sample. Explain who will perform the venipuncture and when. Explain to the patient that he may experience slight discomfort from the tourniquet and the needle puncture. Notify the laboratory and physician of drugs the patient is taking hat may affect test results they may be need to be restricted. Post test: -apply direct pressure to the venipunture site until bleeding stops. -inform the patient that he may resume taking his usual medications stopped before the test.
Group2 A B G L N P P Q R Y
P r e e c l a m p s i a P a g e | 13
Group2
Diagnostic Test
Purpose
Normal Values
Results and interpretation
Nursing responsibilities
P r e e c l a m p s i a P a g e | 14
Bleeding time
-To assess overall hemostatic function (platelet response to injury and functional capacity of vasoconstriction) -To detect platelet function disorders.
3 to 6 minutes Abnormal bleeding time may indicate in the template disorders linked to thrombocytopenia, method such as hodgkins disease, acute 3 to 6 minutes leukemia, disseminated intravascular in the ivy coagulation, hemolytic disease of the method newborn. 1 to 3 minutes in the duke Prolong bleeding time in a pt with method normal platelet count suggest a platelet function disorder and requires further investigation with clot retraction, prothrombin consumption and platelet aggregation test.
Pre test: -Explain o the patient that the bleeding time test measures the time it takes to form a clot and sop bleeding. -Tell the patient who will perform he test and when it will take place. -Inform the patient that he may feel some discomfort from the incisions the antiseptic, and the tightness if the blood pressure cuff. -Inform the patient that depending on the method used, incisions or punctures may leave tiny scars that should be barely visible when healed. -Notify the laboratory and physician of drugs the patient is taking that may affect test results it may be necessary to restrict them. Post test: -In a patient with a bleeding tendency, maintain a pressure bandage over the incision for 24-48 hours to prevent further bleeding. Check the test area frequently, keep the edges of the cuts aligned to minimize scaring.
Group2
P r e e c l a m p s i a P a g e | 15
Diagnostic Test
Purpose
Normal Values
Results and interpretation
Nursing responsibilities Pre test -Explain to pt that this test heart and liver functions. -Inform the pt that the test usually requires three venipunctures one on admission and one each day for the next two days. -Tell the pt that he need not restrict foods and fluids. -Notify the laboratory and physician drug of the pt is taking that may affect test results it may be necessary to restrict them. the until
Liver Enzyme Aspartate Aminotransferase (AST)
-To aid detection and differential diagnosis of acute hepatic disease. -To monitor patient progress and prognosis in cardiac and hepatic diseases. -To aid diagnosis of m.i in correlation with creatine kinase and lactate dehydrogenase levels.
12-31 units/liter
Ast levels fluctuate in response to the extent ofcellular necrosis, being transiently and minimally increase early in disease process and extremely increase durng the most acutephase. Depending on when the initial sample is drawn, ast levels may increase indicating increasing disease severity and tissue damage, or decrease, indicatinf disease resolution and tissue repair. -Maximum elevations more than 20 times normal may indicate acute viral hepatitis , severe skeletal muscle trauma, extensive surgery, drug induced hepatic injury,or severe passive liver congestion-
Post test -high levels 10 to 20 times normal may -Apply direct to indicate a severe m.i, severe infectious venipuncture site mononucleosis, or alcoholic cirrhosis. bleeding stops.
-Instruct the patient that he may resume medications stopped before the test.
Group2
Diagnostic Test
Purpose
Normal values Acceleration of the FHR about 15 bets/min. and remained elevated for 15 seconds (done for 10-20 minutes).
Results and interpretation
Nursing responsibilities
P r e e c l a m p s i a P a g e | 16
Nonstress, Fetal (NST, Fetal Activity Determination)
-The NST is a method to evaluate the viability of a fetus. It documents the placentas ability to provide an adequate blood supply to the fetus. The NST can be used to evaluate any high-risk pregnancy in which fetal well-being may be threatened. These pregnancies includes those marked by diabetes, hypertensive disease of pregnancy (toxemia), intrauterine growth retardation, Rhfactor sensitization, history of stillbirth, postmaturity, or low estriol levels.
Test results for the NST may Pretest be reactive (or normal)- 2 or more fetal heart rate -Explain the procedure to the client. increases in the testing period -Encourage the verbalization of the (usually 20 minutes) patients fears. The necessity for the Non-reactive-there is no study usually raises realistic fears in change in the fetal heart rate the expectant mother. when the fetus moves. This may be indicate a problem -If the patient is hungry, instruct her to that requires further testing. eat before the NST is begun. Fetal activity is enhanced with a high maternal serum glucose level. During -After the patient empties her bladder, place her in the Sims position. -Place an external fetal monitor on the patients abdomen to record the FHR. The mother can indicate fetal movement by pressing a button on the fetal monitor whenever she feels the fetus move. -The FHR and fetal movement are concomitantly recorded on a twochannel strip graph. -Observe the fetal monitor for FHR accelerations associated with fetal movement. -If the fetus is quiet for 20 minutes, stimulate fetal activity by external methods, such as rubbing or compressing the mothers abdomen,
Group2
P r e e c l a m p s i a P a g e | 17
Diagnostic Test
Purpose
Normal values Your baby will be scored on five things during the test. A score of 0 (abnormal) or 2 (normal) will be given in each of these categories: -Muscle movements -Body movements -Breathing movements -Amniotic fluid levels -Heart rate
Results and interpretation
Nursing responsibilities A towel or cloth can be used to wipe off excess gel and dry the abdomen after the test. In the event that test results indicate fetal compromise, a health care professional should remain with the mother to provide emotional support and answer questions as needed.
Biophysical profile
-Measures your baby's heart rate, muscle tone, movement, breathing, and the amount of amniotic fluid around your baby
-A score of eight or 10 out of 10 provides a reassuring BPP score. If the score is eight, with a decrease in amniotic fluid volume, delivery may be indicated, with fetal maturity. -A score of six arouses suspicions of chronic fetal hypoxia. A repeat test within four to six hours may be ordered. Delivery may be indicated if there is a reduction in the amniotic fluid volume. -A score of four is suspicious of chronic fetal hypoxia. A fetal lung maturity test may be done to assess readiness for delivery. Delivery is indicated if a repeat BPP after 24 hours confirms a score of four or below. -A score of zero to two elicits a strong suspicion of chronic fetal hypoxia. The BPP testing period may continue for two hours instead of the usual 30 minutes. If the twohour score is four or below, delivery is indicated if the fetus has a good chance at extrauterine survival.
Group2
P r e e c l a m p s i a P a g e | 18
Diagnostic Test
Purpose
Normal values
Results and Interpretation
Nursing Responsibilities
Platelet Count
platelet Adults: 140,000 >A count below 50,000/ul can cause spontaneous to 400,000/ul bleeding when the count is below 5,000/ul, fatal central nervous system -To assess the effects of bleeding or massive GI chemotherapy or hemorrhage is possible. radiation therapy on platelet production. > A decreased count can result to from aplastic or hypoplastic bone marrow; infiltrative bone marrow disease sush as leukemia, or disseminated infection. -To evaluate production.
Pre test -Explain to the pt. that the platelet count determines whether the clots normally. -Tell the pt that the test requires blood sample. Explain who will perform the venipuncture and when. -Notify the laboratory and physician of drugs the pt is taking that may affect test results, it may be necessary to restrict them. -Inform the pt that he need not to restrict food and fluids. Post test -Make sure subdermal bleeding has stopped before removing pressure. >Instruct the patient that he may resume his usual diet and medications discontinued before the test. -If a large hematoma develops at the venipuncture site, monitor pulses.
Group2
P r e e c l a m p s i a P a g e | 19
Diagnostic Test Hematocrit
Purpose -To aid diagnosis of polycythemia, anemia or abnormal states of hydration. -To aid in the calculation erythrocyte indices.
Normal Value
Results and Interpretation
Nursing Resposibilities Pre test -Explain to the pt. that the hct test detects anemia and other abdominal conditions. -Tell that the test requires a blood sample. -Explain to the pt that he may feel slight discomfort from the tourniquet and needle puncture. -Inform the pt that he need not to restrict food and fluids. -If a pt is a child explain to him and his parents that small amount of blood will be taken from his fingers and ear lobes. Post test - Ensure subdermal bleeding has stopped before removing pressure. - To aid in the calculation of erythrocyte.
In men: 42% to >Low HCT suggest anemia, 52% hemodilution, or massive blood In women: 36% to loss >High HCT indicates 48% polycythemia or hemoconcentration caused by blood loss and dehydration
Group2
P r e e c l a m p s i a P a g e | 20
Diagnostic Test
Purpose
Normal Values
Results and interpretation
Nursing Resposibilities
Alanine Aminotransferase -To detect and evaluate (ALT) treatment of acute hepatic disease specially hepatitis and serosis without jaundice. -To distinguish between myocardial and hepatic tissue damage (use with aspartate amino transferase ). -To assess hepatotoxity of some drugs
8-50 iu/L
-Very high ALT levels up to 50 times normal suggest viral or severe drug induced hepatitis or other hepatic disease with extensive necrosis.
Pre test -Explain to the PT. that this test assesses levels liver functions.
-Tell the patient tat the test requires a blood sample. Explain -Moderate to high levels may who will perform the indicate infectious mononucleosis, venipuncture. chronic hepatitis, intra hepatic cholestasis or cholicystitis, early or -Inform the pt. that he need not improving acute viral hepatitis, or restrict food and fluids. severe hepatic congestion from heart failure. -Notify the laboratory and physician of drugs the pt is taking -Slight to moderate elevations of alt that may affect test results, it may appear in any conditions that may be necessary to restrict produces acute hepatocellular them. injury, such as active cirrhosis and Post test drug induced or alcoholic hepatitis. -Apply direct pressure to the -Marginal elevations occasionally venipuncture site until bleeding occur in acute myocardial stops. infarctions, reflecting secondary -Instruct the pt. that he may hepatic congestions or the release resume medications stop before of small amounts of ALT from the step. myocardial tissue.
Group2
Diagnostic Test
purpose
Normal values
Results and Interpretation
Nursing Responsibilities
P r e e c l a m p s i a P a g e | 21
Urinalysis (UA)
-To screen the patients Color, straw to Protein urine for the renal or urinary dark yellow Increased Levels tract disease Odor, slightly Nephrotic syndrome aromatic Glomerulonephritis Malignant hypertension -To help detect metabolic or Appearance, Diabetic glomerulosclerosis systemic disease unrelated clear Polycystic disease to renal disorder Specific gravity, Lupus erythematosus 100 Goodpastures syndrome Heavy-metal poisoning -To detect substances Bacterial pyelonephritis (drugs) Nephrotoxic drug therapy Renal disease involving the glomeruli is associated with Protein proteinuria. Trauma.Protein can spill into - 0-8 mg/dl the urine as a result of traumatic - 50-80 mg/24 destruction of the blood-urine barrier. hr (at rest) Macroglobulinemia. With - <250 mg/24 hr increased globulin within the (during exercise) blood, albumin is secreted in an attempt to to maintain ocncotic homeostasis. Multiple myelomas. Classically, mulptiple myelomas produce large amounts of protein (e.g., Bence-Jones protein) in the urine. Preeclampsia Congestive heart failure The pathophysiologic factors of these observations are many. Suffice it to say that albumin Group2 A B G L N P leaks from the glomeruli, which P Q R Y are temporarily damage by this illnesses.
Pretest: Explain that this analysis helps to diagnose renal or urinary tract disease and to evaluate over all body functions. Inform the patient that he need not restrict food and fluids. Notify the laboratory and physician of drugs the patient is taking that may affect laboratory results. Posttest: Inform the patient that he may resume his usual diet and medications.
P r e e c l a m p s i a P a g e | 22
Diagnostics
Purpose
Normal values
Results and interpretation Nursing responsibilities Low albumin levels can suggest liver disease. Other liver enzyme tests are ordered to determine exactly which type of liver disease. Low albumin levels can reflect diseases in which the kidneys cannot prevent albumin from leaking from the blood into the urine and being lost. In this case, the amount of albumin (or protein) in the urine also may be measured. Low albumin levels can also be seen in inflammation, shock, and malnutrition. Low albumin levels may Check the albumin level from the protein electrophoresis results. Many clinical problems are the result of a serum albumin deficit. Assess for peripheral edema in the lower extremities when the albumin level is decreased.Albumin is the major protein compound responsible for plasma colloid osmotic pressure. With a decreased albumin level, fluid seeps out of the blood vessels into the tissue spaces.
Serum albumin
A serum albumin test measures the amount of this protein in the clear liquid portion of the blood.
3.4 - 5.4 g/dL
Group2
P r e e c l a m p s i a P a g e | 23
also suggest conditions in which your body does not properly absorb and digest protein (like Crohn's disease or sprue) or in which large volumes of protein are lost from the intestines. High albumin levels usually reflect dehydration. Diagnostics
Assess for urinary output. Renal and collagen (lupus) diseases occur with abnormal protein fractions. Urine output should be 25mL/h or 600mL/24 hours.
Purpose 1st-trimester fetal ultrasound is done to: o Determine how your pregnancy is progressing. o Find out if you are pregnant with more than 1 fetus. o Estimate the age of the fetus (gestational age). o Estimate the risk of a chromosom e defect, such
Normal values
Results and interpretation
Nursing responsibilities A towel or cloth can be used to wipe off excess gel and dry the abdomen after the test. In the event that test results indicate fetal compromise, a health care professional should remain with the mother to provide emotional support and answer questions as needed.
Fetal ultrasound
The developing baby, placenta, amniotic fluid, and surrounding structures are normal in appearance and appropriate for the gestational age. Note: Normal results may vary slightly. Talk to your doctor about the meaning of your specific test results.
Typically, a fetal ultrasound offers reassurance that a baby is growing and developing normally. If your health care provider wants more details about your baby's health, he or she may recommend additional tests.
Group2
P r e e c l a m p s i a P a g e | 24
as Down syndrome. o Check for birth defects that affect the brain or spinal cord. 2nd-trimester fetal ultrasound is done to: o Estimate the age of the fetus (gestational age). o Look at the size and position of the fetus, placenta, and amniotic fluid. o Determine the position of the fetus, umbilica l cord, and the placenta during a procedure, such as an amniocent esis or umbilical cord
Group2
P r e e c l a m p s i a P a g e | 25
blood sampling. o Detect major birth defects, such as a neural tube defect or heart probl ems. 3rd-trimester fetal ultrasound is done to: o Make sure that a fetus is alive and moving. o Look at the size and position of the fetus, placenta, and amniotic fluid.
Group2
P r e e c l a m p s i a P a g e | 26
N
Cardiovascular system
O R M A L
N A T O M Y
&
H Y S I O L O G Y
The cardiovascular/circulatory system transports food, hormones, metabolic wastes,and gases (oxygen, carbon dioxide) to and from cells. Components of the circulatory system include: blood :consisting of liquid plasma and cells blood vessels (vascular system): the "channels" (arteries, veins, capillaries) which carry blood to/from all tissues. (Arteries carry blood away from the heart. Veins return blood to the heart. Capillaries are thin walled blood vessels in which gas/ nutrient/ waste Exchange occurs.) heart : a muscular pump to move the blood There are two circulatory "circuits": Pulmonary circulation, involving the "right heart," delivers blood to and from the lungs. The pulmonary artery carries oxygenpoor blood from the "right heart" to the lungs, where oxygenation and carbon-dioxide removal occur. Pulmonary veins carry oxygen-rich blood from the lungs back to the "left heart."Systemic circulation, driven by the "left heart," carries blood to the rest of the body. Food products enter the system from the digestive organs into the portal vein. Waste products are removed by the liver and kidneys. All systems ultimately return to the "right heart" via the inferior and superior vena cava.
Group2
P r e e c l a m p s i a P a g e | 27
A specialized component
of the
circulatory
system
is the
lymphatic system,
consisting
of
moving fluid (lymph/interstitial fluid); vessels (lymphatics); lymphnodes, and organs ( bone marrow, Liver , spleen, thymus). Through the flow of blood in and out of arteries, and into the veins, and through the lymph nodes and into the lymph, the body is able to eliminate the products of cellular breakdown and bacterial invasion.
Anatomy of the Heart
The heart is about the size of a man's fist. Located between the lungs, two-thirds of it lies left of the chest midline. The heart, along with the pulmonary (to and from the lungs) and systemic (to and from the body) circuits, completely separates oxygenated from deoxygenated blood. Internally, the heart is divided into four hollow chambers, two on the left and two on the right. The upper chambers of the heart, the atria (singular: atrium), receive blood via veins. Passing throughvalves(atrioventricular (AV) valves) , blood then enters the lower chambers, the ventricles. Ventricular contraction forces blood into the arteries.
Group2
P r e e c l a m p s i a P a g e | 28
Oxygen-poor blood empties into the right atrium via the superior and inferior vena cava. Blood then passes through the tricuspid valve into the right ventricle which contracts, propelling the blood into the pulmonary artery. The artery is the only artery that carries oxygen-poor blood. It branches to the right and left lungs. There, gas exchange occurs -- carbon dioxide diffuses out, oxygen diffuses in. Pulmonary veins, the only veins that carry oxygen-rich blood, now carry the oxygenated blood from lungs to the left atrium of the heart. Blood passes through the bicuspid into the left ventricle. The ventricle contracts, sending blood under high pressure through the aorta, the main artery for systemic circulation. The ascending aorta carries blood to the upper body; the descending aorta, to the lower body.
Group2
P r e e c l a m p s i a P a g e | 29
Vascular System - the Blood Vessels
Arteries, veins, and capillaries comprise the vascular system. Arteries and veins run parallel throughout the body with a web-like network of capillaries connecting them. Arteries use vessel size, controlled by the sympathetic nervous system, to move blood by pressure; veins use one-way valves controlled by muscle contractions.
Arteries Arteries are strong, elastic vessels adapted for carrying blood away from the heart at relatively high pumping pressure. Arteries divide into progressively thinner tubes and eventually become fine branches called arterioles. Blood in arteries is oxygenrich, with the exception o f t h e pulmonary artery, which carries blood to the lungs to be oxygenated. Capillaries The arterioles branch into the microscopic capillaries, or capillary beds, which lie bathed in interstitial fluid, or lymph, produced by the lymphatic system. Capillaries are the points of exchange between the blood and surrounding tissues. Materials cross in and out of the capillaries by
Group2
P r e e c l a m p s i a P a g e | 30
passing through or between the cells that line the capillary. The extensive network of capillaries is estimated at between 50,000 and 60,000 miles long. Veins Blood leaving the capillary beds flows into a series of progressively larger vessels, called venules, which in turn unite to form veins. Veins are responsible for returning blood to the heart after theblood and the body cells exchange gases, nutrients, and wastes. Pressure in veins is low, so veins depend on nearby muscular contractions to move blood along. Veins have valves that prevent back-flow of blood. Blood in veins is oxygen-poor, with the exception of the pulmonary veins, which carry oxygenated blood from the lungs back to the heart. The major veins, like their companion arteries, often takethe name of the organ served. The exceptions are the superior vena cava and the inferior vena cava, which collect body from all parts of the body (except from the lungs) and channel it back tothe heart. BLOOD PRESSURE High blood pressure (HBP) is a serious condition that can lead to coronary heart disease (also called coronary artery disease), heart failure, stroke, kidney failure, and other health problems. "Blood pressure" is the force of blood pushing against the walls of the arteries as the heart pumps blood. If this pressure rises and stays high over time, it can damage the body in many ways.
Group2
P r e e c l a m p s i a P a g e | 31
Blood pressure is measured as systolic (sis-TOL-ik) and diastolic (di-a-STOL-ik) pressures. "Systolic" refers to blood pressure when the heart beats while pumping blood. "Diastolic" refers to blood pressure when the heart is at rest between beats. You most often will see blood pressure numbers written with the systolic number above or before the diastolic number, such as 120/80 mmHg. (The mmHg is millimeters of mercurythe units used to measure blood pressure.)
Group2
P r e e c l a m p s i a P a g e | 32
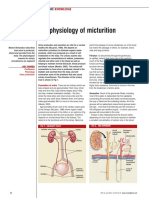
Urinary System
How do the kidneys and urinary system work? The body takes nutrients from food and converts them to energy. After the body has taken the food that it needs, waste products are left behind in the bowel and in the blood. The kidney and urinary systems keep chemicals, such as potassium and sodium, and water in balance and remove a type of waste, called urea, from the blood. Urea is produced when foods containing protein, such as meat, poultry, and certain vegetables, are broken down in the body. Urea is carried in the bloodstream to the kidneys.
Group2 A B G L N P P Q R Y
P r e e c l a m p s i a P a g e | 33
Other important functions of the kidneys include blood pressure regulation and the production of erythropoietin, which controls red blood cell production in the bone marrow.
Kidney and urinary system parts and their functions:
Two kidneys - a pair of purplish-brown organs located below the ribs toward the middle of the back. Their function is to remove liquid waste from the blood in the form of urine; keep a stable balance of salts and other substances in the blood; and produce erythropoietin, a hormone that aids the formation of red blood cells. The kidneys remove urea from the blood through tiny filtering units called nephrons. Each nephron consists of a ball formed of small blood capillaries, called glomerulus, and a small tube called a renal tubule. Urea, together with water and other waste substances, forms the urine as it passes through the nephrons and down the renal tubules of the kidney.
Two ureters - narrow tubes that carry urine from the kidneys to the bladder. Muscles in the ureter walls continually tighten and relax forcing urine downward, away from the kidneys. If urine backs up, or is allowed to stand still, a kidney infection can develop. About every 10 to 15 seconds, small amounts of urine are emptied into the bladder from the ureters.
Bladder - a triangle-shaped, hollow organ located in the lower abdomen. It is held in place by ligaments that are attached to other organs and the pelvic bones. The bladder's walls relax and expand to store urine, and contract and flatten to empty urine through the urethra. The typical healthy adult bladder can store up to two cups of urine for two to five hours.
Group2
P r e e c l a m p s i a P a g e | 34
Two sphincter muscles - circular muscles that help keep urine from leaking by closing tightly like a rubber band around the opening of the bladder.
Nerves in the bladder - alert a person when it is time to urinate, or empty the bladder.
Urethra - the tube that allows urine to pass outside the body. The brain signals the bladder muscles to tighten, which squeezes urine out of the bladder. At the same time, the brain signals the sphincter muscles to relax to let urine exit the bladder through the urethra. When all the signals occur in the correct order, normal urination occurs.
URINE FORMATION
Group2
P r e e c l a m p s i a P a g e | 35
Urine Formation Steps Filtration The first step in formation of urine is filtration. Filtration is the process by which the blood that passes through the glomerulus is filtered out, so that
Group2
P r e e c l a m p s i a P a g e | 36
only certain structures pass through into the proximal convoluted tubule. The rate at which the blood is filtered is known as the glomerular filtration rate, which is normally 125 ml/minute or 180 liters/day! The glomerulus lining is such that it only allows small molecules to filter through, like glucose, plasma, ions like sodium and potassium, urea, etc. The larger molecules, like blood cells and protein cannot pass through the glomerulus. This is the reason that when there are kidney diseases, the glomerulus lining is affected, due to which the protein molecules also pass through, leading to blood and protein in urine. Selective Reabsorption As mentioned above, in filtration step of urine formation, there is only crude and elementary separation of waste products and a lot of water, glucose and other important materials also pass through. Thus, there is need for reabsorption of these important elements back into the body, which is where the second step, that is reabsorptions, comes in. This step is known as selective reabsorption because only some elements are reabsorbed back into the body. Reabsorption occurs in two steps, which is active reabsorption (which requires energy) and passive reabsorption (which does not require energy). Due to the difference in concentration of the fluid inside and outside the tubules, 99% of the water returns into circulation and thus, is passively absorbed, which is important for urine formation and flow. Provided the glucose levels are normal, almost all of the glucose is reabsorbed back into the blood from the proximal tubules. This glucose is actively transported into the peritubular capillaries. However, when there is a very large amount of glucose in the blood, then some of it passes into the urine, which is one of the signs of diabetes. Sodium ions are the only ions that are partially absorbed from the renal tubules back into the blood. Tubular Secretion The last step in urine formation is tubular secretion. This is the step where the urine is made concentrated by increasing the concentration of waste elements. Thus, in this stage, substances move into the distal and collecting tubules from blood in the capillaries around these tubules. These
Group2
P r e e c l a m p s i a P a g e | 37
substances are secreted by the mechanism of active transport. The substances secreted include hydrogen ions, potassium ions, ammonia, and certain drugs or metabolic end products. Thus, the kidney tubules play a crucial role in maintaining the body's acid-base balance and maintaining the electrolyte balance in the body. The distal convoluted tubules then drain the urine into the collecting tubules. Then, several collecting tubules join together to drain their contents into the collecting duct, which finally, after urine formation, flows into the ducts of Bellini. This then eventually reaches the renal pelvis, from where the urine flows into the ureter to reach the urinary bladder. Thus, these were the various urine formation steps that take place right from the time when blood flows into the kidneys, till urine is passed into the ureters. The various urinary system diseases occur when there are problems with the functioning of the kidneys, which reflects in the final urine color, odor and concentration.
The Female Reproductive System
Group2
P r e e c l a m p s i a P a g e | 38
Group2
P r e e c l a m p s i a P a g e | 39
The female reproductive system is designed to carry out several functions. It produces the female egg cells necessary for reproduction, called the ova or oocytes. The system is designed to transport the ova to the site of fertilization. Conception, the fertilization of an egg by a sperm, normally occurs in the fallopian tubes. After conception, the uterus offers a safe and favorable environment for a baby to develop before it is time for it to make its way into the outside world. If fertilization does not take place, the system is designed to menstruate (the monthly shedding of the uterine lining). In addition, the female reproductive system produces female sex hormones that maintain the reproductive cycle. During menopause the female reproductive system gradually stops making the female hormones necessary for the reproductive cycle to work. When the body no longer produces these hormones a woman is considered to be menopausal. The function of the external female reproductive structures (the genital) is twofold: To enable sperm to enter the body and to protect the internal genital organs from infectious organisms. The main external structures of the female reproductive system include: Labia majora: The labia majora enclose and protect the other external reproductive organs. Literally translated as "large lips," the labia majora are relatively large and fleshy, and are comparable to the scrotum in males. The labia majora contain sweat and oil-secreting glands. After puberty, the labia majora are covered with hair. Labia minora: Literally translated as "small lips," the labia minora can be very small or up to 2 inches wide. They lie just inside the labia majora, and surround the openings to the vagina (the canal that joins the lower part of the uterus to the outside of the body) and urethra (the tube that carries urine from the bladder to the outside of the body). Bartholins glands: These glands are located next to the vaginal opening and produce a fluid (mucus) secretion.
Group2
P r e e c l a m p s i a P a g e | 40
Clitoris: The two labia minora meet at the clitoris, a small, sensitive protrusion that is comparable to the penis in males. The clitoris is covered by a fold of skin, called the prepuce, which is similar to the foreskin at the end of the penis. Like the penis, the clitoris is very sensitive to stimulation and can become erect.
The internal reproductive organs include: Vagina: The vagina is a canal that joins the cervix (the lower part of uterus) to the outside of the body. It also is known as the birth canal.
Uterus (womb): The uterus is a hollow, pear-shaped organ that is the home to a developing fetus. The uterus is divided into two parts: the cervix, which is the lower part that opens into the vagina, and the main body of the uterus, called the corpus. The corpus can easily expand to hold a developing baby. A channel through the cervix allows sperm to enter and menstrual blood to exit.
Ovaries: The ovaries are small, oval-shaped glands that are located on either side of the uterus. The ovaries produce eggs and hormones.
Fallopian tubes: These are narrow tubes that are attached to the upper part of the uterus and serve as tunnels for the ova (egg cells) to travel from the ovaries to the uterus. Conception, the fertilization of an egg by a sperm, normally occurs in the fallopian tubes. The fertilized egg then moves to the uterus, where it implants to the uterine wall.
Group2
P r e e c l a m p s i a P a g e | 41
PLACENTA AND FUNCTION
Group2
P r e e c l a m p s i a P a g e | 42
The placentas primary role is to ensure that oxygen is moved into your babys blood stream and carbon dioxide is carried away from your baby however the waste is not limited to oxygen and also includes cleaning out other waste which is produced by your baby. In the same way that it ensures oxygen reaches your baby, it also plays a role in ensuring that some nutrients are received. The placenta is an extremely complex piece of biological equipment. It is a little bit like an artificial kidney, it allows your blood and the baby's to come into very close contact - but without ever mixing. This enables your blood to pass across nutrients and oxygen to the baby, and waste products like carbon dioxide to go back from baby to mother. It acts as the lung, kidney and digestive system for the baby. The placenta also plays an important role in hormone production. Human chronic gonadotropin, or hCG is produced by the placenta. This hormone can be found in your babys blood stream as early as 10 days into your pregnancy. This is of course not the only hormone which the placenta produces as it is also responsible for the production of estrogen and progesterone . The placenta also performs the important function of protecting your baby for possible infection however, it is not always able to distinguish between what is a good substance and what isnt and this is why pregnant women are asked to avoid substances which may cause harm, such as caffeine, alcohol, herbal substances and drugs.
Group2
P r e e c l a m p s i a P a g e | 43
A T H O P H Y S I O L O G Y
Group2
P r e e c l a m p s i a P a g e | 44
N
Problem: Epigastric pain (right upper quadrant)
U R S I N G
A R E
L A N S
Nursing diagnosis: Acute epigastric pain (right upper quadrant) related to poor oxygenation of the pancreas and liver secondary to preeclampsia Cause analysis: In PIH, the cardiac system can become overwhelmed because the heart is forced to pump against rising peripheral resistance. This reduces the blood supply to organs. Most markedly the kidney, pancreas, liver, brain and placenta. ISCHEMIA IN THE PANCREAS AND LIVER may result in EPIGASTRIC PAIN. (Maternal and Child nursing by ADELE PILLITTERI 5th edition pp.426 )
CUES
OBJECTIVE
NURSING INTERVENTION
RATIONALE
EVALUATION
INDEPENDENT SUBJECTIVE: Patient may verbalize, STO: 1. Determine pain history, e.g. location of pain, After 4 hours of frequency, duration, and relaxation, patient will be intensity using pain scale alleviated from pain as and relief measures evidenced by absence used. of facial grimace and pain scale of 4/10. 2. Explain that nerves are severed or damaged but that analgesics and narcotics are available with doctors prescription. LTO: 3. Promote proper body
Group2 A B G L N P P
1. Change in pain characteristics may indicate developing complications
The patient is expected to manifest: Decrease pain scale of 4/10 from 8/10. Maintains rest without disturbance from pain Maintains relaxation technique Resumes ADL
Pain on the right upper quadrant of the abdomen,
2. Reduces abdominal tension and promotes sense of control.
OBJECTIVE:
P r e e c l a m p s i a P a g e | 45
Irritable. From 0-10, pain can be rated as 8. Grimacing face
After 2 days of duty, pain will be relieved and patient resumes to her normal physical activity such walking, reaching out objects, etc.
positioning to promote comfort, such as semi fowlers position and elevation of the arm on the affected side. 4. Provide alternative comfort measures such as backrubs and encourage relaxation techniques such as guided imagery, visualization, quiet diversional activities such as watching T.V and listening to radio.
3. promotes relaxation
4. promote relaxation and enables client to refocus attention and may enhance coping.
5. Aids in relaxing the abdominal muscles
5. Encourage protection and the avoidance of anything that can break through the skin barrier or impose stress on the arm and shoulder.
Reference: Joyce M. Black, et.al. , Medical Surgical Nursing, Clinical Management for Positive Outcomes, 6th edition
Group2
P r e e c l a m p s i a P a g e | 46
Problem: Edema Nursing Diagnosis: Deficient fluid volume related to plasma protein loss, decreasing plasma colloid osmotic pressure allowing shifts out of vascular compartment secondary to preeclampsia Cause analysis: Vasospasm in the kidney increase blood flow resistance. Degenerative changes develop in kidney glomeruli because of backpressure. This lead to increase permeability of glomerular membrane, allowing the serum proteins albumin and globuline to escape into the urine (protinuria) . The degenerative changes also results in decreases in glomerular filtration so there is lowered urine output and clearance of creatinine. Increase kidney tubular reabsorption occurs because sodium retains fluid retention (EDEMA). Edema is further increase because protein is lost the osmotic pressure of the circulating blood falls and fluid diffuses from the circulatory system into the denser interstitial spaces to equalized the pressure. (Maternal and Child nursing by ADELE PILLITTERI 5th edition pp.426 ) CUES OBJECTIVES NURSING INTERVENTIONS INDEPENDENT: SUBJECTIVE: STO: 1. Set an appropriate rate of fluid intake/infusion throughout 24-hour period 2. Monitor urine specific gravity. 3. Weigh daily at same time of day, on same scale, with same equipment and clothing. 1. to prevent peaks/valleys in fluid level. 2. Measures the kidneys ability to concentrate urine. In intrarenal failure, specific gravity is usually equal to/less than 1.010, indicating loss of ability to concentrate the urine. 3. Daily body weight is best monitor of fluid status. A weight gain of more than 0.5 kg/day suggests fluid retention. 4. Edema occurs primarily in The patient is expected to manifest : Increase urine output as evidence by BP within normal range. Stable weight Vital signs within Normal range Absence of EDEMA RATIONALE EVALUATION
The patient may report less amount of urination.
Within 8 hours of effective nursing interventions, patient will be able to manifest increase urine output as evidenced by BP within individuals normal range and urine output within the range of 3040ml/hr.
4. Assess skin, face, dependent areas for edema. Evaluate degree of
Group2
P r e e c l a m p s i a P a g e | 47
edema (on scale of +1+4).
OBJECTIVE:
LTO: 5. Evaluate edematous extremities, change position frequently.
dependent tissues of the body, e.g., hands, feet, lumbosacral area. Patient can gain up to 10 lb (4.5 kg) of fluid before pitting edema is detected. 5. to reduce tissue pressure and risk of skin breakdown
Within 3 days of giving effective nursing Decrease interventions, patient urine will be able to manifest output(less a fluid balance as than 30ml evidenced by /hr). appropriate urinary Blood output, stable weight, pressure above 140/90 vital signs within normal Pulse rate range and absence of greater than edema. 100 Weight gain Edema
6. Auscultate lung and heart sounds. 7. Assess level of consciousness; investigate changes in mentation, presence of restlessness. 8. Place in semi-fowlers position as appropriate 9. Suggest interventions, such as frequent oral care, chewing gum/hard candy, use of lip balm.
6. Fluid overload may lead to pulmonary edema and HF evidenced by development of adventitious breath sounds, extra heart sounds. (Refer to ND: Cardiac Output, risk for decreased, following.) 7. May reflect fluid shifts, accumulation of toxins, acidosis, electrolyte imbalances, or developing hypoxia. 8. to facilitate movement of diaphragm improving respiratory effort.
Group2
P r e e c l a m p s i a P a g e | 48
10. Promote bed rest..
9. to reduce discomforts of fluid restrictions. 10. The best method of aiding increased evacuation of sodium and encouraging diuresis.
COLLABORATIVE:
1. Administer diuretics as prescribed after pregnancy.
1. Promote adequate urine volume
Reference: Joyce M. Black, et.al. , Medical Surgical Nursing, Clinical Management for Positive Outcomes, 6th edition
Group2
P r e e c l a m p s i a P a g e | 49
Problem: Proteinuria Nursing Diagnoses: Altered urinary elimination r/t fluid shifting secondary to preeclampsia Cause analysis: Increase nutrient loses because of the excretion of the protein in the urine. Body proteins are use for energy when calorie intake is insufficient. Increase nutrient requirements as a pregnant women they need sufficient nutrients to provide their needs and to the fetus. Energy requirements are essential for fetal and placental growth but because of some food restrictions it is not well provided.( Med-Surgical 6th edition by: Black,pg.1426.)A
Cues Subjective: The patient may verbalized: Complaints of some food restrictions.
Objectives STO: After 8 hours of effective nursing intervention patient will be able to verbalize understanding about dietary needs consist of intake of high protein foods such as milk product, fish, and poultry. Avoiding high sodium foods such as cheese, goat milk, carrot juice, butter.
Nursing intervention
Rationale
Evaluation The patient is expected to manifest:
Independent: 1. Assess clients nutritional status, condition of hair and nails, and height and pregravid weight. 2. Provide information about normal weight gain in pregnancy,
Objective: LTO: edema excess amount of protein in the urine. After 3 days of nursing interventions patient will be able to demonstrate knowledge of proper diet as evidenced by developing a dietary plan within own financial resources
1. Establishes guidelines for determining dietary needs and educating client. Malnutrition may be a contributing factor to the onset of PIH, specifically When client follows a lowprotein diet, has insufficient
Develop ed a dietary meal plan that was low sodium and low fat diet.
Group2
P r e e c l a m p s i a P a g e | 50
modifying it to meet clients needs because it places the fetus at risk for ketosis.
caloric intake, and is overweight or underweight by 20% or more before conception.
3. Provide oral/written information about action and uses of protein and its role in development of PIH. 4. Provide information about effect of bed rest and reduced activity on protein requirements.
2.The underweight client may need a diet higher in . calories; the obese client should avoid dieting
5. Use flavoring
3. Daily intake of 80100 g/day (1.5 g/kg) is sufficient to replace proteins lost in urine and allow for normal
Group2
P r e e c l a m p s i a P a g e | 51
agents (e.g. lemon and herbs) is salt is restricted
serum oncotic pressure. 4. Reducing metabolic rate through bed rest and limited activity decreases protein needs.
6. Limit fiber/bulk if indicated
7. promote pleasant, relaxing environment, including socialization when possible
5. to enhance food satisfaction and stimulate appetite
8. Prevent/minimiz e unpleasant odors/sights.
6. because it may lead to early satiety
7. To enhance intake.
Group2
P r e e c l a m p s i a P a g e | 52
9. Encourage use of lozenges and so forth 8. May have a negative effect on appetite/eating.
10. Promote adequate/timely fluid intake
9. To stimulate salivation when dryness is a factor
10. Limiting fluids 1 hour prior to meal decreases possibility of early satiety
Collaborative: Refer to
Group2 A B G L N P P Q R Y
Helpful in creating individual dietary
P r e e c l a m p s i a P a g e | 53
dietitian, as indicated.
plan incorporating specific needs/restriction s
Reference: Joyce M. Black, et.al. , Medical Surgical Nursing, Clinical Management for Positive Outcomes, 6th edition
Problem: Risk for Fetal Injury Nursing Diagnosis: Risk for (Fetal) Injury related to reduce placental perfusion secondary to vasoconstriction secondary to preeclampsia Cause Analysis: With severe preeclampsia, the cardiac system can become overwhelmed because the heart is forced to pump against rising peripheral resistance. This reduces blood supply to organs, most markedly in the kidneys, pancreas, liver, brain, and PLACENTA. Poor placental perfusion may reduce the fetal nutrient and Oxygen supply. (Maternal and child nursing by PILLITTERI 5th edition pp.426) CUES Subjective: ST0: OBJECTIVES NURSING INTERVENTIONS Independent: RATIONALE Independent: EVALUATION The fetus is expected to manifest:
Not applicable
After 8 hrs of nursing interventions, the patients placental perfusion will increase sd rvidenced by fetal heart rate within 120-
1. Monitor and assess vital signs. 2. Assess the patients general physical condition.
1. To obtain baseline 2. To determine presence of abnormality. normal HR (120-160 bpm) absence of signs of fetal distress
Group2
P r e e c l a m p s i a P a g e | 54
160 bpm. 3. Instruct mother to assume a left lateral position. 4. Promote bed rest.
3. To avoid putting pressure on the inferior vena cava. 4. To increase uteroplacental circulation and prevent too much workload on the heart. 5. To provide comfort. normal fetal movement in an hour (3 movements/hour)
LTO:
After 3 days of nursing Objective: interventions, the patient will demonstrate a decrease in systemic vasoconstriction to increase uteroplacental circulation as evidenced by intrauterine growth during ultrasound.
Patient manifested: A systemic vasoconstriction
5. Encourage relaxation techniques such as deep Breathing. 6. Encourage patient to avoid constipation by increasing fiber intake.
Patients fetus may manifest: Intrauterine growth retardation Changes in fetal activity/ heart rate(less than or more than 120160 bpm) Fetal demise
6. Straining defecation might put pressure on the uterus which could injured the already compromised fetal health. 7. To enhance patients participation in the treatment regimen. 8. For patient education.
7. Instruct mother on the possible complications the disease can cause to the fetus. 8. Discuss importance of having an adequate
Group2
P r e e c l a m p s i a P a g e | 55
blood circulation going to the placenta. Dependent:
.
1. To help in
respiration.
1. Administer oxygen as indicated. Reference: Nurses Pocket Guide Book, 9th edition by Doenges et.al pp.369
Problem identified; lack of knowledge Nursing diagnosis: Knowledge deficit [Learning Need] regarding condition,prognosis, self care and treatment needs related to lack of exposure/unfamiliarity with information resources, misinterpretation secondary to preeclampsia Cause analysis: Anticipatory anxiety and patient lacks in psychological and educational information. Cause analysis: A new problem or condition will acquire the individual to learn new behaviors to help maintain optimal health & function. Some information will be used only temporarily while other information will result in lifelong behavior change. (NDCP by Neal et.al.) Individuals coping with present illness with varied pharmacological treatment regimen, unfamiliar and often complex procedures, commonly experience a deficit in knowledge. (Medical surgical Nursing by Smeltzer and Bare 7th ed. pg. 1303)
Group2
P r e e c l a m p s i a P a g e | 56
Cues
Objectives STO:
Nursing interventions Independent: 1. Assess clients/couples knowledge of the disease process. 2. Provide information about pathophysiology of Pre-eclampsia, implications for mother and fetus; and the rationale for interventions, procedures, and tests, as needed.
Rationale The patient is expected to: 1. Establishes data base and provides information about areas in which learning is needed. Receiving information can promote understanding and reduce fear, helping to facilitate the treatment plan for the client. provide additional treatment options, such as using lowdose (60 mg/day) aspirin to reduce thromboxane generation by platelets, limiting Note: Current research in progress may severity/incidence of PIH (pre-eclampsia) 1. Verbalize accurate information about diagnosis, prognosis, and potential complications at own level of readiness. 2. Verbalize understanding of the therapeutic needs and will be able to identify/use available resources appropriately.
Questions/request for information misinterpretation Verbalization of problem Statement of misconception Inaccurate followthrough of instructions, development of preventable complications
After 2-3 days of nursing interventions and health teachings, the patient will be able to verbalize accurate information about diagnosis, prognosis, and potential complications at own level of readiness.
LTO: After 4-5 days of nursing interventions and health teachings, the patient will be able to verbalize understanding of the therapeutic needs and will be able to identify/use available resources appropriately.
3. Provide information about signs/symptoms indicating worsening of condition, and instruct client when to notify healthcare provider.
2. Helps ensure that client seeks timely treatment and may prevent worsening of preeclamptic state or
Group2
P r e e c l a m p s i a P a g e | 57
additional complications. 4. Keep client informed of health status, results of tests, and fetal wellbeing.
5. Instruct client in how to monitor her own weight at home, and to notify healthcare provider if gain is in excess of 2 lb/wk, or 0.5 lb/day. 6. Assist family members in learning the procedure for home monitoring of BP, as indicated. 7. Review techniques for stress management and diet restriction. 8. Provide information about ensuring adequate protein in diet for client with possible
3. Fears and anxieties can be compounded when client/couple does not have adequate information about the state of the disease process or its impact on client and fetus.
4. Gain of 3.3 lbs or greater per month in second trimester or 1 lb or greater per week in third trimester is suggestive of PIH. 5. Encourages participation in treatment regimen, allows prompt intervention as needed, and may provide reassurance that efforts are beneficial. 6. Reinforces importance of clients responsibility in treatment. 7. Protein is necessary for
Q R Y
Group2
P r e e c l a m p s i a P a g e | 58
or mild preeclampsia. Review self-testing of urine for protein. Reinforce rationale for and implications of testing.
intravascular and extravascular fluid regulation. 8. A test result of 2+ or greater is significant and needs to be reported to healthcare provider. Urine specimen contaminated by vaginal discharge or RBCs may produce positive test result for protein.
PROBLEM: Seizure NURSING DIAGNOSIS: Risk for injury related to fluid excess in cerebral area secondary to Pregnancy induced hypertension
Group2
P r e e c l a m p s i a P a g e | 59
CAUSE ANALYSIS: in patient having PIH (severe stage) there is vasoconstriction thus decrease blood supply on the brain. Decrease tissue perfusion in the brain will eventually lead to seizures. (Maternal and Child nursing by ADELE PILLITTERI 5th edition pp.426 )
Cues
Objectives
Intervention
Rationale
Evaluation
INDEPENDENT Subjective: The patient may verbalized: -Occurrence of seizure after delivery. STO: After giving nursing intervention, the pt will be able to explain ways to prevent injury as evidence by calling assistance whenever she goes to the restroom. 1. determined risk of falling 2. Thoroughly orient to environment. Show how to call assistance 3. Keep side rails up and maintain bed in low position; ensure that wheels are locked on bed and commode; keep dim light in room at right. 4. Assisted client to voiding at least every 4 hours. Take pt to the bathroom before bedtime. 5. Asked family or SO to stay with client. DEPENDENT: The patient is expected to manifest: Prevent cause of injury as evidence by calling assistance whenever she goes to the restroom. Absence of seizures Performs ADL Perform seizure precautions
1. it can help identify high risk of falling 2. This step alerts the nursing staff the increase risk of falls. 3. This safety measures are use as part of a fall prevention program. 4. studies have indicated that falls are often linked to the need in a hurry 5. To monitor pt and prevent pt from accidentally falling
Objective:
LTO: Within 1 week of hospital stay, the pt will be able to be free from Administered medication as prescribed by physician;
Group2
P r e e c l a m p s i a P a g e | 60
-Neurological deficit -Altered level of consciousness - Affected ADL. -Onset of seizures after surgery
injuries as evidenced by an absence of seizure activity.
magnesium sulfate
Essential for the activity of many enzymes. Plays an important role in neurotransmission and muscular excitability
REFERENCE: Tbers Cyclopedic Medical Dictionary 18th ed. by Thomas, Clayton p 441.
Group2
P r e e c l a m p s i a P a g e | 61
Problem Identified: Shortness of breath, dyspnea Nursing Diagnosis: Ineffective breathing pattern related to pulmonary edema. Cause Analysis: Pulmonary edema is one of the complications of PIH, and is due to the increased permeability of the capillaries causing the leakage of fluids to the insterstitial spaces of the lungs (Maternal and Child nursing by ADELE PILLITTERI 5th edition pp.426 . CUES Subjective: STO: OBJECTIVES NURSING INTERVENTION Independent: 1. Aauscultate lung fields, noting areas of decreased/absent airflow and adventitious breath sounds: e.g., crackles, wheezes. 1. Ddecreased airflow occurs in areas consolidated with fluid. Crackles and wheezes are heard on inspiration and/or expiration in response to fluid accumulation. 2. Ttachypnea, shallow respirations, and asymmetric chest movement are frequently present because of discomfort of moving chest wall and/or fluid in lung. 3. Kkeeping the head elevated lower RATIONALE EVALUATION The patient is expected to manifest: Aabsence of shortness of breath and dypsnea. Clear breath sound. Nno nasal flaring Nno use of accessory muscles
The patient may complain After 4 hours of proper of difficulty of breathing. nursing intervention the patient will be able to identify/demonstrate behaviors to achieve airway clearance as evidenced by absence of nasal flaring, use of accessory muscle, etc. Objective: Difficulty of breathing Orthopnea May have a respiratory rate of less than 12 bpm. Crackles, wheezing Nasal flaring Use of accessory muscle
LTO: After 2 days of proper nursing intervention the patient will display patent airway with breath sounds
Group2
2. Aassess rate/depth of respirations and chest movement.
P r e e c l a m p s i a P a g e | 62
clearing; absence of dyspnea.
3. Eelevate head of bed, change position frequently.
diaphragm, promoting chest expansion, aeration of lung segments, and mobilization and expectoration of secretions to keep airway clear. 4. Ddeep breathing facilitates maximum expansion of the lung/smaller airways. Coughing is a natural self-cleaning mechanism, assisting the cilia to maintain patent airway, and an upright position favors deeper, more forceful cough effort.
4. Aassist with frequent deepbreathing exercises. Demonstrate/help client to perform activity: e.g., effective coughing while in upright position.
5. Fliquids (especially warm liquids) aid in mobilization and expectoration of secretions. 5. Fforce fluids to at 3000mL/day
Group2 A B G L N P P Q R Y
P r e e c l a m p s i a P a g e | 63
(unless contratindicated). Offer warm, rather than cold, fluids. Dependent: 1. Aadminister oxygen as indicated for underlying pulmonary condition. Reference: NCP by Doenges, Moorehouse & Geissler Murr pp. 135-136. 1. Tto help in respiration.
Problem: Increased Blood pressure Nursing Diagnosis: Decreased cardiac output related to vasoconstriction secondary to vasospasm and sensitivity to pressor substances Cause Analysis: Normally, blood vessels during pregnancy are resistant to the effects of pressors substance such as angiotensin and norepinephrine, so blood pressure remains normal during pregnancy. With PIH, this reduce responsive to blood pressure changes appears to be lost. VASOCONSTRICTION occurs and blood pressure increase dramatically. (Maternal and Child nursing by ADELE PILLITTERI 5th edition pp.426 ) CUES Subjective: STO: OBJECTIVES NURSING INTERVENTION Independent: 1. Monitor BP in both
Group2 A B G L N P P Q
RATIONALE 1. Comparison of pressures provides more complete
R Y
EVALUATION The patient is expected to manifest:
P r e e c l a m p s i a P a g e | 64
The patient may verbalize :
Complaint of discomfort in neck, dizziness. Complaint of shortness of breath Complaint of weakness and fatigue.
After 8 hours of giving effective dependent and independent nursing care, the patient will demonstrate increase perfusion as evidenced by decreased BP to 120/90 mmHg.
arms, 3-5 minutes apart while client is at rest, sitting, standing, for initial evaluation. Use correct cuff size and accurate technique. 2. Note presence, quality of central and peripheral pulses.
picture of vascular involvement.
LTO Within 3 days giving effective nursing care, the patient will demonstrate hemodynamic stability as evidenced of BP within acceptable range of 120/80130/80.
3. Identify changes related to systemic peripheral alterations in circulation.
2. Bounding carotid, jugular, radial, femoral pulses maybe observed/ palpated. pulses in the legs/feet maybe diminished, reflecting effects of vasoconstriction and venous congestion. 3. To assess causative/ contributing factors
Participated activities the reduced BP/cardiac workload. Maintain BP within individually acceptable range. Demonstrate stable cardiac rhythm and rate within clients normal range 120/80-130/80.
Objective: Variation in blood pressure(>120/90 mmHg)/hemodynami c reading . Edema Weak pulse pressure Decreased peripheral pulses Cold, clammy skin
4. Elevate head of bed and maintain head neck in midline or neutral position.
5. Measure urine output on a regular schedule of shift provides adequate fluid depending on
4. To provide circulation/ venous drainage
Group2
P r e e c l a m p s i a P a g e | 65
clients need. 6. Cautioned client to avoid activities that increase cardiac workload. And review ways of avoiding constipation and encourage quiet, restful atmosphere. 7. Provide for diet restriction (DASH diet) and increase frequent small feedings. 8. Provide bed rest 9. Observe skin color, temperature, capillary refill time.
5. To provide baseline data
6. Conserves energy and lowers tissue oxygen demands.
10. Provide calm and restful surroundings and minimize environmental activity/noise. Limit the number of visitors and length of stay.
7. To maintain
adequate nutrition and fluid balance. 8. To avoid further
Group2
P r e e c l a m p s i a P a g e | 66
11. Provide comfort measure, e.g. back and neck massage, elevation of head. 12. Instruct in relaxation technique, guided imagery.
increase of blood pressure. 9. Presence of pallor; cool,, and delayed capillary refill time maybe due to peripheral vasoconstriction or reflect cardiac decompensation 10. Help reduced sympathetic stimulation/ promote relaxation.
COLLABORATIVE:
1. Administer medication as indicated: Hydralazine
11. Decrease discomfort and may reduced sympathetic stimulation. 12. Can reduced stressful stimuli, produced calming effect, thereby
Group2
P r e e c l a m p s i a P a g e | 67
reducing BP.
1. A directacting vasodilator that relaxes arteriolar smooth muscle Reference: Nurses Pocket Guide Book, 9th edition by Doenges et.al p.142
Problem: Risk for Fetal Injury Nursing Diagnosis: Risk for (Fetal) Injury related to reduce placental perfusion secondary to vasoconstriction tertiary to Pregnancy Induced Hypertension.
Group2
P r e e c l a m p s i a P a g e | 68
Cause Analysis: With severe preeclampsia, the cardiac system can become overwhelmed because the heart is forced to pump against rising peripheral resistance. This reduces blood supply to organs, most markedly in the kidneys, pancreas, liver, brain, and PLACENTA. Poor placental perfusion may reduce the fetal nutrient and Oxygen supply. (Maternal and child nursing by PILLITTERI 5th edition pp.426) CUES Subjective: ST0: OBJECTIVES NURSING INTERVENTIONS Independent: RATIONALE Independent: EVALUATION The fetus is expected to manifest:
Not applicable
After 8 hrs of nursing interventions, the patients placental perfusion will increase AEB fetal heart rate within 120-160 bpm.
9. Monitor and assess vital signs. 10. Assess the patients general physical condition. 11. Instruct mother to assume a left lateral position. 12. Promote bed rest.
9. To obtain baseline 10. To determine presence of abnormality. 11. To avoid putting pressure on the inferior vena cava. 12. To increase uteroplacental circulation and prevent too much workload on the heart. 13. To provide comfort. normal fetal movement in an hour (3 movements/hour) normal HR (120-160 bpm) absence of signs of fetal distress
LTO:
After 3 days of nursing Objective: interventions, the patient will demonstrate a decrease in systemic vasoconstriction to increase uteroplacental circulation as evidence by
Patient manifested: A systemic
13. Encourage relaxation techniques such as deep Breathing.
Group2
P r e e c l a m p s i a P a g e | 69
vasoconstriction Patients fetus may manifest: Intrauterine growth retardation Changes in fetal activity/ heart rate(less than or more than 120160 bpm) Fetal demise
absence of signs of fetal distress
14. Encourage patient to avoid constipation by increasing fiber intake.
14. Straining defecation might put pressure on the uterus which could injured the already compromised fetal health. 15. To enhance patients participation in the treatment regimen. 16. For patient education. .
15. Instruct mother on the possible complications the disease can cause to the fetus. 16. Discuss importance of having an adequate blood circulation going to the placenta.
Dependent:
2. Administer oxygen as indicated. Reference: Nurses Pocket Guide Book, 9th edition by Doenges et.al pp.369
2. To help in respiration.
Group2
P r e e c l a m p s i a P a g e | 70
Problem: Risk for Injury Nursing Diagnosis: Risk for Injury related to excess fluid build-up in the tissue secondary to retinal edema. Cause Analysis: Spasm of the arteries in the retina leads to vision changes. Cerebral edema occurs, reports may be voiced of visual disturbances such as blurred vision or seeing spots before the eyes.( (Maternal and child nursing by PILLITTERI 5th edition pp.426) CUES Subjective: ST0: OBJECTIVES NURSING INTERVENTIONS Independent: 1. Ascertain type/degree of visual loss. RATIONALE Independent:
1. Affects choice of
EVALUATION The patient is expected to: Verbalize, enumerate factors that will increase potential for injury. Enumerate plans and strategy to maintain safety.
The patient may verbalize: blurring of vision severe headache
After 4 hours of nursing intervention the patient will be able to identify factors that increase potential for injury.
intervention and patients future expectations.
2. Reduces safety
2. Recommend measures to assist patient to manage visual limitations, e.g. arranging furniture
hazards related to changes in visual field and papillary accommodation to environmental light.
3. These measures will
Objective: Progressive loss of visual field.
LTO: After 1 day of nursing intervention the patient will apply safety measures to
3. Orient patient to
environment. Assess patient's ability to use call
A B G L N P P Q R
help patient cope with unfamiliar surroundings.
Y
Group2
P r e e c l a m p s i a P a g e | 71
prevent injury and family members will develop strategy to maintain safety.
bell, side rails and bed positioning controls. Keep bed at lowest level, and conduct close night watch
4. Teach pt and family
about need to safe illumination. Advise pt to wear sunglasses to reduce glare. advise using contrasting colors in household furnishings
5. Observe for factors that
4. These measure will
enhance visual discrimination
5. Increase awareness
may cause or contribute to injury.
of patient, family members, and care givers. 6. To reduce edema. Since if possible medication should not be prescribed since the patient is pregnant.
6. Encourage bedrest.
Collaborative: 1. Administer medication as
Group2 A B G L N P P Q R Y
P r e e c l a m p s i a P a g e | 72
prescribed. Reference: Nurses Pocket Guide Book, 9 edition by Doenges et.al pp.3
th
Problem identified; lack of knowledge Nursing diagnosis: Knowledge deficit [Learning Need] regarding condition,prognosis, self care and treatment needs related to lack of exposure/unfamiliarity with information resources, misinterpretation. Cause analysis: Anticipatory anxiety and patient lacks in psychological and educational information. (Medical surgical Nursing by Smeltzer and Bare 7th ed. pg. 1303)
Cues
Objectives STO:
Nursing interventions Independent: 1. Assess clients/couples knowledge of the disease process. Provide information about pathophysiology of Preeclampsia, implications for mother and fetus; and the rationale for interventions, procedures, and tests, as needed.
Rationale The patient is expected to: 1. Establishes data base and provides information about areas in which learning is needed. Receiving information can promote understanding and reduce fear, helping to facilitate the treatment plan for the client. provide additional treatment options, such as using lowdose (60 mg/day) aspirin to
Q R Y
Questions/request for information misinterpretation Verbalization of problem Statement of misconception Inaccurate followthrough of instructions, development of preventable complications
After 2-3 days of nursing interventions and health teachings, the patient will be able to verbalize accurate information about diagnosis, prognosis, and potential complications at own level of readiness.
LTO:
3. Verbalize accurate information about diagnosis, prognosis, and potential complications at own level of readiness. 4. Verbalize understanding of the therapeutic needs and will be able to identify/use available resources appropriately.
Group2
P r e e c l a m p s i a P a g e | 73
After 4-5 days of nursing interventions and health teachings, the patient will be able to verbalize understanding of the therapeutic needs and will be able to identify/use available resources appropriately.
reduce thromboxane generation by platelets, limiting Note: Current research in progress may severity/incidence of PIH (pre-eclampsia)
2.Provide information about signs/symptoms indicating worsening of condition, and instruct client when to notify healthcare provider.
3.Keep client informed of health status, results of tests, and fetal well-being.
2. Helps ensure that client seeks timely treatment and may prevent worsening of preeclamptic state or additional complications.
4.Instruct client in how to monitor her own weight at home, and to notify healthcare provider if gain is in excess of 2 lb/wk, or 0.5 lb/day.
Fears and anxieties can be compounded when client/couple does not have adequate information about the state of the disease process or its impact on client and fetus.
Group2
P r e e c l a m p s i a P a g e | 74
5.Assist family members in learning the procedure for home monitoring of BP, as indicated.
4. Gain of 3.3 lbs or greater per month in second trimester or 1 lb or greater per week in third trimester is suggestive of PIH. 5. Encourages participation in treatment regimen, allows prompt intervention as needed, and may provide reassurance that efforts are beneficial. 6. Reinforces importance of clients responsibility in treatment. 7. Protein is necessary for intravascular and extravascular fluid regulation. 8. A test result of 2+ or greater is significant and needs to be reported to healthcare provider. Urine specimen contaminated by vaginal discharge or RBCs
6.Review techniques for stress management and diet restriction.
7.Provide information about ensuring adequate protein in diet for client with possible or mild preeclampsia.
8.Review self-testing of urine for protein. Reinforce
Group2
P r e e c l a m p s i a P a g e | 75
rationale for and implications of testing.
may produce positive test result for protein.
Reference: Nurses Pocket Guide Book, 9th edition by Doenges et.al.
H
Objectives:
E A L T H
D U C A T I O N
L A N
After 30 minutes of rendering health teaching, the patient will be able to:
Group2
P r e e c l a m p s i a P a g e | 76
1. Understand the importance of proper nutrition and exercise to promote health and prevention of disease. 2. Understand the importance of adequate rest and avoidance of stress for fast recovery. 3. Verbalize feelings of understanding towards the health teaching.
Materials needed: 1. Visual aids 2. Pentel pen 3. Coloring materials General Support bed rest Specific health teaching - Teach patient with severe preeclampsia, pregnant woman is advice to be hospitalized so that bed rest can be enforced and she can be observed more closely. - Encouraged the family that Visitors are restricted to support people ( e.g husband, father of the child, mother, or older children). - Teach the patient to avoid a loud noise such as a crying baby or dropped tray of equipment may be sufficient to trigger a seizure initiating eclampsia. - Instruct the patient to darken the room if possible because a bright light can trigger seizures. Encouraged patient to promote bed rest. Because when the body is in the recumbent position sodium tends to excreted at a faster rate than during activity. Bed rest, therefore, is the best method of aiding increased evacuation of sodium and encouraging dieresis. Rest should always be in lateral recumbent position to avoid uterine pressure in the vena cava. Group2 A B G L N
Promote Bed Rest
Nutrition
Instruct the mother needs to continue her usual pregnancy diet.
P P Q R Y
P r e e c l a m p s i a P a g e | 77
Eat nutritious and balanced diet (60 70 mg/day; 1200 mg calcium and adequate zinc, magnesium and vitamins). Teach the patient that there is no sodium restriction, however, consider limiting excessive salty foods(processed foods, potato chips, etc.) and add roughage ( bran, fruits, leafy vegetables) to your diet to decrease constipation. Encouraged pt. to eat rich in protein diet such as lean meat, green leafy vegetables, beans, and other rish in protein food. Encouraged to limit fluid intake up to 6 - 8 glasses/ day Teach the client on Circling of hands and feet or gently tensing and relaxing and leg muscles. This improves muscle tone, circulation, and sense of well - being. Encouraged deep breathing exercise Instruct the patient to limit the no. of stairs she climbs to one flight/day for the first week at home. Beginning the second week, if her lochial discharge is normal, she may start to increase this activity. Limit stair climbing to only when necessary for first two weeks. Encourage family participate in the care management. Have significant others to assist you in the care of the house, children and etc. Instruct the mother to relax to help cope with stress. Use guided imagery, pleasant scenes, and smoothing music. Avoid alcohol, limit caffeine intake, and avoid smoking and passive smoke exposure.
Fluid intake Exercise -
Support system
Relaxation Lifestyle
Group2
P r e e c l a m p s i a P a g e | 78
Supplementation
Supplementation of calcium, fish oil, and vitamins C and E
I S C H A R G E
L A N
Group2
P r e e c l a m p s i a P a g e | 79
Medication Medication Hydralazine (Apresoline) Dosage/ frequency 50 to 200 mg/day Nursing responsibilities Inform the patient for the possible side effects of the drugs such as headache, dizziness, palpitations, constipation, vomiting, and anxiety. Take this drug exactly as prescribed and take this dug with food. Instruct pt. to take dose at the same time everyday, alst dose of the day must be taken during bedtime. Do not double dose. Encourage client to comply with additional hypertensive intervention (weight reduction, exercise, low sodium diet, stress management) Instruct family and pt. on proper monitoring of blood pressure. Inform pt. that urine may turn dark. Advise pt. that frequent oral hygiene can minimize dry mouth. Instruct pt. to notify physician if unusualities occur.
Methyldopa (Aldomet)
250 mg PO bid/tid; increase q2d prn; not to exceed 3 g/d
25-100 mg PO qd; not to exceed 200 mg/kg/d Hydrochlorothiazide
Group2 A B G L N P P Q R Y
Instruct pt. to take medication at the same time everyday. Do not double dose. Instruct pt. to monitor weight biweekly
P r e e c l a m p s i a P a g e | 80
( Esidrix)
and notify healthcare professional of significant changes. Advise pt. to make position changes slowly, to avoid orthostatic hypotension. Encourage client to comply with additional hypertensive intervention (weight reduction, exercise, low sodium diet, stress management) Instruct pt. and family in correct technique for monitoring weekly blood pressure.
Exercise Daily brisk walk for 30-60minutes Kegels exercise 10 times a day for 6 weeks How to perform kegels exercise: 1. Identify the correct pelvic floor muscles by contracting them to stop the flow of urine while sitting on the toilet. 2. Repeat this action several times to become familiar with it. 3. Start the exercise by emptying the bladder. 4. Tighten the pelvic muscles and hold for a count of ten seconds. 5. Relax the muscles completely a count of 10 seconds 6. Perform ten exercises at least three times daily and progressively increase.
Group2
P r e e c l a m p s i a P a g e | 81
7. Perform the exercise in different position such as standing. Lying, and sitting. 8. Keep breathing during exercises. 9. Dont contract the abdominal, thigh leg or buttocks muscles during these exercises. 10. Relax while doing kegels exercises and concentrate on isolating the right muscles. 11. Attempt to tighten the pelvic muscles before sneezing, jumping, or laughing to protect them for additional laxness. 12. Be aware that you can perform kegel exercise anywhere and in any place without anyone noticing. Therapy Drug Therapy- It is recommended esp. drugs that aids in lowering the blood pressure of the certain person and to maintain blood pressure with normal ranges such as beta blockers. Example of this is Propranolol, Metoprolol, Nadolol, etc. Health teachings: Instruct patient to lose weight if overweight such as engaging in any activities. Restricts the intake of alcohol for this may cause vasoconstriction thus increasing blood pressure. Have an appropriate exercise regimen because regular activity is a significant factor in weight reduction. Maintain adequate intake of dietary potassium. Maintain adequate intake of dietary calcium and magnesium for general health. Stop smoking and reduce intake of dietary saturated fats and cholesterol for overall cardiovascular health. Stress reduction also is beneficial in any diseases. Encourage client to observe proper perineal hygiene.
Teach the client to report warning signs of problems and where to seek help to eliminate them. Instruct the woman for self care and infant care.
Group2
P r e e c l a m p s i a P a g e | 82
OPD: 1. 2. Diet: Encourage to eat nutritious, balanced diet (60 70 grams protein; 1200 mg calcium and adequate zinc, magnesium, and vitamins). Consult with registered dietician on the diet best suited for you as an individual. There is no sodium restriction; however consider limiting excessively salty foods (luncheon meats, pretzel, potato chips, and pickles). Eat foods with roughage (whole grains, raw fruits, and vegetables). Avoid alcohol, and limit caffeine intake. Adequate fluid intake (6 8 glasses per day help to maintain optimal fluid volume and aids in renal perfusion). Avoid high fat diet. Spiritual: Encouraged to continue to seek Gods guidance and enlightenment. Emphasized the importance of prayers in healing Encouraged to ask for divine assistance in everything Encouraged to continue to pray to God.
Encouraged to continue to have a positive outlook in life.
Have the client follow a check up schedule to visit physician in order to assess extent of treatment and further assessment. Obtain drugs that may be administered at home for further treatment.
Encouraged to keep faith in God and not to give up easily when hard times come
Group2 A B G L N P P Q R Y
P r e e c l a m p s i a P a g e | 83
E D I C A L
A N A G E M E N T
Drugs Magnesium Sulfate (Epson Salt) Pregnancy risk category B
Classification Anticonvulsant
Indication -muscle relaxant -prevents seizures
Mechanism of Action Mg depresses the CNS and control convulsion by blocking the release of acetylcholine and decrease the excitability of the motor membrane.
Dosage -Loading dose 4-6 IV -Maintenance dose 1-2 g/h IV
Adverse Effects CNS: depression CV: flushing, hypotension, depression, of myocardium Magnesium intoxication: Cardiac and CNS depression, preceding
Nursing Considerations Before administering IV, check for the ff : -Absent patellar reflex - RR below 16/min - Urine output below 100 ml in
Group2
P r e e c l a m p s i a P a g e | 84
respiratory past 4 hours paralysis, circulatory collapse, - Early signs of hypermagnesemia; flaccid paralysis. flushing, sweating, hypotension or hypothermia - Past history of heart block or myocardial damage, prolonged RR and widened QRS interval.
Hydralazine HCL (Apresoline) Pregnancy risk category C
Antihypertensive
- preeclampsia, eclampsia - heart failure
A direct- acting vasodilator that relaxes arteriolar smooth muscle.
- Initially, 5-10 mg IV, followed by 5-10 mg IV doses, (range 5-20 mg) q 20 to 30 min, prn or 0.5 to 10 mg/ hour IV infusion.
CNS: headache, dizziness CV: tachycardia, angina pectoris, palpitations EENT: nasal congestion GI: nausea, vomiting, diarrhea, anorexia,
- Monitor pt. blood pressure, pulse rate, and body weight frequently. - Instruct client to take with food to increase absorption.
Group2
P r e e c l a m p s i a P a g e | 85
constipation.
Calcium Gluconate Pregnancy risk category C
Electrolyte and replacement solutions
Antidote for magnesium toxicity
Generally, replaces calcium and maintains calcium level; physiologically antagonize hypomagnesaemi a effect.
- 1g/ IV (10ml of a 10% solution)
CV: mild drop of blood pressure, vasodilation, bradycardia, arrhythmias, cardiac arrest GI: irritation, constipation, chalky taste, nausea, thirst, abdominal pain GU: renal calculi
- Warn pt. to avoid oxalic acid (in rhubarb and spinach), phytic acid (in barn and whole grain cereals), and phosphorus (in dairy products) in the meal preceding calcium consumption; these substances may interfere calcium absorption. - Warn pt. to avoid activities that require alertness and good coordination. - Warn pt. not to abruptly stop drug cause withdraw
Diazepam (Valium) Pregnancy risk category D
Anxiolytic
Adjunct treatment for seizure disorder.
A benzodiazepine that probably potentiates the effects of GABA, depresses the CNS, and suppresses the spread of seizure activity.
A B G L N P
- Adults: 2 to 10 CNS: drowsiness, mg PO bid to fatigue, ataxia, qid. headache, insomnia, minor changes in ECG patterns. CV: hypotension, CV collapse,
Group2
P r e e c l a m p s i a P a g e | 86
bradycardia EENT: blurred vision GI: nausea, constipation GU: incontinence, urine. Hydrochlorothiazide Diuretic ( Esidrix) Antihypertensive (loop) Management of mild to moderat e hyperte nsion. Increases excretion of sodium and water by inhibiting sodium reabsorption in the distal tubule. May produce arteriolar dilation. Dosage: 25-100 mg PO qd; not to exceed 200 mg/kg/d Pediatric <6 months: 2-3 mg/kg/d PO divided bid >6 months: 2 mg/kg/d PO divided bid Dizziness, drowsiness, hypotension, nausea, vomiting, hypokalemia, hypercalcemia, hypovolemia, muscle cramps, rashes.
symptoms may occur.
Monitor blood pressure during dosage adjustment and periodically during therapy. Instruct pt. to take medication at the same time everyday. Do not double dose. Instruct pt. to monitor weight biweekly and notify healthcare professional of significant changes. Advise pt. to make position
Group2
P r e e c l a m p s i a P a g e | 87
changes slowly, to avoid orthostatic hypotension. Caution pt, to wear protective clothing and use sunscreen to prevent photosensitivity reactions. Advise pt. to report muscle weakness, cramps, nausea, vomiting, diarrhea, or dizziness to health care professional. Emphasize on routine follow up exams. Encourage client to comply with additional hypertensive intervention (weight reduction, exercise, low sodium diet,
Group2
P r e e c l a m p s i a P a g e | 88
stress management) Instruct pt. and family in correct technique for monitoring weekly blood pressure. May cause drowsiness; instruct pt. not to do activity requiring alertness.
S
CESAREAN SECTION
U R G I C A L
A N A G E M E N T
Clients with mild preeclampsia can be managed at home with frequents follow-up care. If the preeclampsia is severe, a woman may be admitted to the health care facility. If the pregnancy is 36 weeks or further long or fetal lung maturity can be confirmed by amniocentesis, labor can be induced to end the pregnancy at this point. If the pregnancy is less than 36 weeks or amniocentesis reveals immature lung function, interventions will be instituted to attempt to alleviate the severe symptoms and allow the fetus to come to term. However, if fetus appears to be in imminent danger, cesarean birth is indicated. Definition: It is the delivery of the fetus through incisions in the abdominal wall and the uterus. Indications:
Group2
P r e e c l a m p s i a P a g e | 89
The decision to have C-section delivery can depend on the obstetrician, delivery location, and the womans past deliveries or medical history. Some of the main reasons for C-section instead of vaginal delivery include the following: Cephalopelvic Disproportion (CPD)- occurs when the babys head will not fit through the pelvis. This diagnosis may also be used to indicate the labor that fails to progress. Fetal distress- the baby is not receiving enough oxygen. It may be indacated by an abnormal fetal tracing or a drop of a fetal heart rate when your heathcare provider listens to the rate during or after a contraction. Abnomal Position of the Baby- Instead of the babys head presenting first in the pelvis with his/her chin tucked inward , the presenting part of the baby head extended outward, the shoulder, bottom or leg. Prolapsed Cord- When the umbilical cord in the vagina head of the baby. This most commonly occurs the membranes rupture and the baby is in breech position is not well engaged in the pelvis. This is an emergency and an immediate cs is necessary to prevent the presenting part from compressing the cord and cutting off the oxygen supply to the baby. Abruptio Placentae- The placenta partially separates from the uterine wall before the baby is born. This is an emergency cs birth is necssary yo prevent the mother from hemrrhaging, which can cause the baby to lose all or part. Placenta Previa- A condition in which yhe placenta partilly covers the cervix. The degree of severity determines whether cs birth is indicated. If the cervix is completely coverd, a cesarean is mandatory since the placenta would deliver first in avaginal delivery and the baby would lose his/her oxygen supply. Procedure: Regional anesthesia is most frequently administered to the patient, who is awake. A low transverse or vertical incision consistent with estimated size of the fetus is made. The rectus muscles are separated and the peritoneum incised. Hemostasis is assured. The bladder is reflected from the lower uterine segment, and the uterus is incised. The amniotic sac is entered, and the fluid must be aspirated immediately. Some surgeons prefer to use the suction tubing without a tip to avoid injury. The fetal head is delivered using manual pressure and counter pressure on the fundus. Retactors are removed. As soon as the head is delivered the newborns nares are aspirated by bulb syringe
Group2
P r e e c l a m p s i a P a g e | 90
immediately but very gently; the delivery is completed. The umbilical cord is clamp and cut. The infant is received in a sheet and trasferred to a gowned and gloved member of neonatal team. Standard precauions are observed. Resuscitative measures are provided to the neonate under warming lamps. The pediatrician determines the infants Apgar score. Vernix caseosa and blood are wiped from the infants. Ointment (Erythromycin 0.5%) is applied to the conjuctival sacs of the newborn. The placenta is delivered. The uterus is massaged to encouraged it to contract. Tubal Ligation may be performed. Blood and amniotic fluid are aspirated. Hemostasis is assured. The edges of the uetrine incision are clamped tio aid in its closure; the uterus and bladder are closed in a single or double layer.The peritoneum at the lower uterine segment is sutured to its anatomic position. The wound is closed in layers. An abdominal dressing and perineal pad are applied. Warmed blanket is placed over the mother. The mother and infant, in good condition, are given a moment to bond on the gurney. The infant is rushed to the neonatal unit to be throughly clean and assessed.
Nursing Responsibilities: Preoperative care: Assess the client knowledge of the procedure. The client is NPO after midnight. Relieving the patients and the familys anxiety about the outcome with reasonable information Encourage patient to commence deep breathing, coughing and leg exercises. Teach the client post operative expectations
Group2
P r e e c l a m p s i a P a g e | 91
Post operative care: Monitor vital sign every 15 minutes until the client is stable. Assess the need for pain relief. Assess the client for vaginal bleeding
R O G N O S I S
Usually the high blood pressure, protein in the urine, and other effects of preeclampsia go away completely within 6 weeks after delivery. However, sometimes the high blood pressure will get worse in the first several days after delivery. A woman with a history of preeclampsia is at risk for the condition again during future pregnancies. Often, it is not as severe in later pregnancies. Women who have high blood pressure problems during more than one pregnancy have an increased risk for high blood pressure when they get older. The fetal prognosis in eclampsia is poor because of hypoxia and consequent fetal acidosis. If premature separation of the placenta from vasospasm occurs, the fetal prognosis is even graver. If fetus must be delivered before term, all the risks of immaturity will be faced.
Group2
P r e e c l a m p s i a P a g e | 92
In preeclampsia, the fetal mortality rate is approximately 10%. If eclampsia develops, the mortality rate increases to as high as 25% (Moldenhauer & Sibai, 2003).
B
Books
I B L I O G R A P H Y
Doenges, Marilynn E. and et. al. Nurses Pocket Guide 11th Ed. Philadelphia: F.A. Davis Company, 2006. Doenges, Marilynn E. and et. al. Nursing Care Plans Guidelines for Individualizing Client Care Across the Life Span. Philadelphia: F.A. Davis Company, 2006. Nursing 2009 Student Drug Handbook 10th Ed. Philadelphia: Lippincott Williams and Wilkins, 2009. Nurses Quick Check: Diagnostic Tests. Philadelphia: Lippincott Williams and Wilkins, 2006. Pacardo, Roselyn S. Compiled Notes on Maternal Nursing with Critical Thinking Exercises, 2010.
Group2
P r e e c l a m p s i a P a g e | 93
Pillitteri, Adele. Maternal and Child Health Nursing: Care of the Childbearing & Childbearing Family 5 th Ed., Vol 1., Philadelphia: Lippincott Williams and Wilkins, 2009. Porth, Carol Mattson. Pathophysiology Concepts of Altered Health Status 7th Ed. Philadelphia: Lippincott Williams and Wilkins, 2005. Scanlon, Valerie C. and Tina Sanders. Essentials of Anatomy and Physiology, 5th Ed. Philadelphia: FA Davis Company, 2007. Internet http://emedicine.medscape.com/article/1476919-overview http://familydoctor.org/online/famdocen/home/women/pregnancy/complications/064.html http://www.nlm.nih.gov/medlineplus/ency/article/000898.htm http://www.preeclampsia.org/research http://hubpages.com/hub/PREGNANCY-AND-PRE-ECLAMPSIA-RISK-FACTORS http://www.mayoclinic.com/health/preeclampsia/DS00583/DSECTION=risk-factors
Group2
You might also like
- Draft Concept Note On Goat RearingDocument7 pagesDraft Concept Note On Goat Rearinganoop_100% (1)
- Book of Horn and IvoryDocument96 pagesBook of Horn and IvoryBen A.No ratings yet
- Grade 7 TG SCIENCE 2nd QuarterDocument60 pagesGrade 7 TG SCIENCE 2nd QuarterAilyn Soria Ecot100% (2)
- Elicityl - OligoTech - Human Milk Oligosaccharides HMOs - 2011v2Document4 pagesElicityl - OligoTech - Human Milk Oligosaccharides HMOs - 2011v2pascalsalvaNo ratings yet
- Wings of Arian - Devri WallsDocument528 pagesWings of Arian - Devri WallsJoseph Dela Cruz100% (4)
- DX Roleplaying HandbookDocument520 pagesDX Roleplaying HandbookJeffrey Lee89% (9)
- 1 - Presentation - Management of Preclamplsia, Mild and ModerateDocument22 pages1 - Presentation - Management of Preclamplsia, Mild and ModeratesharonNo ratings yet
- Hypertension in Pregnancy CompiledDocument67 pagesHypertension in Pregnancy CompiledRaiza Love Caparas-PablicoNo ratings yet
- OligohydramniosDocument4 pagesOligohydramniossalamredNo ratings yet
- Preeclampsia and EclampsiaDocument23 pagesPreeclampsia and Eclampsiaapi-3705046100% (6)
- Placenta PreviaDocument11 pagesPlacenta PreviaHomerNo ratings yet
- Ectopic Pregnancy - OMDocument9 pagesEctopic Pregnancy - OMrheindNo ratings yet
- 05 DystociaDocument10 pages05 DystociaRiantiara PutrizaNo ratings yet
- Case Report Non-infection Unit Β-Major ThalassemiaDocument27 pagesCase Report Non-infection Unit Β-Major ThalassemiaimamkdNo ratings yet
- PREECLAMPSIADocument60 pagesPREECLAMPSIAMary Grace MasNo ratings yet
- The Neonate at 24 To 48 Hours Following Early DischargeDocument8 pagesThe Neonate at 24 To 48 Hours Following Early Dischargenursereview100% (2)
- Final Case Study-Bili (ReVISED)Document35 pagesFinal Case Study-Bili (ReVISED)malentot100% (1)
- Obg Icd-10 Pregnancy, Childbirth, PuerperiumDocument11 pagesObg Icd-10 Pregnancy, Childbirth, PuerperiumarifianjuariNo ratings yet
- Malpresentation and Malposition - PostmaturityDocument29 pagesMalpresentation and Malposition - PostmaturityNishaThakuriNo ratings yet
- Hyperemesis GravidarumDocument16 pagesHyperemesis GravidarumBabi PanggangNo ratings yet
- Ectopic PregnancyDocument26 pagesEctopic PregnancyDavid SitinjakNo ratings yet
- Neonatal Sepsis: CausesDocument3 pagesNeonatal Sepsis: CausesGeraldine BirowaNo ratings yet
- Preterm Prelabour Rupture of MembranesDocument12 pagesPreterm Prelabour Rupture of MembranesSeptiany Indahsari DjanNo ratings yet
- Nursing Care Plan General Objective: To Promote Safety Through Prevention of The Spread of InfectionDocument3 pagesNursing Care Plan General Objective: To Promote Safety Through Prevention of The Spread of InfectionitsmeayaNo ratings yet
- Anemia in PregnancyDocument14 pagesAnemia in PregnancyWern Ching Lee50% (2)
- ALTERED POST PARTUM Complications Nursing Lecture and Care PlanDocument13 pagesALTERED POST PARTUM Complications Nursing Lecture and Care PlanKristelle Joy Capili SicatNo ratings yet
- MiscarriageDocument42 pagesMiscarriageAnonymous pJfAvl100% (3)
- Adolescent PregnancyDocument5 pagesAdolescent PregnancyTima SongsNo ratings yet
- EclampsiaDocument47 pagesEclampsiarranindyaprabasaryNo ratings yet
- PROM SANJIDA FInal 2Document32 pagesPROM SANJIDA FInal 2Saiful islam RonyNo ratings yet
- Φ PathophysiologyDocument4 pagesΦ PathophysiologyMariah AshooriyanNo ratings yet
- Intrauterine Growth Restriction IUGR: TH THDocument2 pagesIntrauterine Growth Restriction IUGR: TH THZahra AlaradiNo ratings yet
- Pre EclampsiaDocument8 pagesPre EclampsiaJamie Agbannawag100% (1)
- Complications During Labor and Delivery - HardDocument19 pagesComplications During Labor and Delivery - Hardkrizele ann santosNo ratings yet
- 16 Amniotic Fluid EmbolismDocument46 pages16 Amniotic Fluid EmbolismAhmed TarigNo ratings yet
- DR - Group CaseDocument62 pagesDR - Group CaseRon Lucernas MayugaNo ratings yet
- Post Partum HemorrhageDocument12 pagesPost Partum HemorrhageCristinaCaprosNo ratings yet
- Pyloric StenosisDocument5 pagesPyloric Stenosisensoooooooooo100% (1)
- 68 Abnormal PeuperiumDocument44 pages68 Abnormal PeuperiumGodsonYeboah-AwudziNo ratings yet
- PIHDocument18 pagesPIHArtyom GranovskiyNo ratings yet
- Idiophatic Thrombocytopenic Purpura (ITP) in PregnancyDocument27 pagesIdiophatic Thrombocytopenic Purpura (ITP) in PregnancyAdietya Bima PrakasaNo ratings yet
- Nursing Care Plan: Obstetrics and Gynecology Nursing RotationDocument8 pagesNursing Care Plan: Obstetrics and Gynecology Nursing RotationMary Justine Nuyad-AfricaNo ratings yet
- Case Presentation O&GDocument76 pagesCase Presentation O&GMalvinder Singh DhillonNo ratings yet
- Abortion BSN 0PR-2: Case Study of BelleDocument27 pagesAbortion BSN 0PR-2: Case Study of BellekervinNo ratings yet
- Obstetric Nursing Care PlanDocument30 pagesObstetric Nursing Care PlanReshma KambleNo ratings yet
- Birth Asphyxia: by Anne E. Odaro MCM/2017/69852Document26 pagesBirth Asphyxia: by Anne E. Odaro MCM/2017/69852ElvisNo ratings yet
- Content On Pre-EclampsiaDocument13 pagesContent On Pre-EclampsiaJay PaulNo ratings yet
- Preeclampsia Eclampsia and Hellp SyndromeDocument24 pagesPreeclampsia Eclampsia and Hellp Syndromeapi-403416350100% (1)
- Eclampsia PresentationDocument6 pagesEclampsia Presentationshakuntla DeviNo ratings yet
- Preeclampsia PowerpointDocument14 pagesPreeclampsia Powerpointapi-253602771100% (1)
- Placenta PreviaDocument33 pagesPlacenta PreviaAcohCChao100% (1)
- Heavy Menstrual BleedingDocument29 pagesHeavy Menstrual BleedingsanjupainNo ratings yet
- RH IncompatibilityDocument9 pagesRH IncompatibilityJohn BardeenNo ratings yet
- Gestational Diabetes Mellitus - NISALDocument7 pagesGestational Diabetes Mellitus - NISALKevin de SilvaNo ratings yet
- Gestational DMDocument50 pagesGestational DMKevin MarquezNo ratings yet
- Pregnancy Induced Hypertension (PIH) : Case Scenario 4Document4 pagesPregnancy Induced Hypertension (PIH) : Case Scenario 4Mae Arra Lecobu-anNo ratings yet
- A Case Report On Multifetal PregnancyDocument5 pagesA Case Report On Multifetal PregnancyThreecee VelezNo ratings yet
- PreeclampsiaDocument34 pagesPreeclampsiaTrigo Puro100% (1)
- Ectopic PregnancyDocument65 pagesEctopic PregnancyWen SilverNo ratings yet
- Placental Abruption PresentationDocument30 pagesPlacental Abruption PresentationNafisat AdepojuNo ratings yet
- Antiphospholipid Antibody Syndrome and PregnancyDocument17 pagesAntiphospholipid Antibody Syndrome and Pregnancybidan22No ratings yet
- Neonatal JaundiceDocument37 pagesNeonatal JaundiceAbraham ChiuNo ratings yet
- Prenatal Case ScenarioDocument4 pagesPrenatal Case ScenarioCharles Malcolm DalugdugNo ratings yet
- Case Study - Incomplete Abortion Related To APSDocument8 pagesCase Study - Incomplete Abortion Related To APSRomeo ReyesNo ratings yet
- Preeclampsia (Toxemia of Pregnancy) : Background: Preeclampsia Is A Disorder Associated With PregnancyDocument12 pagesPreeclampsia (Toxemia of Pregnancy) : Background: Preeclampsia Is A Disorder Associated With PregnancyRita AryantiNo ratings yet
- Krampus Hat Free Pattern - Morale FiberDocument1 pageKrampus Hat Free Pattern - Morale FiberAriadna SanchezNo ratings yet
- Si 68-71 Tatlife Layout 1Document2 pagesSi 68-71 Tatlife Layout 1api-292331390No ratings yet
- Insert Paper English Cambridge Checkpoint 2018Document4 pagesInsert Paper English Cambridge Checkpoint 2018brampok86% (7)
- Epicure - November 2015 PDFDocument140 pagesEpicure - November 2015 PDFGeorge Petrakos100% (1)
- Manual On Meat Cold Store Operation and ManagementDocument93 pagesManual On Meat Cold Store Operation and ManagementTùng ĐoànNo ratings yet
- Highlights November 2015Document44 pagesHighlights November 2015Milena100% (2)
- Ig Nobel ListDocument33 pagesIg Nobel ListAnonymous iFgGvfosNo ratings yet
- 8.sadvritta (Code of Conduct)Document47 pages8.sadvritta (Code of Conduct)Vanisha AnoepNo ratings yet
- Canine Genetic Testing Report: MumbaiDocument1 pageCanine Genetic Testing Report: MumbaitonyNo ratings yet
- Lot F Chapter 4 QuestionsDocument3 pagesLot F Chapter 4 QuestionsKanta EngNo ratings yet
- Unit 2 The Physiology of FitnessDocument11 pagesUnit 2 The Physiology of FitnessIas UpscNo ratings yet
- English GrammarDocument29 pagesEnglish GrammarJohn CarloNo ratings yet
- Two - Four - Six - Eight - One - Eight: I. Choose The Correct Answer by Crossing (X) A, B or C!Document5 pagesTwo - Four - Six - Eight - One - Eight: I. Choose The Correct Answer by Crossing (X) A, B or C!Madi AlhajjNo ratings yet
- Micromanipulation of Human Gamates and EmbryoDocument11 pagesMicromanipulation of Human Gamates and EmbryosumanavijitNo ratings yet
- Abdomen - Pelvis: Lecturer: Prof. Dr. Wahyuni Lukita Atmodjo, PH.DDocument33 pagesAbdomen - Pelvis: Lecturer: Prof. Dr. Wahyuni Lukita Atmodjo, PH.DAgatha FeliciaNo ratings yet
- Best Books Years 7Document7 pagesBest Books Years 7MagelicanNo ratings yet
- Describing How Muscles Work Activity SheetDocument3 pagesDescribing How Muscles Work Activity SheetTasnim MbarkiNo ratings yet
- Ajara-Rasayana KSRPrasadDocument56 pagesAjara-Rasayana KSRPrasadksr prasad100% (1)
- PATH - Acute Kidney InjuryDocument12 pagesPATH - Acute Kidney InjuryAyyaz HussainNo ratings yet
- 030722the Physiology of MicturitionDocument3 pages030722the Physiology of MicturitionAnnizah Paramitha100% (1)
- Life Cycle of A FrogDocument27 pagesLife Cycle of A FrogEn CyNo ratings yet
- Fairyland 1 LectiiDocument7 pagesFairyland 1 LectiiLavinia SurmeiNo ratings yet
- Annotated Reading LogDocument13 pagesAnnotated Reading LoggaureliNo ratings yet
- Mam Level 2 FlashcardsDocument38 pagesMam Level 2 FlashcardsAhmedSameh100% (1)