Professional Documents
Culture Documents
Req ER
Uploaded by
mayxzineOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Req ER
Uploaded by
mayxzineCopyright:
Available Formats
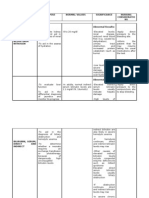
1. Acute Biologic Crisis: prevention. TYPES OF ASSESSMENT SHOCK FINDINGS 1.
Cardio Patient in genic cardiogenic Shock shock may experience angina pain and develop dysrhythmias and hemodynamic instability.
Different types of Shock, assessment findings, medical and nursing management, prognosis and MEDICAL MANAGEMENT The goals of medical management are to (1) limit further myocardial damage and preserve the healthy myocardium and (2) improve the cardiac function by increasing cardiac contractility, decreasing ventricular afterload, or both. Correction of underlying Causes Coronary cardiogenic: Thrombolytic therapy, angioplasty, or coronary artery bypass graft surgery. Noncoronary cardiogenic shock: cardiac valve replacement or correction of a dysrhythmia Initiation of First-Line Treatment Supplying supplemental oxygen Controlling chest pain Providing selected fluid support Administering vasoactive medications Controlling heart rate with medication or by implementation of a transthoracic or intravenous pacemaker Implementing mechanical NURSING MANAGEMENT Preventing Cardiogenic Shock Identify patients at risk and promote adequate oxygenation of the heart muscle and decrease its workload. Conserve patients energy. Promptly relieve angina Administer supplemental oxygen If shock cannot be prevented, work with other members of the health care team to prevent shock from progressing and to restore adequate cardiac function and tissue perfusion. PROGNOSIS Poor, only 1/3 patient actually treated survive initial episode and many of the survival have continuing angina, ccf, and decreased exercise tolerance. Approximately with a surgically correctable lesion leave hospital PREVENTION The best in prevent cardiogenic shock is to preavent a heart attack from happen these lifestyle changes include: -control hig blood pressure Dont smoke Maintain healthy weight Exercise regularly
Monitoring Hemodynamic Status Monitor the patients hemodynamic and cardiac status. Maintain arterial lines and monitor electrocardiographic equipment. Anticipate medications, intravenous fluids, and equipment that might be used. Be ready to assist in implementing measures. Document and report promptly any changes in hemodynamic, cardiac, and pulmonary status.
cardiac support (intra-aortic balloon counterpulsation therapy, ventricular assist systems, or extracorporeal cardiopulmonary bypass Pharmacologic Therapy Dobutamine (Dobutrex) increases/improves cardiac output Nitroglycerin (Tridil) venous vasodilator thus reduces preload Dopamine (Intropin) low dose increases renal and mesenteric blood flow medium-dose improves contractility, and slightly increases heart rate high-dose vasoconstriction, increases cardiac workload (undesirable) Other Vasoactive Medications: norepinephrine (Levophed), epinephrine (Adrenalin), milrinone (Primacor), amrinone (Inocor), vasopressin (Pitressin), and phenylephrine (NeoSynephrine) Antiarrhythmic Medications stabilizes heart rate
Report immediately changes in cardiac rhythm, presence of adventitious breath sounds, and other abnormal physical assessment findings. Aministering Medications and Intravenous Fluids Document and record medications and treatments that are administered as well as the patients response to treatment. Know the desired effects as well as the side effects of medications. Maintaining Inta-Aortic Balloon Counterpulsation Check the neurovascular status of the lower extremities frequently. Enhancing Safety and Comfort Administer medication to relieve chest pain Prevent infection at the multiple arterial and venous line insertion sites Protect the skin Monitor respiratory function Position the patient properly to promote effective breathing without decreasing blood pressure and to increase the patients comfort while reducing anxiety.
2. Hypovo Thirst lemic Increased Shock heart rate Cool and clammy skin Decreased arterial blood pressure Decreased urine output Changes in mentation
Medical goals in treating hypovolemic shock are to (1) restore intravascular volume to reverse the sequence of events leading to inadequate tissue perfusion, (2) redistribute fluid volume, and (3) correct underlying cause of fluid loss as quickly as possible. Treatment of the Underlying Cause: Hemorrhage: apply pressure to the bleeding site or surgery to stop internal bleeding Diarrhea/Vomiting: administer medications to treat diarrhea and vomiting Dehydration: fluid replacement Fluid and Blood Replacement Insert at least two largegauge intravenous lines to establish access for fluid administration Fluids commonly used: Lactated Ringers and 0.9% sodium chloride solutions Colloids (eg, albumin, hetastarch, and dextran) Dextran is not indicated in hemorrhaging patient
Briefly explain each procedure being performed. Use comforting touch to provide reassurance to the patient and family. Primary Prevention: Hypovolemic Monitor closely patients who shock are at risk for fluid deficits and recognized early assist with fluid replacement and treated promptly is Ensure safe administration of associated with prescribed fluids and a good outcome. medication and document their However, administration and effects advanced Monitor for signs of stages of HS w/ complications and side effects a fluid loss of of treatment and report these more than 25% signs early in treatment of total body fluid are Administering Blood and considered Fluids Safely irreversible Administer blood transfusions shock and are safely usually Obtain blood specimens quickly associated w/ a to obtain a baseline complete poor outcome or blood count and to type and death. cross-match the blood in anticipation of blood transfusions Monitor closely for adverse effects Monitor the patient closely for cardiovascular overload and pulmonary edema Monitor hemodynamic pressure, vital signs, arterial blood gases, hemoglobin and hematocrit levels, and fluid and intake and output Monitor temperature to ensure
Hypovolemic shock can be prevented in some instances by closely monitoring patient who are at risk for fluid deficits and assisting with fluid replacement before intravascular volume is depleted.
because it interferes with platelet aggregation. Transfuse packed red blood cells Redistribution of Fluid Place the patient in a modified Trendelenburg position Elevate legs to promote venous return Pharmacologic Therapy Dehydration secondary to hyperglycemia: administer insulin Diabetes Insipidus: administer desmopressin (DDAVP) Diarrhea: antidiarrheal agents Vomiting: antiemetic medications 3. Anaphy lactic Shock Anaphylactic shock is primarily an allergic reaction. To identify anaphylactic shock, first look for symptoms of allergy: Itching Red, raised, blotchy skin (hives) Treatment of anaphylactic shock requires removing the causative agent (eg, discontinuing an antibiotic agent), administering medications that restore vascular tone, and providing emergency support of basic life functions. Epinephrine is given for its vasoconstrictive action Administer Diphenhydramine (Benadryl) to reverse the effects of histamine, thereby reducing capillary
that rapid fluid resuscitation does not precipitate hypothermia Observe for jugular veins for distention and monitor jugular venous pressure Monitor cardiac and respiratory status closely and report changes in blood pressure, pulse pressure, heart rate, rhythm, and lung sounds to physician Implementing Other Measures Administer oxygen to increase the amount of oxygen carried by available hemoglobin in the blood Explain about the need for oxygen mask to reduce fear and anxiety Direct efforts to the safety and comfort of the patient Assess all patients for allergies or previous reactions to antigens (eg, medications, blood products, foods, contrast agents, latex) and communicate the existence of these allergies or reactions to others. Assess the patients understanding of previous reactions and steps taken by the patient and family to prevent further exposure to antigens Advise the patient to wear or
Anaphylaxis is a severe disorder with a guarded prognosis. Symptoms usually resolve with prompt treatment. However, among individuals with severe anaphylactic shock, brain
Prevent anaphylaxis by avoiding the allergens that trigger your symptoms. People with a history of anaphylaxis should wear a medical identification to alert others in the event or another
Wheezin g
Anaphylactic shock happens when the victim shows signs of low blood pressure: Confusio n Weaknes s Pale color Unconsci ousness
permeability. Give nebulized medications such as albuterol (Proventil) to reverse histamine-induced bronchospasm Perform cardiopulmonary resuscitation if cardiac and respiratory arrest are imminent or have occurred Endotracheal intubation or tracheostomy may be necessary to establish an airway. Intravenous lines are inserted to provide access for administering fluids and medications.
Anaphylaxis or anaphylactic shock often have symptoms of shortness of breath: Unable to speak more than one or two words Sitting straight up or with hands on knees Gasping for breath Pursing lips to breathe
carry identification that names the specific allergen or antigen Observe for allergic reaction when administering new medication In the hospital and outpatient diagnostic testing sites, identify patients at risk for anaphylactic reactions to condtrast antigen (radiopaque, dye-like substances that may contain iodine) used of diagnostic tests. Know the clinical signs of anaphylaxis, take immediate action if signs and symptoms occur, and prepare to begin cardiopulmonary resuscitation if cardiorespiratory arrest occurs. Assists with intubation if needed Monitor hemodynamic status Ensure intravenous access for administration of medications Administer prescribed medication and fluids Document treatments and their effects.
damage or death may occur frequently, even with treatment.
reaction.
Using neck muscles to take breaths
4. Neurog enic Shock
Dry, warm skin Bradycardia
Position the patient properly If hypoglycemia is the cause, administer glucose Specific treatment depends on the cause of shock
Elevate and maintain the head
of bed at least 30 degrees to prevent shock when patient is receiving spinal or epidural anesthesia Carefully immobilize the patient to prevent further damage to the spinal cord Apply elastic compression stockings and elevate the foot of the bed to minimize pooling of blood in the legs. Check the patient daily for any redness, tenderness, warmth of calves, and positive Homans sign (calf pain on dorsiflexion of the foot). Administer heparin or lowmolecular-weight heparin (Lovenox) as prescribed, apply elastic compression stockings, and initiate pneumatic compression of the legs to prevent thrombus formation. Perform passive range of motion of the immobile extremities to promote circulation Monitor the patient closely for
neurogenic shock are readily treatable and respond well to medical therapy.
However, it can be a potentially devastating complication, leading to organ dysfunction and death if not promptly recognized and treated.
There is no way to prevent neurogenic shock from occurring other than to avoid any severe injuries that may cause damage to the nervous system. Falls, accidents, and other traumas can be difficult to prevent, however. Use safety precautions whenever possible.
signs of internal bleeding that could lead to hypovolemic shock. 5. Septic Shock First Phase (hyperdynamic, progressive): Increased heart rate (tachycardia) Hyperthermia, with warm, flushed skin and bounding pulses. Elevated respiratory rate Normal or decreased urinary output Nausea, vomiting, diarrhea, decreased bowel sounds Subtle changes in mental status, such as confusion or agitation Later Phase (hypodynamic, irreversible): Low cardiac output with vasoconstrictio Pharmacologic therapy If infecting organism is unknown, broad-spectrum antibiotic agents are started. Third-generation cephalosporin plus an aminoglycoside may be prescribed initially Antibiotic agent may be changed to one that is more specific to the infecting organism and less toxic to the patient when culture and sensitivity reports are available. Nutritional Therapy Nutritional supplementation should be initiated within the first 24 hours of the onset of shock. Enteral feedings are preferred to the parenteral route because of the increased risk of iatrogenic infection associated with intravenous catheters However, enteral feedings may not be possible if decreased perfusion to the gastrointestinal tract reduces peristalsis and impairs absorption. Keep in mind the risks of sepsis and the high mortality tae associated with septic shock All invasive procedures must be carried out with aseptic technique after careful hand hygiene. Monitor intravenous lines, arterial and venous puncture sites, surgical incisions, traumatic wounds, urinary catheters, and pressure ulcers for signs of infection in all patients. Identify patients that are at particular risk for sepsis and septic shock (ie, elderly and immunosuppressed patients or patients with extensive trauma or burns or diabetes) Obtain appropriate specimens for culture and sensitivity to identify the site and source of sepsis and the specific organisms involved. Administer acetaminophen or apply hypothermia blankets to reduce temperature Monitor the patient closely for shivering, which increases oxygen consumption. Administer prescribed intravenous fluids and medications, including Septic shock has poor prognosis when it is associated with organ dysfunction, persistent low blood pressure, and evidence of inadequate circulation to the tissue. Can be prevented by choosing immediate treatment for wounds, bacterial infections or burns. Prevention include: Prompt treatment of sepsis Prompt treatment of septicemia
n Decreased blood pressure Cool and pale skin Temperature may be normal or below normal Rapid heart and respiratory rates Oliguria
antibiotic agents and vasoactive medications to restore vascular volume. Monitor blood levels (antibiotic agent, BUN, creatinine, white blood count) and report increased levels to physician. Monitor hemodynamic status, fluid intake and output, and nutritional status. Weigh the patient daily. Monitor serum albumin level to determine the patients protein requirements.
FIGURE 27-2. ECG electrode placement. The standard left precordial leads are V14th intercostal space, right sternal border; V24th intercostal space, left sternal border; V3diagonally between V2 and V4; V45th intercostal space, left midclavicular line; V5same level as V4, anterior axillary line; V6 (not illustrated)same level as V4 and V5, midaxillary line. The right precordial leads, placed across the right side of the chest, are the mirror opposite of the left leads. RA, right arm; LA, left arm; RL, right leg; LL, left leg. Adapted from Molle, E. A., Kronenberger, J., West-Stack, C., & Durham, L. S. (2005). Lippincott Williams & Wilkins's pocket guide to medical assisting (2nd ed.). Philadelphia: Lippincott Williams & Wilkins.
You might also like
- Nursing Mnemonics: The Ultimate Tips and Notes For NursesFrom EverandNursing Mnemonics: The Ultimate Tips and Notes For NursesRating: 5 out of 5 stars5/5 (1)
- DAY 6 SHOCK StudentsDocument38 pagesDAY 6 SHOCK StudentsTrisha UmaliNo ratings yet
- NCP FinalDocument7 pagesNCP FinalApryll Kristin Villaluna ZafeNo ratings yet
- SHOCKDocument17 pagesSHOCKChithra Saju100% (1)
- Cardiogenic ShockDocument3 pagesCardiogenic Shockmerin sunilNo ratings yet
- Case Analysis: Medical Surgical NursingDocument7 pagesCase Analysis: Medical Surgical NursingMaria ThereseNo ratings yet
- Hypovolemic Shock Nursing Care Management and Study GuideDocument1 pageHypovolemic Shock Nursing Care Management and Study GuideRoselyn VelascoNo ratings yet
- Hypovolemic Shock Neurogenic ShockDocument40 pagesHypovolemic Shock Neurogenic ShockWemslaiNo ratings yet
- Drug StudyDocument2 pagesDrug StudyAjay SupanNo ratings yet
- Clinical Exposure Vi Assignment: Faculty of Medicine Universitas Pelita HarapanDocument16 pagesClinical Exposure Vi Assignment: Faculty of Medicine Universitas Pelita HarapanSteven MatualiNo ratings yet
- Endocrine Disorders and DrugsDocument149 pagesEndocrine Disorders and DrugsJaypee Fabros Edra100% (1)
- Shock, Hypovolemic, AnaphylacticDocument17 pagesShock, Hypovolemic, Anaphylacticmhmdalbdyny764No ratings yet
- Diagnosis of ShockDocument9 pagesDiagnosis of ShockRejina RavindranNo ratings yet
- Hypertension and AnaesthesiaDocument3 pagesHypertension and AnaesthesiaVerico PratamaNo ratings yet
- RNPIDEA-Coronary Artery Disease Nursing Care PlanDocument8 pagesRNPIDEA-Coronary Artery Disease Nursing Care PlanAngie MandeoyaNo ratings yet
- Nursing Care PlanDocument19 pagesNursing Care PlanChic Dian UsmanNo ratings yet
- Biologic CrisisDocument242 pagesBiologic CrisismajNo ratings yet
- U World Cardiac FinalDocument15 pagesU World Cardiac FinalAcohCChaoNo ratings yet
- Severe Sepsis and Septic ShockDocument39 pagesSevere Sepsis and Septic ShockYogi Agil MurdjitoNo ratings yet
- Pulmonary Edema: Prepared byDocument13 pagesPulmonary Edema: Prepared bySumathi GopinathNo ratings yet
- Sim Questions CHFDocument5 pagesSim Questions CHF5Dragoon5No ratings yet
- PowerpointDocument12 pagesPowerpointnkurian1No ratings yet
- Sir ClanDocument109 pagesSir ClanJames AbendanNo ratings yet
- Hypovolemic ShockDocument8 pagesHypovolemic ShockLyka Flores100% (1)
- Cardiovascular System Diseases Part 2Document9 pagesCardiovascular System Diseases Part 2Prince Rener Velasco PeraNo ratings yet
- Cardiovascular System Diseases Part 2Document9 pagesCardiovascular System Diseases Part 2Prince Rener Velasco PeraNo ratings yet
- KHH - Hypertension in Surgical Operation Latest PPT FinalDocument37 pagesKHH - Hypertension in Surgical Operation Latest PPT FinalLearnerNo ratings yet
- Chapter 20 Nursing Management Postoperative CareDocument7 pagesChapter 20 Nursing Management Postoperative Caredcrisostomo8010No ratings yet
- Inotropes in Critical Care UnitDocument48 pagesInotropes in Critical Care UnitKelvin Christopher Ker100% (1)
- CardioDocument9 pagesCardioVirgilio Reyes ManuelNo ratings yet
- Shock Pathophysiology: Basic Cardiac PhysiologyDocument4 pagesShock Pathophysiology: Basic Cardiac PhysiologyChynthea ParamithaNo ratings yet
- Deep Vein Thrombosis (DVT)Document15 pagesDeep Vein Thrombosis (DVT)arcci balinasNo ratings yet
- Anesthesia For Emergency SurgeryDocument85 pagesAnesthesia For Emergency Surgeryansuh22100% (11)
- Pulmonary EdemaDocument6 pagesPulmonary EdemaJelly BeanNo ratings yet
- Decrease Cardiac OutputDocument6 pagesDecrease Cardiac OutputGerardeanne ReposarNo ratings yet
- DiagnosisDocument12 pagesDiagnosisHCX dghhqNo ratings yet
- Risk For: Decreased Cardiac OutputDocument5 pagesRisk For: Decreased Cardiac OutputJamal HudaNo ratings yet
- Hypertensive CrisisDocument13 pagesHypertensive Crisis.Katherine CalderonNo ratings yet
- CC-Concept Map 2Document5 pagesCC-Concept Map 2MDCITY50% (2)
- Acute Heart FailureDocument24 pagesAcute Heart FailureTeddy MauriceNo ratings yet
- Shock: Rahayu Setyowati Bachelor of Nursing, Padjadjaran University IndonesiaDocument35 pagesShock: Rahayu Setyowati Bachelor of Nursing, Padjadjaran University IndonesiazafranNo ratings yet
- Case Study HypertensionDocument7 pagesCase Study Hypertensionsanthyakunjumon67% (3)
- Minutes) PRE TESTDocument12 pagesMinutes) PRE TESTRanes AndyNo ratings yet
- Nursing Diagnosis Fluid ExcessDocument8 pagesNursing Diagnosis Fluid ExcessLuthfiy IrfanasruddinNo ratings yet
- Hypovolemic Shock 09Document58 pagesHypovolemic Shock 09Joanne Bernadette Aguilar100% (2)
- Hypovolemic and Anaphylactic ShockDocument38 pagesHypovolemic and Anaphylactic ShockJennifer AmbrosioNo ratings yet
- Nur 111 Session 18 Sas 1Document11 pagesNur 111 Session 18 Sas 1Zzimply Tri Sha UmaliNo ratings yet
- 1 Dental Management of Patients With Cardiovascular DiseasesDocument14 pages1 Dental Management of Patients With Cardiovascular Diseasesاحمد سلامNo ratings yet
- Clinical Evaluation Test Result Trends: DiagnosisDocument3 pagesClinical Evaluation Test Result Trends: DiagnosisStephen CrossNo ratings yet
- Artery Bypass GraftDocument3 pagesArtery Bypass GraftJasmine ChuaNo ratings yet
- Disease - HTML Nursing Care of Coronary Heart Disease - 5 Diagnosis InterventionsDocument6 pagesDisease - HTML Nursing Care of Coronary Heart Disease - 5 Diagnosis InterventionsJihan Hanifah YasminNo ratings yet
- Cerebrovascular DiseasesDocument43 pagesCerebrovascular DiseasesKoRnflakes100% (3)
- ShockDocument34 pagesShockAnthon Kyle TropezadoNo ratings yet
- NCP Nursing Care Plan For Acute Respiratory Distress Syndrome ARDSDocument6 pagesNCP Nursing Care Plan For Acute Respiratory Distress Syndrome ARDSTina Larsen100% (4)
- Pulmonary Hypertension, A Simple Guide to the Condition, Treatment and Related DiseasesFrom EverandPulmonary Hypertension, A Simple Guide to the Condition, Treatment and Related DiseasesNo ratings yet
- Secondary Hypertension: Clinical Presentation, Diagnosis, and TreatmentFrom EverandSecondary Hypertension: Clinical Presentation, Diagnosis, and TreatmentGeorge A. MansoorNo ratings yet
- 2017 A3 What Can Acupuncture Help WithDocument2 pages2017 A3 What Can Acupuncture Help WithmayxzineNo ratings yet
- Supply List For CampersDocument2 pagesSupply List For CampersmayxzineNo ratings yet
- Medisoft 17 User Guide PDFDocument234 pagesMedisoft 17 User Guide PDFmayxzineNo ratings yet
- Three Secret Strategies of SatanDocument14 pagesThree Secret Strategies of SatanBro. Ignatius MaryNo ratings yet
- The 10 Step Guide To Program PlanningDocument5 pagesThe 10 Step Guide To Program Planningmayxzine0% (1)
- Cit0002e 2Document8 pagesCit0002e 2Lupe PerezNo ratings yet
- SULADS CANADA 2017 NewsletterDocument14 pagesSULADS CANADA 2017 NewslettermayxzineNo ratings yet
- 30 Team-Building Games, Activities, and Ideas: 1. The Game of PossibilitiesDocument23 pages30 Team-Building Games, Activities, and Ideas: 1. The Game of PossibilitiesSrihari VenugopalNo ratings yet
- BBG Free Week of Workouts 1Document11 pagesBBG Free Week of Workouts 1AgitaYunitaPutriNo ratings yet
- 2017 A3 What Can Acupuncture Help WithDocument2 pages2017 A3 What Can Acupuncture Help WithmayxzineNo ratings yet
- 100 Ideas For Working With Our YouthDocument4 pages100 Ideas For Working With Our YouthmayxzineNo ratings yet
- Gerson Therapy-Hand Out2Document9 pagesGerson Therapy-Hand Out2mayxzine100% (1)
- BC Hunting RegulationDocument6 pagesBC Hunting RegulationmayxzineNo ratings yet
- Ôm M Ôm M M Ômmm MM MMM MM MM C MMMMMMCM "M MM MMM MDocument3 pagesÔm M Ôm M M Ômmm MM MMM MM MM C MMMMMMCM "M MM MMM MmayxzineNo ratings yet
- Diagnostic Test Khalid (P I H)Document17 pagesDiagnostic Test Khalid (P I H)mayxzineNo ratings yet
- Postpartum Assessment and Nursing ConsiderationsDocument2 pagesPostpartum Assessment and Nursing ConsiderationsHazel PresbiteroNo ratings yet
- Location and Basic Structure of The KidneysDocument4 pagesLocation and Basic Structure of The KidneysmayxzineNo ratings yet
- Uremic EncephalopathyDocument4 pagesUremic EncephalopathySandi BeyNo ratings yet
- SocialProgress Index 2014 ExecSummary DeloitteDocument16 pagesSocialProgress Index 2014 ExecSummary DeloitteIvan OviedoNo ratings yet
- Field Practice 2Document17 pagesField Practice 2Lea Jane Laurete Calledo75% (4)
- Notice: Medical Devices: Premarket Approval Applications, List Safety and Effectiveness Summaries&rsquo AvailabilityDocument2 pagesNotice: Medical Devices: Premarket Approval Applications, List Safety and Effectiveness Summaries&rsquo AvailabilityJustia.comNo ratings yet
- 3a DnDestiny - BestiaryoftheWilds - v0.5Document46 pages3a DnDestiny - BestiaryoftheWilds - v0.5HectorNo ratings yet
- Outline of The Controversial Issue ParagraphDocument2 pagesOutline of The Controversial Issue ParagraphLeo WangNo ratings yet
- CGHS Enclosure 1Document77 pagesCGHS Enclosure 1bhupendrapawar279No ratings yet
- Psychological DisordersDocument44 pagesPsychological DisordersBushra Shaikh100% (1)
- Gianna Graziani Cover LetterDocument1 pageGianna Graziani Cover Letterapi-733890262No ratings yet
- Infection Control Protocols in I.C.U.: Moderator: PresenterDocument54 pagesInfection Control Protocols in I.C.U.: Moderator: PresenterRajaNo ratings yet
- Quick Guide Effective Record Keeping Ordering MedicinesDocument4 pagesQuick Guide Effective Record Keeping Ordering MedicinesnunikwahyuniNo ratings yet
- Travel Nurse Pdf1Document2 pagesTravel Nurse Pdf1Med NetNo ratings yet
- Annual Operational Plan 2012 NarrativeDocument11 pagesAnnual Operational Plan 2012 NarrativeArianne A ZamoraNo ratings yet
- FSA - Eligible ExpensesDocument24 pagesFSA - Eligible ExpensesCatherine MifsudNo ratings yet
- Lapsus NICUDocument49 pagesLapsus NICUZukmianty SuaibNo ratings yet
- 10 in 1 Prime VG PlusDocument2 pages10 in 1 Prime VG PlusHannahNo ratings yet
- Module C Notes 102Document11 pagesModule C Notes 102mwhite8051No ratings yet
- Homework Policy ScotlandDocument9 pagesHomework Policy Scotlandafmtdenav100% (1)
- The Concept of Value AdditionDocument5 pagesThe Concept of Value AdditionNura BasmerNo ratings yet
- General Dentistry Informed Consent FormDocument3 pagesGeneral Dentistry Informed Consent FormNishtha KumarNo ratings yet
- Health Immunization MMR FormDocument2 pagesHealth Immunization MMR FormHenrique Delfino Almeida AlvesNo ratings yet
- All About Baby MassageDocument20 pagesAll About Baby MassageSeptian Widyo RiniNo ratings yet
- UCLA Application Information Packet As of April 04 2014Document18 pagesUCLA Application Information Packet As of April 04 2014UCLA Center for Prehospital CareNo ratings yet
- Review Related LiteratureDocument3 pagesReview Related LiteraturerdsamsonNo ratings yet
- Dentistry in Historical PerspectiveDocument4 pagesDentistry in Historical PerspectiveSartika AmeliaNo ratings yet
- Prime Health Med. Svcs. Co. Laila Gomaa, MD. (PD PMC)Document10 pagesPrime Health Med. Svcs. Co. Laila Gomaa, MD. (PD PMC)James LindonNo ratings yet
- LESSON PLAN On First Aid GNMDocument6 pagesLESSON PLAN On First Aid GNMSamiran Kumar Das100% (1)
- Real Time Surveys Reveal True Feelings About RegistrationDocument8 pagesReal Time Surveys Reveal True Feelings About RegistrationBrittany LudwigNo ratings yet
- 1 LAPORAN KOMPREHENSIF-dikonversiDocument134 pages1 LAPORAN KOMPREHENSIF-dikonversirizkiNo ratings yet
- Corn PresentationDocument20 pagesCorn PresentationPooja ShrivastavNo ratings yet