Professional Documents
Culture Documents
Specialist Scope Report
Uploaded by
sjs315Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Specialist Scope Report
Uploaded by
sjs315Copyright:
Available Formats
AMERICAN BOARD OF OTOLARYNGOLOGY SCOPE OF KNOWLEDGE STUDY SUMM ARY REPORT SPECIALIST Revised 10/1/2003
INTRODUCTION In 1996, the American Bo ard of Otolaryngology (ABO to) commissioned a national practice analysis study to identify the responsibilities associated with basic (minimal) competence in the specialty of otolaryngology-head and neck surgery and the knowledge required to fulfill these responsibilities. The proced ures used in conducting the practice analysis involved an interactive process that combined:
the pra ctice analysis exp ertise of Knapp & Associates International (K &A I) staff; the professional knowledge of an expert Scope of K nowledge Task Fo rce made up of prom inent members of the profession; and the judgem ents of a nationwide sample o f otolaryngologists.
METHOD The design and implementation of the practice analysis study (h ereafter referred to as the Scope of Knowledge Study) consisted of a number of steps carried out between September 1996 and April 1997. These steps are described below. 1. Establishment of Specialty Scope of Knowledge Task Force Members of the Specialty Scope of Knowledge Task Force were appointed jointly by the ABOto and the American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS). These professionals were highly respected experts in the field of otolaryngology and were selected to be representative with respect to geographic region and practice setting. Append ix A contains a list of the physicians participating in the Task Force. The role of the T ask Fo rce wa s to participate in the develop ment of the Sp ecialty Sc ope of Knowledge survey instrument to ensure that the full range of professional tasks and knowledge areas pertinent to the practice of otolaryngology was com prehensively and accura tely represented. In ad dition, the Task Force reviewed draft and final versio ns of the instrume nt, assisted in the interp retation of the survey da ta, and deve loped examinatio n specifications based on the results of the surv ey. 2. Review of the Otolaryngology Literature AB Oto supp lied K &A I with a list of documents providing an overview of the specialty of otolaryngolo gy. These materials included jo urnal articles and seminal textbooks. 3. Interviews of Practitioners A series of 20 telephone interviews was conducted with specialists and subspecialists to determine the core responsibilities and knowledge areas associated with professional practice. In an attempt to differentiate specialty practice from that of the four sub specialties (facial plastic an d reconstructive surgery, head an d nec k surgery, neuro tology, and p ediatric otolaryngology), practitioners also were asked to identify the types o f patients o r problems that they would refer to subspec ialists. 4. Developm ent of Draft Specialty Inventory A draft survey instrument for the specialty was developed based on information obtained from the literature review and telephone interviews. The instrument listed the important professional tasks that otolaryngologists carry out on a day-to-day basis and the knowledge areas they must assimilate in order to carry out these professional responsibilities Page 1 of 10
5.
Revision of the Draft Specialty Inventory On N ovember 1-3, 199 6, the Specialty Scope of K nowledge Task Fo rce convened to review the draft inventory. The subspecialty Task Force chairs also were present to ensure that subspecialty perspectives were considered in the development of the sp ecialty inve ntory. In addition to revising the draft inventory of tasks and knowledge areas, the Task Fo rce develo ped a number o f demographic questions that would help describe the sample and identify categories for use in data analysis. They also selected rating scales (importance and frequency) to be used on the survey. On the final day of the meeting, the Specialty Task Force and the four subspecialty Task Forces met together to discuss the proceedings of the previous days and present the most salient and distinguishing features of their newly developed inventories. The draft inventory was converted to a survey format and reviewed by mail by the Task Force chair. After the revisions suggested by the chair were made, the survey was mailed to the Task Force mem bers for their review. Recommendations made by the Task Force were discussed with the chairs, as needed, and were subsequently incorporated in the survey doc uments.
6.
Preparation of Final Version of the Specialty Scope of Kno wledge Survey Instrument After the final revisions were made, a camera-ready copy of the Specialty Scope of Knowledge Survey was prepared by K& AI, and the d ocuments were p rinted and mailed b y AB Oto.
7.
Selec tion of the Surve y Sample During the development of the survey document, a mailing was sent to all ABOto-certified otolaryngologists requesting that they return a form indicating the area of otolaryngology (i.e., specialty or subspecialty) in which they spend 60% or more of their professio nal time. For the purp oses o f the Sco pe of Kno wledge study, individuals who devoted 60% or more o f their practice to the specialty were classified as "specialists" in otolaryngology-head and neck surgery. The mailing yielded a 65% return rate and ide ntified a total of 4,848 specialists and subsp ecialists. The sampling plan for the specialist survey included both specialists and subspecialists, as it is planned that the specialist certificatio n will be used as a prerequisite for sub sequent subspecialty certifications. Inclusion of subspecialists in the samp le allowe d for d irect gro up co mpa risons o n tasks and knowledge areas. The survey sa mple also wa s stratified with respe ct to years of practice p ost-residency and geograp hic region. The survey was m ailed to a total of 1,00 0 recipients (60 0 specialists, 100 facial plastic and reconstructive surgery subspecialists, 100 head and neck surgery subspecialists, 100 neurotologists, and 100 ped iatric otolaryngologists).
8.
Administration of the Scope of Knowledge Survey The surveys were mailed in January 1997, along with a postage-paid envelope and a cover letter from ABO to President Eugene N . Myers, M D and A AO -HN S President Cha rles J. K rause, MD, ex plaining the purpose of the survey. In an effort to enhance the total return rate, a reminder postcard was sent to each survey recipient approximately two weeks after the initial mailing.
RESULTS A. Resp onse Rate Four hundred and fifty five (455) surveys were received, resulting in a total return rate of 46%. Data analysis was conducted on 430 surveys -- the number received prior to the cut-off date for beginning the analyses. Based on experience with similar surveys, the numbe r of surveys returned was considered to be adequ ate for the purpose of analysis.
Page 2 of 10
B.
Demog raphic Cha racteristics of Respo ndents It was the consensus of the Task Force that the demographic characteristics of the respondents were consistent with those of otolaryngologists practicing the specialty nationwide and that data obtained from the sample provided a solid foundation from which to make decisions regarding the scope of practice and examination specifications. Additionally, the Task Force concurred that the repre sentativeness of the sample wa s such tha t the subsamp le analyse s could be interpreted w ith confidence.
C.
Analysis of Task Impo rtance Ratings Task importance ratings were analyzed by total sample, focus of practice, years of practice post-residency (1-5, 6-20, 21+), and type of practice (academic vs. clinical). All but 4 of the 109 tasks were judged to be of at least moderate importance by the total sample.
D.
Analysis of Task Frequency Ratings Task frequency ratings also were analyzed by total sample, focus of practice, years of practice, and type of practice. All but 17 of the 109 tasks were judged to be performed at least occasionally (defined as 26-50% of the time in a series of 100 consecutive patients) by the total sample.
E.
Analysis of Knowledge Imp ortance Ratings Knowledge importance ratings were analyzed by total sample, focus of practice, years of practice post-residency (1-5, 6-20, 21+ ), and type of pra ctice (academic vs. clinical). All but 8 of the 226 subknow ledge areas were judged to be of at least moderate importance by the total sample.
F.
Analysis of Knowledge Freq uency Ratings Knowledge freque ncy ratings also were analyzed by total sample, focus o f practice, years of practice, and type of practice. Eighty-three (83) of the 226 subknowledge areas were judged to be used at least occasionally (defined as 26-50% of the time in a series of 100 consecutive patients) by the total sample.
G.
Developm ent of Examination Specifications After a preliminary review of the survey re sults, the T ask Fo rce develo ped decisio n rules for the inclusion of respo nsibility dimensions (and the tasks subsum ed under each d imension) in the exam ination specifications. T he relevance of taking into account both the importance and frequency ratings was discussed with the group; however, the Task Force ultimately decided to focus only on importance ratings. Unless otherwise decided by the Task Force, tasks were included if the mean importance rating for the total sample was above 2.0. W hen reviewing the sub knowled ge areas, the T ask Force once again chose to focus on imp ortance ratings. Initially, the Task Force elected to include subknowledge areas with mean ratings greater than 2.0; however, this decision-rule was later changed to include mean ratings greater than 2.5 due to the group's concern that the number of subknowledge areas retained was too large and the content areas too specific to be adequately addressed on a 240-item examination. In addition, a number of related subknowledge areas were clustered together, thus reducing the total number of subknowledge areas. The subknowledge areas identified as being the m ost imp ortant to the practice of the specialty of otolaryngolo gy are listed in Appendix B . The cognitive level (recall, interpretation, pro blem-solving) at which each subknowledge area was to be assessed was also determined . It was the consensus of the Task Fo rce that the specifications should be flexible with respe ct to co gnitive level, as it was their opinion that each subknowledge area could be assessed at each cognitive level. However, the group did agree that 25% of the examination questions should assess knowledge at the recall level, 25% o f the questions should be at the interpretation level, and 50% of the questions should assess problem-solving. In addition, the Task Force indicated that the oral examination should emphasize problem-solving, with few, if any, questions designed to assess knowledge at the recall or interpretation levels.
Page 3 of 10
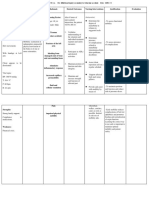
Recomm endations from survey respondents regarding the proportion of the examination to be devoted to the various knowledge areas served as an initial guide to the Task Force in determining this aspect of the examination specifications. The following kno wledge areas and associated p ercen tages were ultimately agreed upon by the Task Force: Know ledge Area Diagnostic and Assessment Procedures Diseases, Disorders and Conditions Habilitation/Rehabilitation Approaches Basic Concep ts Associated with Surgery Specific Surgical Procedures Basic Science Science of Head and Neck Structures Pharmacology Total Numb er of Items Percent of Exam 17 18 4 11 23 8 10 8 Number of Items 41 43 10 27 55 20 24 20 240
The Task F orce no ted that at some p oint in the future, new content areas (i.e., ethical considerations and b usiness practices) should be added to the examination specifications to reflect recent changes in residency training. The Task Force determined that an examination of 240 questions would be of sufficient length to assess the knowledge areas represented on the examination matrix. They then selected the number of exam questions to be dedicated to each subknowledge area, using the knowledge impo rtance ratings from the survey as a guide. Other examination characteristics discussed by the Task Force included the use of visuals and case material. It was agreed that the goal should be for 20-25% of the examination to be based on visuals; however, it was observed that progress toward this goal would likely be gradual as it is dep endent on the num ber o f visuals currently in the poo l and the numb er ob tained in future item -writing drives. T he T ask Fo rce co ncurred that case m aterial sho uld be emphasized on the exam ination, b ut did not decide on a spe cific percentage o f examination questions that should be case based. Although the value of multi-item case sets composed of independent items was discussed, the Task Force d ecided that cases should continue to consist of only one item, as they felt that having more than one item per case might place the candidate in a "double jeopa rdy" situation.
SUMM ARY The primary purpose of the practice analysis was to delineate a body of professional knowledge judged by practitioners to be an impo rtant prerequisite to practicing at a level of basic (minim al) compe tence in the spe cialty of otolaryng ology-head and neck surgery. A select Scope of Knowledge Task Force consisting of prominent physicians representing the specialty developed an inventory of critical tasks and knowledge areas which was subsequently converted to a survey format and mailed to a representative national samp le. The surve y results co nfirmed and su ppo rted the work of the T ask Fo rce and identified the most crucial knowledge areas. Thus, the survey results provided a sound basis for identifying the content appropriate for inclusion in a certification examination. The development of the examination specifications was guided by the results of the survey and the expert opinion of the Task Force. A professional certification examination based upon examination specifications derived from the information collected in the practice analysis study will provide a practice-related and content-valid standard. The practice analysis provided a core bo dy of important professional knowledge areas on which there is substantial agreement. The establishment of an examination developed from databased specifications will serve to advance the specialty of otolaryngology-head and neck surgery and contribute to maintaining high standards of patient care.
Page 4 of 10
APPENDIX A SCOPE OF KNOWLEDGE TASK FORCE Specia list
Harold C. Pillsbury, III, M D, C hair N eil O . W a rd, M D M ic ha el E. J ohns, M D H erbert C . J ones, M D J erome C. G oldste in, M D J onas T. J ohnson, M D J ohn G . C ampbell, M D Lee D. Eise nberg, M D J ames A . H adle y, M D Ira D. Papel, M D G ary T. Turner, M D
Page 5 of 10
APPENDIX B SCOPE OF K NOW LEDGE: SPECIALTY
I.
SCIENCE OF HEAD AND NECK STRUCTURES (10% of Exam/Curriculum) A. Embryology, anatom y, physiology, histology and pathology of: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. B. Ear Nose and paranasal sinuses Ora l cavity Salivary glands Pharynx/esophagus Larynx/trachea Thyroid and parathyroid glands Face and neck/skin, integument, muscles Facial skeleton and skull base Nervous system structures related to the head and neck Other sites important for the evaluation and treatment of the head and neck cond itions
Basic physiology, patho physiology and principles of: 1. 2. 3. Hearing/equilibrium Speech/voice/language Sme ll/taste
II.
BASIC SCIENCE (8% of Exam/Curriculum) A. Basic con cepts and application to otolaryngology: 1. 2. 3. 4. 5. 6. 7. Immunology/allergy Microb iology/virology Endocrinology Neurology Mo lecular biology Genetics Epidemiology
Page 6 of 10
III.
DIAGNOSTIC & ASSESSMEN T PROCEDU RES (17% of Exam/Curriculum) A. Pro per technique, indications, limitations, and normal and patho logical findings o f: 1. Face a. Ear a. b. c.
Aesthetic assessment
2.
Otoscopy/microscopy/pneumatic otoscopy/tuning forks Hearing testing Vestibular function testing
3.
Nose/paranasal sinuses a. Rhinoscopy/endoscopy Ora l Cavity a. Inspection and palpation b. Dental occlusion Nasopharynx a. Mirror examination/endoscopy Hypop harynx/larynx a. Mirror examination/endoscopy Neck a. b. c. d.
4.
5.
6.
7.
8.
Vid eostro boscop y/voice analysis Inspection/palpation/auscultation Fine needle aspiration Eso phagus/trachea (including bro ncho esop hagology, endoscop y, manometry, pH probes, biopsy, pulmonary function tests) Neurological a. Cranial nerves
B.
Indications, limitations, and normal and patholo gical findings of: 1. Imaging studies a. Plain radiographs b. Comp uted tomography c. Magne tic resonance imaging d. Ultrasound e. Nuclear medicine
C.
Pro per technique, indications and norm al and patho logical findings o f: 1. 2. 3. 4. Laboratory studies Histopathology Assessment of psychological and social development and functioning Assessment of occupational functioning
Page 7 of 10
IV.
DISEASES, DISORDERS, AND COND ITIONS (18% of Exam/Curriculum) A. Etiology, diagnostic criteria, differential diagnosis, prognosis, treatment options, common complications, and impact on all spheres of functioning: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. Congenital Degenerative Idiopathic Infectious Inflamm atory - tox ic Inflamm atory - allergic Inflammatory - vascular Inflammatory - immune related Metabo lic Neoplastic Psychoge nic Iatrogenic Pain Foreign Body Trauma - soft tissue Trauma - skeletal Cosmetic and reconstructive
V.
PHARM ACOLO GY (8% of Exam/Curriculum) A. B. Treatment of an aphylaxis Principles of medication use, route of administration, mechanisms of action, indications/co ntraind ications, proper usage, interaction effects, an d limitations of: 1. 2. 3. 4. 5. 6. 7. 8. Antibiotics Nasal decongestants/antihistamines Antivertiginous medications/antiemetics To pical and systemic anti-inflamma tory agents (steroids and nonsteroida ls) Antireflux agents Pain me dications (e.g., analgesics, sedatives, hypnotics, psychotrop ics) Antineoplastic agents Skin m odifying agents
VI.
BASIC CONCEPTS ASSOC IATED WITH SURGERY (11% of Exam/Curriculum) A. B. C. D. Types of surgical facilities and their suitability for various types of procedures Universal precautions Preoperative and postoperative care Basic techn iques, indications and contraindications of anesthetic agents: 1. Sedation 2. Local anesthesia 3. General anesthesia Intraoperative fluids and medications Airway management W ound managem ent Gra fts (autografts, hom ografts, and allo plasts Flaps (cutaneous, myocutaneous, osteomyocutaneous, and free) Prosthetics Mana gement of common co mplications occurring during and following surgery Basic techn iques, indications and contraindications of surgical mod alities: 1. Endosco pic surgery 2. Laser surgery
E. F. G. H. I. J. K. L.
Page 8 of 10
VII.
SPECIFIC SURGICAL PROCEDURES (23% of Exam/Curriculum) Proper tec hniq ue, indications, contra indication s, risks/benefits and com plications o f: A. Facial Plastic and Reconstructive 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. B. Otology 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. Canaloplasty Middle ear exploration Tym panoplasty/myringo plasty Stapedectomy Labyrinthectomy Mastoidectomy Tympanomastoidectomy Meatop lasty Myringotomy Endolymphatic sac surgery Rep air of perilymp hatic fistula Transtympanic installation of ototoxic drugs Cochlear implantation Glomus tympanicum Congenital middle ear reconstruction Rhinoplasty/revision rhinoplasty/reduction of nasal fractures Oto plasty Rhytidectomy Forehead and brow lift Blepharoplasty and other periorbital procedures Mana gement of alopecia and reconstructive scalp surgery Facial implants Scar revision Extratemporal facial reanimation Soft tissue expansion Mandibular reconstruction Reconstruction of cleft lip and palate deformities Reco nstruction of other cran iofacial deformities (e.g., microtia, facial dysotosis) Treatment of facial fractures Excision of skin lesions Reconstruction o f soft tissue defects Skin resurfacing techniques
Page 9 of 10
C.
Head and Neck 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. Tonsillectomy/adenoidectomy Tracheostomy Arterial ligation Maxillectomy (with or without orbital exenteration)/partial maxillectomy/intraoral resection/oral cavity resection/composite resection/glossectomy Pharyngotomy Uvulopharyngopa latoplasty/office uvulop haryngopa latoplasty Direct laryngoscopy/microlaryngoscopy Phonatory surgery/framework surgery Laryngotracheo plasty/ep iglottop lasty Management of laryngeal fractures Repair of caustic injection injuries of pharynx and esophagus and thermal injury of upper airway Partial laryngectomy/total laryngectomy/pharyngectomy Arytenoidectomy/arytenoidopexy Mandibulectomy/mandibular osteotomy Parotidectomy Neck dissection Excision of mass of parapharyngeal space (including chemodectoma, neurilemmoma removal ) Cricopharyngeal myotomy Excision of congenital cysts and sinus (branchial cleft, thyroglo ssal duct) Reconstruction of vascular malformation (lymphatic, venous, hemangioma) Pharyngoesophageal reconstruction Neck abscess drainage Repair of penetrating injuries of the head and neck Zenkers diverticulectomy Treatment of laryngeal clefts and tracheoesophageal fistulas Surgical voice restoration (TEP) Tracheal resection Thyroidectomy Parathyroidectomy Skull base surgery
D.
Sinus Surgery 1. 2. 3. 4. 5. 6. 7. 8. Ethmoid/ethmoidectomy/frontoethmoidectomy Maxillary/Caldwell-Luc Frontal/trephination/obliteration/ablation Sphenoid/hypophysectomy Septoplasty/turbinate surgery Dacryocystorhinostomy Epistaxis management Orbital decompression
VIII.
HABILITATION/REHABILITATION APPROACH ES (4% of Exam/Curriculum) A. B. C. Vocal/speech/language therapy Swallowing rehabilitation Aural habilitation 1. 2. Hearing aids Vestibular rehabilitation
Page 10 of 10
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- LeechDocument3 pagesLeechsjs315No ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Excision of Branchial Cleft CystsDocument10 pagesExcision of Branchial Cleft Cystssjs315No ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Tisseel Package InsertDocument12 pagesTisseel Package Insertsjs315No ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Curriculum 10-19-07 FinalDocument97 pagesCurriculum 10-19-07 Finalsjs315No ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- New 5Document37 pagesNew 5rishi gupta100% (1)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Register Now for the 3rd Hematology Forum 2023Document1 pageRegister Now for the 3rd Hematology Forum 2023modather sanosiNo ratings yet
- A Case-Based Guide To Clinical Endocrinology (October 23, 2015) - (1493920588) - (Springer)Document434 pagesA Case-Based Guide To Clinical Endocrinology (October 23, 2015) - (1493920588) - (Springer)AbdulraHman KhalEd100% (2)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- NCP OrthoDocument2 pagesNCP OrthoJeyser T. GamutiaNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Edna K.huffman - Health Information Managemen 1994Document36 pagesEdna K.huffman - Health Information Managemen 1994gspot967% (6)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- 3 Azarpour Et Al. JNBR 4 (1) 2015 PDFDocument9 pages3 Azarpour Et Al. JNBR 4 (1) 2015 PDFKamailNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Negative Feedback Thyroxine and Adrenelin WsDocument2 pagesNegative Feedback Thyroxine and Adrenelin WsEllie AbelNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- CPR and Aed: Quiz #2 ResultsDocument2 pagesCPR and Aed: Quiz #2 ResultsNathan WhiteNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- It PDFDocument385 pagesIt PDFCosmina UngurNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Pahs Mbbs Information BookletDocument18 pagesPahs Mbbs Information BookletKishor BajgainNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- CommonGround 8 26 BrierleyDocument84 pagesCommonGround 8 26 Brierleytuinbroek_94397869No ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- 5 Weeks To 5km Beginner and Intermediate PDFDocument1 page5 Weeks To 5km Beginner and Intermediate PDFMutsai MusaNo ratings yet
- Chapter 4intestinal NematodesDocument41 pagesChapter 4intestinal Nematodesdeneke100% (1)
- Margaret Moore Bob Tschannen-Moran Erika JacksonDocument201 pagesMargaret Moore Bob Tschannen-Moran Erika JacksonBella100% (18)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Ecg Quick Guide PDFDocument7 pagesEcg Quick Guide PDFansarijavedNo ratings yet
- Bapat Et Al. - 2006 - Quantification of Metabolically Active Biomass Using Methylene Blue Dye Reduction Test (MBRT) Measurement of CFU IDocument10 pagesBapat Et Al. - 2006 - Quantification of Metabolically Active Biomass Using Methylene Blue Dye Reduction Test (MBRT) Measurement of CFU IJosé Matías ZapiolaNo ratings yet
- SURAT KETERANGAN DOKTERDocument1 pageSURAT KETERANGAN DOKTERalha egaNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Classi Fications of Adverse Drug Reactions: 1. EidosDocument6 pagesClassi Fications of Adverse Drug Reactions: 1. Eidosdolemite4No ratings yet
- Master Tong-Style Acupuncturist Interview Part 1Document4 pagesMaster Tong-Style Acupuncturist Interview Part 1Anonymous uMnup2r100% (1)
- Disturbing Art Exposes Modern Culture AbsurditiesDocument15 pagesDisturbing Art Exposes Modern Culture Absurdities2aethicusNo ratings yet
- Stress (Biology) : 1 Etymology and Historical UsageDocument19 pagesStress (Biology) : 1 Etymology and Historical UsageZiedTrikiNo ratings yet
- 12-Channel ECG SpecsDocument5 pages12-Channel ECG SpecsNai PaniaiNo ratings yet
- Latest Guideline on Caries-risk Assessment and ManagementDocument8 pagesLatest Guideline on Caries-risk Assessment and ManagementPriscila Belén Chuhuaicura SotoNo ratings yet
- Chemicals Zetag MSDS Powder Zetag 4139 - 1010Document6 pagesChemicals Zetag MSDS Powder Zetag 4139 - 1010PromagEnviro.comNo ratings yet
- 01 1 PDFDocument8 pages01 1 PDFpravikumar1989No ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Medication Order Unit 11Document10 pagesThe Medication Order Unit 11novie100% (2)
- AnupanaDocument60 pagesAnupanaVaidya Nur50% (4)
- Tugas B.inggrisDocument14 pagesTugas B.inggrisLove.u. TooNo ratings yet
- Nursing Process Record - Nursing FundamentalsDocument17 pagesNursing Process Record - Nursing FundamentalsheidiheffNo ratings yet
- DAFTAR PUSTAKA (Benar)Document6 pagesDAFTAR PUSTAKA (Benar)Yulanda MarestaNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)