Professional Documents
Culture Documents
Nutrition Risks in Pregnancy Assess FU Intervene
Uploaded by
John Lee Lorena GacusanOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nutrition Risks in Pregnancy Assess FU Intervene
Uploaded by
John Lee Lorena GacusanCopyright:
Available Formats
Nutrition Risk in Pregnancy
Assessment:
There are many situations that may lead to compromise of nutritional status just prior to or at the onset of pregnancy. Given that 96% of US women have diets that do not follow the Food Guide Pyramid, many women may be at risk. This list includes items where there is not only a nutritional risk, but also a benefit to nutrition intervention. Risks prior to pregnancy should be monitored, as these risks typically do not disappear, but rather may diminish during pregnancy. At the same time, additional risks may develop due to compromised intake or increased nutritional needs. What appear to be even small concerns should be put into the context of nutritional status.
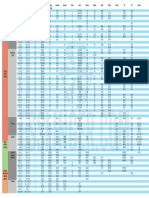
Common Nutritional Risk Factors Prior to or at Onset of Pregnancy
Pre-pregnancy Underweight (BMI<19.8) Pre-pregnancy Obesity (BMI >29.0) Is younger than 15 or has a gynecological age of less than 2 years (< 2 years of menarche) Recent, non-therapeutic weight loss of >5% body weight in less than one month or 7.5% in the past three Frequent diets to lose weight in the last six months Eating disorder current or history of Anemia (<11.0 Hgb) High parity and a young age (less than 20 with three or more pregnancies carried to 20 weeks) Conception within 16 months of the delivery of an infant with birthweight > 500 grams or 20 weeks gestation Faddish food habits; e.g. avoids types or categories of foods; long eating spans; other aversions Vegetarian diet that is not properly planned Has a metabolic disease such as diabetes or inborn error of metabolism (e.g phenylketonuria)
Other chronic condition affecting absorption or utilization of nutrients as well as treatment/medications that interact with nutrients pay special attention to serious gastrointestinal disorders such as Crohns disease and short bowel syndrome; food allergies; lupus erythematosus; prolonged infections; HIV; hypothyroidism; cystic fibrosis; asthma; renal disease; serious dental disease Depression; bi-polar disorder; schizophrenia History of bariatric or gastric bypass surgery Is currently breastfeeding a child Poor obstetrical history that includes poor fetal development Is economically deprived or lives far from a grocery store Elevated blood lead level Substance use (alcohol, illegal drugs, tobacco) Low income/poverty or food insecurity
Nutrition Problems During Pregnancy
Inappropriate weight gain: o Women with low pregravid weight failing to gain 1 # per week after 12 weeks o Loss > 2 # after 13 weeks o Gain < 4# or > 7# per month Nausea and vomiting of pregnancy; constipation; heartburn Serious or significant food aversions including faddish food habits Reported/suspected poor diet quality (often noticed through weight changes, but not always) Faddish food habits Anemia (<9.9 Hgb in any trimester) Multifetal gestation Pregnancy induced conditions such as gestational diabetes; Hyperemesis gravidarum Poor folic acid, calcium, iron intake due to aversions, pica or cravings Use of herbal remedies that may not be safe during pregnancy (See ADA position paper) Food-borne illness Substance use (alcohol, illegal drugs, tobacco) Elevated blood lead level
Created by Improving Pregnancy Care in Vermont (Lisa Richardson, MS, RD, LDN, North Carolina Division of Public Health. 2004). Vermont Child Health Improvement Program, Burlington, VT
Talking About Nutrition
Intervention:
Knowledge is important! Talking about weight gain recommendations is more likely to achieve the Institute of Medicine goals. Set goals together. Frequency of eating is an important indicator for outcome and diet quality. Provide ideas of snacks that are not high calorie nor high fat. Dont overlook readiness to change! Make sure she is ready to talk about it especially if it is a problem. Ask about food security issues not just hunger. Poor income leads to purchase of non-nutrient dense foods that have lots of calories! Overweight and/or high weight gain can go along with lack of access to food. Trigger questions are a great way to get the conversation going. A few simple, open-ended questions can garner a lot of information. Some good examples are below. 1. Have you made any changes to the way you eat since you found out you are pregnant? a. No How many times a day do you eat? Do you intend to make any changes in the near future or because of your pregnancy? If concerned you can ask: what kinds of foods do you usually eat; are there foods that you avoid? b. Yes - Tell me about them. Did someone tell you to do this? How many times a day do you eat? Are you eating a lot more, a little more, a lot less or a little less. 2. Today, you weight was _________How do you feel about that number? a. Have you recently gained or lost a lot of weight? 3. How much weight do you think you should gain during this pregnancy? a. According to how much you weighed before pregnancy, your goal should be__________. Do you think that is something that you can do? 4. Do you always have enough money to buy the food you need? 5. Does the food you buy last and do you (or your household) have enough money to buy more? a. Have you or anyone in your household ever cut the size of your meals or skipped them because there wasn't enough money for food? Refer red flags to nutritional counselor, WIC, Food Stamps, or food pantries as needed and available. Refer to social worker, as available, and nutritional counselor for assistance with stress and more intense nutritional counseling. Refer to a mental health professional and a nutritional counselor if an eating disorder is suspected.
Closing the Nutrition Circle
Follow-up:
Assess weight, appetite, changes to diet, and access to food at every visit, and encourage continued, steady gains. Plot changes in weight on a graph, and look for trends that might indicate inappropriate weight gain. Follow-up on referrals, and continue ongoing re-assessment for changes in nutritional status.
Created by Improving Pregnancy Care in Vermont (Lisa Richardson, MS, RD, LDN, North Carolina Division of Public Health. 2004). Vermont Child Health Improvement Program, Burlington, VT.
VERMONT CHILD HEALTH IMPROVEMENT PROGRAM I MPROVEMENT
You might also like
- Limamg BisitaDocument1 pageLimamg BisitaJohn Lee Lorena GacusanNo ratings yet
- Prayer Before WorkDocument2 pagesPrayer Before WorkJohn Lee Lorena GacusanNo ratings yet
- Training of Trainers On 2013 Manual of Procedures of The NTP, 5 Edition Date: - Venue: - RationaleDocument5 pagesTraining of Trainers On 2013 Manual of Procedures of The NTP, 5 Edition Date: - Venue: - RationaleJohn Lee Lorena GacusanNo ratings yet
- The Anatomy of the Integumentary System: Skin's Two LayersDocument7 pagesThe Anatomy of the Integumentary System: Skin's Two LayersJohn Lee Lorena GacusanNo ratings yet
- Ra 7883Document3 pagesRa 7883John Lee Lorena GacusanNo ratings yet
- Complete Blood CountDocument10 pagesComplete Blood CountJohn Lee Lorena Gacusan100% (1)
- IMPACDocument186 pagesIMPACJohn Lee Lorena GacusanNo ratings yet
- The Cardiovascular SystemDocument21 pagesThe Cardiovascular SystemJohn Lee Lorena GacusanNo ratings yet
- RNHeals AppformDocument1 pageRNHeals AppformmarieNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Battery Cross Reference Chart - UnknownDocument1 pageBattery Cross Reference Chart - UnknownILikeScribd5050No ratings yet
- BEO Meeting GuidanceDocument20 pagesBEO Meeting Guidancesiput23100% (1)
- Workshop 19-10-23Document4 pagesWorkshop 19-10-23nathyoleasNo ratings yet
- Ede MicrprjctDocument21 pagesEde Micrprjct68 Nitesh PundgeNo ratings yet
- 3 Skema Proses Pabrik Kelapa SawitDocument2 pages3 Skema Proses Pabrik Kelapa SawitWynne RaphaelaNo ratings yet
- 7 homemade organic pesticidesDocument3 pages7 homemade organic pesticidesWinssisNo ratings yet
- Simple Saraswati Homa: (1) Om Keśavāya Svāhā (2) Om Nārāya Āya Svāhā (3) Om Mādhavāya Svāhā OmDocument4 pagesSimple Saraswati Homa: (1) Om Keśavāya Svāhā (2) Om Nārāya Āya Svāhā (3) Om Mādhavāya Svāhā OmSoumava PalNo ratings yet
- Product 6Document5 pagesProduct 6TsabitaNo ratings yet
- ANCW30011 - Topic 7 ReadingsDocument41 pagesANCW30011 - Topic 7 ReadingsfaithNo ratings yet
- Phenylketonuria: Dietary Information For The Treatment ofDocument13 pagesPhenylketonuria: Dietary Information For The Treatment ofLuz Del ValleNo ratings yet
- Gcp1a Zambia Manuscript Art of MabisiDocument25 pagesGcp1a Zambia Manuscript Art of Mabisielizabeth haunduNo ratings yet
- 5 PsDocument14 pages5 PsNhật Anh PhạmNo ratings yet
- Hajj PKG 2024 - Labbaik HajjDocument5 pagesHajj PKG 2024 - Labbaik HajjAdil UsmaniNo ratings yet
- Investor - S Guide To The Care Economy - Four Dynamic Areas of Growth - July 2021Document266 pagesInvestor - S Guide To The Care Economy - Four Dynamic Areas of Growth - July 2021simyanliangNo ratings yet
- Barangay Profile of BulasaDocument6 pagesBarangay Profile of BulasaSharlene Mae DeiparineNo ratings yet
- Make It Easy!: BartendingDocument259 pagesMake It Easy!: BartendingObsessionNo ratings yet
- Kisi-Kisi Bing Answered 1-60Document12 pagesKisi-Kisi Bing Answered 1-60Rafli ApiNo ratings yet
- Soal PAT Kelas VIII - Bahasa InggrisDocument7 pagesSoal PAT Kelas VIII - Bahasa InggrisDavira Sandang OriNo ratings yet
- 40 Nov c114Document9 pages40 Nov c114bt20103120 Bharat SinghNo ratings yet
- Another Cup of CoffeeDocument86 pagesAnother Cup of CoffeeKarim ElouedNo ratings yet
- How A Man That Looks 20 at 50 Lives and What His Diet Is Like Bright SideDocument1 pageHow A Man That Looks 20 at 50 Lives and What His Diet Is Like Bright SideAmir AramNo ratings yet
- Math G5 Q1 WK2Document13 pagesMath G5 Q1 WK2MuhammadIshahaqBinBenjaminNo ratings yet
- Max Cafe Menu 2023Document2 pagesMax Cafe Menu 2023max.svjastinNo ratings yet
- Xavier University - Ateneo de CagayanDocument50 pagesXavier University - Ateneo de CagayanSheena AsahidNo ratings yet
- Gelatinized Sweet Potato Starches Obtained at Different Preheating Temperatures in A Spray DryerDocument8 pagesGelatinized Sweet Potato Starches Obtained at Different Preheating Temperatures in A Spray DryerThaís PaesNo ratings yet
- Count and Noncount NounsDocument3 pagesCount and Noncount NounsJorge GamaNo ratings yet
- IAF TC Meeting Minutes DraftDocument46 pagesIAF TC Meeting Minutes DraftArmand LiviuNo ratings yet
- Agroforestry As A Means of Alleviating Poverty in Sri LankaDocument7 pagesAgroforestry As A Means of Alleviating Poverty in Sri LankaArjuna SeneviratneNo ratings yet
- Report On MaFAAS Workshop and General Assembly 8 To 9 May 2013Document112 pagesReport On MaFAAS Workshop and General Assembly 8 To 9 May 2013Paul FatchNo ratings yet
- DEPORTEDocument108 pagesDEPORTEBritany Osorio MoranNo ratings yet