Professional Documents
Culture Documents
Manual Intern
Uploaded by
alvinatOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Manual Intern
Uploaded by
alvinatCopyright:
Available Formats
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
Manual for Paediatric Interns and Residents
4th edition (October 2010) To be reviewed in October 2013
Edited by Dr A Tsang Contributed by Prof CF Chan, Prof YF Cheung, Ms SY Chiu, Dr S Chim, Dr S Chiu, Dr HK Ho, Dr SL Lee, Dr YK Ng, Dr NS Tsoi, Dr KY Wong, Dr R Wong, Dr A Yung
The University of Hong Kong Department of Paediatrics and Adolescent Medicine Queen Mary Hospital
__________________________________________________________________________________
- 1 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
PREFACE
Welcome to the Department of Paediatrics and Adolescent Medicine (UPAM)! Our department, like any other units in this teaching hospital, strives for excellence in quality of patient care, academic and educational pursuits. However, we differ in that we deal with children. Hospitalisation is a very distressing event for both the children and their family. Not only do we need to have the knowledge and technical skills to treat the physical conditions, we must also develop skills in handling the social and emotional needs of the children and their families. Be motivated as this is the pre-requisite for being a good doctor. It is our aim that you will develop clinical competence in managing common paediatric problems through working under supervision and we hope you will share with us the joy of helping children and their families through their illness.
__________________________________________________________________________________
- 2 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
CONTENTS
PREFACE .................................................................................................................... 2 CONTENTS ................................................................................................................. 3 SECTION 1: GENERAL INFORMATION..................................................................... 5 1.1 OUR DEPARTMENT - UPAM................................................................................. 6 1.2 GENERAL INSTRUCTIONS TO INTERNS AND RESIDENTS .............................. 7 1.3 ORIENTATION TO MEDICAL STAFF IN HKWC .................................................... 8 1.4 GOOD CLINICAL DOCUMENTATION AND CASEMIX .......................................... 9 1.5 DISEASE CODING AND COMMON ERRORS IN MAR /MOE..............................11 1.6 INFECTION CONTROL IN PAEDIATRIC WARD ................................................. 13 1.7 ADMISSION OF PAEDIATRIC PATIENTS............................................................ 18 SECTION 2: PROCEDURES IN PAEDIATRICS........................................................ 20 2.1 BLOOD SPECIMEN COLLECTION ..................................................................... 21 2.2 CAPILLARY PUNCTURE (HEEL PRICK) ............................................................ 22 2.3 BLOOD TAKING FROM CENTRAL VENOUS CATHETER.................................. 23 K8 HICKMAN CATHETER BLOOD TAKING (non-touch sterile technique) ............ 23 2.4 PRE-TRANSFUSION COMPATIBILITY TEST IN NEONATES CROSS MATCH ........................................................................................................................ 25 2.5 URINE EXAMINATION......................................................................................... 26 2.6 URINARY BLADDER CATHETERISATION ......................................................... 28 2.7 LUMBAR PUNCTURE ......................................................................................... 29 2.8 MANTOUX TEST ................................................................................................. 31 2.9 SEDATION FOR PROCEDURES ........................................................................ 32 2.10 STEROID PREMEDICATION IN RADIOLOGICAL INVESTIGATIONS .............. 38 2.11.PRE-OPERATIVE FASTING FOR PATIENTS UNDERGOING ANAESTHESIA 2.12 CARDIAC PULMONARY RESUSCITATION ...................................................... 41 2.13 MANAGEMENT OF ANAPHYLAXIS .................................................................. 42 SECTION 3: COMMON PAEDIATRIC PROBLEMS.................................................. 43 SECTION 3.1: RESPIRATORY SYSTEM ................................................................. 44 3.1.1: MANAGEMENT OF CHRONIC ASTHMA ........................................................ 45 3.1.2: MEDICATION FOR ALLERGIC RHINO-CONJUNCTIVITIS............................. 52 3.1.3: MEDICATION FOR ECZEMA........................................................................... 54 3.1.4 ACUTE ASTHMATIC ATTACK........................................................................... 56 3.1.5 ACUTE RESPIRATORY DISTRESS ................................................................. 59 3.1.6 ACUTE UPPER AIRWAY OBSTRUCTION........................................................ 60 3.1.7 ACUTE VIRAL BRONCHIOLITIS ...................................................................... 62 SECTION 3.2: INFECTION........................................................................................ 63 3.2.1 ANTIMICROBIAL THERAPY ............................................................................. 64 3.2.2 COMMONLY USED ORAL ANTIBIOTICS......................................................... 67 3.2.3 FEVER .............................................................................................................. 69 SECTION 3.3: CARDIOLOGY................................................................................... 70 3.3.1 INFECTIVE ENDOCARDITIS PROPHYLAXIS ................................................. 71 3.3.2 HEART FAILURE .............................................................................................. 72 3.3.3 SHOCK ............................................................................................................. 73 SECTION 3.4: NEUROLOGY .................................................................................... 74 3.4.1 ACUTE ENCEPHALOPATHY............................................................................ 75
__________________________________________________________________________________
- 3 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.4.2 FEBRILE CONVULSIONS ................................................................................ 78 3.4.3 PROLONGED SEIZURE, SERIAL SEIZURE, CONVULSIVE STATUS EPILEPTICUS ................................................................................................. 79 SECTION 3.5: GENERAL PAEDIATRICS ................................................................. 85 3.5.1 DIARRHOEA ..................................................................................................... 86 3.5.2 FLUID AND ELECTROLYTES........................................................................... 88 3.5.3 CHILD ABUSE................................................................................................... 92 3.5.4 URINARY TRACT INFECTION ......................................................................... 95 3.5.5 NEPRHITIC SYNDROME ................................................................................. 96 3.5.6 ACUTE POISONING ......................................................................................... 97 SECTION 3.6 : PAEDIATRIC HAEMATOLOGY & ONCOLOGY............................. 103 3.6.1 MANAGEMENT OF NEUTROPENIC FEVER ................................................. 104 3.6.2 MANAGEMENT OF HAEMOPHILIA ............................................................... 106 3.6.3 MANAGEMENT OF THALASSEMIA MAJOR.................................................. 107 3.6.4 MANAGEMENT OF NON-IMMUNE THROMBOCYTOPENIA ........................ 109 3.6.5 MANAGEMENT OF IMMUNE THROMBOCYTOPENIA (ITP)......................... 110 3.6.6. MANAGEMENT OF TRANSFUSION REACTION...........................................111 SECTION 3.7 : NEONATOLOGY............................................................................. 114 3.7.1 NEONATAL INFECTION ................................................................................. 115 3.7.2 MANAGEMENT OF NEONATAL JAUNDICE .................................................. 117 Indications for PT/ET for babies with GA 35 weeks ................................................ 117 Assessment at K8S/K10S (see Appendix 1)............................................................. 120 Assessment of a newborn with jaundice................................................................... 126 Guidelines of use of Minolta JM-103 in postnatal ward ............................................ 132 SECTION 4 : UPAM USEFUL TELEPHONE NUMBERS ........................................ 133 NOTES ..................................................................................................................... 134
__________________________________________________________________________________
- 4 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
SECTION 1: GENERAL INFORMATION
__________________________________________________________________________________
- 5 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
1.1 OUR DEPARTMENT - UPAM
A. Locations: I. Wards: K7 North (N) General Paediatrics ward: Infection control/ Isolation ward Haematology and Oncology (HOI) ward Neonatal Intensive Care unit (NICU) and Special Care Baby unit (SCBU) South (S) General Paediatrics ward: Infection neutral ward Paediatric Ambulatory Day Center (PADC) Paediatric Intensive Care unit (PICU)
K8 K10
D4: Paediatric Cardiology wards (General) E5: Paediatric Cardiology ICU II. Out-patient Clinic: in K block, Ground floor III. UPAM Office: in 1/F, New Clinical Building B. Admission policy 1. According to age : Day 0 to 1 month old: NICU/SCBU 1 month to 18 years old: general ward K7 2. Direct admission without going through A&E: to be arranged with team head on call
C. Departmental Meetings and educational activities
The following departmental meetings are held in 1/F, New Clinical Building: Journal Club: Monday 12:45pm (Seminar Room) Grand Round: Thursday 8:30am (Seminar Room) History Meeting: Friday 12noon (Conference Room) Each specialty area will have their own specialty meetings and ward rounds.
__________________________________________________________________________________
- 6 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
1.2 GENERAL INSTRUCTIONS TO INTERNS AND RESIDENTS
1. Good medical care Make the care of your patient your first concern. Be considerate in handling sick
children. Minimize the number of painful procedures by careful organization of investigation and treatment and perfection of skill in carrying out such procedures. Don't be over-persistent in repeating venipunctures. Avoid separation from parents. Talk and explain to the parents. Good rapport is important for good treatment outcome.
1. Develop your clinical competence in dealing with common paediatric problems "Common sense" need Be the first line of defense. Prioritize your work. Attending to a sick child is your first priority. Technical/practical skills: start with supervision (refer to log sheet of clinical procedures) Discuss with senior in case of doubt. 2. Develop good communication skills. With patients and parents: be sensitive to their needs. Listen and give appropriate information. With fellow colleagues: "coverage at the same level". Handover ill cases/unfinished procedures to intern on call. With seniors: report any significant clinical/laboratory findings once spotted; report problems with parents; confirm whether your decisions made were appropriate. With nursing staff: discuss with nurses on patient management and procedures with patience and courtesy. With referring doctors and doctors from other department: be courteous. Tell your team head or supervisor of any grievances or conflicts early. Remember that quality patient care is achieved through collaborative teamwork. 3. Always respond to calls promptly. 4. Recognize ones own limitations and know when to seek advice. 5. Maintain good medical practice by continuous learning Evidence-based practice : understand the relevance of evidence to support patient care Keep your professional knowledge and skills up to date 6. Be honest and open and act with integrity.
__________________________________________________________________________________
- 7 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
1.3 ORIENTATION TO MEDICAL STAFF IN HKWC
Please refer to the Orientation Handbook for Medical staff in the HKWC website (Click : Cluster Department Information Human Resources Services Centre Orientation & Induction Program for New Staff member of HKWC) (http://hkwc.home/Cluster_Department_Info/HR/Docs/Q&I/2009/Medical%20Staff%20Handbook.pdf) On the following topics: 1. Specialist led and clinical services 2. Good partnership with patients and complaints management 3. Quality clinical practice 4. Clinical management system 5. The management of medical records & proper documentation 6. Discharge summary and coding 7. DNR policy 8. CPR policy 9. How to deal with DAMA 10. Clinical audit 11. Potential medico-legal situation 12. Reportable deaths under coroners ordinance 13. Crises management and disaster plan 14. Infection control 15. Intern orientation & training 16. Core competencies for medical officers/residents 17. Rules & regulations for using houseman quarters at QMH
__________________________________________________________________________________
- 8 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
1.4 GOOD CLINICAL DOCUMENTATION AND CASEMIX
Good clinical documentation Clinical information should be documented accurately, consistently & comprehensively to reflect the patients condition & the treatment given Documentation of the Principal Diagnosis Documentation of Secondary Diagnoses Documentation of Principal & Other Significant Secondary procedures performed When assigning these using ICD9CM codes be specific As vague & missing diagnosis & procedures may lead to a lesser DRG assignment Which does not reflect the complexity of the patient cohort you are treating & Leads to fewer resources being allocated to the cluster Casemix refers to the number and type of patients treated by a hospital Output is generally grouped according to a classification such as Diagnosis Related Groups (DRGs) DRGs are used to classify patients into clinically meaningful groups based on ICD diagnosis, treatment & operative procedures codes A hospitals DRG profile is typically known as its casemix When transposed to ICD9CM it is the basis of complexity & reimbursement measurement of a hospital Casemix Index A measure of a hospitals casemix complexity CMI = Weighted Episodes (i.e. Cost Weights x Number of Episodes) Number of Episodes Reporting the Principal diagnosis Definition of Principal Diagnosis (from 1 Jan 2001): The condition, diagnosed at/after discharge, which is primarily responsible for the patient's need for treatment or investigation in that episode of hospitalization. The principal diagnosis is always sequenced first It might not be the admitting diagnosis but rather the diagnosis found after work up or surgery that proves to be the reason for hospitalization If there is more than one condition which accounts for the reason for hospitalization, select the most severe condition or the most acute condition If no diagnosis was made, the main symptom, abnormal finding or problem should be selected as the principal diagnosis Example 1 : After investigation, the underlying condition is the principal diagnosis A patient was admitted to hospital for pleural effusion. After investigation, doctors discovered that the patient had lung cancer. Lobectomy of lung was performed immediately Principal Diagnosis Secondary Diagnosis Procedure Lung Cancer Pleural effusion
Example 2: The most complex condition is the principal diagnosis A patient was admitted to hospital for acute appendicitis and peritonitis. Appendicectomy was initially performed. Whilst in hospital, the patient had a heart attack and coronary bypass surgery was performed Principal Diagnosis Secondary Diagnosis Procedures Acute Myocardial Infarction Appendicitis & Peritonitis 1. Coronary Bypass Surgery 2. Appendicectomy
__________________________________________________________________________________
Lobectomy
- 9 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Reporting secondary diagnosis Definition of Secondary Diagnosis: Secondary Diagnoses are those for which the patient received clinical evaluation, diagnostic evaluation, treatment (co-morbid condition), & affected the patient's treatment care plan, and/or increase the length of stay; They might have: Existed at the time of the patient's admission to hospital Developed during the patient's hospitalization; Developed as a complication of the care provided to the patient whilst in hospital Diagnoses that need not be reported as secondary diagnoses: Those that relate to an earlier episode that have no bearing on the current hospital stay Reporting Procedures Definition of Principal Procedure: The most significant procedure that was performed for treatment of the principal diagnosis. Significant Procedures: A significant procedure is defined as one that meets one of the following conditions: Is surgical in nature; Carries a procedural or anesthetic risk; or Requires special facilities, equipment or specialized training. Where procedures are undertaken both as a form of treatment & for diagnostic purposes, the principal procedure is the most significant procedure that was performed for definitive treatment rather than for diagnostic or exploratory purposes. When no procedure was performed for treatment of the principal diagnosis, use the following hierarchy: Procedure performed for treatment of additional diagnoses Diagnostic/exploratory procedure related to the principal diagnosis Diagnostic/exploratory procedure related to additional diagnoses Do not report the procedures which are not done in the reported episode
Extracted from The Importance of Good Clinical Documentation & the Role of the Clinician, Performance Office, HKWC (2010) Reference: HA intranet site see casemix project for more detail
__________________________________________________________________________________
- 10 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
1.5 DISEASE CODING AND COMMON ERRORS IN MAR /MOE
Pitfall in disease coding 1. Diagnostic code and procedure code must be completed for all discharge summaries and to be printed out on or before the day of discharge, including all those Day-patients. 2. Choose the appropriate principle diagnosis and code each disease separately. 3. Pick previous diagnosis if available, for chronic patients e.g. Epilepsy, mental retardation. 4. Code the identified causative organism if possible (double coding). e.g. Upper respiratory tract infection 465.9 Influenza A (Influenza with other respiratory manifestation) 487.1 e.g. Urinary tract infection 599.0 E. coli 041.4 5. For most of the common diseases, use clinical data framework for coding. Be careful about congenital pneumonia. 6. All diagnostic code 800-999 must be accompanied by an E-code. 7. All procedure code must be accompanied by diagnostic code. 8. Code G6PD deficiency with V71.8 and enter the data in the Alert page. 9. Code nursing mother/father/maid with V65.0, minimal requirement for the case summary. 10. Code Isolation status for isolation cases. 11. Use V71.9 as code for observation without treatment for all age group. 12. Useful link in the CMS: http://cs4/mastertable Special point about coding for neonates Remember to code prematurity when gestational age < 36 weeks Code the birth weight when BW < 2500 gm, 765.XX Code inborn V30.00 for those babies born in QMH by pick previous diagnosis Code outborn V30.1 for those babies born in other hospitals
1. 2. 3. 4.
Special point for neonates in K8 Day centre 1. Still need to code V30.00 for inborn and V30.1 for outborn if they are admitted within 28 days or 44 weeks of corrected age 2. Code day-patient V72.9 for those admitted for NNJ assessment, ROP assessment and procedures 3. Those babies admitted for ROP screening, pick previous diagnosis for prematurity, birth weight and inborn/outborn 1. 2. 3. 4. 5. 6. 7. 8. 9. How to arrange S5 follow-up for inborn neonate Check the S5 follow-up date of the mother. Find the babys name in the ward list. Go to the <Out-patient Appointment Booking> window through the ward list. Change the <Specialty> to <OBS Obstetric Clinic>. In the <Subspecialty clinic>, choose <BBNZ Neonatal Assessment S5> Enter the follow-up date, preferably the same as that of the mother. In the box of <Appointment Type>, click <Subsequent>. Then press <Search>. Click <Accept> if the date is appropriate and then <OK>.
__________________________________________________________________________________
- 11 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
Common errors in MOE 1. 2. 3. 4. 5. Wrong dosage Dosage of MDI e.g. Pulmicort 200 ug per puff vs 50 ug per puff Dosage of mixed drugs e.g. Seretide 25/125 vs 25/50 Home leave prescription Be careful of drug names with similar spelling
Common errors in MAR 1. Illegible hand writing 2. Decimal points 3. For drug given once per day, must use daily instead of QD Dr YK Ng October 2010
__________________________________________________________________________________
- 12 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
1.6 INFECTION CONTROL IN PAEDIATRIC WARD
Refer to QMH Infection Control Manual (Access through CMS station at HKWC website home page click icon Infection Control) Own immune status All workers in the pediatric ward have to be immune to varicella, measles, mumps and rubella. Indication for Isolation in K7N All patients admitted to K7N should have an order for Isolation on admission. Patients can be preemptively isolated based on epidemiology and syndromes suggesting certain infectious etiology pending microbiologic confirmation. Standard Precaution Practised in all patients regardless of infective status. Infections include: UTI, bacteremia, gastroenteritis other than those indicated for Contact Precaution, CMV, HIV. All other specific isolation precaution entails Standard Precaution plus that additional precaution if needed. Droplet Precaution Theoretically all children with infections transmitted via the droplet route should be hospitalized in a private room. Since in QMH, the majority of the beds are in open cubicles, droplet precaution in K7N is practiced by having patient beds at least 3 feet apart, no mixing of patients in the ward, and staff and visitors wearing a surgical mask. Examples include influenza, S. pneumoniae, pertussis (although CHP seems to want the child isolated in a single room), Group A Streptococcus, rubella.
Airborne Precaution (negative pressure isolation) Infections spread by airborne (aerosol) route: measles, varicella, disseminated zoster (usually in an immunocompromised host) and TB in a child with 1) cavitary pulmonary TB, 2) positive sputum AFB smear 3) laryngeal involvement 4) extensive pulmonary infection. Contact Precaution Organisms that commonly contaminate large surfaces around the patient or with potentially serious infection control implications, including rotavirus, norovirus, salmonella in a diapered or incontinent child, Salmonella typhi, varicella, scabies, enterovirus, RSV, parainfluenza, adenovirus, MRSA, ESBL. Examples of preemptive contact precaution: a baby with acute bronchiolitis (suspicious for RSV), a child with vomiting and diarrhea in winter (suspicious of rotavirus), a child with vomiting and diarrhea (suspicious of norovirus). These children should be placed in a room or cohorting in a cubicle if there are many patients with the same etiology (e.g. rotavirus gastroenteritis in winter).
Reverse isolation This is indicated for an immunocompromised host to protect the patient from other patients who may be infectious. Patients with transient neutropenia secondary to a viral infection do not need reverse isolation. __________________________________________________________________________________
- 13 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ HEPA filter Bone marrow transplant recipients to prevent spores of filamentous fungi such as Aspergillus. None of the negative pressure rooms in K7N has HEPA filter.
HIV testing: counseling and informed consent Testing for HIV infection carries the risks for discrimination in jobs, school and child care. The parents or guardian and the patient, if old enough to comprehend, should be counseled about the possible risks (as stated above) and benefits (early effective treatment if infected, ruled out infection if not) of testing a child and the consequences of HIV infection. Consent should be obtained from the parent or legal guardian and recorded in the patients medical chart. No signed consent is necessary. Maintaining confidentiality in all cases is essential to preserving patient and parent trust and consent. Since this test creates a lot of anxiety in parents and patients, the results should be given to the parents and patient, if appropriate according to age, as soon as they are available. The turnaround report time for HIV serology is about 1 week and that of HIV RNA is about 2 weeks. Follow up appointments for testing result should be made accordingly. Varicella Outbreak There is a standard template for plan of action that should be prepared when there is an outbreak such as varicella in the ward. (See Appendix for sample.) Contact Infection Control Unit (x3553) Dr. Susan Chiu (through Hospital Operator)
Dr S Chiu Updated October 2010
__________________________________________________________________________________
- 14 -
Manual for Paediatric Interns and Residents 4th edition
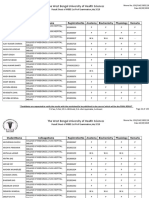
__________________________________________________________________________________ Appendix: Sample of action plan for chicken pox exposure Index patient: CCC Female/ age (ID 1234567) Diagnosis: 1st episode of chickenpox, EBV associated hemophagocytic syndrome 1st day of skin eruption: 17/3 morning 1st day of being infectious: 15/3 morning Background She was admitted to K8N on 5/3 1:00pm for chemotherapy till now. She had been given IVIg (1gm/kg) from 18-20/2, then on IV acyclovir 500mg Q8H since 1/3 for the EBV infection. She did not have any history of chickenpox. She was managed in single/double door room, but she went out of her room for walking exercise during evening. She developed vesicular lesion on 17/3 morning. She was then transferred to K7N for isolation. Microbiologist and ICN informed. Ward arrangement K8 will house the immune and clean cases. K7N isolation room will be used for quarantine patients. Line care and routine blood taking will be done at K8S special room for those under quarantine. Action for patients Mainly for susceptible patients and potentially contacted by the index patient in K8N during period 15/3 to 17/3. They will be given varicella-zoster immune globulin (VariZIG) for 1 dose. They will be put under quarantine for the specified period. The following summarized the data of these patients and quarantine status: Quarantine Remark Name Age Dx History of VZV (ID) chickenpox antibody SJP 5y ALL 25/3-14/4 susceptible LCM KCH YCH 15y 7y 2yr ALL ALL Neuroblastoma 25/3-14/4 25/3- 12/4 27/3- 14/4 susceptible susceptible Susceptible (mother pregnant, pending Ab result)
Immune group: no special action. Name Age Dx History of (ID) chickenpox WHM 11 ALL + KSL 14 Rhabdo + TWT 4 ALL HMY 10 PBMT + HKH 6 ALL + LOK 7 AML +
VZV antibody + + +(vaccine) + +(vaccine) +
Quarantine -
Remark immune immune immune immune immune immune
__________________________________________________________________________________
- 15 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Quarantine period: 25/3 to 12/4 ( + 2days if the last contact is 17/3), inclusive (10 days from first day of contact to 28 days after the last contact. Those who require quarantine and hospital admission will be admitted to K7N isolation. OPD attendance If the patient who require quarantine attend out-patient follow-up, they should be advised to wait outside the OPD clinic rather than coming into the waiting areas. Distribution COS K7 and K8 Team heads and WM KGOPD WM Reported by Dr XXX
__________________________________________________________________________________
- 16 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
Sick Leave recommendation for children with communicable diseases
Disease Acute conjunctivitis Acute poliomyelitis* Bacillary dysentery * Incubation period (days) 1-12 7-14 1-7 Sick leave recommendation Until no abnormal secretion from the eyes At least 14 days from the onset of symptoms Until diarrhoea ceases and stool samples are tested negative for such bacteria (test is to be done on three stool samples collected at least 24 hours apart) About one week or until all vesicles have dried up Until non-infection is confirmed (test is to be done on three stool samples collected at least 1 day apart following 48 hours after the completion of the antibiotic course) Until non-infection is confirmed by negative result on sample culture test (test is to be done on two nasopharyngeal swabs collected at least 24 hours apart following 24 hours after the completion of the antibiotic course) Until all vesicles dry up or as advised by the doctor. If enterovirus 71 is confirmed to be the pathogen, take 2 more weeks of sick leave after all vesicles have dried up Until at least 1 week from the appearance of jaundice or as advised by the doctor 4 days from the appearance of rash Until the completion of the bacteria removal course
Chickenpox * Cholera *
14-21 1-5
Diphtheria *
2-7
Hand, foot and mouth disease Hepatitis A * Measles * Meningococcal infections (invasive)* Mumps * Rubella* Scarlet fever * Tuberculosis * Typhoid fever *
3-7
15-50 7-18 2-10
9 days from the appearance of swelling 7 days from the appearance of rash 5 days from starting the antibiotic course As advised by the doctor Until at least three consecutive stool samples collected no less than 24 hours apart are tested negative for such bacteria (the first stool sample has to be collected 48 hours after the completion of the antibiotic course) Viral gastroenteritis 1-10 Until 48 hours after the last episode of diarrhoea or vomiting Whooping cough * 7-10 5 days from starting the antibiotic course # The recommendation made above is based on the general infection period only. Other factors, such as the clinical conditions of the sick child, have to be considered as well. The attending doctor should exercise his / her professional judgment when making the final decision on the length of sick leave. * Diseases to be reported to the Centre for Health Protection, Department of Health as required by the law. Reference: http://www.chp.gov.hk/files/pdf/School_full_eng_20090115.pdf
12-25 14-23 1-3 Not definite 7-21
__________________________________________________________________________________
- 17 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
1.7 ADMISSION OF PAEDIATRIC PATIENTS
Admission procedure 1. Interns: Attend to admissions immediately when called. Resident should see new admissions within one hour of admission. 2. Identify cases that require immediate isolation e.g. suspected SARS, chickenpox, measles. These should be admitted to the negative pressure rooms in K7N. 3. Take a full history and perform a thorough physical examination. You can use the Template for General pediatric admission on the CMS. 4. Document the time of attendance (e.g. 09:00). Sign and write your name and staff number. 5. Identify any drug allergy and G-6PD deficiency. Enter into CMS Alert. Apply red coloured label onto medical record and drug charts. 6. Write down the name of the referring doctor on the Admission Sheet so that reply letter can be sent for better communication and patient care. Write down the name of your team head in the column "Doctors I/C". 7. Chart the growth parameters. You will be surprised how frequently you pick up abnormalities hitherto unsuspected! 8. Admission of adolescent patient: Fill in the Adolescent Medicine Supplemental History HEADSS. 9. Admission of child abuse cases: Use the Child Abuse Form. 10. Formulate a working diagnosis and manage accordingly. 11. Get help from senior if the child is sick. Medical Orders 1. Write medical orders clearly and legibly. 2. Label each entry with time (e.g. 09:00) and date. Sign properly and write down your staff number or the personal chop provided. 3. An incorrect entry should be cancelled by drawing a single line through it and the order rewritten nearby to avoid confusion. 4. Properly written medical orders should cover the diagnosis and treatment. The following schemes may be used: Diet Dispositions: includes the monitoring of vital signs, weighing the patient, special observations, isolation procedures and permitted activities. Diagnostic tests: Group in logical sequence (e.g. blood and radiographic). Drugs: i. Oxygen ii. Non-parenteral drugs (GREEN MAR form) iii. Parenteral drugs (PINK MAR form) Write clearly on the Medication Administration Record (MAR). Include generic name, dose, route and frequency to be administered and the start date. Note any history of drug allergy and G-6-PD deficiency. (Red label on MAR form). Write "NIL" if there is no history of allergy. Avoid abbreviations and decimal point, e.g. 0.5G should be expressed as 500 mg. The method of underlining the figures after the decimal point is also recommended. (e.g. 1.25 mg). Write "daily" instead of "QD", microgram instead of mcg or ug, units instead of iu. Any change in prescription should involve complete cancellation of whole item and not alternation in part. Drugs should be cancelled by drawing a line through the drug name, signed __________________________________________________________________________________
- 18 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ and dated. Intravenous infusion and drug additives should be prescribed in the MAR. Refer to the Medication Manual from QMH Pharmacy for details on drug information services, 24 hours Emergency Drug Cupboard, procedure guidelines on prescribing, handling of cytotoxic drugs and drug allergy. (Access through CMS Station: Click on QMH intranet > Clinical Information> Drugs> Medication Manual.) Investigations and procedures 1. Explain to the patient and parents clearly and patiently the necessary procedures to alleviate undue anxiety. 2. All procedures should be performed in the treatment room if possible. 3. Allow parents to stay with the child if they request. 4. Minimize the number of painful procedures by good organization of work and perfection of skill. Get help when needed - don't be over persistent. 5. Get the proper specimen/blood samples into the appropriate bottles. It is NOT acceptable that the patient is subjected to another venepuncture because you send the wrong specimen. 6. All laboratory request forms and specimens should be clearly labeled. o o o o Consultation to subspecialty teams and other departments Cardiac assessment for inpatients Contact cardiologist-on-call through paediatric cardiology secretary. Neurology consultation Send the neurology consultation form by fax to Duchess of Kent Child Assessment Centre ( Fax no: 2974 0330) and contact the acute neurology on-call doctor listed in the time-table Consultation to other subspecialties Contact respective subspecialty team heads/fellows by phone. (See time-table.) Consultation to other departments Consultations to other departments should only be initiated after assessment by MO. All urgent consultations should be initiated after discussing with the most senior doctor of the team /on-call.
Category Ultra-urgent Urgent Semi-urgent
Non-urgent Dr A Tsang October 2010
Response time of the department being Your action consulted Within 30 min Inform senior. Call doctor-on-call of other Within 2 hr departments and send consultation form by fax. Within 1 calendar day disregard of Sat, Sun, Send consultation form by fax. public holiday (should only use this during weekends & PH) Within 1 working day
__________________________________________________________________________________
- 19 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
SECTION 2: PROCEDURES IN PAEDIATRICS
__________________________________________________________________________________
- 20 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
2.1 BLOOD SPECIMEN COLLECTION
1. 2. 3. 4. 1. 2. 3. 4. 5. Proper specimen collection Correct patient Correct technique Correct specimen bottles and labeling Correct laboratory request forms/GCR-LRS label Correct method of transport and accurate timing where necessary. Methods of blood specimen collection Capillary puncture (Heel prick) Venipuncture Arterial line Central line Preparing for blood taking Identify patient. Clarify orders and calculate the total volume of blood required. Prepare appropriate specimen bottles and equipment. Informed consent Universal precautions
__________________________________________________________________________________
- 21 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
2.2 CAPILLARY PUNCTURE (HEEL PRICK)
Equipment 1. Gloves 2. Alcohol swabs 3. Sterile gauze pads 4. Sterile lancets Microtainer safety flow lancet with spring loaded and depth control design, suitable for neonate Monolet needle type, for collection of a few drops of blood only e.g. for haemoglucostix Feather blood lancet no safety depth, used with caution 5. Specimen bottles 6. Bandaid Procedure 1. Select the puncture site Heel (neonates and infants) Avoid penetrating the calcaneus by using a lancet puncture smaller than 2.5 mm and by performing the puncture on the medial or lateral plantar surface (shaded area as illustrated). The limits of the calcaneus are defined by two lines, one drawn parallel to the lateral margin of the heel from the space between the fourth and fifth toes and the other drawn parallel to the medial margin of the heel from the center of the great toe. Avoid the bottom of the heel. Avoid site of infection and edema Choose the warm and well-perfused foot. Warming the extremity or placing it in a dependent position may facilitate specimen retrieval. The maximum volume of blood collected is about 1.5ml. 2. Disinfect puncture site with alcohol swab. Allow to air dry. 3. Grasp the heel; slightly occlude the veins by flexing the ankle. 4. Puncture skin with sterile disposable lancet placed perpendicular to the plane of the heel. Make a clean, superficial and small cut. DO NOT rotate or make a cross with the lancet. 5. Wipe away the initial drop of blood with dry gauze. Massage to express blood, allowing enough time for capillaries to refill. Collect subsequent drops in a microtube. Avoid air getting into the sample tube as this will affect air venting and blood flow. 6. DO NOT squeeze the wound as this alters blood composition and invalidates test values. 7. You can improve the blood flow by flexing the ankle. by wiping away the clotted blood on the puncture wound. 8. After finishing blood collection, press the wound with dry gauze to stop bleeding. Cover with Bandaid. Make sure that bleeding has stopped before leaving patient. 9. Tidy up the place. Put lancet to sharp box. 10. Label specimen properly. Send specimen away with appropriate forms and bags. Dr YK Ng Reviewed 2010 __________________________________________________________________________________
- 22 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
2.3 BLOOD TAKING FROM CENTRAL VENOUS CATHETER
K8 HICKMAN CATHETER BLOOD TAKING
(non-touch sterile technique)
Purpose: To draw blood from Hickman Catheter with safe and effective method. ** Wash hands before& after procedure. Sterile items, close system. Very careful for critical area. "Clamp Here". No pulling. No scissors. Use of a 10ml or larger syringe is recommended. Blood culture from red lumen, white lumen, peripheral site. Blood for clotting profile: E.g. discard 3ml blood, take 1.5ml for CBP, LRFT, then another syringe 2ml for clotting Use betadine for blood culture, TPN. Check with staff of K7, K10.
Equipment Alcohol wipe 70% (3+3+1+1). Gloves for Standard Precaution. Heparinized saline 50 units / 5ml. Two different size syringes: one syringe to discard blood, one syringe for blood sampling. Two 10 cc syringes - one for flushing l ml Heparinized saline, then one for flushing 4ml Heparinized saline (in paediatric). Jelco to block the line or sterile needle to cap the IV tubing tip. Blood bottles. Patient labels. Procedure
1. CHECK PATIENT INDENTITY. Wash hands thoroughly with antimicrobial soap and water. 2. Prepare all items in a big tray. Draw up heparinized saline in 10ml syringes. Wear gloves. 3. For continuous infusion: Stop all IV drip, clamp another lumen to avoid the blood result
interference with the IV infusion. e.g. TPN, dextrose, electrolyte. (Press RESET Lifecare pump).
4. Swab the catheter junction with Alcohol wipe vigorously with friction for 3 times. Allow the
antiseptic to air dry. Ensure that the smooth-edged clamp of the catheter is closed.
5. Disconnect the luer lock cap / IV tubing. Cap the IV tubing end with new needle. Swab the hub
thoroughly with Alcohol wipe vigorously with friction for 3 times. Allow the antiseptic to air dry. Connect an empty 5ml syringe.
6. Release the clamp, aspirate 3ml blood to clear the catheter. (2 ml for neonate, re-infuse later). 7. Connect another syringe, unclamp the catheter, and draw the blood sample. 8. Clamp the catheter and change 1 ml heparinized saline syringe to flush the catheter. Then clamp
it. Alcohol wipe swab hub.
9. Release the clamp and inject the heparinized saline 4 ml into the catheter. (Create turbulent) 10. Clamp the catheter while flushing the last 0.5ml heparinized saline, to maintain positive pressure. 11. Close the clamp and remove the syringe. Alcohol wipe swab hub, and allow the antiseptic to air dry.
Connect a new injection cap to the end of catheter, or to connect with infusion tubing.
12. For continuous infusion, OPEN the catheter clamp first. To prevent accidentally rupturing of the
catheter by infusion pump. (Check drip rate if applicable. Press START.).
13. Secure the catheter to the position to patients chest.
__________________________________________________________________________________
- 23 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
14. Mix blood well inside the syringe. Then put the blood sample into appropriate blood bottles and mix
well with the medium immediately. Label specimen and send with lab form. Document in patient's record. Ms SY Chiu 2004
__________________________________________________________________________________
- 24 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
2.4 PRE-TRANSFUSION COMPATIBILITY TEST IN NEONATES CROSS MATCH
1. Four-months rule Apply to all babies up to 4 months of age Both mothers and babys blood samples are required for the first cross-match process If maternal antibody screening is negative, no further sample is required for subsequent transfusion up to the age of 4 months 2. Babys blood sample The minimal volume is 0.8-1 ml of clotted blood for babies less than 4 months If maternal blood is not available, 1.5-2 ml of blood is needed and inform blood bank Enter <Investigation Request> with GCRS blood bank module in the CMS, enter mothers name and ID Print out the job sheet and generate the 2-D barcode label Write mothers name, mothers ID, the blood sampling date and sign your name on the label; remember to sign on the job sheet after blood taking and put on the date Special arrangement required for unmatched blood, urgent whole blood for exchange transfusion Essential information for <paper request form>: Name as B/O . ID number Hospital number Sex / Date of birth Ward / Bed number Mothers name Mothers ID number Name of doctor taking the blood Staff number Signature Date of blood sampling
3. Mothers blood sample Scenario 1: mother as in-patient in OBS unit of QMH - Process cross-match with GCRS Scenario 2: mother as in-patient in another hospital - Process cross-match with <paper request form> - Double check the mothers name and ID number, special attention to the blood sample provide - Cross-match form preferred to be filled by referring hospital, do not accept GCRS form from another HA hospital Scenario 3: mother accompanies the baby - Process cross-match with <paper request form> - If other just recently discharged from QMH OBS unit, can check with blood bank if mothers blood is needed, special attention to mothers ID number, is it UN or passport number Scenario 4: mother not available - Special arrangement with blood bank Dr YK Ng October 2010
__________________________________________________________________________________
- 25 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
2.5 URINE EXAMINATION
1. 2. 3. Principles Urine examination should be done by interns in indicated cases. All infants and young children with febrile illness without localizing source should have urine screened as early as possible. All urine cultures should be sent to the laboratory within 20 minutes of collection. Method of urine examination Urine that has been standing for > 1 hour is best discarded. Uncentrifuged, well-mixed urine should be examined using a counting chamber. Routine chemistry with multistix. Procedure Guides of Using Counting Chamber in Urine Examination The counting chamber and cover glass should be cleaned before use. a. How to fill the counting chamber Sliding on the cover glass The external supports are moistened with water and the cover glass is gently pushed onto the counting chamber from the front (see Fig. 1). Check the cover glass in correct position by the formation of interference lines (Newton rings) between the external support of the chamber and the cover glass.
External supports
Fig. 1
Interference lines
Caution! The cover glass is fragile!
Feeding Draw few drops of well mixed urine sample using a disposable plastic pipette. Wipe the pipette and hold it at an angle until the tip is placed between the cover glass and the counting chamber as indicated in Fig. 2. The urine between the cover glass and the chamber is filled up by capillary action. Before the overflow of urine at the edges of the chamber, the tip of the pipette must be removed. The chamber must be cleaned and re-fed if air bubbles are seen in the chamber or urine overflows Fig. 2 into the grooves.
Possible sources of error: The counting chamber is not clean The cover glass is not placed correctly onto the chamber The chamber is not filled free of bubbles The chamber is overfilled There is not enough time for sedimentation of the urine particles
b. How to clean the counting chamber Immerse the counting chamber and the cover glass into a 10% Clorox solution for 10 minutes for disinfection. Discard the Clorox solution and then rinse the cover glass and counting chamber with tap water. Dry the cover glass and chamber with soft tissue or kimwipes and return it to the box.
__________________________________________________________________________________
- 26 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Using a counting chamber (Improved Neubauer Counting Chamber)
1 mm
1 mm
3 mm
1 mm
Depth = 0.1 mm
There are 9 large squares and each square is 0.1 ul in volume. Therefore, the total volume of 9 squares is 0.9 ul. Use 40x amplification to identify cells morphology. Use 10x amplification for counting. Count all 9 large squares and calculate as follow:
Number of cells ----------------------------------- = cells per ul 0.9 Dr S Chim Reviewed October 2010
__________________________________________________________________________________
- 27 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
2.6 URINARY BLADDER CATHETERISATION
Indications 1. to obtain urine for urinalysis and culture sterilely 2. to monitor urine output 3. for voiding cystogram Complications 1. trauma to urethra or bladder 2. vaginal catherisation 3. infection 4. intravesical knot of catheter ( rarely occurs, but it has happened!) Procedure 1. Prepare the urethral opening using sterile technique. 2. Lubricate the catheter. 3. In boys, gently retract the foreskin. If it cannot be fully retracted, follow the general guideline that the urethra is on the ventral side of the penis. Slide the catheter along that track. Apply gentle traction to the penis to straighten the urethra. Slowly advance the catheter until resistance is met at the external sphincter. Continued pressure will overcome this resistance and the catheter will enter into the bladder. Insert a few cm longer than the shaft of the penis. 4. In girls, labial traction (gentle grasping of the labia and pulling towards you) allows better visualization of the introitus than labial separation. The vaginal opening is more pronounced than the urethral opening. The urethral opening is slightly superior to the vaginal opening. ( Figure 1) Advance the catheter for a few cm to reach the bladder. 5. Carefully remove the catheter once specimen is collected.
Figure 1
Dr A Tsang October 2010
__________________________________________________________________________________
- 28 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
2.7 LUMBAR PUNCTURE
Equipment 1. Sterile gloves 2. Povidone-iodine 3. Lumbar puncture set: Sterile drapes, cotton wool swabs, sterile gauze, sterile collecting tubes 4. Spinal needle Spinal needle size by age Premature infant 22 gauge or smaller, 1.5 inch, plastic hub preferred Neonate 2 year 22 gauge or smaller, 1.5 inch, plastic hub preferred 2 12 years 22 gauge, 2.5 inch > 12 years 20 or 22 gauge, 3.5 inch 5. Manometer separate sterile set to be added and assembled for measuring opening pressure Procedure 1. Informed consent (Pamphlet explaining the procedure available in the ward) 2. Prepare the child for the procedure and apply EMLA. 3. A key component of a successful lumbar puncture is adequate restraint of the patient. Get a good assistant. 4. Place the patient either in the sitting position or in a lateral recumbent position with the head flexed, knees drawn up to the abdomen and back arched. This helps to increase the space between the lower lumbar vertebrae. DO NOT compromise infants cardiorespiratory status by positioning. Monitor the heart rate, respirations and oxygen saturation during procedure especially in neonates, young infants and children with any degree of cardiorespiratory compromise. 5. Palpate the upper aspect of the posterior superior iliac crests. The imaginary line joining the iliac crests intersects the midline just above L4. Identify the interspace between the L3 to L4 and L4 to L5 and one site is chosen for puncture. 6. Aseptic technique 7. Cleanse the site thoroughly with povidone-iodine. Allow to air dry. Drape the surrounding area with sterile towels. 8. The selected interspace is palpated with the sterilely gloved forefinger. Insert the spinal needle with stylet through the skin between the spinous processes. Lateral recumbent position - Angle the needle about 15 degrees cephalad towards the umbilicus, keeping it level with the mid-sagittal plane of the body. Bevel of needle is placed horizontally so that dura mater is pierced parallel to its fibers. Sitting perpendicular to skin (slightly cephalad), bevel of needle held vertically 9. Advance the needle slowly, removing the stylet frequently to check for cerebrospinal fluid (CSF). If you hit the bone, withdraw the needle slightly and change its angle. In a median puncture, the needle punctures through the following structures (in order): skin, subcutaneous fat, supraspinal ligament, interspinal ligament, ligamentum flavum, dura mater and arachnoid mater into the subarachnoid space. There is a slight pop felt as the spinal needle penetrates the dura. In infants, a pop may not be felt and the spinal needle should be advanced approximately 1 to 2 cm. 10. Once in the subarachnoid space, CSF will flow freely. If necessary, connect to manometer to measure the CSF pressure. Have the patient straighten the legs and __________________________________________________________________________________
- 29 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ relax so as not to artificially elevate the opening pressure. 11. Collect the smallest volume of CSF necessary, controlling the rate of flow of CSF with the stylet. Allow the CSF to drip into collection tubes for diagnostic studies. If CSF does not flow, rotate the needle 90 degree. If rotation of the needle does not result in CSF flow, replace the stylet and advance a little farther. 12. Once you have obtained enough CSF, replace the stylet and withdraw the needle. 13. Apply a small sterile dressing to the puncture site. 14. Label the tubes properly and deliver to laboratory immediately. 15. Record procedure start and completion times, patients status, CSF appearance, and CSF pressure readings. 16. The patient should lie prone (flat or horizontal, or on the abdomen) for approximately 4 to 8 hours. Observe for neurologic changes such as altered level of consciousness, change in pupils, change in temperature, increased blood pressure, irritability, and numbness and tingling sensations, especially in the lower extremities. 17. Check the puncture site for leakage. 18. A traumatic tap occurs when the needle penetrates the dura too far to one side into an epidural venous plexus or when the needle is advanced through the subarachnoid space into or adjacent to the vertebral body. If blood is seen during fluid collection but the spinal needle is in proper position, the CSF will usually clear and the specimen does not clot. If the body fluid does not clear and clots in the specimen bottle, the spinal needle is in the wrong position and should be removed. Contraindications 1. Local lumbar skin infection 2. Raised ICP (except pseudotumor cerebri) 3. Supratentorial mass lesions (evaluate by CT scan first) 4. Severe bleeding diathesis (relative contraindication) 5. Platelet count < 50,000/mm3
Dr A Tsang Reviewed October 2010
__________________________________________________________________________________
- 30 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
2.8 MANTOUX TEST
(Extracted from Mantoux test do it the right way by the Centre of Infection HKU)
available at http://www.hku.hk/hkucoi
Procedure 1. Observe universal precautions. 2. Draw up 0.1 ml Tuberculin PPD RT23 into a 1ml syringe. [Each 0.1ml of PPD RT23 contains 2 tuberculin units(MT2) which is equivalent to 5 tuberculin units of PPD-S (MT5)]. 3. Cleanse the skin on the volar aspect of the mid-forearm with alcohol and allow to dry thoroughly. 4. Stretch the skin taut. 5. Hold the syringe at 10-15 degree to the skin and introduce the needle just below the epidermis (about 2mm). Inject the tuberculin into the intradermal skin layer to produce a well-defined bleb of 6 to 10 mm in diameter. If the bleb is <6mm, repeat the process 2.5cm from the first site. 6. Document the time and site of test in the patients record. 7. Read the test results in 48 to 72 hours. Measure the size of the induration. Disregard erythema. Rub a finger lightly from the normal skin area to the indurated zone and mark the zone of induration. Measure the diameter in millimeters perpendicularly to the long axis of the forearm. DO NOT just write down positive or negative. 8. Document the result (report on the size of the induration) in the case record (and the CMS).
__________________________________________________________________________________
- 31 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
2.9 SEDATION FOR PROCEDURES
Admission Protocol for Sedation and Diagnostic procedures in K8 Day ward 1. When arranging the diagnostic procedure for the patient, also assess his/her risk for sedation. 2. Inform parents about the risk of sedation and the risk of the procedure; prescribe steroid for steroid cover if necessary. 3. The parent-ward booking the procedure will inform patient of the appointment when it returns; instruct on the duration of fasting and advise on sleep deprivation. 4. When sedation under GA is required, followed the instruction for consultation to Paediatric anaesthetist. 5. On admission to Day ward, approach by nursing staff; confirm patients identity, procedure and appointment. 6. Confirm time of last meal and drink. 7. Document admission condition, vital signs, measure body weight and body height. 8. Evaluation screening with medical history and focused examination of all patients by interns. 9. Assess the patient risk by a trained resident; to decide on the sedation to be used and degree of monitoring required. 10. Obtain informed consent for the procedure, explained the risk of the procedure. 11. Also explain possible risk of sedation and provide parents with the sedation leaflet. 12. Indicate special point for care on patient record to staff of RD, such SpO2 limits for cyanotic heart patients. 13. Intern will prescribe antibiotic cover and oral sedative drugs under supervision of the trained resident; dosage should be cross-checked by nurse. 14. He will set up intravenous block as necessary. 15. Check if steroid cover has been prescribed and taken for indicated patients. 16. Prescribe iv fluid if prolonged fasting is expected, especially for neonates. 17. Prescribe iv fluid bolus as requested for respective investigations. 18. Check and document vital signs and oxygen saturation of those low risk patients after oral sedation given. 19. Check again and document before transport to diagnostic departments. 20. Advised to have continuous oxygen saturation monitor for all sedated patients. 21. All moderate and high risk sedated patients will also have ECG monitored continuously and documented. 22. Set and check appropriate alarm limits and alarm volume for the monitors during transport. 23. When oral sedation failed, the first 2 doses of iv Midazolam will be given by radiologist. 24. RD will inform the ward when iv sedation has been given; ward will prepare nurse to escort patient back from RD with appropriate monitor and resuscitation kit. 25. RD will inform the ward if their attempt of iv sedation fails. 26. The ward should inform the resident for further sedation, who shall attend RD as soon as possible.
__________________________________________________________________________________
- 32 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ 27. The choice of further sedation will depend on: i. The accumulated dose of iv Midazolam given. ii. The time laps after the last dose of iv Midazolam. iii. As 2 doses of Midazolam had been given by the radiologist, cautious in prescription of further doses unless the dosing interval is long enough, otherwise it is advised to use iv Ketamine. iv. Postpone the procedure if adequate sedation cannot be achieved. v. Put the patient on continuous monitor and consider escalation to the next line of sedation. 28. Contact the resident for any adverse effect related to the procedure and activates emergency pager when resuscitation is necessary. 29. Document the adverse events and resuscitation process. 30. Set and check appropriate alarm limits and alarm volume for the monitors during recovery. 31. Continue the observation and documentation of vital signs, oxygen saturation and conscious state till patient fully conscious and alert or return to his/her usual neurological state. 32. Assess the patient, document the discharge condition when they meet the criteria. 33. Instruct on post-sedation home care with information leaflet.
One trained resident will be assigned to K8 Day ward on TUE am, WED am and THU pm to cover the regular Paediatric RD sessions.
__________________________________________________________________________________
- 33 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
Allocation of Sedation Risk
I. High risk patients (ASA class III or above) a. Systemic illness - Poorly controlled asthma. - Poorly controlled seizure. - Poorly controlled gastro-oesophageal reflux. - Liver or renal impairment. b. Compromised cardiopulmonary status - Congestive heart failure. - Chronic lung diseases. - Premature babies with residual cardiopulmonary problems. - Patients on supplementary oxygen. - Patients require assisted ventilation; include IPPV, BiPAP and CPAP support. c. Airway problems - Severe snoring, obstructive sleep apnoea. - Unable to handle own oral secretion at baseline. - Difficult airway management: atypical anatomy, airway abnormalities. d. Difficult sedation - Children with neurological problems, e.g. Hyperactivity, mental handicap. - Past history of failed sedation or required third line sedation medication. - Past history of adverse effect with sedation. II. Moderate risk patients (ASA class II) a. b. c. d. e. f. Term babies with PCA less than 44 weeks. Premature babies with PCA less than 60 weeks. Patients with mild systemic diseases under control. Failed sedation with full dose oral Chloral hydrate and required iv sedation. Patients require iv sedation. Minor adverse reaction to sedation; e.g. body rash, nausea and vomiting.
III. Low risk patients (ASA class I) a. Patients without the above mentioned risk factors. b. Patients sedated with oral Chloral hydrate only and without airway compromise.
__________________________________________________________________________________
- 34 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Table 2 American Society of Anesthesiology(ASA) Classification of Physical Status Class I II Description A normal health person A patient with mild systemic diseases (No functional limitation) A patient with severe systemic disease (Definite functional limitation) A patient with severe systemic disease that is a constant threat to life A moribund patient who is not expected to survive without the operation Patient requires emergency procedure Risk Low Moderate
III
High
IV
High
High
High
1. Only low risk and selected moderate risk patients can be admitted to day ward for procedural sedation and analgesia. a. Healthy neonates with PCA > 44 weeks and premature babies with PCA > 60 weeks and who are oxygen independent. b. Asthmatic patients with satisfactory control. c. Epileptic patients with satisfactory control. d. Healthy children require first line iv sedation. 2. The other moderate risk and high risk patient are advised to have the procedure as in-patient. 3. High risk patients that may indicate consultation to anaesthetist and GA session for procedures: a. b. c. d. e. f. g. h. Difficult airway, airway malformations. Intractable convulsion. Required assisted ventilation. Neuromuscular diseases. Require prolong sedation. Difficult sedation such as hyperactivity. History of failed sedation with third line sedatives. History of adverse effect with sedation.
__________________________________________________________________________________
- 35 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
Pharmacological intervention
1. Pharmacological intervention for painless procedures a. Neonates: Single dose: Chloral hydrate 50 mg/kg oral 30 minutes before examination. Reduced to 20-30 mg/kg for at risk or premature neonates. Consider to be high risk patient when oral sedation fails. b. Children < 8 years: Chloral hydrate 75 mg/kg oral 30 minutes before examination. First line: A top up dose of 25 mg/kg oral after 30 minutes. Maximum total dose 100 mg/kg or 2 grams. Second line: Midazolam 0.1 mg/kg slow iv. Titrate and repeat doses of 0.1 mg/kg after 2-3 minutes; Up to maximum total dose of 0.4 mg/kg or 5 mg. Ketamine 1-2 mg/kg iv. Third line: Addition boluses of 1 mg/kg after 10 minutes; Up to maximum total dose of 2-4 mg/kg iv. Prefer to have pre-medication with Atropine 0.01-0.02 mg/kg iv 2 minutes before Ketamine injection. c. Children > 8 years: Midazolam 0.1 mg/kg slow iv. First line: Titrate and repeat doses of 0.1 mg/kg after 2-3 minute; Up to maximum total dose of 0.4 mg/kg or 10 mg. Second line: Ketamine 1-2 mg/kg iv. Addition boluses of 1 mg/kg after 10 minutes; Up to maximum total dose of 2-4 mg/kg iv. Prefer to have pre-medication with Atropine 0.01-0.02 mg/kg iv 2 minutes before Ketamine injection.
2. Pharmacological intervention for short painful procedures a. Ketamine 1-2 mg/kg iv; Addition doses of 1 mg/kg after 10 minutes; Up to maximum total dose of 2-4 mg/kg iv. Prefer to have pre-medication with Atropine 0.01-0.02 mg/kg iv 2 minutes before Ketamine injection. OR b. Ketamine 2-4 mg/kg im. Do not repeat the dose if it fails as the first im dose is expected to have prolonged sedative effect. OR c. Midazolam 0.1 mg/kg iv in addition to Local Anaesthetic infiltrate. OR d. Fentanyl 1 microgram/kg iv, maximum 50 microgram/dose; Titrate with Midazolam 0.05-0.1 mg/kg iv. Addition doses after 3 minutes.
__________________________________________________________________________________
- 36 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ 3. Pharmacological intervention for prolonged procedures a. Ketamine 1-2 mg/kg iv and Midazolam 0.05 mg/kg; Addition doses of Ketamine 1 mg/kg after 10 minutes; Up to maximum total dose of 2-4 mg/kg iv. Prefer to have pre-medication with Atropine 0.01-0.02 mg/kg iv 2 minutes before Ketamine injection. OR b. Fentanyl 1 microgram/kg iv, maximum 50 microgram/dose, Titrate with Midazolam 0.05-0.1 mg/kg iv. Addition doses after 3 minutes.
Dr YK Ng Updated Oct 2010
__________________________________________________________________________________
- 37 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
2.10 STEROID PREMEDICATION IN RADIOLOGICAL INVESTIGATIONS
Indications 1. History of drug allergy 2. History of seafood allergy 3. Asthma on long term oral steroid for control Children who are wheezing (i.e. poorly controlled asthmatic) on the day of the intravenous contrast examination and the procedure cannot be postponed However, asthmatics on ventolin or inhaled steroids and on short course (i.e. high dose for a few days) of oral steroids DO NOT merit oral steroid pre-medication 4. Previous contrast reaction 5. ? cardiac diseases All patients with previous contrast reaction should be admitted and observed for 24 hours after contrast study. For children at risk of allergic reactions, please discuss with radiologists to see if there are any alternatives to the contrast study. Corticosteroids are not effective if given less than 6 hours before contrast media injection. Therefore under an emergency situation, the efficacy of steroid premedication is questionable. The examination should not be withheld just solely based on the need for a delay of 6 hours after IV steroid injection but rather after careful consideration on the benefits versus risks issues.
Relative contraindications 1. Diabetes mellitus 2. Acute tuberculosis 3. Acute leukaemia and lymphoma (suspected tumour lysis syndrome) 4. Compromised immune system 5. Systemic fungal disease or other systemic infection 6. Peptic ulcer disease or diverticulitis within the past year Consult respective subspecialty teams if patients have above relative contraindications.
Recommendation for oral steroid premedication Methylprednisolone 0.8mg/kg po, rounding up to the nearest 4mg tablet (maximum 32 mg) OR Prednisolone 1mg/kg po (max 40 mg) at 12 hours and 2 hours prior to IV contrast
Recommendation for IV steroid premedication Hydrocortisone 4mg/kg IV (maximum 200mg) 6 hours before contrast study and 2mg/kg 6 hourly for 2 doses after contrast study
__________________________________________________________________________________
- 38 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Glucocorticoid comparison Agent Equivalent Route of Dose Administration (approx. mg) IM intramuscular IV intravascular PO per oral 0.6-0.75 IM, IV, PO 0.75 IM, IV, PO 20 IM, IV, PO 4 IM, IV, PO 5 PO 5 PO Relative Anti-inflam matory Potency 20-30 25-30 1 5 4 4 Relative Mineralocorticoid Potency 0 0 2 0 1 1 Biologic al Half-life (hours) 36-54 36-54 8-12 18-36 18-36 18-36
Betamethasone Dexamethasone Hydrocortisone Methyl-prednisolone Prednisolone Prednisone
Extracted from Use of steroid premedication COC (Radiology) HA 2002.
__________________________________________________________________________________
- 39 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
2.11 PREOPERATIVE FASTING REGIMEN FOR PATEINTS REQUIRING ANAESTHESIA
(Extracted from Guidelines for preoperative fasting, COC in Anaesthesiology, available online: Click HA intranet Home page> Manuals/Guidelines> Clinical Manuals>Anaesthesiology >Preoperative fasting) For all elective patients requiring anaesthetic care who are NOT at increased risk of pulmonary aspiration: 1. Break the nil by mouth (NPO) after midnight rule. 2. Implement 2-4-6-8 rule for children under 3 years of age Clear fluids include water, fruit juices without pulp, and carbonated beverages up to 10ml/kg can be taken 2 hours prior to operation. Breast milk can be taken 4 hours prior to operation Solid food (including milk/ jelly) can be taken 6 hours prior to operation Fatty food can be taken 8 hours prior to operation. 3. Implement 2-6-8 rule for adults and children above 3 years of age For morning session, no food after midnight. Clear fluid allowed up to 2 hours prior to operation. Clear fluids include water, fruit juices without pulp, carbonated beverages, clear tea and black coffee. Clear fluid should not include alcohol. Only clear fluids allowed between 2 to 6 hours before anaesthesia. For afternoon session commencing after 13:00, light breakfast at 7am. Light breakfast includes either a toast without butter or rice porridge without meat. Clear fluid is allowed up to 11:00, or 2 hours before scheduled time of operation 4. No fluid allowed within 2 hours before anaesthesia except for oral premedications with sips of water. 5. Start IV fluid if operation schedule is unpredictable or fasting period is expected to be longer than 12 hours for a whole day list.
__________________________________________________________________________________
- 40 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
2.12 CARDIAC PULMONARY RESUSCITATION
Successful resuscitation depends on establishing adequate circulation and ventilation before irreparable cerebral and cardiac damage has occurred. Every medical staff must be able to perform external chest compression (ECC) and artificial ventilation. Immediate steps: GET HELP. Call senior. CPR hotline (ext 3333) should be activated by bedside staff. 1. Maintain AIRWAY (clear mouth & pharynx, lift chin up & forward, oropharyngeal airway) 2. Maintain BREATHING (face mask bagging with 100% O2 is effective in most condition, do not hurry with intubation especially if you are not competent) 3. Maintain CIRCULATION (ECC) The following steps should take place simultaneously: 1. Note time of arrest. 2. Attach ECG & SaO2 monitoring. 3. Diagnose rhythm - asystole, VF, electromechanical dissociation (EMD). 4. Establish vascular access for drugs & fluids - IV/ intraosseous(IO). 5. Give appropriate drugs according to rhythm. 6. Asystole : adrenaline (1:10,000) 0.1 ml/kg IV / IO or 0.1 ml/kg of 1:1000 ET 7. VF : DC shock 2 J/kg 8. EMD : adrenaline as above 9. Other drugs 8.4% Na HCO3 1 ml/kg 10% Ca gluconate 0.5 ml/kg
__________________________________________________________________________________
- 41 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
2.13 MANAGEMENT OF ANAPHYLAXIS
Any symptoms of systemic reactions Upper airway obstruction Bronchospasm Hypotension Urticaria following an injection or ingestion of an antigen must be considered as potentially serious. Treatment 1. 100% oxygen (4-6L/min). Call senior. 2. Adrenaline 1:1000 0.01 ml/kg IM or SC (max 0.3 ml ). Repeat Q5 min. IM route more preferred. 3. Establish airway. May need ET intubation/ cricothyroidectomy. 4. Secure IV access. Monitor BP/P, perfusion. If hypovolaemic, give 20 ml/kg NS or Haemaccel. Consider adrenaline or dopamine drip if hypotension persists despite volume replacement. 5. If appropriate, apply venous tourniquet proximal to site of entry of antigen. Contraindicated in snake bites. 6. Diphenhydramine 2 mg/kg IV/IM 7. If there is evidence of lower airway obstruction, add loading dose of IV aminophylline (5 mg/kg) slowly and begin continuous infusion (0.6 -0.8 mg/kg/hr), together with nebulised Salbutamol. 8. Systemic steroid - not effective in emergency management, but useful after the initial manifestations of anaphylaxis.
Dr HK Ho Updated Oct 2010
__________________________________________________________________________________
- 42 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
SECTION 3: COMMON PAEDIATRIC PROBLEMS
__________________________________________________________________________________
- 43 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
SECTION 3.1: RESPIRATORY SYSTEM
__________________________________________________________________________________
- 44 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.1.1: MANAGEMENT OF CHRONIC ASTHMA
Long term management of Asthma General principles: 1. Avoid provoking factors where possible. Parents should be advised to QUIT smoking (smoking cessation hotline information available in KGOPD clinic) 2. Patients and parents involvement and education 3. Selection of best inhaler device with consideration of the type and dosage of inhaled steroids used 4. Treatment stepped up as necessary to achieve good control 5. Treatment stepped down if control of asthma good 6. Choose the step most appropriate to the initial severity of patients, aiming to abolish symptoms and to optimize peak flow soon as possible Management plan STEP 1 Mild intermittent asthma STEP 2 Regular preventer therapy should be consider for any of the following: using inhaled 2 agonists > 3x / week; symptomatic 3x / week; waking 1 night / week; in adults and children aged 5-12 who have had an exacerbation requiring oral corticosteroids in the last 2 years
Inhaled short-acting beta-2 agonist as required Add inhaled steroid 200-400 mcg per day* or leukotriene receptor antagonist if inhaled steroid cannot be used (for children aged < 5 years) Start at a dose of inhaled steroid appropriate to severity of disease for children >12 years - 400 mcg / day 5-12 years - 200 mcg / day < 5 years - higher doses may be required if there are problems in obtaining consistent drug delivery Start with twice daily dosing, can be considered to once daily dosing with good control 1:1 ratio should be assumed when changing between beclomethasone dipropionate (BDP) and budesonide and half the dosage for fluticasone insufficient response
STEP 3 Initial add-on therapy
Add inhaled long-acting beta-2 agonist (LABA) Assess control of asthma: 1. Good response to LABA and good control -> continue 2. Benefit from LABA but control still inadequate -> continue LABA and increase inhaled steroid dose to 800 mcg/day (>12 years) and 400 mcg/day (5-12 years) 3. No response to LABA -> stop LABA and increase inhaled steroid dose to 800 mcg/day (>12 years) and 400 mcg/day (5-12 years) -> if control still inadequate, trial of other add-on therapy like leukotriene receptor antagonist or sustained release theophylline
__________________________________________________________________________________
- 45 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ insufficient response STEP 4 Persistent poor control Thorough re-evaluation Consider trial of 1. Increasing inhaled steroids to 2000 mcg/day (>12 years) or 800 mcg/day (5-12 years) 2. leukotriene receptor antagonists 3. theophylline 4. slow release 2 agonist tablets, caution in patients already on LABA insufficient response STEP 5 add oral prednisolone at lowest possible dose
STEPPING DOWN Review treatment every 3 months once asthma is under control. Patients should be maintained at the lowest possible dose of inhaled steroid. When deciding which drug to step down first and at what rate, the severity of asthma, the side effects of the treatment, time on current dose, the beneficial effect achieved, and the patients preference should all be taken into account. Reduction in inhaled steroid dose should be slow as patients deteriorate at different rates. Reductions should be considered every three months, decreasing the dose by approximately 25-50% each time. Consider stopping inhaled steroids after 6-12 months of few or no symptoms, preferably at end of the season if symptoms are seasonal. Discharge criteria and arrangement : 1. Having stopped inhaled steroids for > 1yr 2. Asthma is mild or infrequent episodic 3. Referral to GP / Govt OPD / family clinic 4. Specialty referral if patient still required regular follow up: - other paediatrics unit upon parental request - adolescent clinic if problems associated with adolescence - adult medical unit if > 18 years or after secondary school N.B. Budesonide is preferred for children < 4 year old if the daily dose of beclomethasone > 400 mcg because of the growth effect and study of fluticasone on young age is lacking. This serves as a guideline only. Please discuss with senior from step 3 onwards.
Dr SL Lee __________________________________________________________________________________
- 46 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ INHALER DEVICES FOR CHILDREN OF DIFFERENT AGE Age (yr ) Device, in order of preference <1 spacer with mask nebuliser spacer with mask Types Babyhaler Aerochamber (infant) PortaNeb Aerochamber (children) Nebuhaler / Volumatic with mask Babyhaler Space chamber Volumatic Nebuhaler Turbuhaler Accuhaler
1-3
3-5
spacer
5-8 >8
dry powder inhaler meter dose inhaler with training dry powder inhaler Autohaler
CHARACTERISTICS OF SPACER DEVICES Types Material Mask Dead-space Aerochamber (infant - red ) Plastic Small --(child - yellow) large Babyhaler Space chamber Nebuhaler Plastic Plastic Plastic Yes No No large -----
Mouth-piece No
No Yes Yes
Volume(ml) Depends on types, around 200-250ml 350 230 750 750
Length(mm) 150
Valve single
Cost(HK$)
300 160 280 230
double single single single
free from QM pharmacy ~ ~
Volumatic Plastic No --Yes Nebuchamber (metal chamber) has been withdrawn from the market.
__________________________________________________________________________________
- 47 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ INHALER TECHNIQUE General principles : provide demonstration and illustrated instructions whenever a new inhaler device is prescribed technique should be checked regularly for all types of inhaler device MDI + spacer device is strongly recommended for paediatric patients of all ages. A face mask is required until the child can breathe reproducibly using the spacer mouthpiece. Where this is ineffective a nebuliser may be required. advise mouth rinse for all types of inhaled steroids to avoid confusion although some types are shown to have minimal systemic effect ; wipe the face if face mask is used instead of mouthpiece for spacer device home nebuliser is not encouraged; please discuss with respiratory team before prescribing it METER DOSE INHALER ( MDI ) Steps 1. Remove the mouthpiece cover 2. Shake the inhaler vigorously 3. Breath out deeply 4. Hold MDI upright 5. Put mouthpiece between lips 6. Head tilt slightly back 7. Actuate MDI 8. At the same time, inhale slowly and deeply via the mouth 9. Hold breath for 10 seconds 10. Exhale through the nose 11. Replace the cover 12. If more than 1 puff is required, wait for at least 30 seconds, repeat step 2 to 10 Common errors 1. Forget to shake well the canister 2. Poor coordination of actuation and inhalation 3. Stop inhalation when the cold aerosol hit the soft palate (cold Freon effect) 4. Actuation of the aerosol into the mouth followed by inhalation through the nose 5. Too rapid inhalation SPACER DEVICES ( SD ) WITH MOUTHPIECE / FACE MASK Steps : 1. Assemble SD 2. Remove the cap of meter dose inhaler ( MDI ) 3. Shake well the canister of MDI 4. Connect MDI to SD securely upright 5. Hold SD horizontally or with MDI side pointing slightly upwards 6. For use with mouth piece Seal lips around mouthpiece of SD Actuate MDI Perform tidal breathing slowly through SD immediately after actuation with rocking sound of SD heard Perform 5-10 tidal breaths before removal of SD __________________________________________________________________________________
- 48 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ 7. For use with face mask Connect face mask onto the mouthpiece of Nebuchamber; remove the mouthpiece before attachment of face mask for Nebuhaler Gently place the face mask over the childs face covering the nose and chin, secure tightly Actuate MDI Let the child breath in 5-10 times through the mask If more than 1 puff is required, repeat steps 3 to 7 Common errors : Actuate before applying mask to face or put mouthpiece to lips Lip / face seal not tight enough Multiple actuation Breath too fast through SD Forget to shake the canister of MDI for the subsequent dose Remarks : Use of SD reduces oro-pharyngeal deposition of drugs by about 50%. The optimal volume of a spacer depends upon the childs tidal volume. For children aged 1-2 years old, the spacer volume is not so important as long as spacer volume not exceed 750ml. All school children can use a spacer effectively during acute attacks. Most preschool children can use a spacer for prophylactic medication, but may not be able to use if efficiently during acute attack. The drug should be administered by repeated SINGLE actuation of pMDI into the spacer, each followed by inhalation. There should be minimal delay between pMDI actuation and inhalation. Tidal breathing is as effective as single breaths. Five tidal breaths is as effective as ten if child is cooperative. Spacers should be cleaned monthly rather than weekly as per manufacturers recommendations or performance is adversely affected. They should be washed in detergent and allowed to dry in air. The mouthpiece should be wiped clean of detergent before use. Priming of the spacer with a few puffs of a reliever Puffer after washing or before use for spacer that is only used occasionally. Plastic spacer should be replaced at least every 12 months.
DRY POWDER INHALER ( DPI ) WITH MULTIPLE DOSES Remarks avoid blowing into DPI as it may clog the powder some studies demonstrated that exhalation before the inhalation or breath holding afterwards is not necessary for DPI the dosage delivered from DPI increases with inspiratory flow rate, thus children should be taught to inhale rapidly through these inhalers many young children and some older children with severe wheezy cannot generate a sufficient inspiratory flow rate, therefore DPIs should not be by routine be prescribed to children younger than 5 years while some older children may need a spacer inhaler during severe acute wheeze
__________________________________________________________________________________
- 49 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ TURBUHALER ( TH ) Steps 1. Unscrew and lift off the cover 2. Check the window on the TH to ensure that it is not empty 3. Hold TH upright 4. Turn the basal rotating disk clockwise and anticlockwise once, with a click sound heard 5. Breath out 6. Seal the mouthpiece around the lips 7. Inhale deeply and rapidly through the mouth 8. Remove the inhaler 9. Hold breath for 10 seconds 10. Breath out slowly 11. If more than one dose is required, repeat step 2 to 8 Common errors 1. Shake TH 2. Forget to check the window 3. Replace the mouthpiece with training whistle ( BIG MISTAKE )
ACCUHALER ( AH ) Steps 1. Hold the inhaler at horizontal level and check the indicator to see the number of doses left 2. Hold the outer case in one hand and put the thumb of the other hand on the thumb grip and push the thumb away as far as it will go 3. Slide the lever away until it clicks 4. Breath out 5. Seal the mouthpiece around the lips 6. Inhale deeply and rapidly through the mouthpiece 7. Remove AH 8. Hold breath for 10 seconds 9. Breath out slowly 10. Close the outer case 11. If more than one dose is required, repeat steps 2 to 9 Common errors : 1. Slide the lever long before inhalation 2. Forget to close the outer case before the second dose if required
__________________________________________________________________________________
- 50 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ MEDICATION FOR CHILDHOOD ASTHMA age Salbutamol ( Ventolin ) Terbutaline ( Bricanyl ) Salmeterol ( Serevent ) > 4 yr Dosage 200mcg 4 to 6 hrly 500mcg 4 to 6 hrly 50mcg b.d. 40mcg t.d.s. 5mg q.i.d. Spacer device Babyhaler Volumatic Aerochamber Nebuchamber Nebuhaler Aerochamber Volumatic Aerochamber Aerochamber Volumatic Nebuhaler Aerochamber Babyhaler Volumatic Aerochamber Nebuchamber Nebuhaler Aerochamber Volumatic Aerochamber MDI (doses) 100mcg (200) Cost DPI Accuhaler 200mcg (60) Turbuhaler 500mcg(200) Accuhaler 50mcg (60) Cost oral syrup:2mg/5ml tablet:4 mg Volmax:4mg syrup:0.3mg/ml tablet:2.5mg durule:5mg Cost
250mcg (400)
25mcg (120) 20mcg (200) 5mg (112 )
Ipratropium (Atrovent ) Sodium Cromoglycate (Intal)
Beclomethasone (Becotide, Becloforte ) Budesonide ( Pulmicort )
100mcg to 200mcg b.d. 100mcg to 200mcg b.d. > 4 yr 50mcg to 100mcg b.d.
50mcg (200) 250mcg (200) 50mcg (200) 200mcg (200)
Becodisk 100mcg(8) 200mcg(8) Turbuhaler 100mcg (200) 200mcg (200) 400mcg (200) Accuhaler 50mcg (60) 250mcg (60) Neulin:80mg/15ml Theodur:200mg /300mg tab Slo-theo:50mg /75mg cap
Fluticasone ( Flixotide )
25mcg (60) 50mcg (60) 125mcg (60) 250mcg(120)
Theophylline
__________________________________________________________________________________
- 51 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.1.2: MEDICATION FOR ALLERGIC RHINO-CONJUNCTIVITIS
SEDATING ANTI-HISTAMINE Chlorpheniramine ( Piriton ) Dextrochlorpheniramine ( Polaramine / Polaramine S.R.) Ketotifen (Zaditen ) NON-SEDATING ANTI-HISTAMINE Cetirizine ( Zyrtec ) Loratadine ( Clarityne ) TOPICAL NASAL DECONGESTANT Phenylephedrine Xylometazoline ( Otrivin Paed ) ( Otrivin Adult ) Oxymetazoline HCl ( Nezeril ) Conc. 0.5% 0.05% 0.1% 0.1mg/ml 0.2mg/ml Syrup 2mg/5ml Unit Cost HK$ Tablet 4mg Unit Cost HK$ Dosage 1-2yr 2-6yr 6-12yr 2-6yr 6-12yr 1mg b.d 1mg t.d.s.-q.i.d. 2mg t.d.s.-q.i.d. 1mg t.d.s.-q.i.d. 2mg t.d.s.-q.i.d.
2mg 6mg 1mg
6/12-2yr 0.5mg b.d. >2yr 1mg b.d. Unit Cost HK$ Dosage > 6yr 5mg b.d./10 mg daily > 6yr 10mg daily
Syrup 10mg/ml
Unit Cost HK$
Tablet 10mg 10mg
Amount / bottle 10ml 10ml 10ml
Unit Cost HK$
__________________________________________________________________________________
- 52 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ TOPICAL STEROID NASAL SPRAY * Beclomethasone ( Aqueous Beconase ) Budesonide ( Aqua Rhinocort ) Budesonide ( Rhinocort Turbuhaler ) Dosage ( to each nostril ) 50mcg to 100mcg b.d. 50mcg to 100mcg b.d. 100mcg b.d. Dose ( per bottle ) 50mcg (200) 50mcg (200) 100mcg (200) 50mcg (120) Unit Cost HK$
Fluticasone ( Aqueous Flixonase ) 50mcg daily * Not recommended for children < 6 years old TOPICAL EYEDROPS Hypromellose Sodium chloride 0.9% Oculosan Cromoglycate Na 2% ( Opticrom ) Amount ( per bottle ) 10ml 10ml 10ml 10ml
Unit cost HK$
__________________________________________________________________________________
- 53 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.1.3: MEDICATION FOR ECZEMA
ANTIHISTAMINES Chlorpheniramine ( Piriton ) Syrup 2mg/5ml Unit Cost Tablet 4mg Unit Cost Dosage 1-2yr 2-6yr 6-12yr 1mg b.d 1mg t.d.s.-q.i.d. 2mg t.d.s.-q.i.d.
Hydroxyzine (Atarax) Promethazine Hcl (Phenergan ) 5mg/5ml/5ml
25mg 10mg 25mg Unit cost / HK$ cream ointment 10% cream 10% cream (20g) 10% cream (60g)
6mth-6yr 15mg/D to 50mg/D q.i.d. >6yr 25mg/D to 100mg/D q.i.d. >2yr 1mg/kg/D
EMOLLIENTS Aqueous Emulsifying Paraffin soft white ( Vaseline ) Urea in Petrolatum Base ( Urederm ) ANTI-PRURITICS Crotamiton ( Eurax )
TOPICAL STEROIDS + ANTI-INFECTIVES Hydrocortisone 1% + clioquinol 3% Hydrocortisone 1% + neomycin 0.5% Synalar + vioform Diflucortolone valerate 0.1% + chlorquinaldol 1% ( Nerisone C ) Triamcinolone acetonide 1mg + neomycin 2.5mg + gramicidin 0.25mg + nystatin 100,000u ( Kenacomb ) cream (5g) ointment (5g) cream (5g) cream (10g) cream (5g) ointment (5g)
Unit cost / HK$
__________________________________________________________________________________
- 54 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ TOPICAL STEROIDS Hydrocortisone Strength ( amount ) 1% lotion (20ml) 1% cream 1% ointment (5g) 0.02% cream (100g) 0.05% cream (25g) 0.0050% cream 0.0125% cream 0.0250% cream 0.1% lotion (30ml) 0.1% cream (15g) 0.05% cream (15g) 0.05% ointment (15g) 0.1% cream (15g) 0.1% ointment (15g) 0.005% cream (15g) 0.050% cream (15g) 0.05% cream (25g) 0.05% ointment (25g) Unit cost / HK$ Dosage t.d.s Potency mild
Triamcinolone Acetonide ( Aristocort ) Clobetasol Butyrate ( Eumovate ) Fluocinolone Acetonide ( Synalar ) Mometasone Furoate ( Elomet ) Betamethasone Dipropionate ( Diprosone ) Betamethasone Valerate ( Betnovate ) Fluticasone Propionate ( Cutivate ) Clobetasol Propionate ( Dermovate )
t.d.s up to q.i.d. up to t.d.s.
mild mod potent mod potent mod potent potent potent potent potent potent very potent
once daily b.d. b.d. - t.d.s. once daily once - b.d.
* should use mildly potent steroids for infant only and mildly or moderately potent steroids for children <5 years old Dr SL Lee
__________________________________________________________________________________
- 55 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.1.4 ACUTE ASTHMATIC ATTACK
Exacerbations of asthma (acute asthma or asthma attacks) are episodes of progressive increase in shortness of breath, cough, wheezing, or chest tightness, or some combination of these symptoms. Treatment of exacerbations depends on severity of attack. Aims of treatment are: To relieve airflow obstruction and hypoxaemia as quickly as possible To plan the prevention of future relapses Assessment of severity (GINA 2009)
Hypercapnea (hypoventilation) develops more readily in young children than in adults and adolescents.
__________________________________________________________________________________
- 56 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Mild / Moderate asthma attack 1. DAT 2. AR/RR Q4h 3. Check SpO2 keep SpO2 95% 4. Peak Flow BD 5. Inhaled beta-2 agonist through pMDI + spacer : Give Salbutamol (Ventolin) or Terbutaline (Bricanyl) via spacer (Volumatic or Neubuhaler) Age < 6 years old Dose of Ventolin MDI and method of administration 6 puffs i.e. 6 x 100 microgram (equivalent to 2.5mg nebule) Load the spacer with one puff at one time and the child should have 5 tidal breaths each time for efficient drug delivery. 12 puffs i.e. 12 x 100 microgram (equivalent to 5mg nebule) Load the spacer with one puff at one time and the child should have 5 tidal breaths or a single vital capacity breath each time for efficient drug delivery.
> 6 years old
If the initial response is inadequate, repeat every 20 minutes for a total of 3 doses. Then space out 1-4 hourly until condition settles. Nebulised Salbutamol (Ventolin) ( 1mg/ml nebule) :0.15mg/kg/dose (max 5mg/dose) can be considered under the following situations: Clinical features of severe/life threatening asthma on admission Patient failed to respond to salbutamol via spacer device especially if < 2 years old Severe asthma attack Recognition of acute severe asthma in children aged over 2 years SpO2 < 92% PEF 33-50% Cant complete sentences in one breath or too breathless to talk or feed Pulse > 125 beats/min ( > 5years old) or > 140 ( 2 to 5 years old) Respiration > 30 breaths/min ( >5 years) or > 40 (2 to 5 years) Life threatening features SpO2< 92% PEF < 33-50% best or predicted Exhaustion Hypotension Confusion Coma Ix: 1. CXR indicated when Suspect pneumothorax or pneumomediastinum Life threatening signs Unsatisfactory response to treatment Signs of pneumonia 2. Blood gas consider if SpO2 < 92% on air or with any life threatening signs Investigations are rarely needed for immediate management and are not routinely indicated. Do not rely on blood gas to decide on the initial management in children.
Silent chest Cyanosis Poor respiratory effort
__________________________________________________________________________________
- 57 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Management of severe asthma attack Immediate treatment High flow oxygen via face mask (up to 100%) Nebulised Salbutamol (Ventolin) Q1h Prednisolone 1 mg/kg/day oral (max 2mg/kg daily up to 60 mg daily) usually for 3-5 days NPO + IV maintenance fluid (Set IV when patient less disturbed) watch out for hypokalemia if very frequent doses of Ventolin are given AR/RR Q1h SpO2 continuous monitoring( Keep SpO2 > 92%) Portable CXR if SpO2 < 92%. Watch out for pneumothorax. PEF before & after nebulised Salbutamol QID for monitoring If life threatening features are present : Inform senior for assessment for ICU admission. IV hydrocortisone 4 mg/kg/dose (max 100mg) Q6h Add nebulised Ipratropium (Atrovent) 1ml (0.5 ml in < 5 years) to nebulised Salbutamol Q6h IV Aminophylline Loading dose : 5 mg/kg, infuse slowly over 30 min. * OMIT loading if already on oral theophylline. Check urgent drug level before giving loading if uncertain. Maintenance infusion 0.6 -0.8 mg/kg/hr If patient is not improving after 15 - 30 min: Continue O2 Give nebulised Salbutamol more frequently, up to Q 15-30min Consider early addition of a single bolus dose of IV salbutamol (15mcg/kg over 10 minutes) in severe cases where the patient has not responded to initial inhaled therapy Transfer to ICU accompanied by MO prepared to intubate if there is: 1. Deteriorating PEF, worsening/persisting hypoxia or hypercapnia 2. Exhaustion, confusion or drowsiness 3. Coma or respiratory arrest Discharge plan : 1. Underlying cause of exacerbation determined and the problem rectified. 2. Regular asthma medication adjusted if necessary 3. Compliance reinforced. Watch out for any underlying psychosocial issues affecting adherence to treatment. 4. Inhalation technique checked and recorded 5. PEF > 95% predicted or best (from OPD record) and diurnal variability <25% 6. Been on discharge medication for 24 hours 7. Follow up arrangement : 1. Mild to moderate attack :ward follow up optional; respiratory / asthma clinic within 2 months 2. Severe attack: ward follow up - 1 week; respiratory / asthma clinic - 4 weeks (Reference: GINA 2009. British Guideline on management of asthma, British Thoracic Society and Scottish Intercollegiate Guidelines Network, Revised June 2009)
__________________________________________________________________________________
- 58 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.1.5 ACUTE RESPIRATORY DISTRESS
DDx: 1. Respiratory tract: upper or lower * Upper (stridor) foreign body viral laryngotracheitis acute epiglottitis bacterial tracheitis (Staphylococcal) spasmodic croup others: angioneurotic edema, retropharyngeal abscess, diphtheria (in non-immunised child) * Lower (wheezes) asthma bronchiolitis pneumonia 2. Cardiac: Heart failure -
congenital heart disease rhythm problems e.g. SVT, heart block myocarditis cardiomyopathy secondary to severe anaemia, thyrotoxicosis, sepsis...
3.
Metabolic * acidotic breathing Diabetic ketoacidosis (# Test urine x sugar & ketone) Salicylate(Aspirin) poisoning Uraemia Fulminating sepsis Other metabolic disorders: MSUD
__________________________________________________________________________________
- 59 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.1.6 ACUTE UPPER AIRWAY OBSTRUCTION
Important causes : 1. Foreign body aspiration 2. Infection Croup (laryngotracheobronchitis) Acute epiglottitis Acute epiglottitis A medical emergency Definitive airway placement is the first priority when epiglottitis is suspected. Any manipulation including throat exam. XR neck, venipuncture or IV placement may precipitate complete obstruction. Management Give O2(blow by). NPO. Have parent accompany child. Keep child propped up and undisturbed. Have physician accompany patient at all times. Call: senior ICU paediatrician, anaesthetist, and ENT surgeon. Escort patient to Operating Theatre where intubation is done under anaesthesia (using O2 and inhaled halothane alone). Place IV catheter in OT before induction of anaesthesia, with patient fully monitored, ENT surgeon standing by with tracheostomy set ready. After airway is secured, draw blood for: o CBP D/C o culture and start IV Cefotaxime. TO ICU Rifampicin prophylaxis for close contacts Acute laryngotracheobronchitis (Croup) Watch out for signs of severe obstruction 1. Hypoxia - restlessness, tachycardia, cyanosis 2. Physical exhaustion - decreased stridor & insucking, lethargy Cyanosis, decreased conscious level, extreme restlessness and decreasing respiratory effort along with decreasing stridor and breath sounds are indications for urgent intubation. Management of moderate to severe croup Minimal handling. Parents should remain with child. No throat examination. No need for arterial puncture. 2. Oxygen 3. NPO + IV fluid (Set IV when patient is less disturbed.) 4. AR/RR Q1h 5. SaO2 monitoring 6. Steroid on admission: dexamethasone PO/IM 0.6 mg/kg or nebulised Budesonide (Pulmicort) 2 mg 7. Nebulized adrenaline 1:1000 0.5ml/kg (max 5 ml) for temporary relief (# Note rebound phenomenon).If frequent repeated doses are necessary, intubation will be required. 8. To ICU if progressive deterioration or signs of severe obstruction __________________________________________________________________________________ 1.
- 60 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Investigations (only when patient is stable) 1. CBP D/C 2. (Blood C/ST) 3. Blood gas, Na K Ca 4. Portable CXR, lateral XR neck 5. NPA x viral IF
Refer to Clinical Guidelines on management of croup by the HK College of Paediatricians available on the eKG Paediatrics section.
__________________________________________________________________________________
- 61 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.1.7 ACUTE VIRAL BRONCHIOLITIS
Occurs in infants, especially those under 6 months Common etiologic agents: RSV, parainfluenza 3 virus, adenovirus Any of the following features should lead to further review and referral for hospital admission: a history of apnoea difficulty feeding may require supportive care and if infants have taken less than 50% of their usual fluid intake in the preceding 24 hours hospital admission is required severe respiratory distress with accessory muscle use or grunting Respiratory rate greater than 60 Diagnostic uncertainty SpO2< 92% in room air
Management * Supportive treatment 1. DAT or NPO with IV fluid (if in distress) 2. AR/RR Q1 - 4 H 3. SpO2 monitoring 4. Nasal O2 to keep SpO2 > 92% 5. Trial of short acting beta-2-agonist (SABA) - continued only in those who showed a clinical improvement. 6. use of systemic steroid is not recommended 7. Antibiotics indicated only for secondary bacterial pneumonia 8. No chest physiotherapy during acute stage 9. Ribavirin is not recommended for infants with bronchiolitis although may have a place in children post transplant Investigations 1. (CBP D/C) 2. NPA x viral IF 3. CXR
__________________________________________________________________________________
- 62 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
SECTION 3.2: INFECTION
__________________________________________________________________________________
- 63 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.2.1 ANTIMICROBIAL THERAPY
General principles Ask for any history of allergies before prescribing. If possible, collect specimens for microbiological examination before starting antimicrobial therapy. When initiating therapy, consider o severity of condition o possible infecting pathogens know the local epidemiology and resistance pattern Modify treatment according to child's progress and bacterial sensitivities.
Suggested initial treatment Meningitis Age Usual organisms < 1 month Gp B streptococci(GBS), Enterobacteriaceae, Listeria monocytogenes
1-3 month
GBS, Streptococcus pneumoniae, Haemophilus influenzae b, Neiserria meningititidis, Enterobacteriaceae S. pneumoniae, Haemophilus influenzae b, Neiserria meningititidis
Infants > 3 months and children
Empiric therapy IV Penicillin 200,000 units/kg/day div Q6h (for neonates > 7 days and > 2kg) or IV Ampicillin 200mg/kg/day div Q6H (>7 days and > 2 kg) AND IV Cefotaxime 150mg/kg/day div Q6H (>7 days and > 2 kg) Alternative: Penicillin/ Ampicillin + aminoglycoside IV Vancomycin 60 mg/kg/day div Q6-8H+ IV Cefotaxime 300mg/kg/day div Q6H for possible penicillin-resistant S. pneumoniae until susceptibility is known. IV Cefotaxime 300mg/kg/day div Q6H or IV Ceftriaxone 100mg/kg/day div Q12H PLUS IV Vancomycin 60mg/kg/day div Q6-8H for possible penicillin-resistant S. pneumoniae until susceptibility is known.
Remarks GBS & Listeria : 14-21 days treatment. Enterobacteriaceae: 21 days treatment
Hib : 7-10 days S. pneumoniae: 10-14 days N. meningititidis: 7 days
Watch out for Salmonella in infants and TB in older children.
Pharyngitis/Tonsillitis Usual organisms Gp A Streptococci
Empiric therapy Penicillin VK 20-50 mg/kg/day div TID or QID po
Remarks 10 days
__________________________________________________________________________________
- 64 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
Pneumonia Age Usual organisms GBS, E. coli, Staph Neonate aureus, Listeria monocytogenes Infant/ Usually respiratory child (< 4 viruses. years) S. pneumoniae, H. influenzae, Moraxella catarrhalis
Empiric therapy IV Penicillin + Gentamicin or IV Penicillin + Cefotaxime No antibiotics Amoxicillin/clavulanate PO (35-45mg amoxicillin/kg/day BD; high does of 80-90 mg amoxiciilin/.kg/day div BD for PCN-nonsusceptible S. pneumoniae) or Cefuroxime 20-30 mg/kg/day div BID IV: Cefuroxime 100-150 mg/kg/day div Q8H, Cefotaxime 50-180 mg/kg/day div Q6-8H, Ceftriaxone 50-75mg/kd/day div Q12-24H Erythromycin PO 30-50mg/kg/day TDS/QID Amoxicillin/clavulanate PO (40 mg amoxicillin/kg/day div BD; high does of 80-90 mg amoxiciilin/kg/day div BD for PCN-nonsusceptible S. pneumoniae) IV: Cefuroxime, Cefotaxime, Ceftriaxone
Remarks Use Ampicillin instead of Penicillin if suspect Listeria. Give 10-21 days.
7-10 days Augmentin = Amoxicillin 400mg + clavulanate 57mg per 5ml, ratio 7:1
Child > 4yr
Consider Chlamydia trachomatis in infants < 3 months S. pneumoniae, H. influenzae, Moraxella catarrhalis
7-10 days
Mycoplasma pneumoniae Erythromycin PO (Atypical pneumonia) 30-50mg/kg/day TDS/QID or Clarithromycin PO 15mg/kg/day BD, or Doxycycline2-4 mg/kg/day div Q12 H the first day, then dose Q24H (for >7 yr, but consider for macrolide resistant M. pneumoniae) or Ciprofloxacin (for > 18 yr, but consider for macrolide resistant M. pneumoniae)
14 days
No data but suggest 7 days for uncomplicated pneumonia and good response
__________________________________________________________________________________
- 65 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
Acute Otitis media/ Acute sinusitis Usual organisms S. pneumoniae, H. influenzae (nontyepable), Moraxella catarrhalis Empiric therapy 1st line: Amoxicillin, or high dose Amoxicillin 80-90mg/kg/day if likely to have PCN-nonsusceptible S. pneumoniae Alt for Penicillin allergy: Cefuroxime, azithromycin Persistent OM: Amoxicillin/clavulanate, Cefuroxime, or Ceftriaxone (IM/IV) Consult ENT Remarks 5-7 days for OM ( 6 yr with mild to moderate disease); 10 days for younger or with severe disease 10-14 days for sinusitis (or 7 days after clinical improvement)
Cellulitis Usual organisms Gp A Streptococci, Staphylococcus aureus Empiric therapy Remarks PO: Flucloxacillin or Amoxicillin/clavulanate 7- 10 days Alt: Cephalexin. If Penicillin allergic, clindamycin IV: Cloxacillin 50-100 mg/kg/day div Q6H (for 1 yr, maximum 4 gm/day). Alt: Cefazolin 50-100 mg/kg/day div Q8H, Clindamycin 20-40mg/kg/day div Q6-8H
__________________________________________________________________________________
- 66 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.2.2 COMMONLY USED ORAL ANTIBIOTICS
Drug Amoxicillin(Amoxil) 125mg/5ml 250mg capsule Dosage 40mg/kg/day div BID or TDS 80-90 mg/kg/d div BID or TID for PCN nonsusceptible S. Pneumoniae Adult: 250-500mg/dose TDS Dosage based on Amoxicillin component 40mg/kg/day div BID or TDS 80-90 mg/kg/d div BID or TID for PCN nonsusceptible S. Pneumoniae Adult: 250-500mg/dose TDS or 750mg/dose BD Azithromycin (Zithromax) 200mg/5ml 250mg capsule 10mg/kg daily loading dose, then a5 mg/kg/day (for otitis media and pneumonia) 12 mg/kg/day Q24H (for pharyngitis) Single dose of 1 g for STD caused by Chlamydia trachomatis Ceftibuten(Cedax) 180 mg/5ml 400mg capsule Cefuroxime(Zinnat) 125mg/5ml 125mg, 250mg tablet Cephalexin 125mg/5ml(Keflex) 250mg, 500mg capsule (Ceporex) Ciprofloxacin(Ciproxin) 250mg, 500mg tablet 9mg/kg/day daily Adult: 400mg/dose daily 20-30mg/kg/day div BID Adult 250-500mg/dose BD 25-50mg/kg/day div BID 100mg/kg/day QID (max 1g) for follow-up oral therapy of osteoarticular infection 15mg/kg/day div BID *given only when benefits outweigh risk of arthropathy Clarithromycin (Klacid) 125mg/5ml 250mg, 500mg tablet Clindamycin 150mg capsule 15mg/kg/day div BiD Adult: 250-500mg/dose BD 10-30mg/kg/day div TID or QID Adult: 150-450mg/dose TDS or QID Co-trimoxazole (Septrin) 240mg/5ml(i.e. 40mg trimethoprim /200mg sulphamethoxazole) 480mg tablet Dosage based on TMP component 8-10mg/kg/day BD UTI prophylaxis: 2-4mg/kg/dose, single dose nocte (or just use trimethoprim)
Amoxicillin & Clavulanic acid (Augmentin) 457mg/5ml (400mg Amoxicillin/57mg Clavulanic acid)
__________________________________________________________________________________
- 67 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Adult: 160mg/dose BD i.e. 2 tablets BD Doxycycline Erythromycin 200mg/5ml 250mg tablet Flucloxacillin 125mg/5ml 2-4 mg/kg/day, Q12H on 1st day, then dose Q24H (for patients > 7 yrs or benefits of therapy outweighs risk of teeth staining) 40mg/kg/day div QID Adult: 500mg/dose QID Children >12y and > 40 kg :1000-2000 mg/day div QID 12 yr and 40 kg: 25-50mg/kg/day div QID Infants < 6m: 25mg/kg/day div QID Adult: 250-500mg/dose QID Nalidixic acid (Wintomylon) 500mg tablet 55mg/kg/day div QID Adult: 1gm /dose QID initially then 500mg/dose QID Nitrofurantoin 50mg tablet 5-7mg/kg/day div QID UTI prophylaxis: 1-2mg/kg/dose, single dose nocte Phenoxymethylpenicillin Potassium (Penicillin V) 125mg/5ml 250mg tablet 25-50mg/kg/day div TDS or QID Adult: 250-500mg/dose TDS or QID
Updated by Dr S Chiu, October 2010
__________________________________________________________________________________
- 68 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.2.3 FEVER
DDx: 1. Infections Respiratory tract infections (commonest) - URI, otitis media, pneumonia UTI Meningitis Gastroenteritis Infective endocarditis Bone & joints: septic arthritis, osteomyelitis Other viral diseases: EBV If prolonged fever, think of TB Typhoid Malaria 2. inflammatory: Kawasaki disease, collagen vascular disease e.g. SLE, JIA 3. Malignancy
Investigations: 1. CBP D/C, smear (thick & thin smear if suspect malaria) 2. ESR, CRP 3. LFT, RFT 4. Blood C/ST (x 3 if suspect SBE) 5. NPA x viral IF 6. Urine x R/M C/ST 7. CXR If prolonged fever, 1. Widal test 2. C3 C4 Ig pattern 3. CRP 4. ANA, anti-DNA, RF 5. Viral titre, EBV panel 6. Mantoux test 7. Stool x C/ST 8. Urine x VMA, HVA (neuroblastoma) Treatment 1. Symptomatic : Paracetamol (Panadol ) 10 mg/kg/dose Q4h prn Tepid sponging, ice pack 2. Treat underlying cause.
__________________________________________________________________________________
- 69 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
SECTION 3.3: CARDIOLOGY
__________________________________________________________________________________
- 70 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.3.1 INFECTIVE ENDOCARDITIS PROPHYLAXIS
Prophylaxis recommended: 1. Prosthetic cardiac valve or prosthetic material used for cardiac valve repair 2. Previous infective endocarditis 3. Congenital heart disease (CHD) - Unrepaired cyanotic CHD, including palliative shunts and conduits - Completely repaired congenital heart defect with prosthetic material or device, whether placed by surgery or by catheter intervention, during the first 6 months after the procedure - Repaired CHD with residual defects at the site or adjacent to the site of a prosthetic patch or prosthetic device (which inhibit endothelialization) 4. Cardiac transplantation recipients who develop cardiac valvulopasty Antibiotics regimen: Dental procedures that involve manipulation of gingival tissue or periapical region of teeth or perforation of the oral mucosa
Respiratory tract procedures that involve incision or biopsy of respiratory mucosa (such as tonsillectomy or adenoidectomy, but NOT simple bronchoscopic examination) Regimen as listed above. Gastrointestinal and genitourinary tract procedure Administration of prophylactic antibiotics SOLELY to prevent endocarditis is NOT recommended. (Reference: Prevention of Infective Endocarditis, Guidelines from the American Heart Association. Circulation 2007; 116:1736-1754) Prof YF Cheung Updated October 2010 __________________________________________________________________________________
- 71 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.3.2 HEART FAILURE
Causes 1. Congenital heart disease - High pulmonary blood flow: VSD, PDA, AVSD - Lt heart obstruction: COA, AS 2. Myocardial causes - Cardiomyopathy - Myocarditis - Myocardial ischaemia 3. Valvar lesions - Infective endocarditis 4. Cardiac arrhythmias: SVT, complete heart block 5. Non-cardiac causes - Thyrotoxicosis - Severe anaemia - Fulminating sepsis - Systemic AV fistula - Fluid overload: acute nephritis Management 1. Bed rest 2. SpO2 monitoring nasal oxygen 1-3L/min 3. BP/P Q1h, cardiac monitoring 4. DAT / NPO + IV fluid, 70-80% maintenance / NG tube feeding 5. Strict I & O 6. Treat arrhythmia if present 7. Drugs: - Diuretics: frusemide + spironolactone - Digoxin - Vasodilator: captopril, hydralazine 8. Treat intercurrent infections Investigation: 1. CBP D/C (ESR) 2. LFT RFT Na K Blood gas Ca 3. CPK, CPK-MB, troponin, LDH for suspected myocarditis 4. Blood C/ST x 3 for suspected SBE 5. CXR, ECG 6. Virus study & viral titre esp for enterovirus (for suspected myocarditis) 7. Others: Digoxin level, urine x RBC, metabolic screening including carnitine, echocardiogram Updated by Prof YF Cheung, October 2010
__________________________________________________________________________________
- 72 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.3.3 SHOCK
Causes 1. Hypovolaemia Blood loss Plasma loss (e.g. burns) Dehydration 2. Cardiogenic Myocarditis, cardiomyopathy Arrhythmia Hypoxia from shunting/ outflow obstruction/ respiratory failure 3. Sepsis 4. Anaphylaxis Immediate management 1. Give 100% oxygen and respiratory support if necessary. 2. Make an initial assessment based on history & PE to determine aetiology 3. Establish IV access 4. ECG monitoring 5. Unless initial assessment indicates a cardiac cause, give 10-20 ml/kg NS or Haemaccel as appropriate over 15 min. Subsequent management 1. Arrange definitive investigations e.g. CBP, blood culture, L/RFT, NaK blood gas, glucose, CXR, ECG etc. 2. ICU admission: may need intra-arterial line and CVP monitoring, urinary catheter (monitor hourly urine output), inotropic support 3. Treat underlying cause
__________________________________________________________________________________
- 73 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
SECTION 3.4: NEUROLOGY
__________________________________________________________________________________
- 74 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.4.1 ACUTE ENCEPHALOPATHY
Definitions of altered states of consciousness Term Clouding of consciousness Lethargy Confusion Delirium Stupor Coma Definition Minimally decreased wakefulness or awareness reduced attention span, easily distracted or startle to stimuli Decreased wakefulness or drowsiness able to engage in activity but tend to fall asleep Stimuli are consistently misjudged. May be disorientated. Have difficulty in following command Disorientated, irritable, misperceive sensory stimuli, have visual hallucination. Patient is loud, talkative, offensive, suspicious and agitated. Unresponsive aroused only by vigorous and repeated stimuli, then lapse back into stupor state on removing stimuli Unarousable
Causes of acute encephalopathy 1. 2. Hypoxic ischaemia respiratory / cardiac failure, asphyxia Infections & parainfectious causes meningitis, encephalitis, cerebral abscess, para-infectious demyelination (ADEM: acute demyelinating encephalomyelitis) Focal lesions Stroke ( ischemic and haemorrhagic), AVM, vasculitis, bleeding diathesis Tumour, abscess Trauma Accidental, non-accidental Toxin/poisoning Drugs (sedatives and hypnotics, anticonvulsants, antihistamines, anticholinergic), substance abuse Lead Metabolic Hypoglycaemia, DKA, non-ketotic hyperglycemia, hypo/hyperthyroidism, Addison crises,pituitary apoplexy hypo/hypernatremia, hypo/hypercalcemia hyperammonaemia, inborn error of metabolism, Reye encephalopathy Organ failure( renal, hepatic) Hypertensive encephalopathy Epileptic post-ictal state, non-convulsive status epilepticus
3.
4. 5.
6.
7. 8.
Management 1. Maintain Airway, Breathing, Circulation. 2. Record vital signs. 3. Record level of coma according to Glasgow coma scale (score 3-15).
__________________________________________________________________________________
- 75 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ 4. Check Dextrostix stat. If hypoglycaemic, give IV D50 2 ml/kg after saving critical sample of blood. 5. Full physical examination and note : Any signs of trauma beware of cervical spine injury or instability Signs BP Possible causes Hypertension: increased ICP ( Cushing triad: bradycardia, hypertension, slow breathing), hypertensive encephalopathy, drugs ( e.g. cocaine, amphetamine, anticholinergics), posterior reversible leukoencephalopathy Hypotension: shock ( hypovolemia, sepsis, cardiogenic, anaphylactic), drug overdose (e.g. narcotics, cyanide), adrenal failure HR Tachycardia: arrhythmia, drugs (e.g. amphetamines, alcohol, theophylline, sympathomimetics) Bradycardia: heart block, drugs (e.g.beta-blockers, narcotics) Breathing Kussmaul breathing( fast and deep): DKA or other metabolic acidosis Cheynes-Stokes breathing, ataxic breathing, slow or irregular breathing: brainstem lesions Pupils ( size, Small and reactive: metabolic disorders, intoxication by opioid, symmetry, cholinergics, hypnotics/sedatives light reflex) Pinpoint pupils: pontine lesion Dilated pupils(mydriasis): sympathomimetics, anticholinergics Fixed and dilated: brain stem lesion Unequal pupils(anisocoria): lesion of III nerve or its brainstem connections Eye Conjugate deviation to one side: ipsilateral cerebral or movements contralateral pontine lesion Limited eye movement in one direction: lesions of III, IV, VI or their connections in brainstem (* VI nerve lesion can be a false localizing sign.) Oculocephalic reflex (Normal: Rotate the head to either side, eyes should turn in opposite direction, indicating intact brainstem.) Oculovestibular reflex (Caloric test): with intact brainstem, irrigate cold water agaisnt tympanic membrane, there is tonic conjugate deviation of eyes towards stimulus for 1 or more minute before returning to midline Corneal reflex Evaluate V, VII nerves Gag reflex Evaluate cranial nerves IX, X Fundi Papilloedema, retinal haemorrhages Involuntary Focal seizure: SOL movement Multifocal myoclonus: metabolic Focal Focal lesion neurological signs
__________________________________________________________________________________
- 76 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Glasgow Coma Scale(GCS) for children Sign Eye opening GCS (>5 yr) Spontaneous To command To pain None Oriented Confused Inappropriate words Incomprehensible sounds None Obeys commands Localizes pain Withdraws Abnormal flexion to pain Abnormal extension to pain None GCS modified (<5 yr) Spontaneous To sound To pain None Alert, babbles, coos, words, or sentences normal for age Less than usual ability, irritable cry Cries to pain Moans to pain None Normal spontaneous movement Localizes pain Withdraws Abnormal flexion to pain Abnormal extension to pain None Score 4 3 2 1 5 4 3 2 1 6 5 4 3 2 1
Verbal response
Motor response
A score of <8 is consistent with severe brain dysfunction. Treatment of acute encephalopathy 1. NPO 2. Strict I & O 3. Neuro-observation Q1h 4. SpO2 & cardiac monitoring 5. D'stix stat. Give D50 if hypoglycaemic. 6. IV fluid : restrict to 1/3 to 1/2 maintenance if suspect increase in ICP. 7. Give toxin antidote (e.g. Naloxone 5-10mcg/kg/dose IM/IV for narcotics) 8. Control seizure if present. 9. Treat underlying cause. 10. Discuss with senior. To ICU. Investigations 1. CBP D/C 2. L/RFT serum osmo 3. Na K Blood gas Ca 4. Sugar 5. NH3 6. Infection screening : Blood x C/ST, urine R/M & C/ST 7. NPA for viral IF+/- Mycoplasma PCR 8. Blood for Viral titre & Throat and rectal swab for virus study 9. Urine & blood for toxicology 10. (Lead) 11. Blood and urine for Metabolic kit (if suspect inborn error of metabolism) 12. CT scan brain urgent. MRI brain to evaluate for demyelination 13. LP contraindicated if signs of increased ICP 14. EEG __________________________________________________________________________________
- 77 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.4.2 FEBRILE CONVULSIONS
Definition 1. Fever > 38 C 2. Age: 6m to 5 yr 3. Duration < 15 min 4. Convulsion: generalized, no focal features. 5. No past history of afebrile seizures 6. No past history of CNS damage 7. No evidence of meningitis/metabolic cause Management 1. DAT if fully conscious 2. Convulsion chart 3. Syr Panadol 10 mg/kg/dose Q4h x 1 day then Q4h prn 4. Identify the focus of infection & treat accordingly. 5. Rectal valium 5 mg prn for convulsions > 5 min Investigations 1. CBP D/C 2. Blood C/ST 3. Na K Blood gas Ca Glucose 4. RFT, LFT 5. NPA x viral IF 6. Urine x R/M & C/ST 7. CXR 8. Consider L.P. if cannot confidently exclude meningitis, especially in those under the age of one CSF x R/M, smear, gram stain Biochemistry C/ST Virus + HSV /enterovirus PCR Refer to Clinical Guidelines on Management of Febrile Convulsion by the HK College of Paediatricians July 2002 for details.
__________________________________________________________________________________
- 78 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.4.3 PROLONGED SEIZURE, SERIAL SEIZURE, CONVULSIVE STATUS EPILEPTICUS
Causes: 1. Meningitis, encephalitis 2. Poisons/drugs * lead 3. Sudden withdrawal of anticonvulsant 4. CNS tumour 5. Metabolic disorder: e imbalance, IEM 6. Hypertension 7. Trauma (intracranial haemorrhage) 8. Idiopathic
Convulsive status epilepticus
1. Convulsive status epilepticus (CSE conventionally defined as epileptic activity persisting for 30 minutes wide spectrum of clinical symptoms Children who fail to respond to initial emergency medication should be managed according to CSE protocol. Treatment should be started without waiting till seizures last beyond 30 minutes. Intravenous lorazepam or diazepam is indicated for the treatment of initial CSE If benzodiazepines fail to control seizures, intravenous phenytoin (preferred) or phenobarbitone is indicated. A trial of intravenous pyridoxine should be given to children under 3 years of age with a prior history of chronic active epilepsy or SE of unclear aetiology.
2. 3. 4.
Management 1. Airway. Left lateral position, suction, oxygen. 2. Check BP and vital signs. Neuro obs Q1H. 3. Check D'stix: if hypoglycaemic, IV D50 2 ml/kg 4. IV fluid (restrict to 60% maintenance) if BP normal 5. Control seizure 6. Discuss with senior. To PICU. 7. Treat underlying cause Investigations: 1. CBP D/C 2. RFT, LFT 3. Na K Blood gas sugar, Ca, Mg 4. NH3 5. Urine & blood for toxicology (*Lead), AED level if known epilepsy 6. Metabolic kit if suspect IEM 7. CT scan brain urgent. 8. L.P. contraindicated if signs of increased ICP 9. Viral titre and virus studies
__________________________________________________________________________________
- 79 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ The following is extracted from Clinical Guidelines on Management of Prolonged Seizures, Serial Seizures and Convulsive Status Epilepticus in Children HK J Paediatr (New Series) 2010;15:52-63
Protocol for in-hospital management of CSE Antiepileptic drug Early SE (within 20/30 min) General measures Airway: oxygen Cardio-respiratory function and regular monitoring: ECG,blood pressure and SaO2 Intravenous access Physical examination and history Blood investigations:AED level (known epilepsy) Blood glucose, blood gas Urinalysis RFT/LFT Calcium and magnesium level (for child under 1 year old) Plasma ammonia Complete blood picture (If pre-hospital benzodiazepine has been given, early initiation of treatment for established SE is recommended) 1-2 ml plasma, 1-2 ml serum and 10 ml urine saved for later analysis Blood culture Investigations Glucostix
__________________________________________________________________________________
- 80 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Established SE (30/60 min) Intravenous* phenytoin (preferred) or / and phenobarbitone (for patients already on phenytoin) Cardio-respiratory function and monitoring Metbolic disturbances should be identified and corrected Arrange ICU admission Intravenous pyridoxine for children <3 yr with unknown aetioloty Call paediatric Fellow Refractory SE Midazolam infusion or or Other medications (propofol, valprote, etc.) can be considered (see text) * Intraosseous route if intravenous route cannot be established ICU care Ventilatory and haemodynamic support Monitor metabolic disturbances and systemic complications Monitor electrolytes andblood gas EEG monitoring Arrange EEG If no contraindication andclinically indicated:neuroimaging +/- CSF studies
(>60/90 min) Thiopentone infusion
Refractory SE
Refractory SE : defined as failure to respond to 2 or 3 antiepileptic drugs in combination with seizure duration of at least 60 minutes. Patient should be managed in the intensive care unit. Metabolic disturbances should be monitored closely and corrected. General anaesthesia should be instituted for refractory SE as soon as possible EEG monitoring is required when managing refractory SE. Midazolam, propofol and pentobarbitone are the drugs of choice in controlling refractory SE. Intravenous sodium valproate can be an alternative to diazepam infusion in refractory SE.
__________________________________________________________________________________
- 81 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Common drugs used in CSE Drug Lorazepam Diazepam Dosage IVI: 0.1 mg/kg (max 4 mg) IVI: 0.1-0.3 mg/kg (max 10 mg) Rectal: 0.5 mg/kg, 10-20 mg for adult Midazolam Buccal: 0.3 mg/kg IVI infusion: 0.1-0.5 mg IVI bolus followed by continuous infusion 1-2 microgram/kg/min and increased as needed to 30 microgram/kg/min Phenytoin IVI: 15-20 mg/kg not faster than 1 mg/kg/min under cardiac monitor
Phenobarbitone IVI: 15-20 mg/kg at a maximum rate 1 mg/kg/min High dose phenobarbitone: 10 mg/kg IVI, repeated every 30 min Thiopentone Propofol Pentobarbitone Sodium valproate Pyridoxine Paraldehyde IVI: 3-5 mg/kg bolus followed by infusion 3-5mg/kg/hr IVI: bolus of 1-2 mg/kg (max 10 mg/kg) followed by infusion of 1-2 mg/kg/hour, to a maximum of 5 mg/kg/hour. IVI: 5 mg/kg loading dose, followed by 1-3 mg/kg/hour IVI: 20-30 mg/kg, periodic dosing (twice per day) may be appropriate if seizures are terminated. If seizure continue, a continuous infusion of 5 mg/kg/hr may be effective. IVI: 50-100 mg Rectal, 0.3-0.4 ml/kg, give with same volume of olive oil
__________________________________________________________________________________
- 82 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
Common anticonvulsants
Drug Indication Daily dose No. of time/day 2-3 Elimination half-life (hr) 8-24 (Chronic) 24-36 (Before autoin-duction) 9-40
Carbamazepine (Tegretol) Tab: 200mg ; CR:200mg; Syr 100mg/5ml Phenytoin (Dilantin) Cap: 30, 100mg; Syr 125mg/5ml Phenobarbitone(Luminal)Tab: 15, 30, 60mg; Elix 60mg/5ml Primidone (Mysoline) Tab: 250mg Valproic acid (Epilim) Tab: 200mg; Syr 200mg/5ml Ethosuximide (Zarontin) Cap: 250mg Clonazepam (Rivotril) Tab: 0.5, 2mg Clobazam (Frisium) Tab: 10mg Diazepam (Valium) Tab: 2, 5mg Rectal: 5, 10mg
Partial ; generalized sz
10-20 mg/kg
Generalized, partial sz
8-10 mg/kg<3 yr 4-7 mg/kg> 3 yr 3-5 mg/kg < 5 yr 2-3 mg/kg > 5 yr 10-20 mg/kg 15-40 mg/kg
Generalized, partial sz
2, or nocte
37-73 > 100 hr in 1st 2 weeks of life 5-10 7-15
Generalized, partial sz 1_ gen epilepsies, myoclonic attacks, generalized & partial sz Absences & myoclonic sz All forms All forms, development of tolerance frequent All forms, mainly status epilepticus
2 2-3
20-40 mg/kg 0.1-0.2 mg/kg 0.5-1.0 mg/kg 0.25-1.5 mg/kg (0.1-0.3 mg/kg iv; 0.25-0.5 mg/kg rectal)
1-2 2 2
20-40 20-30 10-30 10-20
__________________________________________________________________________________
- 83 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Nitrazepam Infantile spasm, myoclonic 0.25-1.0 mg/kg Tab: 5mg epilepsies Lamotrigene(Lamictal) Tab:50mg Gabapentin (Neurontin) Cap:100,300,400mg Vigabatrin (Sabril) Tab: 500mg Partial, generalized sz 2mg/kg, increase to 5-15mg/kg If used with valproate, begin 0.5mg/kg, to 1-5mg/kg Begin 300mg, increase by 300mg every 3-5 days. Max 900-1200mg (Adult) 40-80 mg/kg 100-150mg/kg (in infantile spasm) 2 2
Partial, generalized sz Partial, generalized sz; Infantile spasm
3 2
5-7 5-7#
# Not significant, as the drug binds irreversibly to glutamate transaminase, thus _ the brain GABA level; the important half-life is that for restoration of the enzyme level.
__________________________________________________________________________________
- 84 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
SECTION 3.5: GENERAL PAEDIATRICS
__________________________________________________________________________________
- 85 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.5.1 DIARRHOEA
DDx of acute diarrhoea: 1. Gastroenteritis - bacterial, viral, parasitic 2. Food poisoning 3. Systemic infection (especially in young infants) 4. Others : antibiotics-associated, Hirschsprung colitis.. 5. Watch out for intussusception Consider any of the following as possible indicators of diagnoses other than gastroenteritis: C C 1. Fever: 38 or higher in children <3 months or 39 children >3 months 2. Shortness of breath 3. Altered conscious state 4. Neck stiffness 5. Bulging fontanelle in infants 6. Non-blanching rash 7. Bloody diarrhoea (red currant jelly stool) 8. Bilious (green) vomit 9. Severe or localised abdominal pain 10. Abdominal distension or rebound tenderness. Management 1. Contact precaution for rotavirus, norovirus, salmonella in a diapered or incontinent child, Salmonella typhi. 2. ORS (oral rehydration solution) for mild/ moderate dehydration Rehydration therapy Mild to moderate dehydration:
50ml/kg ORS within 4 hours
Start maintenance therapy (100 ml/kg for infants) after signs of dehydration have gone. Maintenance fluids can be given as breast milk, formula, or other fluids appropriate for age, offered ad libitum. Ongoing losses - can be replaced by normal diets given ad libitum in children with mild diarrhea and no signs of dehydration - For those with persistent profuse diarrhea or vomiting, replace ongoing loss with ORS: For each watery or loose stool 5ml/kg For each episode of emesis 2ml/kg 3. IV fluid (Deficit + maintenance + ongoing loss) if shock diminished consciousness intractable vomiting massive stool output Refer to section on "Fluid and electrolytes". In infants less than 3 months old with significant diarrhoea
4.
__________________________________________________________________________________
- 86 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Perform blood x C/ST even when afebrile If fever + bloody diarrhoea, consider full sepsis workup (Blood x C/ST, LP, tap urine) and start IV antibiotics 5. Antibiotics are not recommended for uncomplicated diarrhoea.
Pathogen Salmonella
Campylobacter
Shigella
Indication for antibiotics : Consider in young infants < 3 months, any ill or septic looking patient and immunocompromised patient Salmonella typhi Only of value if given early In institutional settings to shorten bacterial excretion In ill patients Those still symptomatic when pathogen is detected
Drug of choice 3rd generation cephalosporins (or oral Ciprofloxacin 15 mg/kg/dose BD in Salmonella typhi) Erythromycin Co-trimoxazole
Clostridium difficile Giardiasis Amoebiasis
Stop associated antibiotics. Metronidazole 30mg/kg/day Q6h If fails, use Vancomycin po 40mg/kg/day Q6h (Max 2g/day) Metronidazole 15mg/kg/day TDS Metronidazole 50mg/kg/day TDS
6. Antidiarrhoeal agents are not recommended for acute diarrhea in children. They should not be used in children with fever, toxaemia or blood in stool. Investigations 1. CBP D/C 2. Blood x C/ST (if febrile or < 3 months old) 3. Na K Blood gas 4. Urea creatinine 5. Stool x C/ST, virus 6. Fresh stool x ova & cyst (Giardia, amoeba) References Guidelines for the Management of Acute Diarrhoea in Young Children by the HK College of Paediatricians July 2003 NICE guidelines (last update Oct 2010)
Dr A Tsang, June 2003 Updated by Dr R Wong, October 2010
__________________________________________________________________________________
- 87 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.5.2 FLUID AND ELECTROLYTES
Maintenance requirement 1. Fluid Holliday-Segar method:estimates caloric expenditure from weight alone and assuming that for each 100 calories metabolized, 100 ml water will be required. Not suitable for neonates < 14 days. BW 1st 10kg 2nd 10kg Each additional kg Fluid maintenance (ml/kg/day) 100 50 20
Example: 8 year old weighing 25 kg 1st 10 kg: 100 ml x 10 = 1000ml 2nd 10 kg: 50ml x 10 = 500ml additional 5 kg: 20ml x 5 = 100ml
Total = 1600ml/day
Body surface area method: assuming caloric expenditure is proportional to surface area. Should not be used for children < 10kg. Water required = 1500ml/m 2/day (Insensible water loss = 400ml/m 2)
Body surface area = square root of (height in cm x body weight in kg) divided by 60
2. Sodium 3. Potassium
2 - 3 mmol/kg/day 2 mmol/kg/day
* 5.85% NaCl 1 ml = 1 mmol Na * 14.9% KCl 1 ml = 2 mmol K Commonly used IV fluids Dextrose solutions : 5%, 10% (D5, D10) Normal saline (NS): 0.9% NaCl 1/5 solution: NaCl 0.18%+ Dextrose 4.3% (Na 31 mmol/L) 1/3 solution : NaCl 0.3% + Dextrose 3.3% (Na 51 mmol/L) 1/2 : 1/2 solution : NaCl 0.45% + Dextrose 2.5% (Na 77 mmol/L) Others Hartmanns solution : Na 131 mmol/L, K 5 mmol/L, Cl 111 mmol/L, lactate 29 mmol/L, Ca 2 mmol/L 8.4% sodium bicarbonate ( 1mEq/ml) : Na 1000 mmol/L, HCO3 1000 mmol/L 3% NaCl : Na 513 mmol/L, Cl 513 mmo/L
__________________________________________________________________________________
- 88 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
Principles of management 1. Total fluid required = Maintenance requirement + Deficit replacement 2. Calculate the amount of water, sodium and potassium required over a 24 to 72 hour period. The speed of rehydration depends on the type of dehydration, chronicity of the problem and whether patient is acutely symptomatic. 3. Symptomatic hyponatremia and hypernatremic dehydration demands extra caution for fear of central pontine myelinosis and cerebral edema respectively. 4. Extreme caution where there is cardiac failure &/or renal impairment Assessment of degree of dehydration % dehydration Mild (~ 5%) Clinical signs HR 10-15% above baseline Slightly dry mucous membrane Concentrated urine Increased severity of above Decreased skin turgor Oliguria Sunken eyeball/ anterior fontanelle Marked severity of above signs BP drop Delayed capillary refill Acidosis (large base deficit)
Moderate (6-9%)
Severe (10% or more)
Parenteral rehydration Phase 1 Where necessary, rapid volume expansion to improve circulation & renal function: 10 - 20 ml /kg bolus NS IV Phase 2 1. Calculate deficit Volume of rehydrating fluid (ml) = BW (kg) x % dehydration x 10 2. Add on maintenance requirement and ongoing losses. 3. Rate of rehydration depends on type of dehydration:
__________________________________________________________________________________
- 89 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Case Examples 1. Normonatremic dehydration 10kg infant with gastroenteritis presented with vomiting and diarrhoea for 3 days. Estimated to have 10% dehydration. Na 140. K 3.6. Urea 6.5 Water (ml) BW x 100ml/kg for 10% dehydration = 10kg x 100ml/kg = 1000ml Na (mmol) Na deficit associated with the isotonic loss of fluid =145 x BW loss (kg) x 0.6 =145 x 10 x 0.1 x 0.6 =87 mmol BW x 3mmol/kg/day =10 x 3 =30 mmol 117mmol
Deficit
Maintenance
Total required
BW x 100ml/kg/day =10kg x 100ml/kg =1000ml 2000ml
Add maintenance potassium: 3-4 mmol/kg/day and monitor RFT. Prescription: 2000 ml fluid + 117mmol Na + 40mmol K per day (i.e. 58 mmol/L Na) = 1/3 solution 500 ml + 5 ml 5.85% NaCl + 5ml 15% KCl added to each pint, run at 83ml/hr Ongoing loss to be replaced accordingly e.g. with ORS. Need careful ongoing careful monitoring of clinical state and serum electrolytes.
2. Hyponatremic dehydration (Na < 130)- correct over 24 hours 10kg infant with gastroenteritis presented with vomiting and diarrhoea for 3 days. Estimated to have 10% dehydration. Na 125. K 3.6. Urea 6.5
Same calculation as case 1 except to add the Na required to correct the hyponatremia (e.g. aim at correcting Na to 135) Na deficit (mmol) = (Proposed serum Na - current serum Na) x BW (kg) x 0.6 = (135-125) x10x0.6 = 60mmol Total Na = 87 + 30 + 60 = 177 mmol Prescription: 2000ml water + 177 mmol Na + 40 mmol K per day = : solution 500ml + 5 ml 15% KCl + 8ml 5.85% NaCl added to each pint, run at 83ml/hr If the patient is symptomatic, correct it with 3% hypertonic saline. Aim at 6mmol rise per attempt. o o Na required to treat symptomatic hyponatremia= target Na rise x BW x 0.6= 6x10x0.6 = 36 mmol Give 72ml half diluted 5.85% NaCl over 30 min to 3 hours depending on urgency of situation.
Hypernatremic dehydration (Na > 150) Circulatory disturbance is seen later as circulatory volume is relatively preserved at the expense of cellular water. Give 1/2NS as the rehydrating solution. Slow correction of rehydration over 48-72 hr. Avoid dropping serum Na >15 mmol/L over 24 hr.
__________________________________________________________________________________
- 90 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Hypokalemia (serum K+ < 3.0 mmol/L)
CAUTION: Administration of Potassium Chloride in undiluted solution or rapid infusion will be fatal Put on ECG monitor, assess heart rate and rhythm & recheck K+ level Identify cause of hypokalaemia Ensure adequate renal function & urine output before K+ replacement Note that serum potassium is a poor indicator of body potassium status.
Potassium Replacement: **Always consider replacement via oral route rather than IV route** Oral Preparation: Syrup KCl 1gm/10ml (1gm = 13.3mmol) Tab KCl 600mg/tab (600mg = 8 mmol) IV Preparation : IV KCl 14.9% (1ml = 2 mmol)
1. Usual daily requirement 2mmol/kg/day over whole day fluid 2. Oral replacement i. Recommended dose 75mg/kg/day (~1mmol/kg/day) in divided dose & adjust accordingly ii. For SYRUP dilute with milk /juice. iii. For TAB SLOW K do not chew/crush to ensure slow release 3. Rapid bolus IV replacement ONLY IF patient is symptomatic or K+ < 2.5mmol/L i. Maximum concentration - Peripheral line : 40mmol/L (14.9% KCl 0.2ml in 10ml IVF) - Central line : 80mmol/L (14.9% KCl 0.4ml in 10ml IVF) ii. Recommended dose 0.5mmol/kg over 1 hr iii. Monitor patient closely vital signs, IV site, serum K+ level
Hyperkalemia 1. 2. 3. 4. 5. 6. Stop all potassium administration ( IV or oral) IV calcium chloride 25mg/kg to antagonize the effect. IV NaHCO3 1 mEq/kg IV insulin glucose insulin 0.1 unit/kg + glucose 0.5g/kg Promote potassium excretion by resin, dialysis or hemofiltration Treat underlying cause.
Metabolic acidosis Metabolic acidosis associated with dehydration will usually resolve with rehydration. Treat only if acidosis is severe especially when there is circulatory impairment. HCO3 (mmol) = Base deficit x BW (kg) x 0.3 Usually give half the dose.
__________________________________________________________________________________
- 91 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.5.3 CHILD ABUSE
Cases of suspected abuse can be admitted directly to the ward through the Medical Co-ordinator of Child Abuse, MCCA (Dr Patrick Ip, Dr Anita Tsang or Dr Maria Wong) or the 2nd call MO, without going through the A&E. Refer to SWD Procedures for handling Child Abuse cases for details. (Available on CMS station: click HA intranet home page> Manuals/Guidelines> A&E > Child Abuse)
Physical abuse
Suspect physical abuse if the following features are found: 1. Fractures in a child < 2 years old 2. A history inconsistent with physical findings 3. A history of repeated accidents 4. Delay in seeking medical help 5. Multiple injuries and bruises ( especially bruises around face and mouth, over back) 6. Signs of emotional deprivation, neglect or failure to thrive 7. Retinal haemorrhages in the absence of head injury - "Shaken baby syndrome" Management 1. Take a full history. Note especially : Mode of injury & antecedent events(severity) Previous abuse history(frequency) Psychosocial background(assess risks and resourcefulness) Prior contact with social services 2. Thorough PE. Look carefully for any hidden injuries (e.g. bruises behind the ears, torn frenulum, pharyngeal injuries). Document all the injuries precisely with diagrams and clinical photos (obtain consent). Chart growth parameters. Look for retinal haemorrhages in inflicted head injury. 3. Avoid confrontation and repeated interrogation, but be honest. Tell the parents that notification is being made. Explain the assessment procedure. 4. Consult MSW fax the notification form to MSW. May consult Family and Child Protective Services Unit of Social Welfare Department (FCPSU, SWD) directly if required. (FCPSU CWSI : Telephone no. 9460 4013, 2835 2733) 5. Consult Child Psychiatrist. 6. Consult Eye or other specialists if indicated. 7. Notify Police (after discussion with team-head +/- social worker). Consult Child Abuse Investigation Team (CAIU, Police)/Child Protection Special Investigation Team (CPSIT = CAIU + FCPSU) in serious abuse (OC CAIU HKI: Telephone no. 2860 7815, 2860 7814). 8. Investigations if indicated: CBP D/C PT APTT ( if there is history of bleeding tendency) L/RFT Skeletal survey (for those under 2 years old) CT scan brain ( if suspect intracranial injury) 9. Multidisciplinary Case conference (MDCC) - Welfare of the child is the primary concern
__________________________________________________________________________________
- 92 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
Child Sexual abuse ( Victims < 18 years old)
In handling child sexual abuse, consult MCCA if in doubt . Assessment after admission (most relevant to adolescent victims) 1. Attitude Be sensitive and supportive. Experiencing sexual assault is a traumatic experience. The investigation for sexual assault can be equally traumatic if not handled properly. Be non-judgemental. The victim must never be blamed for invoking the incident even though they may be involved in high risk behaviour. 2. Requiring the child to describe the abuse incident(s) repeatedly should be avoided as far as possible and the number of examination should be kept to the minimum. 3. Consent The patient and parents/guardian should be given full explanation of the medical evaluation and consent obtained whenever appropriate or possible. History 1. The Incident Gather information from the referrer and parents. Do not enquire into the details of the incidents. Avoid contaminating the evidence. Obtain essential information of the incident that is relevant to the immediate well-being of the patient : i. Form of assault fondling, genital contact, vaginal/anal penetration ( detail not necessary) ii. Immediate symptoms after the incident pain, bleeding, discharge iii. ? intoxicated just before the incident 2. Medical history Menstrual history: LMP Sexual history, use of contraception, history of STD and pregnancy Use of cigarette, alcohol, substance Past health Physical Examination Allow the child to have a trusted adult accompanying him/her during PE. Explain to the child what you are going to do. Be gentle. General PE to identify injuries or conditions that require immediate treatment Consult Gynaecologist if immediate medical attention is required for significant genital injuries Genital examination or colposcopy should be performed by trained personnel. Consult Forensic Pathologist (through Police) if sexual assault occurred within 72 hours prior to admission.
Investigations Pregnancy test Toxicology screen if indicated Screening for sexually transmitted diseases o HVS for gram smear and culture, Trichomonas vaginalis o Urethral( for male) and endocervical swab for N. gonorrhoea, Chlamydia culture and IF/PCR o Throat/pharynx/rectal swab for gonorrhoea if needed o VDRL o HIV serology
__________________________________________________________________________________
- 93 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
Medical Treatment Emergency contraception o Preferred: Levonorgestrel 1.5mg po once ( or 0.75mg po 12 hours apart) o Alternative: Eugynon 2 tab 12 hours apart po for 2 doses ( 1 tab = Norgestrol 0.5mg + ethinylestradiol 0.05mg)
Pre-emptive treatment for STD: o Ceftibuten 400 mg orally in a single dose OR Ceftriaxone 250 mg imi single dose (for gonorrhoea) o Doxycycline 100mg BD po for 7 days OR single dose of Azithromycin 1gm ( for Chlamydia)
Other management: 1. Consult MSW. Consult FCPSU. 2. Notify Police. CAIU(Police) & FCPSU(SWD) will form CPSIT to conduct the video-recorded interview. 3. Consult Child Psychiatrist.
Discharge and follow up For adolescents, FU Adolescent Clinic in 4 weeks to see if menses return. Repeat serology test at 12 weeks. Monitor for psychosocial issues.
Dr A Tsang Updated October 2010
__________________________________________________________________________________
- 94 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.5.4 URINARY TRACT INFECTION
Common presentation: infants unexplained fever; older children typical symptoms & signs Diagnosis of UTI 1. Screening tests (non-invasive collection method including bag urine): 2. Dipsticks for leucocyte esterase and nitrite; microscopy for pyuria (WBC >10/HPF) 3. Any of these positive should lead to confirmatory tests 4. Confirmatory tests: Urine collection method < 12 months: suprapubic aspiration, catheterized urine, clean catch urine > 12 months: clean catch urine, midstream urine, catheterized urine Sent for microscopy, leucocyte esterase, nitrite and culture Diagnosis: symptoms, signs, urinalysis results and positive culture Treatment of acute infection 1. Clinically treated as upper UTI if fever 380C or loin pain / tenderness 2. Identify G6PD deficiency 3. If < 3 months or seriously ill: IV cephalosporins or aminoglycoside for 7-10 days 4. If > 3 months: oral antibiotics for 7-10 days If oral antibiotics cannot be used, use IV antibiotics for 2-4 days, followed by oral antibiotics for total 10 days Subsequent workup USG
MCUG DMSA (prophylaxis: Zinnat 10 mg/kg) (4-6 months after infection) Girls < 3yrs All Atypical UTI or recurrent UTI or Atypical UTI or recurrent UTI or Abnormal USG VUR grade 3-5 Boys < 3yrs All Atypical UTI or recurrent UTI or All Abnormal USG or Abnormal DMSA > 3yrs All No Recurrent UTI Prophylactic antibiotic with trimethoprim 2mg/kg nocte if VUR grade 3-5 Definition of Atypical UTI Seriously ill Poor urine flow Abdominal or bladder mass Raised serum creatinine Septicaemia Failure to respond to treatment with suitable antibiotics within 48 hours Infection with non-E.coli organisms Definition of Seriously ill Unable to arouse or if aroused does not stay awake Weak high-pitched or continuous cry Pale/mottled/blue/ashen Reduced skin turgor Bile-stained vomiting Moderate or severe chest indrawing Respiratory rate > 60/min Grunting Bulging fontanelle Appearing ill to a healthcare professional Infants < 3 months old with > 380C and infants aged 3-6 months old with > 390C Ref: 1. Wong SN et al (2010). Pediatr Nephrol 25:2083-2091 2. WONG SN ET AL (2009). HK J PAEDIATR 14:74-85 Dr S Chim, October 2010 __________________________________________________________________________________
- 95 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.5.5 NEPRHITIC SYNDROME
Most common cause: acute post-streptococcal GN Clinical features: haematuria, proteinuria, hypertension, oedema, oliguria and renal insufficiency
Management 1. Renal chart 2. Strict I & O 3. BP/P Q1-4h 4. Bed rest if hypertensive or with significant oedema 5. Restrict fluid: insensible water loss (400 ml/m2/day) + previous day urine output 6. Low salt diet 7. Oral Penicillin 50 mg/kg/day QID x 10 days 8. IV Lasix 1-4 mg/kg/day Q6h to promote diuresis 9. Control BP by Nifedipine (Adalat) 0.25 mg/kg/dose. Investigations 1. CBP D/C, ESR 2. LFT, RFT, albumin, Ca PO4 3. Blood gas Na K Ca 4. C3 C4, ANA, anti-dsDNA, Ig GAM 5. Streptozyme 6. Viral titre (including Hepatitis B markers) 7. Urine x R/M C/ST 8. 24 hour urine x protein & creatinine 9. Throat swab x C/ST 10. CXR
__________________________________________________________________________________
- 96 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.5.6 ACUTE POISONING
Resource: HA Toxicology Service Tel 2635 1111 Fax 3513 5649 Website Ha.home/hkpic
HK Poison Information Center (HA) PWH Poison Treatment Center Toxicology Reference Laboratory HAHO Duty Officer
2632 6209 2990 1941 71163328 call 999
2145 7160 2990 1942 trl.home
eKG : Toxicology
Toxic syndromes (Toxidrome) Sympathomimetic (e.g. aminophylline, amphetamines, caffeine, cocaine)
Opioid (e.g. codeine, Lomotil, Heroin, morphine)
Agitation Diaphoresis Fever Mydriasis Tachycardia
Respiratory depression Miosis Coma Bradycardia
Anticholinergic (e.g. antihistamines, Tricyclic antidepressants
Cholinergic
D-efecation U-rination M-iosis, muscle fasciculations, muscle weakness B-ronchorrhea, bradycardia, bronchospasm E-mesis L-acrimation S-alivation
Blind as a batmydriasis Dry as a bonedry skin Hot as Hadesfever Red as a beetred Mad as a hattercentral nervous system stimulation Decreased gastrointestinal motilitydecreased bowel sounds Urinary retentionfull bladder
__________________________________________________________________________________
- 97 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Agents that cause seizure
Pphenothiazine, phencyclidine, pesticides, propranolol Llithium, lidocaine, lindane Aanticholinergics, alcohol withdrawal, amphetamine Ssalicylate, sedative-hypnotic withdrawal, sympathomimetics, strychnine Ttheophylline Iinsulin, isoniazid Ccarbon monoxide, camphor, cocaine
Principles of Management A. resuscitationattention to the ABCs (airway, breathing, and circulation) and D (disabilityaltered mental status and seizures), B. decontamination, C. administration of specific antidotes, D. enhanced elimination, and E. supportive care. Identify the suspected poison Note the dose, likely time of ingestion
GI decontamination 1. Gastric lavage Performed when risk of toxicity is high, likelihood of recovering toxin is high, or other treatment modalities are unavailable Certain agents such as anticholinergic agents or opioid agents may delay gastric emptying and slow GI transit time -may remain in the stomach for more than an hour and available for removal by lavage. Contraindicated in caustic/hydrocarbon ingestion Airway protection important Lavage with NS 15 ml/kg/cycle (max 200-400 ml in adult) till clear.
2. Activated charcoal (Mainstay of treatment) Dose: (1 g/kg in water slurry diluted at least 1:4) Small children : 15-30 g po Adolescents: 50-60 g po *Emesis (Ipecac) No longer recommended. Contraindicated in unconscious/convulsing patient, ingestion of caustics/acids, TCA Enhanced elimination 1. Forced alkali diuresis -May be effective in salicylate or phenobarbital overdoses 2. Haemodialysis 3. Hemoperfusion __________________________________________________________________________________
- 98 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Specific antidote
Substance Acetaminophen Antidote/ Dose N-acetylcysteine IV: 150 mg/kg over 15 min, then 50 mg/kg over 4 hr, then 100 mg/kg over 16 hr PO: 140 mg/kg load, then 70 mg/kg/dose every 4 hr for 17 doses Anticholinergic agents (eg, atropine) Physostigmine Child: 0.5 mg IV slowly Adult: 2 mg IV slowly Benzodiazepines Flumazenil Child: 0.01 mg/kg IV slowly every min (max 1 mg) Adult: 0.1-0.2 mg IV slowly every min (max 1 mg) SE: cholinergic symptoms occur with excessive dosing. Titrate to effect or maximal dose. May not reverse respiratory depression. If positive response is of short duration, may give a continuous infusion. SE: withdrawal symptoms in dependent or chronic use; seizures or dysrhythmias in cyclic antidepressant overdose. Can repeat dose every 2-3 min until response or max dose. If no response to total 10-mg dose, unlikely opioid intoxication. If positive response is of short duration, may give a continuous infusion. In setting of possible opioid dependence, consider initial dose of 0.05 mg to avoid withdrawal. SE: opioid withdrawal (piloerection, agitation, vomiting). Cholinergic agents (eg, malathion) Atropine Child: 0.02 mg/kg IV initial dose (minimum 0.1 mg) Adult: 0.5-1 mg IV initial dose Pralidoxime Child: 25-50 mg/kg over 30-60 min, then 20 mg/kg/hr Adult: 1-2 g IV over 15-30 min, then 0.5 g/hr Double dose every 3-5 min. Titrate to reduced bronchorrhea or improved oxygen saturation. May require total doses 5 or 10 times the initial dose or higher. SE: anticholinergic toxicity. Pralidoxime should be administered in addition to atropine. Continue therapy for 24-72 hr. May repeat dose after 15 min. Remarks SE: vomiting (PO); anaphylactoid reaction (IV). IV protocol requires large volumes of free water, may cause hyponatremia and seizures in children.
Opioids
Naloxone 0.5-2 mg IV/IM/SC/ET (max 10 mg)
__________________________________________________________________________________
- 99 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
General supportive measures: 1. Maintain Airway, Breathing, Circulation. 2. NPO 3. IV fluid 4. BP/P/RR/SaO2 monitoring/cardiac monitoring or neuro-observation Q1h till stable Investigations 1. CBP D/C 2. Na K Blood gas 3. Blood sugar 4. L/RFT 5. Drug level if indicated e.g. salicylate, paracetamol, theophylline or anticonvulsants (arrange with lab for urgent test) 6. Blood, urine, gastric lavage for toxicology 7. ECG 8. (Urine for pregnancy test) Psychosocial assessment 1. Psychosocial history -HEADSS H: Home E: Education, Employment A: Activities D: Drugs S: Sex S: Suicide 2. Consult Psychiatrist for all cases of drug overdose. 3. Consult MSW if necessary. 4. Watch out for child abuse.
__________________________________________________________________________________
- 100 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Acute Acetaminophen (Panadol) overdose 1. Stages of acute acetaminophen poisoning Stage I II III Time Post-ingestion 0-24 hr 2472 h 72-96 hr Clinical features Anorexia, nausea, vomiting RUQ abdominal pain (common) AST, ALT, and, if poisoning is severe, bilirubin and PT elevated Vomiting and symptoms of liver failure Peaking of AST, ALT, bilirubin and INR Sometimes renal failure and pancreatitis Hepatic dysfunction resolves or progress to multi-organ failure ( sometimes fatal)
IV
> 5 days
2.
Likelihood and severity of toxicity predicted by i. Amount ingested : Toxic dose : 150 mg/kg (about 7.5 g in adults) within 24 hours ii. plasma acetaminophen level (More accurate) For a single acute overdose of traditional or rapid-relief acetaminophen (absorbed 7 to 8 min faster), measure level at 4 h after ingestion and plot on the nomogram (Check BNF in ward). Hepatotoxicity is very unlikely if level 150 g/mL ( 990 mol/L) and absence of toxic symptoms. Higher levels indicate possible hepatotoxicity. For a single acute overdose with extended-relief acetaminophen (which has 2 peak serum levels about 4 h apart), measure levels at 4 h after ingestion and 4 h later; if either level is above the Rumack-Matthew line of toxicity, treatment is required.
Antidote: N-acetylcysteine (NAC) most effective if given within 8 hours of ingestion. After 24 hours, questionable benefit. Therapy 1-4 hr of ingestion: Give charcoal and draw level at 4 hrs > 4 hr of ingestion : Draw level and treat with NAC (* Charcoal adsorbs oral NAC; avoid simultaneous administration) Oral NAC (PO/ NG): Give NAC diluted 1:4 in carbonated beverage/fruit juice as a loading dose of 140 mg/kg, then 70 mg/kg Q4H for 17 doses. If vomiting occurs within 1 hr of ingestion, repeat the dose. IV NAC : (20 % NAC solution) Give 150 mg/kg in 200 ml D5 over 15 min. Then 50 mg/kg in 500 ml D5 over 4 hr, then 100 mg/kg in 1000 ml D5 over next 16 hrs. Small risk of anaphylaxis Check plasma level at 24 hrs.
3. 4.
__________________________________________________________________________________
Liver failure is treated supportively. Patients with fulminant liver failure may require liver transplantation.
- 101 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
Rumack-Matthew nomogram for single acute acetaminophen poisoning. Semilogarithmic plot of plasma acetaminophen levels vs time. Cautions for use of this chart: (1) The time coordinates refer to time of ingestion. (2) Serum levels drawn before 4 h may not represent peak levels. (3) The graph should be used only in relation to a single acute ingestion. (4) The lower solid line 25% below the standard nomogram is included to allow for possible errors in acetaminophen plasma assays and estimated time from ingestion of an overdose. Adapted from Rumack BH, Matthew H: Acetaminophen poisoning and toxicity. Pediatrics 55(6): 871876, 1975.
__________________________________________________________________________________
- 102 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
SECTION 3.6: PAEDIATRIC HAEMATOLOGY & ONCOLOGY
(Extracted from Manual of Paediatric Haematology/Oncology/Immunology by Dr GCF Chan, Dr SY Ha, Dr TL Lee and Professor YL Lau, April 2003, Protocol on neutropenic fever updated in 2009)
__________________________________________________________________________________
- 103 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.6.1 MANAGEMENT OF NEUTROPENIC FEVER
Definitions: a. Neutropenia: Absolute neutrophil count (ANC) <1x109/L b. Fever: Core temperature >=38.5oC once, or >=38oC twice in 1 hour Neutropenic fever is an oncologic emergency as infection (especially by Gram negative bacteria) can progress rapidly resulting in significant morbidity and mortality. Investigations: a. Evaluate the patients condition, paying particular attention to vital signs and possible source of infection, which commonly include oral mucosa, perineal/perianal area, and central or peripheral venous catheter exit sites. b. Blood cultures from central venous catheter (2 sets, aerobic cultures only) For bi-luminal central venous catheter, take blood culture from both lumens. For single lumen central venous catheter, take blood culture from the lumen and inject into 2 aerobic culture bottles. 3 5 ml blood for each blood culture bottle Peripheral blood culture is not required for the usual case of neutropenic fever at first instance. Peripheral blood culture may be required subsequently to distinguish catheter-related infection from genuine bacteremia. c. Other investigations according to possible focus of infection Anti-microbial treatment: Commence broad-spectrum antibiotics within 1 hour of fever onset (after patient evaluation by house-officer/medical officer and blood cultures) First-line antibiotics: Tazocin 90mg/kg iv Q6H (max single dose 4.5g) Use meropenem 20mg/kg iv Q8H (max single dose 2g) instead of tazocin in the following situations: 1. life-threatening sepsis, hypotension or septic shock 2. history of infection with ESBL producing organisms or suspected infection with such organisms 3. Allergy to penicillin or cephalosporin Add amikacin 20mg/kg iv Q24H (max single dose 1.5g) in the following situation: 1. history of Pseudomonas infection or suspected Pseudomonas infection Add vancomycin 10-15mg/kg iv Q6H (max single dose 500mg) in the following situations: 1. life-threatening sepsis, hypotension or septic shock. 2. severe mucositis 3. blood or site-specific isolates of MRSA, coagulase-negative Staphylococcus, Enterococcus, Bacillus or Gram positive cocci or bacilli pending identification (repeat line culture before starting vancomycin, if repeated culture is negative in 2 days, stop vancomycin) 4. obvious catheter-related infection (ie. tunnel or exit site infection) or soft tissue infection. As patients condition can change rapidly, patient should be reassessed at 4-6 hours after the first evaluation. Familiarize with management of septic shock and establish early communication with senior colleagues on unstable cases. If fever persists after 48-72 hours, repeat blood culture and consider switching tazocin to meropenem, adding amikacin and/or vancomycin __________________________________________________________________________________
- 104 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ If fever persists after 4-7 days, repeat blood culture for bacteria and fungus and consider adding empirical antifungal therapy with either: 1. Caspofungin 70mg/m2 iv loading dose on Day 1 (max single dose 70mg), then 50mg/m 2 iv Q24H (max single dose 50mg); OR 2. Ambisome 3mg/kg iv Q24H for young children <17kg Alternative antifungals include: 1. Itraconazole 2.5mg/kg iv Q12H (max single dose 200mg), may decrease to 2.5mg/kg iv daily after 2 days 2. Amphotericin B 0.5-1mg/kg iv Q24H, infuse over 4-24 hours, with premed piriton 0.1-0.2mg iv and pethidine 0.5-1mg/kg iv with or without hydrocortisone 0.5-1mg/kg iv Timing of Stopping Antibiotics if no positive blood culture a. ANC<0.5: If afebrile for 3 consecutive days, can stop antibiotics one at a time (if >1 antibiotics). If afebrile for 5 consecutive days, can stop all antibiotics. b. ANC>0.5: Can stop antibiotics if afebrile Microbiologist should be consulted in case of persistent fever, or problems in cultures or antibiotic regimen.
References : Paul M, Schlesinger A, Grozinsky S, et al. Beta-lactam versus beta-lactam-aminoglycoside combination therapy in cancer patients with neutropenia. Cochrane Database of Systematic Reviews 2009, 3. 2. Paul M, Borok S, Fraser A, et al. Additional anti-Gram-positive antibiotic treatment for febrile neutropenic cancer patients. Cochrane Database of Systematic Reviews 2009, 3. 3. Goldberg E, Gafter-Gvili A, Robenshtok E, et al. Empirical antifungal therapy for patients with neutropenia and persistent fever: systematic review and meta-analysis. European Journal of cancer 2008; 44: 2192-2203. 4. NCCN Practice Guidelines in Oncology. Prevention and treatment of cancer related infections. http://www.nccn.org/professionals/physician_gls/PDF/infections.pdf.
1.
Updated Oct 2009
__________________________________________________________________________________
- 105 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.6.2 MANAGEMENT OF HAEMOPHILIA
A. The desired level of coagulation factors to be achieved : Minor trauma / Haemorrhage Dental extraction / Minor Surgery Severe haemathrosis / bleeding Major surgery / serious accidents 20 30 30 80 to 30% to 80% to 80% to 100%
B. Dose Calculation of coagulation Factors No of unit required = % rise required x wt. in Kg *K *K : Factor VIII : 2.0, Factor IX : 1.0 ie. A 10 Kg boy with Haemophila A & acute haemarthorsis of left ankle No. of unit required = 50 % x 10 / 2 = 250 units But if it is Haemophilia B, then it will be 50% x 10 / 1.0 = 500 units * Factor VIII is given by IV bolus q8 - 12 hrs * Factor IX is given daily or q12 hr due to its longer half life C. Measure of response Response = Measured rise x weight in kg Units given
i.e after the above 10kg boy was given 250 units of Factor VIII, the 1 hr post-level was 45%. Response = 45x 10kg /250 =1.8 (up to 1.5 is acceptable) Since the maximum response is 2, 1.8/2 x 100% = 90% response (if <75% rise, has to screen for inhibitor) D. Reminder In short, every unit of Factor VIII/kg body weight will increase the plasma Factor VIII level by 2% If in doubt, better treat first ! Double the initial dose at all times (Loading dose) Be careful of thrombosis when using intermediate purity Factor IX concentrate Following major surgery, level should not fall below 50% for at least 10 days For haematuria, treat with forced diuresis first if it is not severe. Beware of urinary tract obstruction when using coagulation factor E. Follow-up guidelines for Haemophilia 3 monthly review Clinical review and *full blood screen (all HIV + patients) 6 monthly review Clinical review and * full blood screen (all severe haemophilia) Annual review Clinical review and * full blood screen ( mild haemophilia) *Full blood screen: CBC, R/LFT, IgGAM, virology(HIV, HCV, HBV), VIII Ab screen __________________________________________________________________________________
- 106 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.6.3 MANAGEMENT OF THALASSEMIA MAJOR
A. Blood transfusion : 1. Use packed red blood cell (pre-filtered : to minimize WBC induced febrile reaction) & preferably less than 10 days old *All scheduled transfusion will be provided with pre-filtered PRBC by Red Cross 2. Amount Volume in ml = [14(expected Hb) - pre-trans Hb] x B.wt. x *4.7 ie. Patient 10 Kg with pre-transfusion Hb of 9 gm/dl [14 - 9] x 10 x 4.7 = 235 ml * 4.7 is a constant which is determined by the PCV of the blood product available Avoid wastage of blood product, the calculated volume should be round off according to the unit volume available. One unit of packed RBC is around 250 - 350 ml. 3. Rate of transfusion : No cardiac problem : 2 -3 hours/unit (max 5ml/kg/hr) With cardiac problem : 2 ml/Kg/hr, may give transfusion 2 weekly Pre-medication : Chlorpheniramine (Piriton) 0.1-0.2 mg/Kg IV or PO 30 min. before transfusion Frusemide (Lasix) 0.5 mg/Kg IV (max. 20mg) at the start of transfusion 4. 5. 6. 7. Transfuse at 4 weekly interval (5 - 6 weekly interval are acceptable) Keep pre-transfusion Hb at 9.5 - 10gm/dl and post-transfusion Hb at 14gm/dl (to suppress marrow hyperactivity) Avoid post-transfusion Hb higher than 15 gm/dl (increase risk of viscosity & thrombosis) No folate supplement once on regular transfusion
B. Desferal Therapy Desferal is a siderophore produced by Streptomyces pilosus, 1 gm of desferal can bind 93 mg of iron. 1. Start desferal treatment when a. Patient is 3-year-old b. Serum ferritin rises > 2000ng/ml c. Transfusions > 20 units 2. Intravenous desferal (during blood transfusion) a. 60 mg/Kg/dose over a minimal period of 10 hrs b. Not to exceed 15 mg/Kg/hr c. Given as piggy-back 3. Subcutaneous desferal (home treatment): aim at serum ferritin between 1000 to 2000 ng/ml a. Average daily dose 20-50 mg/Kg/day b. Usually not recommend to exceed 50 mg/Kg/day c. Preferably 5 to 6 days per week d. Average daily dose (mg/Kg/day) = weekly no. of ampules x 500 BW (Kg) x 7 ie. Patient 50 Kg on 4 ampules/day, 5 days/week 4 x 5 x 500 = 28.6 mg/Kg/day 50 x 7 __________________________________________________________________________________
- 107 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ e. Toxicity index (T.I.) : not to exceed 0.025 to avoid desferal toxicity T.I. = Average daily dose (mg/Kg/day) Ferritin level (ng/ml)* * ferritin in umol/L divided by 2.2 = ng/ml f.. Give vitamin C only if desferal is given (2 - 5 mg/Kg daily, max 200 mg/day) In general, 50 mg for < 10 yrs, 100 mg for > 10 yrs (to augment the renal excretion of chelated iron) (without desferal, vit. C will increase Fe absorption in the gut) g. Recommended desferal dilution : 500 mg / 5 ml distilled water for injection. If develop persistent local reaction, report to the senior doctor. Add hydrocortisone (max. 2 mg/ml) in infusion solution if indicated ie. 4 ampules in 20 ml water and add 40 mg hydrocortisone h. Liver iron assessment: mol/gm x 0.0559 =mg/gm optimal liver iron content : 3 to 7 mg/gm liver iron overload at risk of complications : 7 to 15mg/gm severe liver iron overload at risk of death: > 15mg/gm 4. Continuous intravenous desferal therapy (for high dose treatment) : 50-70 mg/Kg/day Portacath and special infusion set is required
C. Investigations : 1. Before each transfusion : pre-transfusion Hb, cross-match, ferritin level, urine for glucose 2. After transfusion : post-transfusion Hb 3. Every 6 months : serum Ca, PO4, blood glucose, fructosamine, thyroid function, infection screening (HIV, HBV, HCV) 4. Yearly : endocrine assessment, cardiac assessment (MUGA scan, ECG, CXR), serum Zn & Cu eyes & hearing assessment
__________________________________________________________________________________
- 108 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.6.4 MANAGEMENT OF NON-IMMUNE THROMBOCYTOPENIA
1. 2. Exclude immune causes of thrombocytopenia. Keep platelet count >20 x 10^ 9/L in chemotherapy induced thrombocytopenia Give platelet if there is neutropenic fever & platelet <30 x 10^ 9/L If active bleeding present, give platelet even if platelet > 30x 10^9/L Dosage guidelines a. Infant : 10ml/Kg increase platelet count 75 - 100x 110^9/L b. Older child & adult : 1 unit/10Kg B.wt or 4 units/m^2 BSA increase platelet 50x 10^9/L ie. 40Kg boy with platelet count of 10x 110^9/L 4 units of platelet transfusion will increase his platelet count to 60x 10^9/L 4. Detection of platelet refractoriness Check 1 hour post-platelet transfusion platelet level Correct count increment (CCI) = (Post Pre-platelet count) x S.A. no. of platelet transfused *
3.
* no. of platelet transfused = no. of units x 0.55 * for apheresed platelet = no. of units x 3 i.e. SA of 1.5m^2, post-transfusion platelet count 40 x 10^9/L & pre-transfusion count 10x 10^9/L after 4 units of platelet transfusion (40 10) x 1.5 =20.45 x 10^9/L 4 x 0.55 (<7.5 x 10^9/L increment indicates refractoriness)
__________________________________________________________________________________
- 109 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.6.5 MANAGEMENT OF IMMUNE THROMBOCYTOPENIA (ITP) Acute ITP
1. 2. Check complete blood count, blood smear, auto-immune markers (eg. ANA, RF, C3, C4) No specific treatment if there is no clinical evidence of bleeding (except bruises & petechiae) and platelet count is >10 x 10^9/L
Start treatment if : a. Clinical evidence of bleeding with platelet count <20x 110^9/L 1) Nose bleeding cannot be stopped for > 15 min. 2) Oral mucosal bleeding (eg. Gum bleeding, blood retention cyst) 3) GI bleeding (eg. Melena) b. Severe bleeding disregards the platelet count (eg. Intracranial hemorrhage, retinal hemorrhage) Treatment options a. Steroid induces a slower rise of platelet count (median: 4 days) but the effect is more sustained. b. IVIG induces a rapid rise of platelet count (within hours) but the effect is transient (1 to 2 weeks). c. Never give platelet transfusion except in emergency situation (eg. Intracranial hemorrhage). d. Rhogam has similar efficacy as IVIG but is associated with higher incidence of therapy-induced haemolytic anemia Steroid treatment a. Has to perform bone marrow aspirate to rule out leukaemia before starting b. Use prednisolone 2 mg/Kg/day for 2 weeks and then taper over another 1 week c. Monitor BP and urine sugar q2wks d. Advice to take after food intake or with antacid IVIG a. When a rapid rise of platelet is indicated or when there is concomitant active infection (ie. Fever) b. No difference in using small dose (500 mg/Kg) or high dose (2 gm/Kg) c. Give it over one or 2 days rather than 4 days d. Infuse the drug gradually 5 ml/15 min, then 10 ml/15 min, then 15 ml/15 min, then 20 ml/15 min Rest over 4 - 5 hrs e. Pre-medication : Piriton 0.2 mg/Kg 30 min before infusion f. Anti-Rh(D) is a special form of Ig that can be used but is associated with alloimmune haemolysis secondary to anti-Rh(D) and is not indicated for routine clinical use
Chronic ITP (when thrombocytopenia lasts for 6 months or longer)
1. 2. 3. Perform bone marrow aspirate (rule out marrow pathology) No treatment if there is no clinical evidence of bleeding (except bruises and petechiae) and platelet count is > 10x 10^9/L Treatment options Highly controversial with no universally accepted approach Alternate day steroid Vs pulse steroid Splenectomy (if steroid dependent for > 1.5 to 2 years) Cytotoxic drugs
__________________________________________________________________________________
- 110 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.6.6. MANAGEMENT OF TRANSFUSION REACTION
A. Choice of Blood Products 1. CMV negative product Rationale : to prevent CMV infection in severe immuno-compromised patients Indications : CMV neg. patients who will undergo or undergo allogeneic or autologous BMT Source : blood from CMV neg donor or filtered (high efficiency filter) product 2. Filtered product Rationale : to remove white blood cell down to 106/unit Indications : 1) when CMV neg product is needed or 2) recurrent febrile transfusion reaction or 3) Also for severe aplastic anaemia patients awaiting for BMT (WBC sensitization will increase chance of graft rejection ) Source : either pre-storage or bed side filter 3. Irradiated blood (1) Rationale : to prevent transfusion associated graft versus host disease in severe immunocompromised patients by inactivating lymphocytes in donor's blood product
candidates for allogeneic or autologous BMT (D0 to 6 months) 2) severe immunodeficiency 3) intrauterine transfusion 4) transfusion from near relatives even in immuno-competent patients (resemble HLA-Ag may allow donor lymphocytes to escape the detection of recipient's lymphocytes but not vice versa)
Indications : 1)
B. Management of Febrile Nonhemolytic Transfusion Reaction (FNHTR) Background : Most commonly encountered type of transfusion reaction (1%) Definition : 1degree Celsius rise from basal temperature (min. 38C during or within 24 hrs after transfusion with no other medical explanation *It is a diagnosis by exclusion Caused by antileukocyte Ab present in the patient's plasma and release of cytokines from transfused WBC Can be reduced by using leukocyte filter
Management : 1. Exclude other causes of fever 2. Stop the transfusion if fever >38.5C (core temp.) & proceed to sepsis work-up 3. Give Panadol 10-15 mg/Kg PO 4. If fever subsided, can resume transfusion 30 min. later 5. Can be reduced by premedication (piriton) and use of leukopoor filtered product C. Allergic (Urticarial) Transfusion Reaction Background : Almost as common as NFHTR Probably caused by the foreign plasma protein or reagins (IgE or IgG) in the donor's product and triggers histamine & leukotrienes release Usually manifested as itchiness, local erythema and hives with or without fever __________________________________________________________________________________
- 111 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Management : 1. Give antihistamine (Piriton 0.1 to 0.2 mg/Kg/dose) IV 2. If reaction is quite extensive, can add hydrocortisone 2 to 4 mg/Kg IV bolus 3. Stop transfusion if develop anaphylaxis 4. Give O2 and adrenalin 0.01 ml/Kg/dose of 1:1000 s.c. if develop bronchospasm or hypotension Can repeat q15min. for 3 to 4 doses 5. Give volume replacement (10 ml/Kg, any isotonic solution, ie. haemocel, NS) if develop hypotension D. Management of Bacterial Contamination Reaction Background : Around 1 in 2000 for platelet transfusion (due to storage at room temp.) Much less common in whole blood or packed RBC transfusion (stored at 4?C) Bacillus and coagulase neg. Staphylococcus contamination are common for platelet transfusion Pseudomonas sps., E. coli, Yersinia enterocolitica contamination are common for RBC transfusion (bacteria capable of growing in cold temperature (psychrophilic) Septic reactions usually appear rapidly during transfusion (within 30 min.) Manifested initially as fever, flushing, chills, myalgia, GI upset, and hypotension Management : 1. Stop the transfusion 2. Treatment of shock and start broad spectrum antibiotics 3. Blood culture and culture of the blood product bags (microbiology lab.) 4. Inform Blood Bank and send blood specimens for checking of haemolytic reaction E. Management of Acute Haemolytic Transfusion Reaction Background : Uncommon but can be fatal Mainly due to transfusion of incompatible blood product Manifested initially as dyspnoea, chest pain, fever, chills, flushing, backpain, oliguria, generalized oozing, hypotension Management : 1. Immediate procedure : Stop the transfusion and perform clerical checks Monitor vital signs and urine output (by urine catheter) 2. Send blood for direct Coomb's test , compatibility test (pre- & post), blood culture (patient & blood product), coagulation profile, renal function test Repeat coagulation profile and blood chemistry q2-4hrs 3. Forced diuresis (hydration with 125ml/m2/hr isotonic solution then frusemide IV) Preferably monitor the CVP and keep at 5 - 10 cm water) 4. If urine output < 0.5 ml/Kg/hr x 2 hrs, manage as acute renal failure 5. If urine output > 0.5 ml/Kg/hr, adjust intravenous fluid infusion rate accordingly 6. Correct electrolytes and acid base balance 7. If patient is severely anaemic, can give another unit of blood, no increase risk of 2nd reaction
__________________________________________________________________________________
- 112 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ F. Summary Conditions Causes 1. Fever/Chills (FNHTR) Anti-WBC Ab
Onset Management During or within hrs of Paracetamol transfusion Use WBC filter
3. Anaphylactoid reaction 4. Infection septicaemia 5. Intravascular haemolysis
During transfusion
Resuscitation (life threatening)
Contamination ABO mismatch
Within 30 min. after transfusion Often shortly after manage as ARF , DIC transfusion (a few ml)
__________________________________________________________________________________
2. Urticaria
Infused plasma protein or allergens Ab to IgA
During transfusion
Piriton
Hydrocortisone
- 113 -
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
SECTION 3.7 : NEONATOLOGY
114
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.7.1 NEONATAL INFECTION
Onset of infection Early onset infection (first 3 days of life) sepsis screening surface swab blood culture CBP D/C empirical treatment penicillin + gentamicin (if gestational age >34 weeks postnatally) OR cefuroxime (for GA34 weeks or patients with renal impairment or significant asphyxia) consider C-RP (24-48 penicillin / cloxacillin / hours after initial vancomycin + and sepsis screening) if ceftazidime or amikacin short course and antibiotics intended optional investigation consider C-RP (24-48 hours after initial sepsis screening) if short course antibiotics intended
Late onset CBP D/C infection (after 3 blood culture days of life) urine R/M culture CSF R/M culture
Dosage of antibiotics Penicillin G: 25,000-100,000 units/kg/dose IV postmenstrual age (weeks) postnatal age (days) Interval (hours) 0-28 12 29 >28 8 30-36 0-14 12 >14 8 37-44 0-7 12 >7 8 all 6 45 Gentamicin (first week of life). Check serum level if treatment is prolonged (>7days). Postmenstrual age (weeks) Dose (mg/kg/dose) Interval (hours) 34-37 4 36 4 24 38 For dosing after the first week of life, administer an initial dose of 4mg/kg. Dosing interval is guided by serum level. Cefuroxime: 30-50mg/kg/day divided q8-12h IV Cloxacillin: 50-100mg/kg/day divided q8-12h IV Vancomycin: 10-15mg/kg/dose. Serum level should be checked for neonates. Postmenstrual age (weeks) Postnatal age (days) Interval (hours) 0-14 18 29 >14 12 30-36 0-14 12 >14 8 37-44 0-7 12 >7 8 all 6 45
Ceftazidime: 30mg/kg/dose IV Postmenstrual age (weeks) 29 30-36 37-44 45
Postnatal age (days) 0-28 >28 0-14 >14 0-7 >7 all
Interval (hours) 12 8 12 8 12 8 6
115
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Amikacin: first week of life. Check serum level if treatment is prolonged (>7 days). Postmenstrual age (weeks) Dose (mg/kg/dose) Interval (hours) 18 48 27 28-30 18 36 31-33 16 36 15 24 34 For dosing after the first week of life, administer an initial dose of 15mg/kg IV. Dosing interval is guided by serum level. Dr KY Wong May 2002
116
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
3.7.2 MANAGEMENT OF NEONATAL JAUNDICE
New Intervention Guidelines for Neonatal Jaundice, 2010 Please refer to the action guidelines on Indications for Phototherapy (PT) and Indications for Exchange Transfusion (ET) for term and preterm infants (Chart 1). Major changes: (1) intervention based on Total Serum Bilirubin (TSB) which is roughly equal to Bu+Bc. (2) For babies born at or after 35+0 weeks of gestation (the upper two lines), the thresholds of treatment are elevated (compared with old guidelines). (3) In the of presence of risk factors e.g. dehydration, abnormal neurologic behaviour, asphyxia, low serum albumin (if ever measured), temperature instability, G6PD deficiency or other hemolysis settings (maternal blood group O), or follow up cannot be ensured, consider starting intervention at a lower TSB level.
Indications for PT/ET for babies with GA 35 weeks
>37+0 weeks of gestation 24 hours PT level 165 (mol/L) ET 280 level(mol/L) 48 hours 220 325 72 hours 265 370 96 hours 300 385 120 hours 310 385
35+0 36+6 weeks of gestation 24 hours 48 hours PT 130 200 level(mol/L) ET 255 290 level(mol/L)
72 hours 230 315
96 hours 250 325
120 hours 255 325
Day-Phototherapy (K10S) Giving PT during daytime while allowing home leave at night may facilitate breast feeding without adverse effect. Please check BuBc at 4pm and decide on suitability of home-leave during afternoon ward round. Cases with borderline TSB (very near PT level) can be admitted for day-PT.
Stopping PT
PT can be stopped when the TSB level is around 250 mol/L or 30-40 mol/L below PT level, whichever lower. Rebound jaundice TSB should be checked (6-24 hours after stopping PT) if possible, especially when there is a suspicion of hemolysis or if the rise of TSB before PT is significant.
General management of NNJ to be covered in separate file (Appendix 5)
117
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Chart 1. Indications for PT and ET (2009)
Indication for Phototherapy
350 >=37+0w 300 35-36+6w 250 32-34w;1501-2000g umol/L 200 28-31w;1001-1500g 150 <28w;<1000g 100 50 0 0 1 2 3 Days 4 5 6 7
Indication -- Exchange Transfusion
450 400 350 300 umol/L 250 200 150 100 50 0 0 1 2 3 Days 4 5 6 7 >=37+0w 35-36+6w 32-34w;150-2000g 30-31w;1251-1500g 28-29w;1001-1250g <28w;<1000g
118
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
119
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Referral for NNJ Assessment to QMH There are three sites where NNJ can be assessed, depending on opening hours of individual site: Opening hours Monday to Friday 1:30 pm5:00pm; Saturday 9am-12noon 9:00am to 5:00pm, Monday to Friday Other times Eligibility Babies born at QMH and younger than 10 days old All other newborns All newborns
S5 Day service (OBS) K8S Paediatric Day center K10S
Babies can also be followed up at KGOPD as Discharge follow up (DFU). For SYPMCHC where serum bilirubin can be checked and treatment is deemed necessary (according to new guidelines), the patient can be forwarded to K10S directly for admission and treatment. (see Appendix 4) For newborns that require further follow up because of high or increasing jaundice, they can be referred for NNJ assessment as above accordingly. In cases of weekends or long holidays, the baby can be referred to K10S for assessment. The medical record of previous assessment should preferably be provided e.g. jaundice meter level, serum bilirubin level.
Assessment at K8S/K10S (see Appendix 1)
Babies with NNJ referred from MCHC (or S5 occasionally) to K8S/K10S will be seen by interns and Paediatric residents of K10S. PT by biliblanket should be started for babies with JM>22 / 250 (JM102/103) while awaiting TSB results. Serum bilirubin (Bu+Bc) should be checked as early as possible, preferably within 1 hour after admission. Inform paediatric residents (K10S) immediately if JM>24 (280).
120
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
(A) Short term follow up Follow up schedule
Follow up should be ensured for the following categories: When TSB level is close to PT level Less than 20 mol/L below PT level follow up 24 hours 21-40 mol/L below PT level follow up 24 - 48 hours The follow up can be done at Day Service (S5), MCHC, K10S (as day patient), private paediatricians, DFU or NNC (if time slots available) If follow up cannot be ensured, call paediatric resident to consider admission for PT at lower TSB level. Follow up schedule Babies with GA >37+0 then FU in24 hr If TSB at 48 hrs 200-219 TSB at 72 hrs 245-264 TSB at 96 hrs 280-299 TSB at 120 hrs 290-309 Babies with GA 35+0 36+6 then FU in24 hr If TSB at 48 hrs 180-199 TSB at 72 hrs 210-229 TSB at 96 hrs 230-249 TSB at 120 hrs 235-254
FU in 24-48 hr 180-199 225-244 260-279 270-289
*FU routine <180 <225 <260 <270
FU in 24-48 hr 160-179 190-209 210-229 215-234
*FU routine <160 <190 <210 <215
*FU Routine: according to physicians discretion, depending on age of patients, abnormal physical signs, or suspicion of pathological causes of jaundice. (B) Long term follow up Long term follow up should be arranged for patients whose TSB has reached or exceeded Day 4 ET level (e.g. 385mol/L for babies with GA >37 weeks, and 325 mol/L for babies born at 35+0 36+6 weeks) A formal elective BAEP should be booked on discharge to detect hearing loss. Follow up schedule: 1 week after discharge (if jaundice has not yet resolved before discharge) 4 month (with AIMS physiotherapist assessment) 8 month (with AIMS physiotherapist assessment) 12 month (with AIMS physiotherapist assessment). Case can be closed when the childs physical assessment is normal at 12 months old. Kernicterus: Specific movement disorder dystonic cerebral palsy Hearing loss Upward gaze palsy Enamel staining
121
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
Appendix 1 K8S Management of Neonatal Jaundice MCHC A&E Others Jaundice referred for blood test and assessment
Inform Paed resident (Dect 1280) Admit K10S
Yes
PT needed?
* Inform Paed Resident (1280) immediately if baby is ill e.g.lethargic, pale, dehydrated, septic
*Follow up (1) within 20 mol/L below PT level FU 24 hrs (2) 21-40 mol/L below PT level FU 24-48 hrs (3) >40 mol/L below PT level FU routine
No
JM Clinical assessment by intern (General) and K10S Paed. Resident* TSB (Bu+Bc) other blood tests if indicated
JM (103) 250 JM (102) 22 Yes Biliblanket
No
K10S (weekends, PH)
MCHC
Trace blood result Private
Scheduled follow up* 1 day 2 days routine
122
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Appendix 2 S5 (Day service) guidelines for management of babies with NNJ Clinical assessment as usual (history, feeding pattern etc) Checklist for abnormal clinical signs or history body weight loss of >10%; signs of dehydration poor feeding lethargy / irritability / high pitched cry pallor temperature instability G6PD deficiency /maternal blood group O siblings with severe NNJ Jaundice meter (minolta JM 102) Call Paediatric resident immediately if there are clinical suspicion of abnormalities dehydration, irritability, temperature instability Otherwise check TSB (urgent if JM24)
e.g.
Presence of abnormal signs No TSB
Yes
call Paedi and send pt to K8S (for biliblanket PT, assessment and TSB)
PT level
No
within 20mol/L below PT level 21-40 mol/L below PT level >40 mol/L below PT level
FU 24 hours
borderline
Yes
FU 24-48 hours
Routine FU
Inform Paed for admission to K10S Call Paed. resident to consider Day-PT e.g. breast feeding, living far away etc. Ask pt to come early next morning (to K10S) for PT.
123
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
Appendix 3 Referral for Assessment of Prolonged Jaundice
Etiologies (1) Breast milk jaundice (2) Infection especially urinary tract infection, CMV (3) Hemolysis (4) Neonatal hepatitis syndrome (5) Obstructive jaundice e.g. biliary atresia, choledochal cysts (6) Others e.g. Gilbert syndrome, Hypothyroidism, IEM
Jaundice by Day 14 (clinical or JM)
Worrying signs and symptoms e.g. Clay colour stool, hepatosplenomegaly, green hue, poor feeding, pallor, poor wt gain
Yes
No
Breast feeding (solely or partially)
No
Yes Monitor at MCHC by clinical assessment + JM (serum bilirubin)
Day 28 Persistent or progressive jaundice
No
Breast Milk Jaundice
Yes
Refer to QMH as new case (NNC or General) Appointment available in 1-2 weeks Refer to A&E if emergency
124
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
Appendix 4 MCHC Referrals for NNJ Assessment and Treatment (excluding investigations for prolonged jaundice) SYP MCHC Follow Up JM
TSB
PT needed
PT not needed
Refer K10S for admission and PT
Yes
MCHC appointment available
Yes
Follow up needed?
No Consider Follow up at K10S or S5 (Saturday morning, QMH inborn)
No routine
Other MCHC
Referral if JM (103) 220mol/L or JM (102) 20 (similar to referral to PYNEH)
125
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
Appendix 5 Inpatient treatment of NNJ
Assessment of a newborn with jaundice
4.1 History Age (in hours) and gestational age Antenatal risk factors e.g. gestational DM, pregnancy induced hypertension, IUGR, multiple pregnancy, Rhesus incompatibility Peripartum risk factors e.g. prolonged rupture of membrane, delayed cord clamping, traumatic delivery Feeding breast feeding /formula; adequacy of feeds; feeding problems e.g. vomiting, number of bowel motions, use of parenteral nutrition; General signs of well being e.g. general activity, sleeps Drug intake especially herbs, exposure to naphthalene in G6PD deficient subject Neonatal screening results (G6PD, Thyroid function) Family history e.g. NNJ, G6PD deficiency 4.2 Physical examination Confirm jaundice and assess severity Visual (useful but less reliable than transcutaneous bilirubinometry) yellow sclera and skin cephalocaudal progression greenish hue (cholestatic jaundice) pale yellow (with anemia, suggests hemolytic jaundice) Transcutaneous bilirubinometer TcB (e.g. Minolta JM102/103) Good predictor of TSB particularly when TSB level is less than 250mol/L; higher discrepancy in severe jaundice Needs blood tests (TSB) for confirmation and direct treatment, yet obviate the need for blood tests in mild jaundice for infants 35 weeks Not reliable during phothotherapy (recovery needs 18-24 hours) Look for causes of jaundice General status hydration, fever, general activities, features of sepsis, hypothyroidism Head cephalhematoma Skin bruises Abdomen enlarged liver, spleen Enquire /inspect stool and urine colour Look for features of acute bilirubin encephalopathy Fever, poor sucking Conscious state: lethargy irritable; high pitched cry stupor, coma Muscle tone: hypotonia hypertonia, neck stiffness, opisthotonus Convulsion
126
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Further investigations based on clinical suspicion 5.1.1 blood picture, reticulocyte count and smear hemolysis, infection 5.1.2 end-tidal carbon monoxide/carboyhaemoglobin -- hemolysis 5.1.3 blood group, direct antiglobulin test (direct Coombs test) 5.1.4 bilirubin: albumin ratio (an estimation of free bilirubin) 5.1.5 conjugated (or direct reacting) bilirubin and hepatic enzymes when hepatitis or cholestasis suspected unconjugated bilirubin conjugated bilirubin
look for causes of hemolysis or enterohepatic circulation
look for hepatobiliary disease
5.1.6 full liver function tests, including albumin and coagulation profiles when liver disease suspected 5.1.7 sepsis screening including urine and blood culture 5.1.8 viral studies, syphilis serology congenital infection syndrome 5.1.9 imaging of hepatobiliary system for evidence of surgical obstruction endocrine and metabolic screening thyroid function, urine for reducing substance, 1-antitrypsin phenotype etc
127
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Treatment of Neonatal jaundice
The goal of therapy is to prevent bilirubin encephalopathy in high risk infants and avoid unnecessary treatment to low risk infants. Specific Treatment options for unconjugated hyperbilirubinemia 8.1 Phototherapy (PT) blue (special) /green /turquoise /white fluorescent tubes/ fibreoptic biliblankets / LED / tungsten-halogen works by photo-isomerisation and photo-oxidation of unconjugated bilirubin into water-soluble forms (lumirubin) and excreted without need of conjugation effectively reduces need for exchange transfusion higher power (intensity) associated with a quicker fall in TSB o double (two units) or triple (three units) in combinations more effective than single o use of reflective curtain also effective in enhancing phototherapy effect the greater the body surface area exposed, the greater the decline of bilirubin intensive PT (defined as 30 W/cm2 per nm in 430- to 490- nm band) more effective and reduce the need of ET intermittent PT appears to be effective Indications of PT referred to chart for PT Monitoring during PT Regular intake and output, hydration state Body temperature Body weight daily Eye-patch position TSB regularly (every 6-12 hours) Complications usually well tolerated corneal /retinal damage (use eye-shield) increase in insensible water loss (encourage liberal milk intake) hyperthermia/ thermal skin injury (monitor body temperature, use halogen PT units at recommended distance) transient skin rash loose stool bronze baby syndrome (when significant conjugated bilirubin present) rebound hyperbilirubinemia after cessation (especially when there is evidence of hemolysis) bullous eruption in porphyria Discontinuation of PT: Intermittently check TSB to decide for discontinuation of PT at a level that is safe while considering the age, gestation, presence of risk factors, and the possibility of rebound when PT is discontinued. (see practice guideline) Follow up assessment at 12-24 hours may be necessary for high-risk cases. 9 Exchange transfusion (ET) Rapid way of removing serum bilirubin (and antibody-coated red cells) Indications severe or extremely high hyperbilirubinemia (Figure 2 and 4) despite intensive PT, or in addition, a high bilirubin: albumin ratio (Table 1) when there is already evidence of acute bilirubin encephalopathy (ET should be performed for all infants who manifest signs of acute bilirubin encephalopathy even if TSB is falling with PT)
9.1
8.1.1 8.1.2
Table 1. Bilirubin/albumin ratio (B/A) can be added when considering indication for ET B/A mg/dL: g/dL mol/L:mol/L Infants 38 weeks o Well 8.0 0.94 o Hemolysis 7.2 0.84 6 Infants 35-36 /7 o Well 7.2 0.84 o Hemolysis 6.8 0.80 9.2 9.2.1 Procedures (refer to appendix on ET) double blood volume exchange (traditional) single volume exchange: 60% of blood exchange double volume exchange: 85% of blood exchange 9.2.2 use fresh whole blood (<3-5 days) or reconstituted blood components (washed red cells with plasma) 9.2.3 use wild bored intravenous catheters and exchange blood in small aliquots (central or peripheral) 9.2.4 needs cardiopulmonary monitoring during and immediate after the procedure 9.3 Complications varies with different patients status, higher rate in preterm infants 9.3.1 Procedure associated mortality <1% (well term infants) to 12% (ill or preterm infants) 9.3.2 Complications Catheter induced: thrombosis, embolism, bleeding, cardiac arrhythmia Transfusion related: blood compatibility problems, thrombocytopenia, hypothermia, apnea, bradycardia, cyanosis, metabolic acidosis, hypocalcemia, hyperkalemia, necrotising enterocolitis Infection 9.4 Risk and benefit must be weighed and explained to parents before decision for exchange transfusion, and a formal consent obtained The procedure must be performed by trained personnel in a neonatal intensive care unit with full monitoring and resuscitation capabilities
8.1.3
8.2
9.5
128
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ Procedure: Exchange transfusion (ET) Clarify indication and contraindications Obtain consent o Cross match Required volume should be 2 80ml/kg body weight (double blood volume) + dead space of blood tubings (30-50ml) (blood volume of preterm infant is 100-120ml/kg) use type O, Rh compatible blood (with low anti-A and anti-B titre) for ABO hemolytic disease use ABO type specific Rh-negative blood for Rhesus hemolytic disease o Use fresh whole blood (<3-5 days old) or red cells with o Warm blood with blood warmer to 27-37C o Consider white cell filter o Freshly irradiated blood may reduce chance of graft-vs-host disease Preparation of baby o Fast 2-4 hours before procedure. Empty stomach by feeding tube immediately before procedure. o Stabilize vital signs e.g. supplementary oxygen, glucose infusion for hypoglycemia etc. before starting procedure o Place baby under open incubator with radiant heater o Connect baby to continuous cardiopulmonary monitor. o Use restrainer if necessary o Consider setting arterial catheter for continuous blood pressure monitoring or for isovolumetric method (see below) o Keep IV glucose infusion during the procedure if necessary (to prevent hypoglycemia) o Keep baby warm with radiant heat warmer. Do not hang blood pack directly in the heat path of radiant warmer Procedure o Universal precautions, use strict aseptic technique for setting up exchange system. o Prepare Syringes with heparinised saline Appropriate sized syringes (3ml, 10ml or 20ml) for drawing of blood Wastage bag Stopcocks (three ways) X 2 10% Calcium gluconate IV (optional)
129
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
Exchange using umbilical venous catheter (single lumen push-pull method) o set up three-way exchange system as o save the first and last aliquot for investigations shown draw blood from baby slowly push blood into wastage bag draw same volume of blood from donor pack slowly inject blood into umbilical vein over 1 minute watching out for bubbles wait for 30 seconds and repeat above steps until the desired volume exchanged NOTE: patients blood should not be left inside the circuit since it will clot quickly o shake blood pack every 15 minutes to prevent early settling of red cells o Use of calcium gluconate infusion (optional, and may not be necessary in normocalcemic patients): o catheterize umbilical vein preferable in For every 100ml blood exchanged, give 1ml 10% IVC or at a site where blood can easily calcium gluconate IV SLOWLY and CAUTIOUSLY aspirated and infused for more emergency (bradycardia or cardiac arrest if given too quickly) situations (usually 4-5cm from umbilical or give 0.5ml IV slowly for every 50ml exchanged if stump in term infants) baby is small o start aliquots of exchange (aliquot volume followed by SLOW saline flush afterwards should be <10% of blood volume each o monitor babys vital signs throughout the procedure, shift; use lower volume for unstable including central venous pressure if possible. patients) o Expose the baby for easier observation rather than cover >2500gm: 20ml up. 1801-2500gm: 15ml o Accurately document volumes of blood in-and-out, 1201-1800gm: 10ml number of cycles, drugs given and vital signs of baby <1200gm: 5ml o Total duration 90-120 minutes volume of blood withdrawn and o End of exchange transfused must be accurately Send last lot of blood for investigations measured and should be documented Decide the need for second exchange keep umbilical by an assistant catheter if necessary (by saline infusion).
Specimens to be collected
(1) Pre-ET a. Umbilical swab for bacteriology b. Blood for CBC, LFT, blood culture, c. Na K Ca blood gas, spot glucose d. Coagulation profile e. Genetic studies (if necessary) (2) Post-ET a. Blood for CBC, LFT, blood culture, b. Na K Ca blood gas, spot glucose c. Coagulation profile d. Repeat cross match if necessary
Monitoring after exchange
1. Vital signs: continuously for at least 4-6 hours 2. Hypoglycemia (rebound hypoglycemia due to dextrose containing blood preservatives): q2h- q4h blood glucose for 12 to 24 hours 3. Rebound hyperbilirubinemia: check TSB 4-6 hours after procedure while continuing intensive phototherapy 4. Feeding can be resumed 2-4 hours after procedure, and feeding tolerance closely monitored (if umbilical catheters used)
130
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________ 10 Intravenous gammaglobulin (IVIg) has been used effectively to reduce need for exchange transfusion in Rh and ABO isoimmune hemolytic disease dose 0.5-1g/kg over 2 hours; may be repeated in 12 hours if necessary
11 Other drugs 11.1 Metalloporphyrin heme oxygenase inhibitors not yet available 11.2 Phenobarbital has been used successfully for mothers antenatally to reduce the severity of jaundice in fetal hemolytic disease. It has also been used for patients with Crigler-Najjar syndrome. Albumin infusion has not been shown to be effective in reducing bilirubin encephalopathy in well studied trials, although theoretically it may alter the bilirubin:albumin ratio. In some studies, a dose of albumin at 1g/kg 1 hour before ET has been shown to increase the efficiency of exchange by 40%. 12 Other supportive measures Counseling and support for breast feeding and NNJ Ensure adequate hydration by liberal intake of milk; Consider additional supplementary formula milk/ expressed breast milk or intravenous fluid if dehydrated Routine water supplement has not been shown to benefit breast fed jaundiced infants
131
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
Guidelines of use of Minolta JM-103 in postnatal ward Measure 2 readings from sternum, and take the higher reading
1. Measure at least once daily for all neonates during the first five days of hospital stay
>37+0 weeks of gestation 24 hours PT level 165 (mol/L)
48 hours 220
72 hours 265
96 hours 300
120 hours 310
CHECK BLOOD FOR BUBC WHEN JM-103 (mol/L) >135 >190 >235 >260 >260
35+0 36+6 weeks of gestation 24 hours 48 hours PT level 130 200 (mol/L) CHECK BLOOD FOR BUBC WHEN JM-103 (mol/L) >100 >170
72 hours 230
96 hours 250
120 hours 255
>200
>210
>210
Updated on 24 Feb 2010 by Dr KY Wong
132
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
SECTION 4 : UPAM USEFUL TELEPHONE NUMBERS
Paediatric general on-call MO: DECT phone # 1279 Neonatal on-call MO: DECT phone # 1278 PICU on-call MO: DECT phone # 1280
Ward/Office D4 Cardiac K7S K7N K8S K8N K10N K10S KGOPD UPAM office UPAM IT Lab (Clinical photo) DKCAC Secretary, Division of Paediatric Cardiology
Ext 5644/5645 3439/ 3440 3434/3435 3450/3451 3445/3446 3468/3469 3480/3481 3237/ 3386 ( Appointment) 3241/3343 ( Nurse) 4482 (Teresa) 4299/4945 2974 0328 3847/3848
133
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
NOTES
134
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
NOTES
135
Manual for Paediatric Interns and Residents 4th edition
__________________________________________________________________________________
136
You might also like
- Attitudes of Hemodialysis Patients, Medical and Nursing Staff Towards Patients' Physical ActivityDocument12 pagesAttitudes of Hemodialysis Patients, Medical and Nursing Staff Towards Patients' Physical Activityyanuar esthoNo ratings yet
- Public DoucmentDocument67 pagesPublic DoucmentNavanath Darwante100% (1)
- Facilities of HospitalsDocument11 pagesFacilities of HospitalsGretzen Ensuya GurreaNo ratings yet
- Emergency Ward PDFDocument30 pagesEmergency Ward PDFdolar buhaNo ratings yet
- Sri Guru Ram Das Charitable Hospital, Vallah, Sri Amritsar OPD ScheduleDocument3 pagesSri Guru Ram Das Charitable Hospital, Vallah, Sri Amritsar OPD ScheduleTarlochan SinghNo ratings yet
- Case Study HospitalDocument8 pagesCase Study HospitalNur NezzahNo ratings yet
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- College Cut Off PHDocument71 pagesCollege Cut Off PHAkankshaNo ratings yet
- CVS II Tutorials Apr 12-17Document7 pagesCVS II Tutorials Apr 12-17rishitNo ratings yet
- Attapadi Report EDocument12 pagesAttapadi Report ESabujosephNo ratings yet
- Chronic Kidney Disease-Mineral Bone DisorderDocument49 pagesChronic Kidney Disease-Mineral Bone DisorderÀi ZìjǐNo ratings yet
- Cross Culture InfluenceDocument40 pagesCross Culture Influencepatelhashir100% (4)
- Orthopedic Hospital Intro, O.T. & BMWDocument4 pagesOrthopedic Hospital Intro, O.T. & BMWjahanavi sharmaNo ratings yet
- Current Concepts in Operative Room Sterilisation: Allied Ophthalmic SciencesDocument5 pagesCurrent Concepts in Operative Room Sterilisation: Allied Ophthalmic SciencesRaghavendra Rao100% (1)
- Pediatric Hospital PresentationDocument61 pagesPediatric Hospital PresentationLindsay Khryss Cendy MadahanNo ratings yet
- Emergency Department-Group 3Document16 pagesEmergency Department-Group 3Hardeep SinghNo ratings yet
- Design Brief PDFDocument8 pagesDesign Brief PDFNur Shahmira Ahmad ShahNo ratings yet
- MEDICALLY COMPROMISED Patients in Orthodontics / Orthodontic Courses by Indian Dental AcademyDocument107 pagesMEDICALLY COMPROMISED Patients in Orthodontics / Orthodontic Courses by Indian Dental Academyindian dental academyNo ratings yet
- Critical Care Environment - Design Stucture and FacilitiesDocument22 pagesCritical Care Environment - Design Stucture and FacilitiesProf. Ramsharan MehtaNo ratings yet
- 5 Reducing Time To Analgesia in The Emergency Department Using ADocument10 pages5 Reducing Time To Analgesia in The Emergency Department Using AMegaHandayaniNo ratings yet
- Hospital BriefDocument8 pagesHospital Briefvignesh rulzNo ratings yet
- Mechanisms of Drug Toxicity: Proceedings of the Third International Pharmacological MeetingFrom EverandMechanisms of Drug Toxicity: Proceedings of the Third International Pharmacological MeetingH. RaškováNo ratings yet
- Syllabus of MD General MedicineDocument5 pagesSyllabus of MD General Medicine2shubhoNo ratings yet
- 220100718arunkumar PDFDocument128 pages220100718arunkumar PDFAnand Babu100% (1)
- Doctor On Call Preview-1Document58 pagesDoctor On Call Preview-1Fourth YearNo ratings yet
- 101to 200 Baded HospitalDocument97 pages101to 200 Baded Hospitalar_danishNo ratings yet
- Layout of HospitalDocument11 pagesLayout of HospitalRitesh Kumar PatroNo ratings yet
- Study of Healthcare Facilities and Access To Healthcare in Badshahibagh and Near VillagesDocument17 pagesStudy of Healthcare Facilities and Access To Healthcare in Badshahibagh and Near VillagesMd Kashif RazaNo ratings yet
- Advances in Cattle WelfareFrom EverandAdvances in Cattle WelfareCassandra TuckerNo ratings yet
- AETCOM 1.1 What Does It Mean To Be A DoctorDocument7 pagesAETCOM 1.1 What Does It Mean To Be A DoctorDev Malav100% (1)
- ENT - Clinical Treatment Guidelines PDFDocument76 pagesENT - Clinical Treatment Guidelines PDFDokimi LemeNo ratings yet
- DessertationDocument36 pagesDessertationAaquib MahfuzNo ratings yet
- Muzaffarnagar Medical College MagazineDocument106 pagesMuzaffarnagar Medical College MagazineVaibhav Jain100% (1)
- Project ReportDocument94 pagesProject ReportKeshava NagalkarNo ratings yet
- Topic - All India Institute of Ayurveda (Aiia) Is in Plan To Setup All India Institute of Ayurveda at Dhargal in Pernem, GoaDocument8 pagesTopic - All India Institute of Ayurveda (Aiia) Is in Plan To Setup All India Institute of Ayurveda at Dhargal in Pernem, Goabharati survaseNo ratings yet
- Services in HospitalDocument22 pagesServices in HospitalAShu SainiNo ratings yet
- FAST PACES CLINICAL MEDICINE - CDRDocument30 pagesFAST PACES CLINICAL MEDICINE - CDRTaniaNo ratings yet
- Benefit and Harm: The Stanford Prison Experiment..Document3 pagesBenefit and Harm: The Stanford Prison Experiment..SahrulNuhuyanan0% (1)
- Ward LayoutsDocument70 pagesWard LayoutsArnav DasaurNo ratings yet
- Chairman's Note-MRCGP INTDocument2 pagesChairman's Note-MRCGP INTSalah Elbadawy100% (1)
- HOSPITAL Design: Case Study & Literature StudyDocument33 pagesHOSPITAL Design: Case Study & Literature StudyShrey SharmaNo ratings yet
- Surgical Remix For Medical StudentsDocument108 pagesSurgical Remix For Medical StudentsOmar AhmedNo ratings yet
- MBBS From Medical University in Russia 2020-21 PDFDocument3 pagesMBBS From Medical University in Russia 2020-21 PDFtwinkle227No ratings yet
- 100 Bedded Hospital LectureDocument53 pages100 Bedded Hospital LectureIngyin KhinNo ratings yet
- Anaphylaxis CEACCP 2004Document3 pagesAnaphylaxis CEACCP 2004kuruppukarlNo ratings yet
- The West Bengal University of Health SciencesDocument9 pagesThe West Bengal University of Health Sciencesbhaskar rayNo ratings yet
- Paediatric Handbook - Amanda GweeDocument5 pagesPaediatric Handbook - Amanda GweezekijuraNo ratings yet
- People Management in Hospitat IndustryDocument29 pagesPeople Management in Hospitat Industrychintamani_krishnaNo ratings yet
- 500 Bed Thesis ProposalDocument74 pages500 Bed Thesis ProposalJul Parale100% (1)
- Hospital RegulationDocument97 pagesHospital RegulationKarthikeyan JothiramalingamNo ratings yet
- Laboratory Test Report: Male 25 YearsDocument5 pagesLaboratory Test Report: Male 25 Yearsom_prakash1986100% (1)
- Set 1 Checked: E. Pathological ConditionDocument60 pagesSet 1 Checked: E. Pathological ConditionKunal BhamareNo ratings yet
- DR, Junaid CV 2016Document10 pagesDR, Junaid CV 2016Junaid NazarNo ratings yet
- PG Primary Health CareDocument58 pagesPG Primary Health CareIkhazuangbe Edison Omon100% (1)
- En - PPR - Nursing College & School of NursingDocument129 pagesEn - PPR - Nursing College & School of NursingDonor CrewNo ratings yet
- Out-Patient Department: S.Mallikarjuna MHADocument14 pagesOut-Patient Department: S.Mallikarjuna MHAsandhyakrishnanNo ratings yet
- Recommendation On ICU DesignDocument7 pagesRecommendation On ICU DesignIhab Sadek FaekNo ratings yet
- ARU-355 Design Project-I Multi-Specialty HospitalDocument4 pagesARU-355 Design Project-I Multi-Specialty Hospitalsnehael goelNo ratings yet
- Hpcsa Booklet 2 Generic Ethical Rules With AnexuresDocument58 pagesHpcsa Booklet 2 Generic Ethical Rules With Anexuresapi-301960722No ratings yet
- Effectiveness of Homeopathy For Clinical Conditions - Evaluation of The Evidence PDFDocument301 pagesEffectiveness of Homeopathy For Clinical Conditions - Evaluation of The Evidence PDFYaniv AlgrablyNo ratings yet
- Hiv - From Epidemiology To DiagnosisDocument5 pagesHiv - From Epidemiology To DiagnosisalvinatNo ratings yet
- Newborn Life Support: Resuscitation Council (UK)Document10 pagesNewborn Life Support: Resuscitation Council (UK)alvinatNo ratings yet
- By Karen Black (Mnurssci, RNC)Document22 pagesBy Karen Black (Mnurssci, RNC)alvinatNo ratings yet
- Nyu Csaah Conference 2007 D Hong CBWDocument28 pagesNyu Csaah Conference 2007 D Hong CBWalvinatNo ratings yet
- Nyu Csaah Conference 2007 D Hong CBWDocument28 pagesNyu Csaah Conference 2007 D Hong CBWalvinatNo ratings yet
- 4.2 MDS01 - Definition Table of The MDS Items - Ver0.94Document7 pages4.2 MDS01 - Definition Table of The MDS Items - Ver0.94AriniDwiLestariNo ratings yet
- NCP (Orif)Document13 pagesNCP (Orif)Jay Jay JayyiNo ratings yet
- Lra e Doenças TropicaisDocument13 pagesLra e Doenças Tropicaisadrianoneto60No ratings yet
- DIARHEA IN CHILDRENDocument33 pagesDIARHEA IN CHILDRENRifka AnisaNo ratings yet
- 2 - Determinants of Acute Malnutrition Among Children Aged 6-59 Months Visiting Public Health Facilities in Gambella Town, Southwest Ethiopia Unmatched Case-Control StudyDocument10 pages2 - Determinants of Acute Malnutrition Among Children Aged 6-59 Months Visiting Public Health Facilities in Gambella Town, Southwest Ethiopia Unmatched Case-Control StudyRezki Purnama YusufNo ratings yet
- An Introduction To Probiotics: Key PointsDocument6 pagesAn Introduction To Probiotics: Key PointsDinesh PuppalaNo ratings yet
- Nutrolin-B Syrup 60 ML Price, Uses, Side EffectsDocument1 pageNutrolin-B Syrup 60 ML Price, Uses, Side EffectsanuraganNo ratings yet
- Otc Practice Lec 1Document54 pagesOtc Practice Lec 1mahgadNo ratings yet
- Guide To DHS Statistics: The Demographic and Health Surveys ProgramDocument645 pagesGuide To DHS Statistics: The Demographic and Health Surveys ProgramfebyolandaNo ratings yet
- 2018 Persistent DiarrhoeaDocument8 pages2018 Persistent DiarrhoeaDanielaRojasNo ratings yet
- FHIS Version 2014Document254 pagesFHIS Version 2014Sphero Castillo100% (1)
- Abnormalities of StoolDocument9 pagesAbnormalities of StoolanaNo ratings yet
- Family Medicine QuestionDocument16 pagesFamily Medicine QuestiondrusmansaleemNo ratings yet
- Pro-Ctcae EnglishDocument18 pagesPro-Ctcae EnglishyouldenaNo ratings yet
- Parasitology Collection, Preservation of SpecimensDocument20 pagesParasitology Collection, Preservation of SpecimensSwar KlesNo ratings yet
- ACG Clinical Guideline Diagnosis, Treatment, And.14Document21 pagesACG Clinical Guideline Diagnosis, Treatment, And.14Jeremy A H.L.No ratings yet
- Bowel Elimination: Diarrhea Dehydration Secondary To Profuse Diarrhea. He Is Awake, Alert, and Oriented (×3, Has A Low-Grade FeverDocument2 pagesBowel Elimination: Diarrhea Dehydration Secondary To Profuse Diarrhea. He Is Awake, Alert, and Oriented (×3, Has A Low-Grade FeverBashracel Marie M. SALMORINNo ratings yet
- NSTP Unit 4Document14 pagesNSTP Unit 4Sophie DatuNo ratings yet
- National Health Programme Related To CHNDocument76 pagesNational Health Programme Related To CHNArchanaNo ratings yet
- AntidiarrhoealDocument16 pagesAntidiarrhoealSuraj VermaNo ratings yet
- 2 Prebiotics and Probiotics - Modifying and Mining The Microbiota PDFDocument6 pages2 Prebiotics and Probiotics - Modifying and Mining The Microbiota PDFvanessaNo ratings yet
- Discharge Planning Diarrhea PatientDocument2 pagesDischarge Planning Diarrhea PatientSulvian ayuNo ratings yet
- Rabbit ProductionDocument19 pagesRabbit ProductionPASKAL GWALTUNo ratings yet
- Development of Water Safety Plan Models For Water Refilling Stations in The PhilippinesDocument5 pagesDevelopment of Water Safety Plan Models For Water Refilling Stations in The PhilippinesDIONISIO BALBABOCONo ratings yet
- Gi NclexDocument8 pagesGi NclexDerek Scott Tripp67% (3)
- Herbal Medicines Used in PHC in ASEAN-For ASECDocument272 pagesHerbal Medicines Used in PHC in ASEAN-For ASECKirstie Imelda100% (1)
- Case Presentation 4rth Year AnemiaDocument15 pagesCase Presentation 4rth Year AnemiaHarshini VempatiNo ratings yet
- IMNCI Part 1 Final Print-Ready March 2011 PDFDocument126 pagesIMNCI Part 1 Final Print-Ready March 2011 PDFBirhanu AyenewNo ratings yet
- AJEERNA (Indigestion)Document37 pagesAJEERNA (Indigestion)m gouriNo ratings yet
- Choler A: Prepared By: Angelou Mortos John Radley SantosDocument11 pagesCholer A: Prepared By: Angelou Mortos John Radley SantosAdhaNo ratings yet