Professional Documents
Culture Documents
Communty Health Nursing Study Guide For Hesi Final All Parts
Uploaded by
teokie0824Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Communty Health Nursing Study Guide For Hesi Final All Parts
Uploaded by
teokie0824Copyright:
Available Formats
Community Study Guide for the Hesi Population Groups across the Lifespan Health Risks Infants Number
1 cause of injury or death is suffocation followed by Motor Vehicle Accident then Homicide. Sudden Infant Death Syndrome Infection is the most significant cause of illness in infants and children. Children Obesity Healthy people objectives have addressed youth fitness and obesity Defined by using BMI which is a ratio of weight to height Risks for childhood obesity were related to obesity in the parents Obesity rates higher populations such as Native American, Hispanic, and African Americans groups. Lower socioeconomic groups in urban settings have been associated with higher rates Injuries and Accidents- Number one cause of death in ages 1 24 yrs. Motor vehicles accidents are the leading cause of death among children and teenagers. Toddlers experience a large number of falls, poisonings, and motor vehicle accidents School age children has the lowest injury death rate; however, this group has difficulty judging speed and distance, placing them at risk for pedestrian and bicycle accidents. Adolescents injury accounts for 75% of all deaths and risk-taking becomes more conscious at this time especially among males. Suicide is the second leading cause of death among youths between the ages of 15 and 24. Suicide s the third leading cause of death among youth between the ages of 10 and 24 years. Acute Illness- also a significant cause of illness in children. Chronic Health Problems- improved medical technology has increased the number of children surviving with chronic health problems. Examples: Down Syndrome, spina bifida, cerebral palsy, asthma, diabetes, congenital heart disease, cancer, hemophilia, broncopulmonary dysplasia, and AIDS Routine immunizations have been very successful in preventing selected diseases. Good nutrition is essential for healthy growth and development and influences disease prevention in later life. Women The womens health movement was pivotal in bringing national recognition to womens health issues. Women have a longer life expectancy than men
Women are more likely to have acute and chronic conditions that require them to use more services than men. Women of color are more statistically more likely to have poor health outcomes because of poor understanding of health, lack of access to health care, and lifestyle practices. Heart disease leading cause of death in women Lung Cancer leading cause of cancer in women and 2nd leading cause of death Men Men are physiologically the more vulnerable gender, shorter life span and higher infant mortality rate Life expectancy of men in the US is one of the lowest in the developed countries Men engage in more risk-taking behaviors than women Men tend to avoid diagnosis and treatment of illnesses that may result in serious health problems Elderly Steadily growing population Increase in chronic conditions, demand for services, and strained health care budgets More older adults live in the community Nurses address the chronic health concerns of elders with a focus on maintaining or improving self-care and preventing complications to maintain the highest possible quality of life. Assessing the elderly incorporates physical, psychological, social, and spiritual domains. Individual and community focused interventions involve all three levels of prevention through collaborative practice. U.S. Healthcare problems More than 43 million people in the United States are uninsured, and many more simply lack access to adequate health care. Health care reform measures seek to make changes in the cost, quality, and access of the present system. The integration of primary care and public health is necessary for the future health of the nation To achieve the specific health goals of programs such as healthy People 2010, primary care and public health must work within the community for community-based care. The most sustainable individual and system changes come when people who live n the community have actively participated. Nurses are more than able to fill the gap between personal care and public health because they have skills in assessment, health promotion, and disease and injury prevention; knowledge of community resources; and ability to develop relationships with community members and leaders.
Home Visits- give a more accurate assessment of the following than do clinical visits: - the family structure - the natural or home environment - behavior in that environment Home visits provide opportunities to identify both barriers and supports for reaching family health promotion goals. Home visits afford the opportunity to gain a more accurate assessment of the family structure and behavior in the natural environment. Home visits also provide opportunities to observe the home environment and to identify both barriers and supports to reducing health risks and reaching family health goals. Parish nurses: nurses who respond to health and wellness needs within the faith context of population of faith communities and are partners with the church in fulfilling the mission of health ministry. Parish nursing: a community-based and population-focused professional nursing practice with faith communities to promote whole person health to its parishioners usually focused on primary prevention. Parish nurse coordinator: a parish nurse who has completed a certificate program designed to develop the nurse as a coordinator of a parish nursing service. Parish nurse services respond to health, healing, and wholeness within the context of the church. Although the emphasis is on health promotion and disease prevention throughout the life span, the spiritual dimension of nursing is central to the practice. The parish nurse partners with the wellness committee and volunteers to plan programs and consider health-related concerns within faith communities To promote a caring faith community, usual functions of the parish nurse include personal health counseling, health teaching, facilitating linkages and referrals to congregation and community resources, advocating and encouraging support resources, and providing pastoral care. Parish nurses collaborate to plan, implement, and evaluate health promotion activities considering the faith communitys beliefs, rituals, and polity. Healthy People 2010 guidelines are basic to the partnering for the programs. Nurses working in the parish nursing specialty must seek to attain adequate educational and skill preparation for the accountability to those served and to those who have entrusted the nurse to serve Nurses are encouraged to consider innovative approaches to creating caring communities. These may be in congregations as parish nurses, among several faith communities in a
single locale, or regionally; or in partnership with other community agencies or models such as block nursing. To sustain oneself as a parish nurse healer, the nurse takes heed to heal and nurture self while supporting individuals, families, and congregation communities in their healing process. Hospice: palliative system of health care for terminally ill people; takes place in the home with family involvement under the direction and supervision of health professionals, especially the visiting nurse. Hospice care takes place in the hospital when sever complications of terminal illness occur or when family becomes exhausted or does not fulfill commitments. Professional Preparedness Requires nurses and other personnel to be aware of and understand the disaster plans at their workplace and community- participate in mock drills Adequately prepared nurses will function in leadership capacity and assist towards smoother recovery phase Fieldwork, shelter management requires creativeness and willingness American Red Cross provides training for health professionals to adapt existing skills to disaster setting Role of Community Health Nurse Can initiate or update disaster plans at workplace and community and ensure education, drill participation Knowledge of vulnerable populations, available community resources Assessing and reporting of environmental hazards, unsafe equipment, faulty structures, disease outbreaks, e.g., measles, flu Before anything happens: Prepare for Safety in a Disaster : Four steps 1. Find out what could happen to you: a. Determine what types of disasters are most likely to happen b. Learn about warning signals in community c. Ask about care for pets d. Review the disaster plans at workplace, and other places where families spend time together e. Determine how to help the elderly or disabled 2. Create a disaster plan a. Discuss types of disasters that are likely to happen and review what to do b. Pick 2 types of places to meet c. Choose an out-of-state friend to contact d. Review evac. Plans
3. Complete this checklist a. Post emergency numbers next to phone b. Teach how to call 911 c. Determine when and how to turn of water, gas, and electricity d. Check adequacy of insurance coverage e. Locate and review use of fire extinguishers f. Install and maintain smoke detectors g. Conduct a home hazard hunt h. Stock emergency supplies i. CPR certification j. Locate all escape routes k. Find safe spots 4. Practice and maintain your plan a. Review every 6 mos. b. Conduct drills c. Replace stored water every 3 mos. and stored food every 6 mos. d. Test and recharge fire extinguisher e. Test smoke detectors Personal Preparedness Nurses who are disaster victims themselves and provide care to others will experience considerable stress. American Red Cross and Federal Emergency Management Agency (FEMA) are two well known authorities on disaster preparedness, response, and recovery Three levels 1st level Personal Preparedness 2nd level- Professional Preparedness 3rd level- Community Preparedness Most states and counties have an Office of Emergency Management (OEM) that is responsible for developing and coordinating emergency response plans within their defined area. The state office supports local OEMs and other state agencies that participate in disaster response. It provides planning and training services to local governments, including financial and technical assistance. During an actual emergency or disaster, the state OEM coordinates a state response and recovery program if necessary. County OEMs are in charge of creating a comprehensive, allhazard plan that should address realistic dangers to the community and list available resources. **Nurses need to review the disaster history of community, including how past disasters have affected the health care delivery system, how their particular organizations fit into the plan, and what role they and their organizations are expected to play in a disaster.
Stages: Preparedness, Response, and Recovery Preparedness: Know who is at risk, Personal, Professional and Community Preparedness Personal Preparedness Entails plan for keeping oneself ready for disaster, both mentally and physically Individuals not personally prepared will have less to give to family, community, job, and other disaster victims Nurses can be disaster victims- personal preparation needed to attend to patients Checklist helpful to prepare Professional Preparedness Requires nurses and other personnel to be aware of and understand the disaster plans at their workplace and community- participate in mock drills Adequately prepared nurses will function in leadership capacity and assist towards smoother recovery phase Fieldwork, shelter management requires creativeness and willingness American Red Cross provides training for health professionals to adapt existing skills to disaster setting
Community Preparedness Level of preparedness only as high as people/ organizations in the community make it Well-prepared communities have written disaster plans, conduct drills, have adequate warning system, and backup evacuation plan Office of Emergency Management- state/ county office coordinating regional plans Understanding past disasters can influence planning for future, liabilities in resources Response The primary objective of disaster response is to minimize morbidity and mortality. The level of disaster determines FEMAs response. Levels are not determined by the number of casualties but by the amount of resources needed. FEMA Levels of Disaster Response Level III- a minor disaster, involves a minimal level of damage but could result in the president declaring an emergency. A minimal request for federal help Level II- moderate disaster- likely to result in major disaster being declared. Regional federal resources engaged, other outside area may be called on Level I- massive disaster, severe damage or multistate scope. Full engagement of federal regional and national resources Citizens and health professionals must be attached to official agencies with disaster management responsibilities to avoid further risk
American Red Cross 3 ways to classify a disaster : Type- agent that caused the event, such as hurricane, hazmat, transportation
Level- anticipated or actual Red Cross response and relief costs
Level I. costs less than $10,000 Level II costs $10,000 or more, but less than $50,000 Level II costs $50,000 or more, but less than $250,000 Level IV costs $250,000 or more but less than $2.5 million Level V costs $2.5 million or more
Scope- magnitude of the event, units affected and responding ,e.g., single-family, local,
state, major, federally declared Single family affects an individual or single family- occurs within the jurisdiction of a single Red Cross chapter Local Disaster- Affects more than one family, occurs within the jurisdiction of a single Red Cross chapter State Disaster- Affects multiple families, occurs within the jurisdiction of one or More Red Cross chapters within a single state Major Disaster- has one or more of the following characteristics -coordinated response of multiple Red Cross units - affects more than a single state - creates national news - result in emergency or disaster declaration by the President etc. Presidentially Declared Disaster- requires full or partial implementation of the National Response Plan The National Response Plan Once a federal emergency has been declared, the National Response Plan may take effect, depending on specific needs arising from the disaster. The NRP is a concerted effort to prevent terrorist attacks within the US; reduce Americans vulnerability to terrorism, major disasters, and other emergencies; and minimize the damage and recover from attacks, major disasters, and other emergencies that occur. Role of the Nurse Role in disaster response depends on nurses past experience, role in community disaster preparedness, specialized training, special interest
Community
health nurses valued for skills in community assessment, case finding, prevention, education, surveillance, working with aggregates
Plans
for triage must begin as soon as rescue workers arrive- highest priority given to life-threatening injuries with high probability of survival- nurses accurate assessment info will help match available resources to populations emergency needs
Recovery The recovery stage of disaster occurs as all involved agencies pull together to restore the economic and civic life of the community. For example: the government takes the lead in rebuilding efforts whereas the business community tries to provide economic support. Nurses Role in Recovery Multifaceted responsibilities- flexibility required to assist in successful recovery Teaching health promotion, disease prevention, assessment of physical, psychological problems incurred in cleanup efforts, as well as threat of communicable disease Case finding, referral for mental distress Assessment and reporting of environmental health hazards resulting from event Get community back to normal, deal with emotional matters and after effects Assess what might be going on in community using primary, secondary and tertiary care Terrorism Role of the Nurse: Help people cope with the aftermath of terrorism Allay public concerns and fears of bioterrorism Identify the feelings that you and others may be experiencing Assist victims to think positively and move to the future Prepare nursing personnel to be effective in a crisis situation Nurses are concerned with anthrax and small pox and should have awareness of these diseases Need to have vaccine for small pox Levels of prevention r/t Disaster Management Primary Prevention- Participate in developing a disaster management plan for the community Secondary Prevention- Assess disaster victims and triage for care Tertiary Prevention- Participate in home visits to uncover dangers that may cause additional injury to victim or cause other problems (e.g. house fires from faulty wiring). Population at Greatest Risk for Disruption After a Disaster Persons with disabilities Persons living on a low income, including the homeless Non-English speaking persons and refugees Persons living alone
Single-parent families Persons new to the area Institutionalized persons or those with chronic mental illness Previous disaster victims or victims of traumatic events People who are not citizens or legally documented immigrants Substance abusers The five components to a comprehensive public health response to outbreaks of illness are the following - Detecting the outbreak - Determining the cause - Identifying factors that place people at risk - Implementing measures to control the outbreak - Informing the medical and public communities about treatments, health consequences, and preventative measures Triage: the process of separating casualties and allocating treatment on the basis of the victims potentials for survival. Highest priority is always given to victims who have life threatening injuries but who have a high probability of survival once stabilized Second priority is given to victims with injures that have systemic complications that are not yet life threatening and could wait 45 60 minutes for treatment Last priority is given to those victims with local injuries without immediate complications and who can wait several hours for medical attention. Rationale from Saunders In an emergency department, triage is classifying clients according to their need for care and includes establishing priorities of care. The kind of illness, the severity of the problem, and the resources available govern the process. Clients with trauma, chest pain, severe respiratory distress or cardiac arrest, limb amputation, acute neurological deficits, and those who sustained chemical splashes to the eyes are classified as emergent and are the number 1 priority. Clients with conditions such as a simple fracture, asthma without respiratory distress, fever, hypertension, abdominal pain, or the client with a renal stone have urgen needs and are classified as number 2 priorities. Clients with conditions such as a minor laceration, sprain, or cold symptoms are classified as nonurgent and are the number 3 priority. Older adult health risks Nutrition, safety, social isolation, and depression Need to assess the health literacy of the client first
Program outcomes: smoking cessation, weight management, diabetic management - look at the evaluation of the specific outcome - Identifying changes in the clients health status that result from nursing care provides nursing data that demonstrate the contribution of nursing to the health care delivery system. Research studies using the tracer or sentinel method to identify clients outcomes and client satisfaction surveys can be used to measure outcome standards. From data, strengths and weaknesses in nursing care delivery can be determined. The most common measurement methods are direct physical observations and interviews. Primary Care- refers to organized community efforts designed to prevent disease and promote health (education). Secondary Care- an intermediate level of health care that includes diagnosis and treatment. Screening. Tertiary Care- rehabilitation and return of a patient to a status of maximum usefulness and a minimum risk of recurrence of a physical or mental disorder Levels of Prevention Primary Prevention- Counsel clients in health behaviors related to lifestyle Secondary Prevention- Implement a family-planning program to prevent unintended pregnancies or young couples who attend the primary clinic Tertiary Prevention- Provide a self-management asthma program for children with chronic asthma to reduce their need for hospitalization (prevent from getting worse) Federal Agencies Many federal agencies are involved in government health care functions. The agency most directly involved with the health and welfare of Americans is the U.S. Department of Health and Human Services
U.S. Department of Health and Human Services (USDHHS) Largest health program in the world, its mission is to enhance the health and well-being of the American people through the following: - Alcohol, drug abuse, and mental health programs - Disease tracking and identification - Health care access for all and integrity of the nations health entitlement and safety net programs - Identification and correction of health hazards - Medical assistance after disasters - Medical research - Promotion of exercise and healthy habits - Protection of the nations food and drug supply The Health Resources and Services Administration of the USDHHS contains the Bureau of Health Professions, this bureau includes separate divisions for nursing, medicine, dentistry, public health, and allied health professions The Division of Nursing administers nurse education legislation, interprets trends and nursing needs of the nations health care delivery system, and serves as a liaison with the nursing community and with international, state, regional, and local health interests Two other agencies with the DHHS: The National Institute for Nursing Research (NINR) and Healthcare Research and Quality (AHRQ) This institution is the focal point of the nations nursing research activities. It promotes the growth and quality of research in nursing and patient care, provides important leadership, expands the pool of experienced nurse researchers, and serves as a point of interaction with other bases of health care research Nurses can apply for support for research, projects, or training from a variety of agencies within the federal government besides the NINR of the Division of Nursing. Other federal agencies: Dept. of Commerce, Dept. of Defense, Dept. of Labor (includes OSHA), Dept. of Agriculture (includes WIC), Dept. of Justice, Food and Drug Administration. Voluntary and Private Nonprofit Agencies Voluntary and private agencies are grouped together as nonprofit home health agencies, voluntary agencies are supported by charities such as United Way, Medicare, Medicaid, other third-party payers, and client payment. The amount of financial assistance the voluntary agency receives depends on the community it serves. With Medicare, the private nonprofit agency emerged as an alternative agency to the public-supported program. These agencies included rehabilitation agencies, based in either rehabilitation facilities or skilled facilities.
Nurses use assessment skills to detect potential and actual exposure pathways and outcomes for clients cared for in the acute, chronic, and healthy communities of practice. Risk communication is an important skill and must acknowledge the outrage factor experienced by communities with environmental hazards. Vulnerable populations- are those groups who have an increased risk to develop adverse health outcomes, vulnerable populations often experience multiple cumulative risks and they are particularly sensitive to the effects of those risks. Vulnerable populations often are more likely than the general populations to suffer from health disparities. Examples of areas that show health disparities across populations groups are infant mortality, childhood immunization rates, and disease-specific mortality rates. Vulnerable Population Groups of Special Concern to Nurses - Poor and homeless people - Pregnant adolescents - Migrant workers and immigrants - Severely mentally ill individuals - Substance abusers - Abused individuals and victims of violence - Persons with communicable disease and those at risk - Persons who are human immunodeficiency virus (HIV positive) or have Hep B or sexually transmitted disease. Behavioral (Lifestyle) Health Risk Assessment Families are the major source of factors that can promote or inhibit positive lifestyles. It is important to look at risks for the family as a unit. Critical dimensions of lifestyle risks include the following: - Value placed on behavior - Knowledge of the behavior and its consequences - Effect of the behavior on the family - Effect of the behavior on the individual - Barriers to performing the behavior - Benefits of the behavior It is important to assess the frequency, intensity, and regularity of specific behaviors. It also is important to evaluate the resources available to the family for implementing the behaviors.
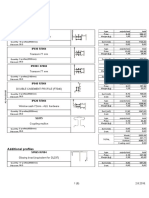
Modifiable Risk and Unmodifiable Risks Risk factors that are "unmodifiable," are things that neither you nor your patients can do anything about. You need to know the "unmodifiable" risk factors, because they help you to define high-risk individuals and groups for whom treating or controlling the "modifiable" risk factors is a priority. Mmodifiable risks can be changed such as smoking. Epidemiology how to calculate a rate The denominator includes the numerator Example Crude birth rate Number of live births during 1 year X1000 Midyear population
Evaluating Outcomes Outcomes can be measured by looking at changes from before and after the intervention to solve the problems. Changes in the following can be used to see the outcomes of the interventions: - Demographics - Socioeconomic factors - Environmental factors - Individual and community health status - Use of health services In the example of infant malnutrition, one would look for the number of cases of infant malnutrition in the community before providing education to other health providers about assessment of infant development. A time period for evaluation would be chosen and perhaps 1 year later (the time frame). The number of cases of infant malnutrition would be measured to see if a change had occurred and there were fewer cases. Incidence rate- the frequency or rate of new cases of an outcome in a populations; provides an estimate of the risk of disease in that population over the period of observation Prevalence: number of existing cases in a population at a given time Nursing Process- Always assess before starting an intervention Community assessment Most nurses are familiar with the nursing process as it applies to individually focused nursing care. Using it to promote community health makes this same nursing process community focused. Community assessment- the process of critically thinking about the community and involves getting to know and understand the community as partner. The community
assessment phase involves a logical, systematic approach to the initial phase of the nursing process. Community assessment helps as follows: - To identify community needs - To clarify problems - To identify strengths and resources Assessing the community health requires the following three steps: - Gathering relevant existing data and generating missing data - Developing a composite database - Interpreting the composite database to identify community problems and strengths Data Collection and Interpretation The primary goal of data collection is to get usable information about the community and its health. The systematic collection of data about community health requires the following: - Gathering or compiling existing data - Generating missing data - Interpretation of data Identifying community health problems and community abilities Data gathering is the process of obtaining existing, readily available data. The following data usually describe the demography of a community - Age of residents - Gender distribution of residents - Socioeconomic characteristics - Racial distributions - Vital statistics, including selected mortality and morbidity data Identify needs, problems, strengths, resources and apply what you know. Windshield survey- are the motorized equivalent of simple observation. They involve the collection of data that will help define the community, the trends, stability, and changes that will affect the health of the community School Nurse: Primary -The school nurse monitors the children for all of their state-mandated immunizations for school entry. - Secondary- School nurse is involved in screening children for illnesses and providing direct nursing care - Tertiary The school nurse cares for children with long-term health needs, including asthma and disabling conditions School nurses carry out catheterizations, suctioning, gastrostomy tube feedings, and other skills in school.
The concern for health promotion of adolescents is safety because of their propensity to take part in risky behavior. To effectively reach a population group you must connect with someone in the community and establish trust. Occupational Exposure Job categories Exposure Farm workers pesticides, infectious Agents, gases, sunlight Chemical workers solvents, cleansers, etc. Work-related diseases and conditions HTN, mood disorders, cardiovascular disease Cancer, etc.
Complete list on page 637 in textbook Medicare Provides hospital insurance and medical insurance to persons ages 65 years and older, permanently disabled persons, and persons with end-stage renal failure Part A covers: hospital care and home care (home care or hospice cant have both), skilled nursing care Part B- covers: (non-institutional care insurance) Medical care, diagnostic services and physiotherapy. Medicaid- Financial assistance to states and counties to pay for medical services for poor older adults, the blind, the disabled, and families with dependent children. WIC- a special supplemental food program administered by the Department of Agriculture through the state health departments; provides nutritious food that add to the diets of pregnant and nursing women, infants, and children younger than 5 years. Eligibility is based on income and nutritional risk as determined by a health professional Outreach worker: a health worker who makes a special, focused effort to find people with specific health problems for the purpose of increasing their access to health services - evaluate effectiveness find out if successful and use ways to measure success Epidemiologic triangle agent, host, and environment changes in one of the elements of the triangle can influence the occurrence of disease by increasing or decreasing a persons risk for disease. Risk is the probability that an individual will experience an event. Agent: an animate or inanimate factor that must be present or lacking for a disease or condition to develop Host: a living species (human or animal) capable of being infected or affected by an agent Environment- all that is internal or external to a given host or agent and that is influenced and influences the host and/or agent
Agent- an animate or inanimate factor that must be present or lacking for a disease or condition to develop - causive example: E. coli - Infectious agents (bacteria, viruses, fungi, parasites) - Chemical agents (heavy metal, toxic chemicals, pesticides) - Physical agents (radiation, heat, cold, machinery) Host- a living species (human or animal) capable of being infected or affected by an agent - anything capable of being infected - Genetic susceptibility - Immutable characteristics (age, sex) - Acquired characteristics (immunologic status) - Lifestyle factors (diet, exercise) Environment- all that is internal or external to a given host or agent and that is influences the host and or agent - anything external - climate (temperature, rainfall) - Plant and animal life (agents or reservoirs or habitats for agents) - Human population distribution (crowding, social support) - Socioeconomic factors (education, resources, access to care) - Working conditions (levels of stress, noise, satisfaction) Relationship between the above 3 cause disease, try to break the connection, if a break then there will be no disease. Web of Causality- complex interrelations of factors interacting with each other to influence the risk for or distribution outcomes. - recognizes the complex interrelationships of many factors interacting, sometimes in subtle ways, to increase (or decrease) the risk of disease. - Associations are sometimes mutual, with lines of causality going in both directions Family assessment Ecomap- represents the familys interactions with other groups and organizations, accomplished by using a series of circles and lines. - It is represented by a circle in the middle of the page - Other groups and organizations are then indicated by circles - Lines representing the flow of energy are drawn between the family circle and the circles representing other groups and organizations - An arrowhead at the end of each line indicates the direction of the flow of energy (into or out of the family) - The weight of the line indicates the intensity of the energy
Genogram- is a pictorial display of a person's family relationships and medical history. It goes beyond a traditional family tree by allowing the user to visualize hereditary patterns and psychological factors that punctuate relationships. It can be used to identify repetitive patterns of behavior and to recognize hereditary tendencies. Prevention Strategies for Violence Individual and Family levels - Assess during routine examination (secondary) - Assess for marital discord (secondary) - Educate on developmental stages and needs of children (primary) - Counsel for at-risk parents (secondary) - Teach parenting techniques (primary) - Assist with controlling anger (secondary) - Treat for substance abuse (tertiary) - Teach stress-reduction techniques (primary) Community Level - Develop policy - Conduct community resource mapping - Collaborate with community to develop systematic response to violence - Develop media campaign - Develop resources such as transition housing and shelters High school students and middle school students- steer away from violence and teach to work on their own skills and build their self-esteem.
You might also like
- HesiDocument16 pagesHesiJazzmyne T.No ratings yet
- Community Hesi Study GuideDocument17 pagesCommunity Hesi Study Guidewhereswaldo007yahooc100% (2)
- Community HESI Study GuideDocument26 pagesCommunity HESI Study Guidemscostello985394% (32)
- Community Study Guide For The HESIDocument4 pagesCommunity Study Guide For The HESIDean WinchesterNo ratings yet
- Study Guide HESI CommunityDocument29 pagesStudy Guide HESI CommunityBeth Ann100% (1)
- Day 2 Overview of CHNDocument10 pagesDay 2 Overview of CHNAliya Nicole CNo ratings yet
- Remembering 2020: Year of the Most Memorable National ChallengesFrom EverandRemembering 2020: Year of the Most Memorable National ChallengesNo ratings yet
- CHN 2-Chapter 1-2Document10 pagesCHN 2-Chapter 1-2Majo Ramirez Mataverde100% (1)
- CommunityDocument1,395 pagesCommunityAnonymous Cskgr1Bgv100% (2)
- The Role of Nursing in Public HealthDocument38 pagesThe Role of Nursing in Public HealthNurdiansyahNo ratings yet
- FHN MODULE1 (PART 1) OVERVIEW of COMMUNITY HEALTH NURSING-1 PDFDocument5 pagesFHN MODULE1 (PART 1) OVERVIEW of COMMUNITY HEALTH NURSING-1 PDFKyedae ShymkoNo ratings yet
- The Role of Public Health NursesDocument16 pagesThe Role of Public Health NursesCarl Chariven A. PaguyoNo ratings yet
- NCM 107 1Document5 pagesNCM 107 1Clint Mikael EulatrizNo ratings yet
- Community Heallth FinalDocument5 pagesCommunity Heallth Finalapi-737302715No ratings yet
- PopulationprojectDocument4 pagesPopulationprojectapi-458055311No ratings yet
- Community and School NRSG - Project.n100Document4 pagesCommunity and School NRSG - Project.n100Jonathan JamesNo ratings yet
- Introduction To Community and Family MedicineDocument54 pagesIntroduction To Community and Family MedicineCieIo Navarra - MorenoNo ratings yet
- CHN1 Worksheet1Document5 pagesCHN1 Worksheet1Chariza MayNo ratings yet
- Reseach FinalDocument8 pagesReseach Finalapi-737850316No ratings yet
- CDX Group 2 FinalDocument161 pagesCDX Group 2 Finaljuel_navarro100% (1)
- Aging Well: Solutions to the Most Pressing Global Challenges of AgingFrom EverandAging Well: Solutions to the Most Pressing Global Challenges of AgingNo ratings yet
- PHC ReviewerDocument16 pagesPHC ReviewerRandom videosNo ratings yet
- Population - Term Used To Describe The Recipients of The Health Motion and Disease and DisabilityDocument4 pagesPopulation - Term Used To Describe The Recipients of The Health Motion and Disease and DisabilityJohn FredNo ratings yet
- Sample of Case PresentationDocument43 pagesSample of Case PresentationAyaBasilio100% (1)
- Unit 2Document35 pagesUnit 2Shaira Abigail AninoNo ratings yet
- Summarized Notes Core 1 Health Priorities in AustraliaDocument21 pagesSummarized Notes Core 1 Health Priorities in AustraliaHaNo ratings yet
- The ROLE OF The Public Health Nurse-AnnievadneDocument39 pagesThe ROLE OF The Public Health Nurse-AnnievadneDolores BeeNo ratings yet
- Prelim NotesDocument13 pagesPrelim Notesjohncarlo ramosNo ratings yet
- Health 499 Senior Capstone Artifact 2 ReflectionDocument4 pagesHealth 499 Senior Capstone Artifact 2 Reflectionapi-622203747No ratings yet
- Final OutputDocument73 pagesFinal OutputBrian ColemanNo ratings yet
- Culture and Cultural Competence: The Importance of Culture in CareDocument4 pagesCulture and Cultural Competence: The Importance of Culture in CarejomarlesinoNo ratings yet
- A Doctor's Dozen: Twelve Strategies for Personal Health and a Culture of WellnessFrom EverandA Doctor's Dozen: Twelve Strategies for Personal Health and a Culture of WellnessNo ratings yet
- Family Health Care 2Document12 pagesFamily Health Care 2saifadin khalilNo ratings yet
- Program ProposalDocument19 pagesProgram ProposalChristian John BingayanNo ratings yet
- CHN-Week 1Document4 pagesCHN-Week 1Bryan Emmanuel AliadoNo ratings yet
- Introduction and Overview of Community Health Nursing: Mary Ann Rosa MSN, RN, CS, GNPDocument66 pagesIntroduction and Overview of Community Health Nursing: Mary Ann Rosa MSN, RN, CS, GNPphoenix18075% (4)
- Community Health Nursing VocabDocument2 pagesCommunity Health Nursing VocabMaureen Beldorin0% (1)
- Community Health NursingDocument14 pagesCommunity Health NursingKira100% (13)
- Community Health Nursing 1: (Individual and Family As Clients)Document63 pagesCommunity Health Nursing 1: (Individual and Family As Clients)Wilma Nierva Beralde100% (4)
- CHNDocument3 pagesCHNNicole Bertulfo100% (1)
- NCM 113 Final Module 8 LectureDocument8 pagesNCM 113 Final Module 8 LectureAngel Khrisna BacasmotNo ratings yet
- Module 1 Overview of Public Health Nursing in The PhilippinesDocument13 pagesModule 1 Overview of Public Health Nursing in The PhilippinesJoycee BoNo ratings yet
- The Domain of Family PracticeDocument5 pagesThe Domain of Family PracticeNUNGSEP100% (1)
- Dementia Strategy Final 2016 2020Document16 pagesDementia Strategy Final 2016 2020Natasa ZdravkovskaNo ratings yet
- Family Medicine Concept and Patient ManagementDocument5 pagesFamily Medicine Concept and Patient ManagementLegenda AkNo ratings yet
- Chapter 1 - The Nature and Content of General Practice: DefinitionsDocument9 pagesChapter 1 - The Nature and Content of General Practice: Definitionsprofarmah6150No ratings yet
- Community Health NursingDocument13 pagesCommunity Health NursingXandra Basnillo100% (1)
- Integrative Health Nursing Interventions for Vulnerable PopulationsFrom EverandIntegrative Health Nursing Interventions for Vulnerable PopulationsAmber VermeeschNo ratings yet
- Capp Activity 2 (Operaña)Document6 pagesCapp Activity 2 (Operaña)Ellayza OperanaNo ratings yet
- Guidelines For Enhancing Access To Palliative CareDocument8 pagesGuidelines For Enhancing Access To Palliative CareDeepika LingamNo ratings yet
- Different Fields in CHN - ReportDocument8 pagesDifferent Fields in CHN - ReportSACHI DANIELLA TATOYNo ratings yet
- Community Health NursingDocument18 pagesCommunity Health NursingCharmagne Joci EpantoNo ratings yet
- June 2007-NPT 1 - RationaleDocument15 pagesJune 2007-NPT 1 - Rationaleяoxel яayмoи eитяeиaNo ratings yet
- 9 Summary Health Education in Chronic IllnessDocument5 pages9 Summary Health Education in Chronic IllnessSteffiNo ratings yet
- Lab CPHDocument73 pagesLab CPHYam100% (1)
- CHN Lecture 1Document20 pagesCHN Lecture 1knotstm100% (1)
- ANP - Family and Home NursingDocument11 pagesANP - Family and Home NursingRinal Barad100% (1)
- Community Health Final-Nursing Final Turn inDocument8 pagesCommunity Health Final-Nursing Final Turn inapi-719825532No ratings yet
- 002 Constraints and Generalized Coordinates PDFDocument27 pages002 Constraints and Generalized Coordinates PDFNiveCeciliaNo ratings yet
- Book - IMO Model Course 7.04 - IMO - 2012Document228 pagesBook - IMO Model Course 7.04 - IMO - 2012Singgih Satrio Wibowo100% (4)
- Instructional MediaDocument7 pagesInstructional MediaSakina MawardahNo ratings yet
- Adventure Shorts Volume 1 (5e)Document20 pagesAdventure Shorts Volume 1 (5e)admiralpumpkin100% (5)
- Philippine Literature During American PeriodDocument5 pagesPhilippine Literature During American PeriodMi-cha ParkNo ratings yet
- Robbins Ob14 PPT 11Document27 pagesRobbins Ob14 PPT 11daneshnedaieNo ratings yet
- K Unit 1 SeptemberDocument2 pagesK Unit 1 Septemberapi-169447826No ratings yet
- Modern State and Contemporaray Global GovernanceDocument34 pagesModern State and Contemporaray Global GovernancePhoebe BuffayNo ratings yet
- The Christ of NankingDocument7 pagesThe Christ of NankingCarlos PérezNo ratings yet
- Simple Past Story 1Document7 pagesSimple Past Story 1Ummi Umarah50% (2)
- Equilibrium of Firm Under Perfect Competition: Presented by Piyush Kumar 2010EEE023Document18 pagesEquilibrium of Firm Under Perfect Competition: Presented by Piyush Kumar 2010EEE023a0mittal7No ratings yet
- Reaction PaperDocument3 pagesReaction PaperPatrick Ramos80% (15)
- Minimum Structural Properties and Test Procedure For TG20 Compliant Prefabricated Structural Transom UnitsDocument16 pagesMinimum Structural Properties and Test Procedure For TG20 Compliant Prefabricated Structural Transom UnitsPrimelift Safety Resources LimitedNo ratings yet
- Projectile Motion PhysicsDocument3 pagesProjectile Motion Physicsapi-325274340No ratings yet
- A Re Ection On The Dominant Learning Theories: Behaviourism, Cognitivism and ConstructivismDocument13 pagesA Re Ection On The Dominant Learning Theories: Behaviourism, Cognitivism and Constructivismchill protocolNo ratings yet
- Lecture 7Document28 pagesLecture 7Nkugwa Mark WilliamNo ratings yet
- Educ 323 - The Teacher and School Curriculum: Course DescriptionDocument16 pagesEduc 323 - The Teacher and School Curriculum: Course DescriptionCherry Lyn GaciasNo ratings yet
- Upanikhat-I Garbha A Mughal Translation PDFDocument18 pagesUpanikhat-I Garbha A Mughal Translation PDFReginaldoJurandyrdeMatosNo ratings yet
- High Court Judgment On Ex Party DecreeDocument2 pagesHigh Court Judgment On Ex Party Decreeprashant pathakNo ratings yet
- DonatelloDocument12 pagesDonatelloGiorgia Ronfo SP GironeNo ratings yet
- Elc650 Ws Guidelines (250219)Document3 pagesElc650 Ws Guidelines (250219)panda_yien100% (1)
- Asphalt Hot Mix Training ManualDocument91 pagesAsphalt Hot Mix Training Manualyazqa50% (2)
- Spoken KashmiriDocument120 pagesSpoken KashmiriGourav AroraNo ratings yet
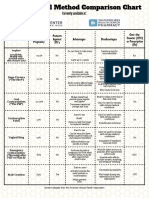
- Birth Control Comparison Chart 2018Document1 pageBirth Control Comparison Chart 2018Eric SandesNo ratings yet
- Colour Communication With PSD: Printing The Expected With Process Standard Digital!Document22 pagesColour Communication With PSD: Printing The Expected With Process Standard Digital!bonafide1978No ratings yet
- Mark Scheme (Final) January 2020Document16 pagesMark Scheme (Final) January 2020aqib ameerNo ratings yet
- Lista Materijala WordDocument8 pagesLista Materijala WordAdis MacanovicNo ratings yet
- MCQ On ErgonomicsDocument4 pagesMCQ On Ergonomicszoom milind67% (3)
- Speaking C1Document16 pagesSpeaking C1Luca NituNo ratings yet
- 5 Reported Speech - T16-6 PracticeDocument3 pages5 Reported Speech - T16-6 Practice39 - 11A11 Hoàng Ái TúNo ratings yet