Professional Documents
Culture Documents
Nursing The Person With A CAST
Uploaded by
Bianca Zamora Labis - MindaroOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nursing The Person With A CAST
Uploaded by
Bianca Zamora Labis - MindaroCopyright:
Available Formats
Nursing the Person with a CAST What is a FRACTURE?
Any disruption in the normal continuity of a bone caused by trauma, twisting as a result of muscle spasm or indirect loss of leverage or bone decalcification Interventions for a FRACTURE What is a CAST? A temporary device made of synthetic materials such as fiberglass, thermoplaster polymer or plaster of Paris PURPOSES Immobilization of bone and joints after a fracture or injury Prevention or correction of deformity Maintenance, support and protection of realigned bone Promotion of healing to allow early weight bearing for ambulation EQUIPMENTS
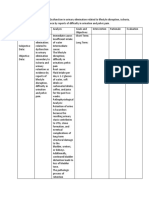
Cast Application Nsg Action 1.Spread the newpaper on the floor 2.Explain to patient that there will be feeling of warmth as the plaster is applied 3.Apply stockinette and roll cast padding on the extremity or part to be immobilized 4.While keeping the thumb under the forward edge of the bandage, submerge the plaster bandage vertically in water 5.Expel excess water Nursing Interventions Keep the cast and extremity elevated Allow a wet cast 24 to 48 hours to dry (synthetic casts dry in 20 mins)
Handle a wet cast with the palm of the hands until dry Turn the extremity unless contraindicated so that all sides of the wet cast will dry Cool setting on a hair dryer can be used to dry a plaster cast
Examine the skin and cast for pressure areas Monitor the extremity for circulatory impairment such as pain, swelling, discoloration, tingling, numbness, coolness or diminished pulse. Notify the physician immediately if circulatory compromise occurs Prepare for bivalving or cutting the cast if circulatory impairment occurs Monitor the client s temperature
Monitor for the presence of foul odor, which may indicate infection Monitor for drainage and circle the area of drainage on the cast If an open draining area exists on the affected extremity, the physician will make a cut-out portion of the cast or a window Instruct the client not to stick objects inside the cast Teach the client to keep the cast clean and dry Instruct the client in isometric exercises to prevent muscle atrophy
<span> </span> <span>plaster casts</span> Pinexpensive Pheavy
Psets in ~ 3 -1 5 minutes, then takes 24 - 72 h to dry (varies with thickness) Pmessy to apply Pgives more support for bad breaks <span> </span> <span>fiberglass casts</span> Phas durability of plaster but is lighter weight Phardens within minutes Pis porous and \ there are fewer skin problems Pdoes not soften when wet - hair dryer quickly dries skin beneath PCosts more COMPARTMENT SYNDROME What is Compartment Syndrome? An increased pressure within one or more compartments, causing massive compromise of circulation to an area Leads to decreased perfusion and tissue anoxia Within 4 to 6 hours after the onset of CS, neuromuscular damage is IRREVERSIBLE COMPARTMENT SYNDROME Assessment vUnrelieved or incresed pain vSwelling vPain with passive motion vInability to move joints vLoss of sensation (paresthesia) vPulselessness Intervention vNotify the physician immediately BLEEDING may occur beneath a cast if
there is trauma to the skin at the time of injury surgery is required to reduce the fracture this will be documented as ORIF open reduction & internal fixation To detect bleeding visualize the cast carefully. Give particular attention to areas over known wounds &/or incisions dependent areas - remember that liquid flow follows the line of gravity Typical appearance @ 1000 hours Follow-Up continue to monitor instruct client to call you if additional bleeding is noted &/or if s/he notices any other changes notify MD if bleeding continues there is a significant change in vital signs client condition changes
Document in narrative notes & indicate size location vitals other signs of bleeding TRACTION
Traction the application of a pulling force to a part of the body <span>Purpose</span><span>:</span> to minimize muscle spasms; to reduce, align, and immobilize fractures; to reduce deformity; and to increase space between opposing surfaces <span>PRINCIPLES OF EFFECTIVE TRACTION</span> Countertraction must be used to achieve effective traction. Countertraction is the force acting the opposite direction. Usually, the patient's body weight and bed position adjustments supply the needed countertraction. <span>Traction may be applied</span> to the skin (skin traction) directly to the bony skeleton (skeletal traction). Interventions to Clients on Traction Maintain proper body alignment Ensure that the weights hang freely and do not touch the floor Do not remove or lift the weights without a physician s order Ensure that pulleys are not obstructed and that ropes in the pulleys move freely Place knots in the ropes to prevent slipping <span>Skin Traction</span><span>:</span> Skin traction is used to control muscle spasms and to immobilize an area before surgery.
Skin traction is accomplished by using a weight to pull on traction tape or on a foam boot attached to the skin. The amount of weight applied must not exceed tolerance of the skin. Types of Skin Traction used for adults include Buck's extension traction Cervical head halter Pelvic belt Cervical Skin Traction Relieves muscle spasm and compression in the upper extremities and neck Uses a head halter and a chin pad to attach the traction Position the client with HOB elevated 30 to 40 degrees, and attach the weights to a pulley system over the HOB Buck s Skin Traction qUsed to alleviate muscle spasm and immobilizes a lower limb by maintaining a straight pull on the limb with the use of weights qA boot appliance is applied to attach the traction qNot more than 8 to 10 lb of weight should be applied qElevate the foot of bed to provide traction Pelvic Skin Traction Used to relieve lower back, hip, or leg pain and to reduce muscle spasm Apply the traction snugly over the pelvis and iliac crest and attach to weights Use measures as prescribed to prevent the client from slipping down in bed
No more than 2 to 3.5 kg (4.5 to 8 lb) of traction can be used on an extremity. Pelvic traction is usually 4.5 to 9 kg (10 to 20 lb), depending on the weight of the patient. Complication of Skin Traction: qSkin breakdown q qNerve pressure q qCirculatory impairment <span>Skeletal Traction</span><span>:</span> to treat fractures of the femur, the tibia, and the cervical spine. The traction is applied directly to the bone by use of a metal pin or wire Gardner Wells Traction Interventions Monitor color, motion, and sensation of the affected extremity Monitor the insertion sites for redness, swelling or drainage Provide insertion site care as prescribed Balanced Suspension Traction Used with skin or skeletal traction Used to approximate fractures of the femur, tibia, or fibula Produced by a counterforce other than the client Balanced Suspension Traction with Thomas Splint w/ Pearson attachment Interventions
Position the client in low Fowler s on either the side or the back Maintain a 20-degree angle from the thigh to bed Protect the skin from breakdown Provide pin care if pins are used with the skeletal traction Clean pin sites with sterile normal saline and hydrogen peroxide or povidone-iodine as prescribed <span>Nursing Process: The patient in Traction</span> <span>Assessment:</span> evaluate the body part to be placed in traction and neurovascular status (ie, color, temperature, capillary refill, edema, pulses, ability to move, and sensation) and compare it to the unaffected extremity. <span>Diagnosis:</span> Deficient knowledge related to the treatment regimen Anxiety related to health status and the traction device Acute pain related to musculoskeletal disorder Self-care deficit: feeding, bathing/hygiene, dressing/groom ing, and/or toileting related to traction Impaired physical mobility related to musculoskeletal dis order and traction <span>Potential complication:</span> <span>Pressure ulcer </span> <span>Pneumonia </span> <span>Constipation </span> <span>Anorexia </span> <span>Urinary stasis and infection </span> <span>Venous stasis with DVT</span> <span>Planning and Goals:</span> The major goals for the patient in traction may include understanding of the treatment regimen, reduced anxiety, maximum comfort, maximum level of self-care, maximum
mobility within the therapeutic limits of traction, and absence of complications <span>Nursing Intervention:</span> promoting understanding of treatment regimen: Reducing Anxiety. Achieve a maximum level of comfort. Achieving Maximum self care. Attaining maximum Mobility with traction. Monitoring and managing potential complication. <span>Evaluation:</span> Demonstrates knowledge of traction regimen Exhibits reduced anxiety States increased level of comfort Performs self-care activities Demonstrates increased mobility Experiences no complications
You might also like
- A Detailed Lesson Plan in Science GradeDocument6 pagesA Detailed Lesson Plan in Science GradeninaNo ratings yet
- Lesson PlanDocument4 pagesLesson PlanBianca Zamora Labis - MindaroNo ratings yet
- Science CG - With Tagged Sci Equipment - Revised PDFDocument203 pagesScience CG - With Tagged Sci Equipment - Revised PDFRonnelMananganCorpuzNo ratings yet
- Lesson Plan ScienceDocument2 pagesLesson Plan ScienceBianca Zamora Labis - MindaroNo ratings yet
- Lesson Plan ScienceDocument2 pagesLesson Plan ScienceBianca Zamora Labis - MindaroNo ratings yet
- Tale of Two Brothers SynopsisDocument2 pagesTale of Two Brothers SynopsisBianca Zamora Labis - MindaroNo ratings yet
- Crutch WalkingDocument2 pagesCrutch WalkingBianca Zamora Labis - MindaroNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Algorithm For Cant Intubate Cant VentilateDocument8 pagesAlgorithm For Cant Intubate Cant VentilateprashsubbuNo ratings yet
- Crack The Core Exam - Volume 2 4th PDFDocument508 pagesCrack The Core Exam - Volume 2 4th PDFQuỳnh Trâm86% (7)
- The Who Emergency Care System Framework and Assessment Tool: The Ethiopian Federal Moh ExperienceDocument23 pagesThe Who Emergency Care System Framework and Assessment Tool: The Ethiopian Federal Moh ExperienceshoriatNo ratings yet
- ISICAM TimetableDocument8 pagesISICAM TimetableMichael SusantoNo ratings yet
- AnalPleasureSlides PDFDocument59 pagesAnalPleasureSlides PDFGorbatiuc Leonid67% (6)
- Pilot Study of The Effectiveness of Butterfly Technique of SCENAR Therapy On Heart Rate VariabilityDocument7 pagesPilot Study of The Effectiveness of Butterfly Technique of SCENAR Therapy On Heart Rate VariabilityParallaxsterNo ratings yet
- Surgical Notes A Pocket Survival GuideDocument197 pagesSurgical Notes A Pocket Survival Guidevin100% (12)
- Janatin Hastuti, PHD Lab of Bio-& Paleoanthropology Faculty of Medicine, UgmDocument25 pagesJanatin Hastuti, PHD Lab of Bio-& Paleoanthropology Faculty of Medicine, UgmSaharNo ratings yet
- BucensDocument6 pagesBucensEmily GirardNo ratings yet
- Impaired Urinary EliminatonDocument5 pagesImpaired Urinary EliminatonLoriejae Marie DesulocNo ratings yet
- Hip Replacement Pref CardDocument5 pagesHip Replacement Pref CardNikkie SalazarNo ratings yet
- Cesarean Hysterectomy With Cystotomy in Parturient Having Placenta Percreta, Gestational Thrombocytopenia, and Portal Hypertension - A Case ReportDocument4 pagesCesarean Hysterectomy With Cystotomy in Parturient Having Placenta Percreta, Gestational Thrombocytopenia, and Portal Hypertension - A Case ReportasclepiuspdfsNo ratings yet
- Instruments and Equipment For Labour RoomDocument3 pagesInstruments and Equipment For Labour RoomHerrero, Donna Bhel A.No ratings yet
- How To Read A CTG - CTG InterpretationDocument45 pagesHow To Read A CTG - CTG InterpretationlicencaNo ratings yet
- PTB AFO For Fracture Patient at PT - Ottobock Healthcare IndonesiaDocument1 pagePTB AFO For Fracture Patient at PT - Ottobock Healthcare Indonesiamoh Irfan rNo ratings yet
- Cephalometric Evaluation of GrowthDocument79 pagesCephalometric Evaluation of GrowthAhmedsy Ahmedsy AhmedsyNo ratings yet
- Protocolo Triage ObstétricoDocument15 pagesProtocolo Triage ObstétricoNEONATOLOGIA SAN FRANCISCO100% (1)
- ICS and START Triage for Mass Casualty IncidentsDocument66 pagesICS and START Triage for Mass Casualty IncidentsNom Nom100% (1)
- Cast PostDocument3 pagesCast PostsmilekkmNo ratings yet
- Sabiston Textbook of Surgery, 18th Ed. The Biological Basis of Modern Surgical PracticeDocument5 pagesSabiston Textbook of Surgery, 18th Ed. The Biological Basis of Modern Surgical PracticeNunsio NallaNo ratings yet
- Urology Surgical Instruments CatalogDocument11 pagesUrology Surgical Instruments CatalogGerMedUsa.Com100% (1)
- Anatomy Answer KeyDocument16 pagesAnatomy Answer Keylovelots1234No ratings yet
- 3rd Annual Radiology For Non-Radiologists (5-6 Oct 2019)Document2 pages3rd Annual Radiology For Non-Radiologists (5-6 Oct 2019)itnnetworkNo ratings yet
- 5831Document45 pages5831rahimulNo ratings yet
- 123456789-Lectures On Homoeopathic Philosophy by JT Kent-123456789Document181 pages123456789-Lectures On Homoeopathic Philosophy by JT Kent-123456789fapatel95No ratings yet
- Benefit Manual - Aecom IndiaDocument32 pagesBenefit Manual - Aecom IndiaAnil PuvadaNo ratings yet
- Normal Lab Values For PediatricsDocument15 pagesNormal Lab Values For PediatricsJE MagbanuaNo ratings yet
- Bromage Motor Blockade Score - A Score That Has Lasted More Than A LifetimeDocument2 pagesBromage Motor Blockade Score - A Score That Has Lasted More Than A LifetimeGeter PairikasNo ratings yet
- Cerebral Palsy Guide to Types, Causes, Diagnosis and PrognosisDocument14 pagesCerebral Palsy Guide to Types, Causes, Diagnosis and PrognosisAfifah NaurahNo ratings yet
- Alberta Infant ScaleDocument17 pagesAlberta Infant ScaleDuong HungNo ratings yet