Professional Documents
Culture Documents
ICU Nursing
Uploaded by
juanita canoyOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ICU Nursing
Uploaded by
juanita canoyCopyright:
Available Formats
Name: Calleno, Joan Charliz C.
BSN-IV/Section:4/Group: C 06-22-11 ICU Nursing-Nurse Interventions in Acute Exacerbations of COPD Intensive Care Unit (ICU) nursing is commonly referred to as critical care nursing. Critical care nursing deals specifically with the human response to life threatening conditions. Critical care nursing is challenging due to the lifethreatening health situations in the ICU. Critical care nurses are often in high-stress situations which demands complex assessments, high-intensity therapies and interventions and continuous vigilance. Chronic obstructive pulmonary disease (COPD), also known as chronic obstructive lung disease (COLD), is a term used to describe progressive lung diseases, which include emphysema, chronic bronchitis and chronic asthma. The common symptoms of COPD are progressive limitations of the airflow into and out of the lungs and shortness of breath. Emphysema and chronic bronchitis are closely related and patients with COPD may have both, which affects lung function. Emphysema involves destruction of the alveoli in the lungs. Chronic bronchitis is characterized by chronic cough and mucus production. Over a period of time the patient experiences abnormal ventilation-perfusion, insufficient oxygenation of blood (hypoxemia), hypoventilation and right-sided heart failure. People with COPD have a variety of illnesses such as, atelectasis which occurs due to the collapse of part or all of a lung by blockage of the bronchus or bronchioles or by very shallow breathing; bronchiectasis, which is an acquired disorder of the large bronchi that become dilated due to destructive infections of the lungs; congestive heart failure (CHF),a disorder in which the heart loses its ability to pump and cor pulmonale ,where the right ventricle gets enlarged because of pulmonary hypertension from lung disorders. COPD symptoms, when ignored, usually lead to hospitalization in intensive care (ICU) units.
People with chest deformities or neurologic conditions that cause shallow breathing benefit from mechanical devices that assist breathing, such as continuous positive airway pressure, which delivers oxygen through a nose or face mask that prevent airways collapse, even at the end of a breath. Additional respiratory support can be provided with a mechanical ventilator. The primary treatment for acute massive atelectasis, a common complication in COPD is removal of the underlying cause (Brooks-Brunn, 1995). If the blockage cannot be removed by coughing or by suctioning the airways then it should be removed by bronchoscopy. Antibiotics are to be given for any detected infection as in chronic atelectasis, when infection is almost inevitable. Treatment of atelectasis due to deficient or ineffective surfactant is done by treating the low blood oxygen either with mechanical ventilation or positive end expiratory pressure. For cor pulmonale, supplemental oxygen can be administered to increase the level of oxygen in the blood. A low salt diet is recommended. Diuretics are given to remove excess fluid from the body. Calcium channel blockers, intravenous prostacyclin, or the oral medication bosentan are frequently used to treat pulmonary hypertension. Blood thinning anticoagulants are also useful. Oxygen administration relieves symptoms and prolongs survival. Careful intervention is essential because progressive pulmonary hypertension and cor pulmonale often leads to severe fluid retention, life-threatening shortness of breath, shock, and death. Benzodiazepines are not recommended to relieve anxiety in patients with COPD because they decrease respiratory drive and compromise lung function (Brooks-Brunn, 1995). An anxiolytic, buspirone, have been found to be safe in reducing anxiety in COPD patients. Dyspnea is common in individuals with chronic obstructive pulmonary disease. Respiratory assessment of the patient should include present level of dyspnea measured using a quantitative scale such as a visual analogue or numeric rating scale. Usual dyspnea is measured using a quantitative scale such as the Medical Research Council (MRC) Dyspnea
Scale. The other assessments include Vital signs, pulse oximetry, chest auscultation, chest wall movement and shape/abnormalities, presence of peripheral edema, accessory muscle use, presence of cough and/or sputum, ability to complete a full sentence and the level of consciousness. By doing so, nurses should be able to detect stable and unstable dyspnea and acute respiratory failure (American Thoracic Society, 1998). Nurses should also be able to offer interventions for all levels of dyspnea including acute episodes of respiratory distress which includes acceptance of patients' self-report of present level of dyspnea, medications, controlled oxygen therapy, secretion clearance strategies, non-invasive and invasive ventilation modalities, energy conserving strategies, relaxation techniques, and nutritional strategies and breathing retraining strategies. It is important for the nurses to remain with patients during episodes of acute respiratory distress. Nurses have to assess patients for hypoxemia/hypoxia and administer appropriate oxygen therapy for individuals for all levels of dyspnea. Medications include bronchodilators, beta 2 agonists, anticholinergics and methylxanthines, corticosteroids, antibiotics, psychotropics and opioids (www.guidelines.gov). Patient safety checks include circuit leaks; maintenance of positive pressure; adequate inspiratory air flow and not leaving the patient alone. Continuous Positive Airway Pressure Oxygen therapy is part of any ICU and requires absolute attention. Managing the therapy involves maintenance of the desired FIO2; level of positive airway pressure and time period for CPAP therapy, attaching CPAP machine medical air and oxygen gas lines to wall sources, preparation of humidification source ,selection of prescribed FIO2 on oxygen blender, turning flow on to level above 25 litres / min., positioning of rubber securing band behind the patient's head, centred on occiput, positioning of face mask over the patient, adjusting the level of positive expiratory pressure to prescribed level, adjusting inspiratory gas flow so that minimal fluctuations are present on pressure gauge, observing and documenting respiratory rate; work of breathing and SpO2, increasing
inspiratory flow if respiratory work is excessive or the patient complains of continuing dyspnea, maintaining continuous SpO2 monitoring with alarm function in place, maintaining humidification temperature at 36 degree C or at temperature tolerated by the patient (American Thoracic Society, 1998). Patient observations include, visual check every half an hour, documentation of respiratory rate, SpO2, nausea and vomiting, monitoring pulse rate and rhythm; blood pressure; peripheral circulation and proper functioning of humidification system every hour, checking the condition of skin around and under mask and rubber securing band, documentation of condition and interventions, condition of conjunctivae every two hours, auscultation of lungs for equal air entry and palpitation of abdomen for distension every four hours (Vollman,1997). Ventilator-Associated Pneumonia is a common nosocomial infection in the ICU accounting for 13% to 18% of all nosocomial infections (Rello et.al, 1996). Infection may be even due to improper hand washing, not changing the gloves from patient to patient, and contamination of respiratory devices like nebulizers, spirometers, oxygen sensors, bagvalve mask devices, and suction catheters (Shelby Hixson, 1998). Oral care includes brushing the patients teeth, use of solutions and mouthwash to cleanse the mouth, and periodical suctioning of oral secretions. Nasal care and proper cleansing of the nasopharynx reduces bacterial infection. Source: http://www.medicalnewstoday.com/releases/106674.php
Summary: The term chronic obstructive pulmonary disease is used to describe several conditions that lead to airway outflow obstruction. Two acquired conditions that can result in COPD are emphysema and chronic bronchitis. Emphysema is characterized by abnormal permanent enlargement of the air spaces distal to the terminal bronchioles, accompanied by destruction of their walls without obvious fibrosis. Chronic bronchitis is defined as a chronic cough or mucus production lasting at least three months during at least two successive years when other causes of chronic cough have been excluded. Emphysema and chronic bronchitis may exist in a patient with both alveolar destruction and mucous production. In addition, patients with COPD may have some degree of airway inflammation, reactive airway disease, or asthma. When considering the treatment options for the patient with COPD, the underlying pathophysiologic changes must be taken into account. Tracheobronchial infections are believed to be a common inciting cause of acute exacerbations of COPD; however, controversy exists regarding the nature of the infectious agent, as well as its exact role. Sputum obtained from patients with mild to moderately severe chronic bronchitis routinely grow a variety of bacteria in cultures, including Haemophilus influenzae Pseudomonas aeruginosa(15%), Streptococcus
pneumoniae (10%), and Moraxella catarrhalis (9%).7Nonpathogenic bacteria, such as Haemophilus parainfluenzae, account for up to one third of all isolates. Also, the following certain groups of patients are more likely to be
colonized with resistant organisms such as Pseudomonas: patients from nursing homes; patients recently treated with antibiotics; and patients admitted to ICUs. The role of these colonizers in the pathogenesis of acute exacerbation remains unclear, and their presence makes the interpretation of any sputum culture difficult. Some investigators also have proposed thatMycoplasma pneumoniae or Chlamydia pneumoniae may precipitate between 1% and 10% of exacerbations, and others have pointed out that the presence of eosinophilic inflammation in bronchial biopsy specimens of patients with exacerbations is consistent with viruses (notably rhinovirus) playing an important role. Acute exacerbations are clearly associated with environmental exposures as well, as significant correlations between levels of respirable particles (diameter, < 10 m) and ozone have been linked to hospital admission rates. Finally, severe exacerbations may be precipitated by other serious clinical conditions, such as heart failure, nonpulmonary infections, pulmonary embolism, and pneumothorax. Reaction: The ICU setting demands stressful nursing interventions and constant monitoring of the patients especially with conditions like COPD. Nurse interventions should be based on assessment of dyspnea, vital signs, pulse oximetry, chest auscultation, chest wall movement and presence of peripheral edema, cough and/or sputum, ability to complete a full sentence and the level of consciousness. Proper oral and nasal care reduces lung infection.
You might also like
- Application For Permit To Operate (DENR)Document2 pagesApplication For Permit To Operate (DENR)juanita canoyNo ratings yet
- Quick Garlic Pasta Aglio E Olio RecipeDocument1 pageQuick Garlic Pasta Aglio E Olio Recipejuanita canoyNo ratings yet
- Liver CancerDocument1 pageLiver Cancerjuanita canoyNo ratings yet
- MicahgroupDocument7 pagesMicahgroupjuanita canoyNo ratings yet
- Operating Room TeamDocument5 pagesOperating Room Teamjuanita canoyNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Key Points: Schwartz's Principles of Surgery Chapter 23. Arterial DiseaseDocument142 pagesKey Points: Schwartz's Principles of Surgery Chapter 23. Arterial DiseaseMohammad FareedNo ratings yet
- Thoracic Surgeon CVDocument4 pagesThoracic Surgeon CVFrancisco MooreNo ratings yet
- Tammy Querrey Builds Excellence in Heart Care Based On Her Past As A NurseDocument1 pageTammy Querrey Builds Excellence in Heart Care Based On Her Past As A NurseAnonymous hFBFKggFkNo ratings yet
- CCPVDocument16 pagesCCPVdastgirrajaNo ratings yet
- VitiligoDocument1 pageVitiligoaizee_manluluNo ratings yet
- Osce EmergenciesjDocument31 pagesOsce EmergenciesjTess WilliamsNo ratings yet
- Strickland PresentationDocument1 pageStrickland Presentationmariopi2495No ratings yet
- AsphyxiaDocument35 pagesAsphyxiaAna Cristina Montillano100% (1)
- Commercial Index - SV - CarlislecDocument308 pagesCommercial Index - SV - CarlislecRobert RangstanNo ratings yet
- New England Journal Medicine: The ofDocument11 pagesNew England Journal Medicine: The ofahmadto80No ratings yet
- First Draft of A CommentaryDocument4 pagesFirst Draft of A CommentaryPablo VaNo ratings yet
- Auditory Processing DisorderDocument4 pagesAuditory Processing DisorderRuztiqa Kasih Pramudya Vardani100% (1)
- Cranial Nerve Exam TechniquesDocument19 pagesCranial Nerve Exam Techniquesifer_018No ratings yet
- Lateralizing Value of Todd's PalsyDocument3 pagesLateralizing Value of Todd's PalsyLakshya J BasumataryNo ratings yet
- Gap Co2 Cocc 2018Document9 pagesGap Co2 Cocc 2018Cesar Rivas CamposNo ratings yet
- Nursing Care Plan for Skin IntegrityDocument3 pagesNursing Care Plan for Skin IntegrityCrystal Joy Misa100% (1)
- ERA System Brochure1Document6 pagesERA System Brochure1Ana Massiel NarváezNo ratings yet
- Copd (Chronic Obstructive Pulmonary Disease)Document5 pagesCopd (Chronic Obstructive Pulmonary Disease)Kirin JoiezNo ratings yet
- Payment Agreement PDFDocument1 pagePayment Agreement PDFLisa HalajkoNo ratings yet
- Summary of Product Characteristics: 4.1 Therapeutic IndicationsDocument6 pagesSummary of Product Characteristics: 4.1 Therapeutic IndicationsMustika Dwi SusilowatiNo ratings yet
- MOLA's Osteology BooksDocument1 pageMOLA's Osteology BooksMOLA (Museum of London Archaeology)No ratings yet
- Know Your Magnetic FieldDocument75 pagesKnow Your Magnetic FieldAtma Jnani100% (5)
- Hyper Parathyroid IsmDocument7 pagesHyper Parathyroid IsmEllene Mae Dejapa VillasisNo ratings yet
- Multiple SclerosisDocument35 pagesMultiple SclerosisJc SeguiNo ratings yet
- Nres1dm-Chapter I and IIDocument35 pagesNres1dm-Chapter I and IImlmmandapNo ratings yet
- Week 10: Drugs Administered For The Treatment of Diabetes MellitusDocument7 pagesWeek 10: Drugs Administered For The Treatment of Diabetes Mellitusashley larsonNo ratings yet
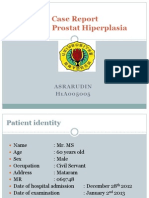
- Case Report on BPH and Heart DiseaseDocument18 pagesCase Report on BPH and Heart DiseaseAsrarudin HamidNo ratings yet
- Fetal valproate syndrome review: teratogenic effects and managementDocument8 pagesFetal valproate syndrome review: teratogenic effects and managementKumar Gavali SuryanarayanaNo ratings yet
- Thyroid CancerDocument82 pagesThyroid Cancerom100% (1)
- Assessing Radial PulseDocument4 pagesAssessing Radial PulseMatthew RyanNo ratings yet