Professional Documents
Culture Documents
Baranwal MASCC 2007
Uploaded by
Amaninder S DhillonOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Baranwal MASCC 2007
Uploaded by
Amaninder S DhillonCopyright:
Available Formats
Efficacy and Safety of Eltrombopag, a Novel Oral Platelet Growth Factor, on Platelet Counts in Patients With Cancer Receiving
Carboplatin/Paclitaxel Chemotherapy
A. Baranwal,1 J. L. A. Fraser,1 D. Jayawardene,1 A. Jagiello-Gruszfeld,2 I. Bondarenko,3 J. L. Mendoza4
GlaxoSmithKline, Collegeville, PA, USA; 2ZOZ MSWiA z Warminsko-Mazurskim Centrum Onkologii, Olsztyn, Poland; 3 Radiodiagnostic and Radiotherapy Chair of Dnepropetrovsk State Medical Academy, Dnepropetrovsk, Ukraine; 4Salem Research Institute, Inc., Salem, VA, USA.
1
INTRODUCTION
Chemotherapy-induced thrombocytopenia (CIT) is a significant source of morbidity for many cancer patients Chemotherapy dose delay and reduction due to thrombocytopenia (TCP) is common Eltrombopag is the first oral platelet growth factor for the treatment of TCP Eltrombopag is a thrombopoietin receptor agonist that boosts platelet production and may reduce the severity of TCP in patients receiving chemotherapy Eltrombopag has previously been shown to increase platelet counts in healthy volunteers and in patients with refractory idiopathic thrombocytopenic purpura and hepatitis C-associated TCP This analysis assessed the safety and efficacy of eltrombopag in cancer patients receiving chemotherapy at risk for CIT
METHODS: PATIENTS
Inclusion Criteria Patients were to have the following: Advanced solid tumors Received carboplatin/paclitaxel Study Populations Modified intent-to-treat population (mITT): Patients who were randomized and administered at least 1 dose of the study treatment in Cycle 1 and for whom baseline and at least 1 on-therapy platelet count was collected Safety population: Patients who received at least 1 dose of study medication during any cycle
RESULTS: SAFETY
The prevalence of adverse events in patients who received placebo, eltrombopag 50 mg, eltrombopag 75 mg, or eltrombopag 100 mg were 83%, 75%, 68%, and 87%, respectively (Table 2) The prevalence of serious adverse events in patients who received placebo, eltrombopag 50 mg, eltrombopag 75 mg, or eltrombopag 100 mg were 13%, 9%, 7%, and 13%, respectively (Table 2)
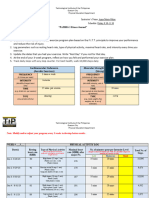
TABLE 2. OVERALL SUMMARY OF ADVERSE EVENTS DURING 2 CYCLES OF TREATMENT
Placebo (n = 46) n (%) Events 38 (83) 6 (13) 13 (28) 4 (9) 218 6 30 4 Eltrombopag 50 mg (n = 44) n (%) Events 33 (75) 4 (9) 7 (16) 0 (0) 227 6 19 0 Eltrombopag 75 mg (n = 44) n (%) Events 30 (68) 3 (7) 11 (25) 4 (9) 137 6 26 4 Eltrombopag 100 mg (n = 46) n (%) Events 40 (87) 6 (13) 14 (30) 11 (24) 210 6 17 11 Total (N = 180) n (%) Events 141 (78) 792 19 (11) 45 (25) 19 (11) 24 92 19
Characteristic Any AE Serious AE Drug-related AE AE that lead to withdrawal
RESULTS: BASELINE CHARACTERISTICS PRIMARY OBJECTIVE
To evaluate the efficacy of oral eltrombopag compared with placebo in Cycle 2 of carboplatin/paclitaxel chemotherapy, administered to patients with an advanced solid tumor Patients were primarily female (58%) and had a median age of 58 years (Table 1) 78% of patients had baseline platelet counts 250,000/L (Table 1) Most patients had either non-small cell lung (61%) or ovarian (26%) tumors (Table 1)
TABLE 1. PATIENT CHARACTERISTICS
Serious AE that lead to withdrawal Ongoing AE at the end of study/withdrawal
AE, adverse event.
1 (2)
0 (0)
2 (5)
4 (9)
7 (4)
11 (24)
25
12 (27)
20
9 (20)
11
14 (30)
20
46 (26)
76
The most common adverse events recorded during 2 cycles of treatment are presented in Table 3
TABLE 3. SUMMARY OF THE MOST COMMON ADVERSE EVENTS DURING 2 CYCLES OF TREATMENT
Placebo (n = 46) 38 (83) 15 (33) 10 (22) 14 (30) 8 (17) 7 (15) 4 (9) 4 (9) 3 (7) 5 (11) 5 (11) 7 (15) 3 (7) 3 (7) 1 (2) 3 (7) 1 (2) 0 (0) 3 (7) Eltrombopag 50 mg (n = 44) 33 (75) 16 (36) 17 (39) 6 (14) 4 (9) 7 (16) 8 (18) 5 (11) 5 (11) 1 (2) 3 (7) 3 (7) 5 (11) 5 (11) 1 (2) 4 (9) 6 (14) 4 (9) 4 (9) Eltrombopag 75 mg (n = 44) 30 (68) 13 (30) 8 (18) 9 (20) 3 (7) 4 (9) 4 (9) 4 (9) 5 (11) 6 (14) 1 (2) 1 (2) 2 (5) 1 (2) 4 (9) 0 (0) 1 (2) 2 (5) 0 (0) Eltrombopag 100 mg (n = 46) 40 (87) 10 (22) 12 (26) 10 (22) 8 (17) 3 (7) 4 (9) 5 (11) 3 (7) 3 (7) 5 (11) 2 (4) 2 (4) 3 (7) 6 (13) 3 (7) 2 (4) 3 (7) 2 (4) Total (N = 180) 141 (78) 54 (30) 47 (26) 39 (22) 23 (13) 21 (12) 20 (11) 18 (10) 16 (9) 15 (8) 14 (8) 13 (7) 12 (7) 12 (7) 12 (7) 10 (6) 10 (6) 9 (5) 9 (5)
METHODS: STUDY DESIGN
Characteristic Placebo (n = 45) 58 (23-73) 29 (64.4) 16 (35.6) 37 (82.2) 20 (44.4) 24 (53.3) 1 (2.2) 27 (60.0) 13 (28.9) 5 (11.1)
Eltrombopag 50 mg (n = 41) 58 (35-75) 20 (48.8) 21 (51.2) 25 (61.0) 20 (48.8) 21 (51.2) 0 (0.0) 26 (63.4) 8 (19.5) 7 (17.1)
Eltrombopag 75 mg (n = 41) 59 (33-75) 27 (65.9) 14 (34.1) 35 (85.4) 16 (39.0) 25 (61.0) 0 (0.0) 25 (61.0) 10 (24.4) 6 (14.6)
Eltrombopag 100 mg (n = 43) 59 (34-81) 22 (51.2) 21 (48.8) 35 (81.4) 14 (32.6) 29 (67.4) 0 (0.0) 25 (58.1) 14 (32.6) 4 (9.3)
Total (N = 170) 58 (23-81) 98 (57.6) 72 (42.4) 132 (77.6) 70 (41.2) 99 (58.2) 1 (0.6) 103 (60.6) 45 (26.5) 22 (12.9)
Characteristic, n (%) Any Nausea Alopecia Neutropenia Vomiting Leukopenia Arthralgia Fatigue Diarrhea Anemia
Randomized, double-blind, multicenter phase II study Placebo and eltrombopag 50, 75, and 100 mg were administered orally for 10 days (Days 2-11) of each cycle Carboplatin (AUC 5-6 IV over 15-30 min) and paclitaxel (175-225 mg/m2 IV over 3 hours) were administered on Day 1 and repeated every 21 days Patients received a maximum of 8 cycles of placebo or eltrombopag treatment
Figure 1. Study design.
Begin Cycle 2 (Day 22) Carboplatin and paclitaxel (Day 1) End Cycle 1 (Day 21)
Age, y Median (range) Gender, n (%) Female Male Platelet count 250,000/L, n (%) ECOG/Zubrod score, n (%) 0 1 2 Tumor type, n (%) Non-small cell lung Ovary Other
ECOG, Eastern Cooperative Oncology Group.
Constipation
RESULTS: DR UG DOSES
All groups received comparable baseline doses of carboplatin and paclitaxel Mean doses of carboplatin for the placebo and eltrombopag 50-, 75-, and 100-mg arms were 556.1, 545.8, 567.7, and 531.8 mg, respectively Mean doses of paclitaxel for the placebo and eltrombopag 50-, 75-, and 100-mg arms were 320.7, 327.8, 321.1, and 313.8 mg, respectively
Pain in extremity Myalgia Pyrexia Thrombocythemia Asthenia Headache Anorexia Cough
Eltrombopag or placebo (Days 2-11)
METHODS: PRIMARY STUDY ENDPOINT
Change in platelet count from Day 1 in Cycle 2 to the platelet nadir in Cycle 2 Platelet nadir is defined as the minimum platelet count during Days 8-18
RESULTS: EFFICACY
All patients who received eltrombopag had higher platelet counts at the end of Cycles 1 and 2 (Figure 2A and 2B, respectively) compared to those who received placebo
Figure 2A. Mean (SD) platelet counts by visit in Cycle 1.
700
Figure 2B. Mean (SD) platelet counts by visit in Cycle 2.
700
Platelet count (x1,000/L)
500 400 300 200 100 0 1 2 5 8 11 15 18
Placebo Eltrombopag 50 mg Eltrombopag 75 mg Eltrombopag 100 mg
Platelet count (x1,000/L)
METHODS: SECONDARY STUDY ENDPOINTS
Change in platelet count from Day 1 in Cycle 1 to the platelet nadir in Cycle 1 Safety and tolerability as indicated by physical exam, laboratory tests, and adverse event reporting
600
600 500 400 300 200 100 0 1 2 5 8 11 15 18
Placebo Eltrombopag 50 mg Eltrombopag 75 mg Eltrombopag 100 mg
Day
Day
CONCLUSIONS
Eltrombopag 50, 75, and 100 mg resulted in a dose-dependent increase in platelet counts from Day 8 to the end of Cycles 1 and 2 In this study, the safety profile of eltrombopag was comparable to placebo Pharmacodynamic data from this study will be used to design future studies to understand the optimal eltrombopag schedules for improving platelet nadir counts following chemotherapy
Poster presented at the 20th Anniversary International Multinational Association of Supportive Care in Cancer (MASCC)/International Society for Oral Oncology (ISOO) Symposium, June 28-30, 2007, St. Gallen, Switzerland.
You might also like
- Neuroendocrine Tumors: Surgical Evaluation and ManagementFrom EverandNeuroendocrine Tumors: Surgical Evaluation and ManagementJordan M. CloydNo ratings yet
- Comparison of Low Dose, Single Loading Dose, and Standard Pritchard Regimen of Magnesium Sulfate in Antepartum EclampsiaDocument4 pagesComparison of Low Dose, Single Loading Dose, and Standard Pritchard Regimen of Magnesium Sulfate in Antepartum EclampsiaMartha MaiguaNo ratings yet
- SUGAR-DM-HF TrialDocument38 pagesSUGAR-DM-HF TrialToheed AshrafNo ratings yet
- Vel CadeDocument20 pagesVel CadeSerly MarcelinaNo ratings yet
- Otite Si SinDocument29 pagesOtite Si Sinminerva_stanciuNo ratings yet
- 1 s2.0 S0735109708008656 MainDocument10 pages1 s2.0 S0735109708008656 MainraniahNo ratings yet
- Standard Operating Procedure FOR Molecular Genetics Test Spinal Muscular Atrophy (Sma) AT Human Genome Center, Usm Health Campus, Kubang KerianDocument4 pagesStandard Operating Procedure FOR Molecular Genetics Test Spinal Muscular Atrophy (Sma) AT Human Genome Center, Usm Health Campus, Kubang KerianmyalvinNo ratings yet
- Improved Survival Outcome of Childhood Acute Myeloid Leukemia With Intensified Chemotherapy in Chinese ChildrenDocument12 pagesImproved Survival Outcome of Childhood Acute Myeloid Leukemia With Intensified Chemotherapy in Chinese ChildrenneizhaNo ratings yet
- Professional Information BrochureDocument16 pagesProfessional Information BrochureKane SmithNo ratings yet
- Kohan 2011Document10 pagesKohan 2011David DwiputeraNo ratings yet
- Empa-Kidney 1Document5 pagesEmpa-Kidney 1api-660408385No ratings yet
- Ustekinumab Psoriasis SingaporeDocument14 pagesUstekinumab Psoriasis SingaporeCHONG WEI SHENGNo ratings yet
- ASH CaplacizumabDocument4 pagesASH CaplacizumabMagdalena Górska-KosickaNo ratings yet
- Strobilanthes CrispusDocument46 pagesStrobilanthes CrispusHilman AdzimNo ratings yet
- CCO Gastric Cancer LL SlidesDocument63 pagesCCO Gastric Cancer LL SlidesPoncho Silva100% (1)
- Ventavis® (Iloprost) Inhalation SolutionDocument19 pagesVentavis® (Iloprost) Inhalation SolutionImanuel Far-FarNo ratings yet
- Ricci F Guffanti F Damia G Broggini M Author Information: BackgroundDocument10 pagesRicci F Guffanti F Damia G Broggini M Author Information: BackgroundJennyJessicaSNo ratings yet
- Article Type: Original Article Journal: Annals of Oncology TitleDocument30 pagesArticle Type: Original Article Journal: Annals of Oncology TitleLeisa A PNo ratings yet
- The MERCURY I OpenDocument12 pagesThe MERCURY I OpenSharmil IyapillaiNo ratings yet
- Molitch - Hot Topics Cushings Disease and AcromegalyDocument69 pagesMolitch - Hot Topics Cushings Disease and AcromegalyMaryONo ratings yet
- Electrocorticographic Monitoring As An Alternative Tool For The Pre-Surgical Evaluation of Patients With Bi-Temporal EpilepsyDocument7 pagesElectrocorticographic Monitoring As An Alternative Tool For The Pre-Surgical Evaluation of Patients With Bi-Temporal Epilepsydavidmy227464No ratings yet
- Dysphagia: Impact On Quality of Life After Radio (Chemo) Therapy of Head and Neck CancerDocument7 pagesDysphagia: Impact On Quality of Life After Radio (Chemo) Therapy of Head and Neck CancerNurul Afika LubisNo ratings yet
- Breast Cancer FinaleDocument30 pagesBreast Cancer Finaleخايزورا راهيمNo ratings yet
- ASCO 2010 Tivozanib PosterDocument1 pageASCO 2010 Tivozanib PosterAndika AfriansyahNo ratings yet
- Capecitabina BQQDocument8 pagesCapecitabina BQQAccelerium ClinicalNo ratings yet
- 2020-Iwamoto - Weekends Off Lenvatinib Dose HolidayDocument16 pages2020-Iwamoto - Weekends Off Lenvatinib Dose Holiday728transportNo ratings yet
- ContentServer - Asp 13Document7 pagesContentServer - Asp 13Fitria NurulfathNo ratings yet
- Three-Year Follow-Up of A Randomized Trial Comparing Focal/Grid Photocoagulation and Intravitreal Triamcinolone For Diabetic Macular EdemaDocument7 pagesThree-Year Follow-Up of A Randomized Trial Comparing Focal/Grid Photocoagulation and Intravitreal Triamcinolone For Diabetic Macular EdemaDikiArmaDuhaAlaydrusNo ratings yet
- A Multicentre, Randomised, Double Blind, Phase IIDocument11 pagesA Multicentre, Randomised, Double Blind, Phase IIveaceslav coscodanNo ratings yet
- EUA 2019 Outcomes of SGLT2 Inhibitors Use in Diabetic RenalDocument4 pagesEUA 2019 Outcomes of SGLT2 Inhibitors Use in Diabetic RenalLaura GarciaNo ratings yet
- A Comparison of Efficacy Between Rebamipide and Omeprazole in The Treatment of Nsaids GastropathyDocument6 pagesA Comparison of Efficacy Between Rebamipide and Omeprazole in The Treatment of Nsaids GastropathyNurulAlviFauzianaNo ratings yet
- Impetigo Due To Staphylococcus Aureus (Methicillin - Susceptible Isolates Only) or Streptococcus PyogenesDocument18 pagesImpetigo Due To Staphylococcus Aureus (Methicillin - Susceptible Isolates Only) or Streptococcus PyogenesjoelrequenaNo ratings yet
- Age +estimated+glomerular+filtration+rate+and+ejection+fraction+score+predicts+contrast-Induced+acute+kidney+injury+in+patients+with+diabetes+and+chronic+kidney+disease +insight+from+the+TRACK-D+studyDocument5 pagesAge +estimated+glomerular+filtration+rate+and+ejection+fraction+score+predicts+contrast-Induced+acute+kidney+injury+in+patients+with+diabetes+and+chronic+kidney+disease +insight+from+the+TRACK-D+studyangga_darmawan26No ratings yet
- (750299866) Niesvizky3135Document24 pages(750299866) Niesvizky3135Teuta DuletićNo ratings yet
- AMADEO Full PaperDocument6 pagesAMADEO Full PaperAnggraeni PermatasariNo ratings yet
- The Safety of COX-2 Inhibitors: John J. Cush, MD Presbyterian Hospital of DallasDocument29 pagesThe Safety of COX-2 Inhibitors: John J. Cush, MD Presbyterian Hospital of DallaskitsilcNo ratings yet
- Endocrinology Metabolism Saq Sample Exam eDocument11 pagesEndocrinology Metabolism Saq Sample Exam eعمر كمالNo ratings yet
- CYP2C9 Polymorphism in Non-Steroidal Anti-Inflammatory Drugs-Induced GastropathyDocument6 pagesCYP2C9 Polymorphism in Non-Steroidal Anti-Inflammatory Drugs-Induced GastropathyFariz NurNo ratings yet
- Vavuranakis 2022Document7 pagesVavuranakis 2022Amro MahmoudNo ratings yet
- Upper Gastrointestinal Cancers in The ElderlyDocument32 pagesUpper Gastrointestinal Cancers in The ElderlyRadha ChiombonNo ratings yet
- Nolvadex: TabletsDocument38 pagesNolvadex: TabletsDwi Kartika SariNo ratings yet
- Jurnal Reading 1 DR NatasshaDocument28 pagesJurnal Reading 1 DR NatasshaRama TanjungNo ratings yet
- External SourceDocument9 pagesExternal SourceEmre AktaşNo ratings yet
- Esophageal CancerDocument21 pagesEsophageal CancerYogesh ShindeNo ratings yet
- Rituximab For Severe Membranous Nephropathy: A 6-Month Trial With Extended Follow-UpDocument11 pagesRituximab For Severe Membranous Nephropathy: A 6-Month Trial With Extended Follow-UpNarinder SharmaNo ratings yet
- Artigo Samuel ValençaDocument5 pagesArtigo Samuel ValençaKleber DennisNo ratings yet
- Cam40002 0234Document9 pagesCam40002 0234Domenico LombardiniNo ratings yet
- Thyroid Eye Disease PresentationDocument39 pagesThyroid Eye Disease PresentationyoadhajyahyaNo ratings yet
- The Oncologist 1998 Goumas 50 3Document4 pagesThe Oncologist 1998 Goumas 50 3Kammi HumedNo ratings yet
- Erbitux MonotherapyDocument7 pagesErbitux MonotherapyMaulik PatelNo ratings yet
- BangaloreDocument3 pagesBangaloreAulia MursyidaNo ratings yet
- Metabolic Complications of Endocrine Surgery in Companion AnimalsDocument22 pagesMetabolic Complications of Endocrine Surgery in Companion AnimalsEduardo PalaciosNo ratings yet
- Zhang COR 2022Document12 pagesZhang COR 2022icemoonNo ratings yet
- PDF JTN 164Document4 pagesPDF JTN 164Gede SuputraNo ratings yet
- Amant Frederic MD PHD Gynaecological Oncologist Uz Gasthuisberg Katholieke Universiteit Leuven BelgiumDocument32 pagesAmant Frederic MD PHD Gynaecological Oncologist Uz Gasthuisberg Katholieke Universiteit Leuven Belgiumtriunfadorforever-1No ratings yet
- Gastric Cancer Discussion Slides - Final Version - PptnewDocument18 pagesGastric Cancer Discussion Slides - Final Version - PptnewPundi Pandan Putri PinantiNo ratings yet
- Teprotumumab - EyeWikiDocument4 pagesTeprotumumab - EyeWikiCristina Georgiana ȘerbanNo ratings yet
- Use of FET-PET in Glioblastoma: Journal Club May 4 2011Document41 pagesUse of FET-PET in Glioblastoma: Journal Club May 4 2011tienloNo ratings yet
- Development and Preclinical Evaluation of Therapeutic Radiopharmaceuticals Based On Lu-177 and Y-90 Labeled Monoclonal Antibodies andDocument39 pagesDevelopment and Preclinical Evaluation of Therapeutic Radiopharmaceuticals Based On Lu-177 and Y-90 Labeled Monoclonal Antibodies andEmilija JanevikNo ratings yet
- Challenges in Managing Hepatitis C Virus InfectionDocument57 pagesChallenges in Managing Hepatitis C Virus InfectionAhmed ElwassiefNo ratings yet
- Notice: Reports and Guidance Documents Availability, Etc.: Engagement of Institutions in Human Subjects ResearchDocument4 pagesNotice: Reports and Guidance Documents Availability, Etc.: Engagement of Institutions in Human Subjects ResearchJustia.comNo ratings yet
- Week 8 Pesonality DevelopmentDocument8 pagesWeek 8 Pesonality DevelopmentLawrence ToquirreNo ratings yet
- Botox For SyringomaDocument3 pagesBotox For SyringomaAdi WijayantoNo ratings yet
- Argumentative Essay: Is Meat Murder?Document2 pagesArgumentative Essay: Is Meat Murder?Petra Gabriella PatakiNo ratings yet
- NURSING CARE PLAN - JayDocument8 pagesNURSING CARE PLAN - JayJaylord VerazonNo ratings yet
- Healthy Lives, Brighter Futures - The Strategy For Children and Young People's HealthDocument35 pagesHealthy Lives, Brighter Futures - The Strategy For Children and Young People's Healthdhubhat4056No ratings yet
- White Lies ReportDocument85 pagesWhite Lies ReportinvisibleveganNo ratings yet
- IPE Interprofessional EducationDocument10 pagesIPE Interprofessional EducationdewaNo ratings yet
- AGE Case PresentationDocument14 pagesAGE Case Presentationdodong skyroseNo ratings yet
- IMT PGDM - Executive: We Are Suited Up!Document3 pagesIMT PGDM - Executive: We Are Suited Up!Anuj SachdevNo ratings yet
- Show Me Strong Recovery - Phase 1 GuidanceDocument8 pagesShow Me Strong Recovery - Phase 1 GuidanceKevinSeanHeldNo ratings yet
- REGO ET EL TQUK Assessment Syllabus 5-15-2023Document41 pagesREGO ET EL TQUK Assessment Syllabus 5-15-2023Itz Lovaboi ChurchillNo ratings yet
- Free Essay On CovidDocument4 pagesFree Essay On CovidJade LazarNo ratings yet
- Hse Plan Asl PDFDocument87 pagesHse Plan Asl PDFBudi Prasetyo100% (1)
- The DR Sebi Diet A Healing Journey 100 - DR Sebi Research CenterDocument159 pagesThe DR Sebi Diet A Healing Journey 100 - DR Sebi Research CenterDEEJAY NERVSNo ratings yet
- Doroga Bahrm21s1 Pe003 Fitness Journal LogDocument4 pagesDoroga Bahrm21s1 Pe003 Fitness Journal LogJeah Joyce LagrimasNo ratings yet
- Anglais 2ndeDocument33 pagesAnglais 2ndeMario RobillardNo ratings yet
- The START and JumpSTART MCI Triage ToolsDocument54 pagesThe START and JumpSTART MCI Triage ToolsAdreiTheTripleANo ratings yet
- Ayurveda Positive HealthDocument2 pagesAyurveda Positive HealthmuralipmdNo ratings yet
- IDocument14 pagesIjasdeepkaurnagra100% (1)
- Brosur EnglishDocument2 pagesBrosur EnglishSumiari LuhNo ratings yet
- Neonatal Respiratory Distress SyndromeDocument12 pagesNeonatal Respiratory Distress SyndromeRazelVillanueva67% (3)
- CSHPDocument2 pagesCSHPKeren EbarleNo ratings yet
- CarcinosinDocument42 pagesCarcinosinHilery DorrianNo ratings yet
- EcardDocument2 pagesEcardBITI Education Pvt. Ltd.No ratings yet
- Exercise and Disease Management Second Edition PDFDocument253 pagesExercise and Disease Management Second Edition PDFGajen Singh100% (1)
- Health Immunization MMR FormDocument2 pagesHealth Immunization MMR FormHenrique Delfino Almeida AlvesNo ratings yet
- Recalls 6Document16 pagesRecalls 6Charisse Caydan0% (1)
- IV Therapy - Asynchronous ActivityDocument2 pagesIV Therapy - Asynchronous ActivityNicole Chloe OcanaNo ratings yet
- Official MDR PDFDocument1 pageOfficial MDR PDFBesarioLouiseCassandraNo ratings yet