Professional Documents
Culture Documents
Emerging Opportunities
Uploaded by
Hazel CabreraOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Emerging Opportunities
Uploaded by
Hazel CabreraCopyright:
Available Formats
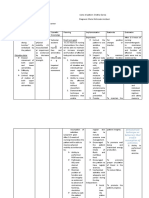
EMERGING OPPORTUNITIES Within the traditional hospital setting, the levels of nursing hierarchy are established: vice president/director
r of nursing, nurse managers, and staff nurses. This hierarchy allow for promotion and advancement. Since the mid-1980s, however, the trend has been to flatten the levels of nursing management; that is, have fewer managers and additional clinical nurses including bedside nurses, nurses with expanded roles, and advanced practice nurse.
Certification Professional certification in nursing is a measure of distinctive nursing practice. This is an example of professional credentialing and is voluntary process undertaken by practicing nurses. The rise in consumerism in the face of a compelling nursing shortage and the professions movement to elevate nursing as a career option have given prominence to the value of certification in nursing ( Shirley, 2005). Basic eligibility requirements for specialty nursing certification often include the following: Hold a currently active RN licensure in its territories. Have practiced the equivalent of two years full-time as an RN. Hold a baccalaureate or higher degree in nursing. Note that candidates with an associate degree/ diploma may apply for certification in several areas of nursing practice. Have a minimum of 2000 hours of clinical practice within the past three years.
Traveling Nurse As the demand for nursing has increased, the supply has often been low, and hospitals are frequently understaffed. One option o fill the nursing shortage is traveling nurse. These nurses usually work in three-month assignments on the same unit. The benefits to the health care institution of using traveling nurses include having a nurse with a variety of experiences providing continuity of care for a three-month period. Traveling nurse need to be aware of differing nursing methodologies and licensure requirements from state to state and will require a license for each state in which they practice. Most travelers exhibit flexibility, adaptability, assertiveness, strong organizational and interpersonal skills, confidence, independence, and the ability to learn new skills and techniques.
Flight Nursing
In numerous tertiary care centers, nurses are functioning in the role of flight nurse for both helicopter and fixed-wing transports. Flight nursing actually started in 1933 with the emergency Flight Corps of the Armed Services which present in both the Korea and Vietnam wars. The concept of air ambulance was initiated in Denver in 1972. One needs numerous advanced technical skills to practice flight nursing, such as patient intubation, EKG interpretation, intravenous (IV) and chest tube insertion, medication administration, sedation, and central line placement. The vast majority of flight teams consist of an RN and respiratory therapist. Although there are no true national standards for becoming flight nurse, most of the opportunities available nationally require the following: Two to three years critical care experience Advanced Cardiac Life Support certificate (ACLS) Pediatric Advanced Life Support certificate (PALS) Neonatal Resuscitation Program (NRP) Graduation from a nationally recognized trauma program. Certification such as Critical Care Registered Nurse (CCRN), Certified Emergency Nurse (CEN), and Certified Flight Registered Nurse (CFRN) may also be required.
Health Care Sales/ Pharmaceutical Representatives Some nurses have left clinical staff nursing and have become representatives for companies that work in conjunction with traditional health care institutions. There are frequently many salary enhancement, or perks, given with these positions, including having a company car, going on business trips, attending national and regional meetings and conferences, participating in profit-sharing and stock option plans, and meeting a variety of health care personnel.
Case Manager The Case Management Society of America defines case management as a collaborative process which assesses, plans, implements, coordinates, and evaluates options and services to meet an individuals health needs through communication and available resources. The ANA defines goals of case management as providing quality health care along a continuum, decreasing fragmentation of care across many setting, enhancing the patients quality of life, and cost containment. In performing the role, the nurse care manager should have expert clinical skills and knowledge of the health care system, health care finances, and legal issues, as well as be an effective communicator. Nurse case managers must provide care that focuses on outcome achievement and assist in arranging, coordinating, and monitoring patient care services.
Nurse Entrepreneur Many nurses are leaving the bedside for the world of entrepreneurship in a variety of consultative, educational, or technical areas. The term entrepreneurship is an interpretation of a French word that means to undertake (Simpson, 1998). Merriam Webster Collegiate Dictionary describes an entrepreneur as one who organizes, promotes, and manages risk for an activity (2003). Some of the major characteristics and attributes of nurse entrepreneurs include te following: Are visionary, self motivated, and a risk taker Ave common sense Are good decision makers and problem solvers Are self confident, assertive, autonomous, and creative Are responsive to a perceived need Are market driven, with good financial foresight Recognize the possibility of success as well as the possibility of failure.
Wound, Ostomy, Continence Nurse Specialist In 1958 the field of enterostomal therapy was initiated at Cleveland Clinic, with the first enterostomal therapists (ETs) being nonnurses. The first nursing training program was started in 1961, and in 1972, new standards for the schools of enterostomal therapy were established. The year 1976 marked a significant change when the governing body of International Association of Enterostomal Therapists determined that only RNs would be admitted to enterostomal therapy educational programs. Nurses with this training and education practice both in hospitals and community-based settings such as visiting nurse associations, public health, nursing homes, and long-term care facilities. Over the past o years, these specialists have truly become the clinical experts in managing patients with ostomies, alterations in skin integrity, and wounds.
ADVANCED PRACTICE NURSING The concept of advanced practice nursing originated in the mid-to late nineteenth century, with the creation of the role of nurse anesthetist. The concept further developed in the twentieth century with nurse-midwifery, clinical nurse specialists, and finally, nurse practitioners. Why is there a need for advanced practice nurses (APNs)? The last quarter of the twentieth century taught that detection, prevention, early intervention, and education are not only cost-effective but also rational. APNs are ideally suited to deliver this type of health care.
In 1992, the ANA define APNs nurses who have a graduate degree in nursing and who conduct comprehensive health assessments, demonstrate a high level of autonomy, and possess expert skills in the diagnosis and treatment of complex responses of individuals, families, communities to actual or potential health problems. The AACN has provided a position statement that describes the APN as an umbrella term appropriate for a licensed registered nurse prepared at the graduate degree level with specialized knowledge and skills that are applied within a broad range of patient populations in a variety of practice settings. Are the APNs contributions unique and valuable, and can this be shown to others? Consider the following: o Clinical nurse specialist (CNS): In a hospital setting, the CNS must be able to identify how performance contributes to the patient-focused mission and goals of the organization. o Certified nurse midwife (CNM): The CNMs ability to better meet patients needs, or to provide services to groups of patients at a lower cost than services provided by practitioners, should be measurable. o Nurse practitioner (NP): In both inpatient and outpatient settings, the NP needs to document both the quantity and quality of services provided to patients and the NPs ability to reduce hospitalization. o Certified registered nurse anesthetist (CRNA): In evaluating anesthesia services in a chronic low back pain clinic, the CRNA should clearly document quality of service and patient outcomes. Clinical nurse specialist/Nurse practitioner (CNS/NP): A combined role Historically, the major differences between the CNS and NP were the settings and focus of their practice. The CNS role has been credited with creating an advanced level of nursing with an eye toward theory-based practice. The NPs have been credited with the movement of nursing beyond traditional roles and increasing the public awareness of advanced practice nursing. Following are some factors to consider when examining these two roles: Patient populations Future roles for CNS and NP Narrower perspective and focus for both the CNS and NP Horizontal violence within nursing nurses fighting among themselves.
You might also like
- PrintDocument6 pagesPrintHazel CabreraNo ratings yet
- NCP of Impaired MobilityDocument3 pagesNCP of Impaired MobilityHazel Cabrera0% (1)
- FatsDocument8 pagesFatsHazel CabreraNo ratings yet
- Hot PacksDocument2 pagesHot PacksHazel CabreraNo ratings yet
- Related StudiesDocument1 pageRelated StudiesHazel CabreraNo ratings yet
- Normal ValuesDocument6 pagesNormal ValuesHazel CabreraNo ratings yet
- BSN 3Document1 pageBSN 3Hazel CabreraNo ratings yet
- LabsDocument8 pagesLabsHazel CabreraNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Adi Setya Frida Utami - FIKES PDFDocument108 pagesAdi Setya Frida Utami - FIKES PDFZyy VyeNo ratings yet
- Electromyography & It's Application in OrthodonticsDocument22 pagesElectromyography & It's Application in Orthodonticsprasadgayake100% (1)
- Mental Practice in Chronic StrokeDocument6 pagesMental Practice in Chronic StrokeIsa AbdantauhidNo ratings yet
- Antenatal CareDocument6 pagesAntenatal CareFancy DisouzaNo ratings yet
- Pathogenic Fungal Infection in The Lung: Zhi Li, Gen Lu and Guangxun MengDocument20 pagesPathogenic Fungal Infection in The Lung: Zhi Li, Gen Lu and Guangxun Mengbanteng wibisonoNo ratings yet
- Chapter6 - Feeds and Feeding The FishDocument23 pagesChapter6 - Feeds and Feeding The Fishፋሲል ታደሰ100% (3)
- Automatic Stop Orders (ASO)Document3 pagesAutomatic Stop Orders (ASO)Bae BeeNo ratings yet
- Farfalle With Creamy Bacon Sauce - Spend With PenniesDocument2 pagesFarfalle With Creamy Bacon Sauce - Spend With PenniesrectagleNo ratings yet
- Lifeline Supreme BrochureDocument5 pagesLifeline Supreme BrochureSumit BhandariNo ratings yet
- Listening ComprehensionDocument5 pagesListening ComprehensionLaura michell Núñez SuarezNo ratings yet
- Gout Guide: Lifelong Transformation, One Healthy Habit at A Time®Document9 pagesGout Guide: Lifelong Transformation, One Healthy Habit at A Time®Rocco McWhitebeardNo ratings yet
- Match The ProverbsDocument1 pageMatch The ProverbsКристин ВалентиноваNo ratings yet
- Anatomy of The Male Reproductive SystemDocument70 pagesAnatomy of The Male Reproductive SystemDaniel HikaNo ratings yet
- Practical Research 2Document6 pagesPractical Research 2meioNo ratings yet
- Life - Line ECMO Sell - Sheet ECMO FEB22 1 WebDocument2 pagesLife - Line ECMO Sell - Sheet ECMO FEB22 1 WebJavier Dario Cifuentes SandovalNo ratings yet
- SSB201 Group Assigment 1 - Design ThinkingDocument3 pagesSSB201 Group Assigment 1 - Design ThinkingLe CuongNo ratings yet
- Nov Art IsDocument6 pagesNov Art IsSaran KuttyNo ratings yet
- Woman Burned by Acid in Random Subway Attack Has 16th SurgeryDocument1 pageWoman Burned by Acid in Random Subway Attack Has 16th Surgeryed2870winNo ratings yet
- ACTIVITY DESIGN-first AidDocument4 pagesACTIVITY DESIGN-first AidShyr R Palm0% (1)
- HDR 2015 Statistical AnnexDocument73 pagesHDR 2015 Statistical AnnexsssshekharNo ratings yet
- MNT CancerDocument62 pagesMNT CancerSaufi ZakariaNo ratings yet
- BBB Month 10 Workout LogDocument8 pagesBBB Month 10 Workout LogLi SaNo ratings yet
- Moral Issues of Birth DeformitiesDocument3 pagesMoral Issues of Birth DeformitiesPham PhamIoNo ratings yet
- Grass Cutting Risk AssessmentDocument4 pagesGrass Cutting Risk AssessmentKaiser Carlo100% (1)
- Cold Cook Methods An Ethnographic ExplorDocument6 pagesCold Cook Methods An Ethnographic ExplorJason100% (1)
- AK Vegan Animals Lifescape 2008 (May) 74-6Document3 pagesAK Vegan Animals Lifescape 2008 (May) 74-6Pepa GarcíaNo ratings yet
- Heat StrokeDocument4 pagesHeat StrokeGerald YasonNo ratings yet
- Atarax Uses, Dosage & Side EffectsDocument5 pagesAtarax Uses, Dosage & Side EffectspatgarettNo ratings yet
- HIIT Academy Total Body Blast Phase 1 PDFDocument33 pagesHIIT Academy Total Body Blast Phase 1 PDFAndre ChinassoNo ratings yet
- Block Learning Guide (BLG) : Block II Hematoimmunology System (HIS)Document6 pagesBlock Learning Guide (BLG) : Block II Hematoimmunology System (HIS)ASTAGINA NAURAHNo ratings yet