Professional Documents
Culture Documents
Urinary System Anatomy and Physiology
Uploaded by
Louie YumulOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Urinary System Anatomy and Physiology
Uploaded by
Louie YumulCopyright:
Available Formats
Urinary System Anatomy and Physiology Part I
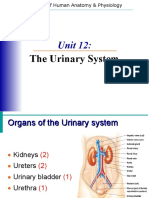
Urinary System Kidneys (2) Most important excretory organ Eliminate waste
Ureters (2) Bladder (1) Urethra (1) Nephron Unit Functional unit of the kidney Formation of urine Tubular and vascular structures
Kidney Location and Protection
Kidneys are located in the posterior wall of the abdominal cavity In the retrope ritoneal space Connective tissue (renal fascia) hold the kidneys in place Adipos e tissue cushion the kidneys The lower rib cage partially enclose the kidney and protect them
Urinary System Anterior/Posterior Views
Kidney Structures
Kidney is reddish-brown Looks like a bean Approximately 4 inches x 2 inches Hilu s indentation where blood vessels and structures enter or exit the kidney Three Regions in the kidney if sliced in half renal cortex, renal medulla, renal pelvi s
Average adult kidney weighs 113-170 g. 10 12 cm long. 6 cm wide. 2.5 cm thick. R ight kidney is lower than the left due to location of liver.
Adrenal gland lies on top of each kidney. Renal parenchyma is divided into two p arts: ~ Cortex ~ Medulla
Renal Cortex Light, outside region Cortex means bark Contains: Nephron
Renal Medulla
Dark, triangular structure Form small cone shaped regions called renal pyramids Each pyramid is separated by renal columns The lower ends of the pyramids point to the renal pelvis
Renal Medulla Contains: Loops of Henle, Vasa Recta and collecting ducts of the juztamedullary nephrons.
Each kidney contains 8 -18 pyramids. Pyramids drain into 4 13 minor calices. 2 3 major calices.
Renal pelvis
A basin that collects the urine made by the kidney and helps form the upper end of the ureter The edges of the renal pelvis closest to the renal pyramids are ca lled calices Calices collect the urine formed in the kidney
Renal pelvis Is the beginning of collecting system and composed structures that are designed to COLLECT and TRANSPORT URINE.
How do they work?
Need a blood supply Brought to the kidney via the renal artery Renal artery stem s from the abdominal aorta 20-25% of cardiac output goes to the kidneys Smaller arteries supply blood to the nephron unit Blood leaves the kidney via the renal veins The renal veins empty into the inferior vena cava
Functions of the Kidneys Excrete nitrogenous waste from the body Urea Ammonia Creatinine
Regulate blood volume Help regulate electrolyte content of the blood Regulate ac id-base balance (pH) Regulate blood pressure Regulates red blood cell production
The Formation of Urine
The Nephron Unit Each kidney contains about 1 million nephron units The number d oes not increase after birth They cannot be replaced if damaged 2 parts Tubular component (renal tubule) Vascular component
Renal Tubules
Glomerular capsule (Bowmans Capsule) C shaped capsule surrounding the glomerulus Gl omerulus cluster of capillaries Proximal convoluted tubule Loop of Henle ascending and descending limb Distal Convoluted tubule Collecting duct
Nephron
Renal Vasculature
Receives blood from the renal artery Renal artery branches into the afferent art erioles (Branches to form glomerulus) Afferent arterioles feed into Bowmans capsu le The efferent arterioles exit Bowmans capsule The efferent arterioles form the peritubular capillaries The peritubular capillaries empty into the venules, larg e veins, and then into the renal veins It is imperative you know the relationshi p between the tubular and vascular structures.
Urine Formation
Formed in the nephron unit Water and dissolved substances move through the renal tubules and vessels Three processes are involved in urine formation Glomerular filtration Tubular reabsorption Tubular secretion
Normal Urine
Clear and pale to deep yellow or amber Slightly aromatic in odor Slightly acidic 5.0 8.0 With a sp. Gravity of 1.010 1.030 (+) NA, K ions, urea uric acid, creat inin, ammonia, and HCO3 ions (-) Glucose, CHON, RBC, and WBC and bile pigments
Composition of Urine
Sterile 95 % water Nitrogen containing waste urea, uric acid, ammonia, creatinin e Electrolytes Light yellow color of urine is due to a pigment called urochrome Urochrome is formed from the breakdown of hemoglobin in the liver
Urine Specific Gravity
Ratio of the amount of solute to the total volume Solute = substance dissolved i n the urine The greater the solute = greater the specific gravity Concentrated U rine = high specific gravity Ex. dehydration Ex. Overhydration, diabetes insipidus
Dilute Urine = low specific gravity
Urine Characteristics
Amount 1500 ml in 24 hours pH average 6.0 Specific Gravity heavier than water (1 .0101.030) Color yellow (amber, straw colored, concentrated, orange, brown, red, sediment, clear or cloudy) Dehydrated = deep yellow, dark Overhydrated = pale y ellow, colorless
Abnormal Constituents of Urine Albumin (protein) Glucose Red blood cells Hemoglobin White blood cells Ketone bo dies Bilirubin
Urine Testing Urinalysis Microscopic exam Culture and sensitivity Urine dipstick Urine Drug an d alcohol screening 24 hour urine testing
Your Plumbing The Urinary Tract (Ureters, Urinary bladder, Urethra) Ureters Transport urine, they do not alter it in any way Urine moves in response to gravity and muscular movements called peristalsis through ureters.
Your Plumbing
The Bladder
Stores urine temporarily until elimination Located behind the symphasis pubis A distended bladder or full bladder can be palpated above the syphasis in the abdo minal cavity. Bladder has 4 layers Mucous membrane Submucosa Detrusor muscle involuntary smooth muscle Serosa
Contain rugae to allow for stretching Trigone triangular area in the floor of th e bladder
Urination Micturition
Expelling urine from the bladder The urge to urinate (void) happened at about 20 0 ml of urine in the bladder At about 300 ml urine in the bladder, the urge beco mes more uncomfortable Moderately full = 500 ml urine Overdistended bladder may have over 1000 ml urine Bacteria in your bladder doubles every 4 hours. Stimulat ed by stretch receptors
Urethra
Carries urine from the bladder to the outside of the body Internal sphincter pre vents urine from emptying; composed of smooth muscle; involuntary External sphin cter at the upper portion of the urethra allows you to resist the urge to urinat e; composed of skeletal muscle; voluntary Female short, opens to the outside at the urethral meatus Male longer, passes through the prostate gland; carries urin e and sperm
Urinary Retention and Suppression Retention - Inability to void Post operative; anesthesia Bladder dysfunction
Suppression no urine formation Kidney dysfunction
Data Collection & Documentation Characteristics of urine Color Sediment Clear or cloudy Odor
How does the patient/resident void? Urinary diversions? Signs and symptoms Urgency Frequency Burning sensation Hesitancy
What is the Costovertebral Angle? T11 R. Kidney T12 L1 L. Kidney 12th Rib Costovertebral Angle Region to assess for kidney tenderness
Disorders of the Urinary System Glomerulonephritis Polycystic Kidney Pyelonephritis Renal Calculi kidney stones Renal Failure UTI urinary tract infection
As We Age
By age 80 there is a 50% reduction in nephron units; therefore a decreased abili ty to concentrate urine Urinary bladder shrinks and becomes less able to contrac t and relax; therefore the elderly must void frequently Bladder infection incide nce increases Increase in bladder incontinence due to weakened muscles
Functions of Genitourinary System Filtration Reabsorption Secretion Excretion Regulation
You might also like
- Urinary System: Anatomy and PhysiologyDocument42 pagesUrinary System: Anatomy and PhysiologyYum C100% (2)
- General Anatomy of Urinary SystemDocument43 pagesGeneral Anatomy of Urinary Systemiqra riazNo ratings yet
- Handouts - Urinary System Sp11 BIO 160Document7 pagesHandouts - Urinary System Sp11 BIO 160Kelly Trainor100% (2)
- General Anatomy of Urinary SystemDocument62 pagesGeneral Anatomy of Urinary SystemSARABIA, ARVIN JR.No ratings yet
- Urinary FinalDocument45 pagesUrinary FinalGwynethNo ratings yet
- Urinary SystemDocument40 pagesUrinary SystemRene T. TalaranNo ratings yet
- Anatomi Blok 17Document34 pagesAnatomi Blok 17Lintang SuroyaNo ratings yet
- Urinary System: Anatomy and Physiology IiiDocument48 pagesUrinary System: Anatomy and Physiology IiiShelby Dawn100% (1)
- Module 25 Handouts Urinary SystemDocument5 pagesModule 25 Handouts Urinary Systemgianarido30No ratings yet
- The Excretory SystemDocument31 pagesThe Excretory Systemapi-3759646100% (12)
- Anatomy of Urinary SystemDocument43 pagesAnatomy of Urinary Systemandrea titus100% (1)
- Genitp Urinary SystemDocument200 pagesGenitp Urinary SystemQuolette ConstanteNo ratings yet
- Urinary SystemDocument27 pagesUrinary Systemtareqhaddad123No ratings yet
- The Urinary SystemDocument19 pagesThe Urinary SystemCecil AlbaNo ratings yet
- Excretion & OsmoregulationDocument35 pagesExcretion & OsmoregulationChetan KuteNo ratings yet
- Urinary SystemDocument2 pagesUrinary SystemCharlayne AnneNo ratings yet
- Human Excretory SystemDocument51 pagesHuman Excretory SystemVinoj MnoNo ratings yet
- Overview of RENAL: Dr. Wilson Arthur Zein, M. BiomedDocument34 pagesOverview of RENAL: Dr. Wilson Arthur Zein, M. BiomedAnnisNo ratings yet
- Urinary SystemDocument8 pagesUrinary SystemanyaNo ratings yet
- The Human Renal SystemDocument8 pagesThe Human Renal SystemRobert CaseyNo ratings yet
- Function of The Urinary SystemDocument7 pagesFunction of The Urinary SystemMary EnsomoNo ratings yet
- Urinary SystemDocument25 pagesUrinary Systembessan alfqeatNo ratings yet
- Urinary System: Nurmila Sari Anatomi FKIK UIN Syarif Hidayatullah JakartaDocument44 pagesUrinary System: Nurmila Sari Anatomi FKIK UIN Syarif Hidayatullah JakartaSeptiara IqraNo ratings yet
- Unit 20 Urinary System NotesDocument45 pagesUnit 20 Urinary System NotesRyann SmithNo ratings yet
- Urinary SystemDocument67 pagesUrinary SystemHanna Soriano100% (1)
- BIOLOGYDocument15 pagesBIOLOGYmanigbasrea15No ratings yet
- Kidneys and ExcretionDocument28 pagesKidneys and ExcretionD-Cristen OrlandoNo ratings yet
- Anatomy and Physiology: Urinary System (Renal System)Document27 pagesAnatomy and Physiology: Urinary System (Renal System)dima_FlaviaNo ratings yet
- Lect-Urinary Syst - 21Document75 pagesLect-Urinary Syst - 21f20231186No ratings yet
- General Urinary SystemDocument41 pagesGeneral Urinary SystemCollin LucasNo ratings yet
- Urinary System 0004Document4 pagesUrinary System 0004Mario Jay CadulioNo ratings yet
- General Anatomy of Urinary SystemDocument41 pagesGeneral Anatomy of Urinary Systemtriana_niman100% (2)
- Xcretory System: BY: Pramod KumarDocument50 pagesXcretory System: BY: Pramod KumarCay C. CordovaNo ratings yet
- Genital Urinary System-Anatomy HX & ExamDocument46 pagesGenital Urinary System-Anatomy HX & ExamMayfield MulelaNo ratings yet
- Bped 65 Urinary SystemDocument26 pagesBped 65 Urinary SystemDollie May Maestre-TejidorNo ratings yet
- Chapter 6Document3 pagesChapter 6John ErickNo ratings yet
- Chap 18 - The Urinary SystemDocument23 pagesChap 18 - The Urinary SystemLora Mae Delos SantosNo ratings yet
- Kidney Anatomy and PhysiologyDocument5 pagesKidney Anatomy and PhysiologyDianne MacaraigNo ratings yet
- KidneysDocument8 pagesKidneysmarlyxsukiNo ratings yet
- MLT 1027 Learning Outcome 14 Renal UrinaryDocument94 pagesMLT 1027 Learning Outcome 14 Renal UrinaryMelanie TranNo ratings yet
- Urinary Organs - MahasiswaDocument43 pagesUrinary Organs - MahasiswaJendral Andi Wijaya KusumaNo ratings yet
- Anatomy and Physiology - Kidney - ForDocument3 pagesAnatomy and Physiology - Kidney - ForKristelle ModalesNo ratings yet
- Urinary SystemDocument31 pagesUrinary Systemrenzvalorant28No ratings yet
- The Urinary SystemDocument78 pagesThe Urinary Systemdesireemassy8No ratings yet
- Urinary System Anatomy and PhysiologyDocument12 pagesUrinary System Anatomy and PhysiologyCris Vincent Suma-oy100% (1)
- THE Urinary System: Charlotte R. Espiritu RN. MANDocument25 pagesTHE Urinary System: Charlotte R. Espiritu RN. MANLenny Ronalyn QuitorianoNo ratings yet
- XQ WFHKLJW WWHAfu 0 DGWFDocument10 pagesXQ WFHKLJW WWHAfu 0 DGWFGiridharan & Balaji RNNo ratings yet
- Urinary SystemDocument18 pagesUrinary Systemwmaximoff426No ratings yet
- Funda SL FinalsDocument3 pagesFunda SL FinalsKarylle Joy ValenciaNo ratings yet
- Location and External Anatomy of The KidneysDocument15 pagesLocation and External Anatomy of The KidneysKyla Malapit GarvidaNo ratings yet
- Retroperitonium: Yosef TadesseDocument94 pagesRetroperitonium: Yosef Tadessetesfaye mekonnenNo ratings yet
- #1 Anatomi Fisiologi Urogenital SystemDocument24 pages#1 Anatomi Fisiologi Urogenital SystemNur azriyati PutriNo ratings yet
- Urinary System: THE KIDNEY and TheDocument40 pagesUrinary System: THE KIDNEY and TheEmNo ratings yet
- Urinary EliminationDocument80 pagesUrinary EliminationMentari WardhaniNo ratings yet
- Urinary System - & Fluid and Acid-Base BalanceDocument74 pagesUrinary System - & Fluid and Acid-Base BalanceReneilwe MoshidiNo ratings yet
- Nephrone and Urine FormationDocument25 pagesNephrone and Urine FormationNurikamal ShaimerdenNo ratings yet
- Urinary SystemDocument77 pagesUrinary SystemJushelle Anne Tigoy PilareNo ratings yet
- Kidney Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandKidney Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- P ADocument10 pagesP AJamie Marianne Maniquis TorresNo ratings yet
- MatterDocument1 pageMatterJamie Marianne Maniquis TorresNo ratings yet
- Communicable Dse.Document4 pagesCommunicable Dse.Jamie Marianne Maniquis TorresNo ratings yet
- Pa Tho Physiology of Pott's DiseaseDocument1 pagePa Tho Physiology of Pott's DiseaseJamie Marianne Maniquis TorresNo ratings yet
- Profhegde PDFDocument130 pagesProfhegde PDFRahul Pagidala100% (1)
- Untitled 1Document5 pagesUntitled 1YuliaAnggrainiNo ratings yet
- Surgery Blue QuestionsDocument25 pagesSurgery Blue QuestionsJamie ElmawiehNo ratings yet
- Chronic Kidney Disease Chronic Kidney Disease: Shinta Mayasari, S.Farm, M.Farm, Klin.,AptDocument11 pagesChronic Kidney Disease Chronic Kidney Disease: Shinta Mayasari, S.Farm, M.Farm, Klin.,Aptnurul hasanahNo ratings yet
- FST (Boys) 2023Document3 pagesFST (Boys) 2023Abdul qadoosNo ratings yet
- Kidney Filtration Lab ReportDocument5 pagesKidney Filtration Lab ReportEiraPocoyoNo ratings yet
- BPSC TEST-8 Answer (English)Document24 pagesBPSC TEST-8 Answer (English)gaurow guptaNo ratings yet
- VIVO - Dialysis Technician: Course DescriptionDocument1 pageVIVO - Dialysis Technician: Course Descriptionpushp00No ratings yet
- Tetada Kalimasad1Document16 pagesTetada Kalimasad1Rasaraj Ramon Castaneda100% (2)
- Hypovolemic Shock Pathophysiology, Symptoms, Signs, Treatment - EHealthStarDocument15 pagesHypovolemic Shock Pathophysiology, Symptoms, Signs, Treatment - EHealthStarKaloy KamaoNo ratings yet
- Life Processes Notes (Yashvi Modi)Document15 pagesLife Processes Notes (Yashvi Modi)YASHVI MODI60% (5)
- Renal Tumors in AdultsDocument23 pagesRenal Tumors in AdultsmadhuNo ratings yet
- Handbook Specialist Training in Nephrology 2021 - Nephrology - Curriculum - vAGM23!7!2021 - ISBNDocument124 pagesHandbook Specialist Training in Nephrology 2021 - Nephrology - Curriculum - vAGM23!7!2021 - ISBNVanroNo ratings yet
- Medical Services - Alphabetical List (A-Z), Best Healthcare, Latest Medical Technology - UCLA Health, Los Angeles, CADocument8 pagesMedical Services - Alphabetical List (A-Z), Best Healthcare, Latest Medical Technology - UCLA Health, Los Angeles, CAsunny siligamNo ratings yet
- Acid-Base BalanceDocument47 pagesAcid-Base BalanceEmmanuel RocksonNo ratings yet
- A. Case Study Thesis-Front Page (Revised)Document10 pagesA. Case Study Thesis-Front Page (Revised)Lopirts NiganiNo ratings yet
- Chapter 25: The Urinary System: Page 19 of 25Document1 pageChapter 25: The Urinary System: Page 19 of 25JAGDEV PANESARNo ratings yet
- 6 - Clinical Biochemistry - 1001411Document14 pages6 - Clinical Biochemistry - 1001411bsmallahNo ratings yet
- Case Study On End Stage Renal FailureDocument19 pagesCase Study On End Stage Renal Failurelenecarglbn100% (1)
- Renin-Angiotensin-Aldosterone System (RAAS) : Hyponatremia or Increased Sympathetic ToneDocument2 pagesRenin-Angiotensin-Aldosterone System (RAAS) : Hyponatremia or Increased Sympathetic ToneDrbee10No ratings yet
- The Urinary System PPT EdDocument30 pagesThe Urinary System PPT EdGirmay GebrehiwotNo ratings yet
- Dialysis Report - NURS 302Document3 pagesDialysis Report - NURS 302AmalNo ratings yet
- Urinalysis InterpretationDocument9 pagesUrinalysis InterpretationNicku MalanceaNo ratings yet
- 0610 - s08 - QP - 3 IGCSE Biology 2008 Paper by Hubbak KhanDocument33 pages0610 - s08 - QP - 3 IGCSE Biology 2008 Paper by Hubbak KhanHubbak Khan100% (18)
- Sample Lesson PlanDocument2 pagesSample Lesson PlanAfzan ZawawiNo ratings yet
- Practical Necropsy GuideDocument52 pagesPractical Necropsy GuideDulNo ratings yet
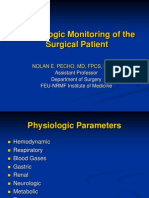
- Physiologic Monitoring of The Surgical PatientDocument56 pagesPhysiologic Monitoring of The Surgical PatientSeid Adem100% (2)
- Giving Direction in and Around Hospital MATERIAL-1Document5 pagesGiving Direction in and Around Hospital MATERIAL-1RahmatunnisaNo ratings yet
- Unit VII Lecture NotesDocument3 pagesUnit VII Lecture NotesSteve Sullivan100% (1)
- Integrated Therapeutics-Ii For 3 Year STS: Chapter-1Document69 pagesIntegrated Therapeutics-Ii For 3 Year STS: Chapter-1Geleta GalataaNo ratings yet