Professional Documents
Culture Documents
Pervasive Developmental Disorders (PDD) : About The Disorder
Uploaded by
chubbymale33326Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pervasive Developmental Disorders (PDD) : About The Disorder
Uploaded by
chubbymale33326Copyright:
Available Formats
Pervasive Developmental Disorders (PDD)
About the Disorder
*For children younger than 24 months, Multi-System Development Disorder (MSDD) is preferred. For more on MSDD, see box on the back of this fact sheet.
Early Childhood Mental Health Fact Sheet
clumsy. They may also have an aversion to affection and/or physical contactduring infancy this may mean the child seems uncomfortable when being cuddled. As the child matures and begins to play with toys, they may tend to relate to the inanimate environment better than they relate to people. For example, a child with autism may be clearly enamored with a certain toy, but will not likely rush to share the special toy with their primary caregiver. The child may also seem to have little understanding of the needs of others and may even seem not to notice another persons distress. It is these behaviors that lead to difficulty in developing friendships and problems with social skills. It may seem that young children with PDD have little or no interest in establishing friendships. They may even seem as though they have not formed a secure bond or attachment to a particular caregiver. As children with a PDD diagnosis get older, they often desire friendships and express sadness or depression as they gain understanding of being different. Early intervention, therefore, is especially important because it can help them to develop necessary and useful social skills, communication skills, and cognitive skills. With intense behavioral intervention, some preschoolers with autism have achieved higher IQ scores, more expressive speech, and a reduction in behavior problems.
Pervasive developmental disorders (PDD) include autistic disorder, Retts disorder, childhood disintegrative disorder, Aspergers syndrome, and PDD-NOS (not otherwise specified). For children with autism, the disorder will progress continually; children with other disorders in this category may develop normally and then experience a regression. For all disorders of this type, however, the onset will occur in early childhood, and except for Retts Disorder, which has been seen only in females, the rates of occurrence are higher in males than in females. This category of disorders involves a delay in a childs development of basic social, communicative, and learning skills. Children with this diagnosis may have impairments in the use of several nonverbal behaviors such as eye contact, facial expressions, body posture, as well as other gestures used in social interactions and to communicate. Because every child is unique and PDD covers a wide spectrum of symptoms and behaviors, no two children with this diagnosis will behave the same. In general, however, children with a PDD diagnosis have difficulty establishing social relationships, resist change, and need consistent structure and routine.
What You May See
In children for whom the onset of the disorder occurs during infancy, parents and caregivers may notice a lack of socially directed smiles and that the child does not respond to their caregivers voice. This sometimes leads caregivers to be concerned that their child may be deaf. Infants may also exhibit sensory sensitivities, avoid direct eye contact, be inflexible with regard to routines, and/or they may seem
What You May See At a Glance
The spectrum of PDD is broadsome of these characteristics may be more indicative of autism than Aspergers.
When Infancy What May exhibit sensory sensitivities, avoid direct eye contact, be inflexible with regard to routines, and/or may seem clumsy; may reject cuddling. When Toddler What As a child with PDD matures, the initial indications may become more pronounced. Beyond avoiding eye contact, they will avoid direct interactions; language problems may become more apparent or a regression in language development may occur; inflexibility with regard to routine will be more fixed; difficulties in processing visual, auditory, and tactile sensations may appear; and problems with vestibular (sense of balance and equilibrium) and proprioceptive (sense of ones body in space) sensations may occur. When Preschooler What Children at this age may not engage in socially imitative play or they may engage in limited types of play; they may also begin to have more pronounced difficulties with peer relationships.
IMPORTANT
This fact sheet is not intended to be used as a diagnostic tool. It is meant to be used only as a reference for your own understanding and to provide information about the different kinds of behaviors and mental health issues you may encounter.
While it is important to respect a childs need for confidentiality, if you work with children or families, you are legally required to report suspected child abuse or neglect. For more information, consult Reporting Child Abuse and Neglect: A Resource Guide for Mandated Reporters, available from the Minnesota Department of Human Services.
Minnesota Association for Childrens Mental Health MACMH
165 Western Avenue N, Suite 2, St. Paul, MN 55102 800-528-4511 651-644-7333 www.macmh.org
Pervasive Developmental Disorders (PDD)
(continued) Symptoms and Behaviors
Inflexible adherence to routines or rituals Avoidance of eye contact Impairment in non-verbal communication Abnormally intense focus or interest in a specific area (for example, may be intensely focused on vehicle wheels or may insist that every toy is a guitar) Language problems may be apparentthe child may rarely speak, may be unable to initiate or sustain a conversation, or may repeat phrases over and over Lack of varied play Lack of social imitative play typical of developmental level (for example, will not have tea parties or play store) May lack sensitivity to or be highly sensitive to sounds, lights, smells, touch, and/or the taste and texture of foods Teach basic skills such as responding to their name, sitting with a group, and following directions. Teach social skills like taking turns and looking at the person you are talking to; if eye contact is too intense, teach the child to look at a persons forehead or nose instead. Structure playtime to help the child interact with peers (for example, assign peer buddies or establish cooperative groups to ensure inclusion). Find a creative way to show affectionalthough some children with PDD do not like to be touched, some do enjoy firm hugs. Ask the childs primary caregiver if there are any strategies (such as language games the child plays at speech therapy) that could be incorporated into the childs play.
Documenting Your Concerns and Next Steps
When documenting behavior, avoid generalizations such as Katie appears to have autistic tendencies or difficulty communicating. Instead, record specific behavior, for example, This afternoon we did not go outside because it was rainingKatie threw the blocks and laid on the floor crying for 30 minutes and no amount of redirecting or consoling seemed to help. I think I am beginning to see a pattern with Katie; she has exhibited similar difficulty with changes in the schedule at other times as well. If a childs behaviors are causing concern, you may want to suggest to the parents that they take their child to their primary care provider who may refer the parents to a mental health professional, an early childhood behavior specialist, or a developmental pediatrician. When discussing your concerns, focus on the childs behaviors and avoid drawing conclusions about whether the behaviors are indicative of a mental health problem. For more information about early childhood mental health, see MACMHs A Guide to Early Childhood Mental Health, available for order at www.macmh.org.
Strategies
Provide a highly structured environment. Use graphic or visual schedules. Prepare the child for changes and transitions.
Multi-System Developmental Disorder (MSDD)
For children younger than 24 months, Developmental Disorder (MSDD) is preferred. Multi-System
A child with MSDD does not totally lack the ability to develop a social/emotional relationship with a primary caregiver but will have impairment in developing this relationship. The child may avoid contact with caregivers, but will give slight cues that show attachment. These children have difficulty forming, maintaining, and/or developing communication, including preverbal gestures. For many toddlers with MSDD, language does not serve a communicative intent. They may memorize parts of songs or dialogue but they do not use speech to communicate. A child with MSDD may have major difficulty processing visual, auditory, tactile, proprioceptive (spatial awareness of ones body), and vestibular sensations. Most have poor motor planningthey lack the ability to sequence their movements to create a desired outcomeand may appear very clumsy when learning a new skill. Infants and toddlers diagnosed with MSDD also show impairments in processing sensations. For example, they may be extremely sensitive to touch (startling or even having a tantrum when touched lightly), or they may show great pleasure in heavy pressure (being sat on or wedging themselves in small spaces behind furniture). Early interventions can be very successful in helping a child with MSDD develop processing tools and coping strategies. An assessment and intervention plan that utilizes a speech therapist, occupational therapist, family psychologist, and other professionals as necessary is crucial.
Ready Resources
Autism Society of America at www.autism-society.org Kami M. Talley Reading and Resource Center at the University of Minnesota offers a bibliography of resources at http://education.umn.edu/ChildCareCenter/Kamihealing throughbooks/ National Institute of Mental Health at www.nimh.nih.gov SAMHSAs National Mental Health Information Center at www.mentalhealth.samhsa.gov ZERO TO THREE at www.zerotothree.org
Information included in this fact sheet comes from the DSM-IV-TR (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision) and DC:03R (Diagnostic Classification of Mental Health and Development Disorders of Infancy and Early Childhood: Revised Edition). Funding for the development and publication of this fact sheet was sponsored in part by a grant from the Minnesota Department of Education using federal dollars from CFDA 84.323A, Special Education - Program Improvement Grants.
You might also like
- 21 Insights to Support and Connect with Your Autistic ChildFrom Everand21 Insights to Support and Connect with Your Autistic ChildNo ratings yet
- Boundless Love: Embracing The Energy And Challenges Of Special ChildrenFrom EverandBoundless Love: Embracing The Energy And Challenges Of Special ChildrenNo ratings yet
- The ADHD Parenting Guide for the Boy Child: Thriving Minds, Unleashing Potential: Nurturing Boys with ADHD - A Practical Parenting GuideFrom EverandThe ADHD Parenting Guide for the Boy Child: Thriving Minds, Unleashing Potential: Nurturing Boys with ADHD - A Practical Parenting GuideNo ratings yet
- Overcoming Challenges of Autism in Kids: 7 Effective Strategies Autism Parents Can Leverage for Successfully Raising an Autistic Kid: The Master Parenting Series, #14From EverandOvercoming Challenges of Autism in Kids: 7 Effective Strategies Autism Parents Can Leverage for Successfully Raising an Autistic Kid: The Master Parenting Series, #14No ratings yet
- Presentation 1Document17 pagesPresentation 1api-547492718No ratings yet
- Autism Spectrum Disorders: A Booklet For Parents and CarersDocument40 pagesAutism Spectrum Disorders: A Booklet For Parents and CarersAndreea SanduNo ratings yet
- Parent’s Guide to Overcoming Autism Spectrum Disorder in ChildrenFrom EverandParent’s Guide to Overcoming Autism Spectrum Disorder in ChildrenNo ratings yet
- Nice Guidelines On Asd Signs and SymptomsDocument5 pagesNice Guidelines On Asd Signs and SymptomsHoney ReyesNo ratings yet
- Autism Spectrum Disorder: Group 1Document26 pagesAutism Spectrum Disorder: Group 1LAARNI MARIE G. CARIÑONo ratings yet
- Meeting Special Needs: A practical guide to support children with DyspraxiaFrom EverandMeeting Special Needs: A practical guide to support children with DyspraxiaNo ratings yet
- The Effect ADHD Has On Marriage: Fostering A Strong RelationshipFrom EverandThe Effect ADHD Has On Marriage: Fostering A Strong RelationshipRating: 2 out of 5 stars2/5 (2)
- Sensation Me Crazy: A Guide, Tools, and Fun Games to Assist and Help Develop Your Child With Sensory Processing Disorder (SPD)From EverandSensation Me Crazy: A Guide, Tools, and Fun Games to Assist and Help Develop Your Child With Sensory Processing Disorder (SPD)No ratings yet
- Raising Kids With Disabilities: Understanding Differences in Autism, Asperger's, ADHD and How Parents Can Help Children With Disabilities Overcome Challenges to Live a Happier and More Fulfilling Life: The Master Parenting Series, #15From EverandRaising Kids With Disabilities: Understanding Differences in Autism, Asperger's, ADHD and How Parents Can Help Children With Disabilities Overcome Challenges to Live a Happier and More Fulfilling Life: The Master Parenting Series, #15No ratings yet
- STEP Autism ToolkitDocument29 pagesSTEP Autism ToolkitMiha PopaNo ratings yet
- Rupal Arora - ASDDocument23 pagesRupal Arora - ASDrupal aroraNo ratings yet
- 312-Ops Asd Autism Parents Q and A BookletDocument16 pages312-Ops Asd Autism Parents Q and A Bookletapi-233394844No ratings yet
- Childhood Psychological DisordersDocument7 pagesChildhood Psychological DisordersineedthisforaschoolprojectNo ratings yet
- Autism (Asd)Document28 pagesAutism (Asd)Mona SabharwalNo ratings yet
- ADHD Guide Attention Deficit Disorder: Coping with Mental Disorder such as ADHD in Children and Adults, Promoting Adhd Parenting: Helping with Hyperactivity and Cognitive Behavioral Therapy (CBT): Helping with Hyperactivity and Cognitive Behavioral Therapy (CBT)From EverandADHD Guide Attention Deficit Disorder: Coping with Mental Disorder such as ADHD in Children and Adults, Promoting Adhd Parenting: Helping with Hyperactivity and Cognitive Behavioral Therapy (CBT): Helping with Hyperactivity and Cognitive Behavioral Therapy (CBT)Rating: 2 out of 5 stars2/5 (2)
- Common Mental Health DiagnosisDocument19 pagesCommon Mental Health Diagnosisapi-400016232No ratings yet
- Understanding Autism Spectrum Disorders (Asds) :: An IntroductionDocument4 pagesUnderstanding Autism Spectrum Disorders (Asds) :: An IntroductioneviherdiantiNo ratings yet
- Neurodiversity and Co-Occurring DifferencesDocument4 pagesNeurodiversity and Co-Occurring DifferencesNosparesNo ratings yet
- Behaviour Problems in Children and HomoeopathyDocument6 pagesBehaviour Problems in Children and HomoeopathyHomoeopathic Pulse100% (1)
- Attention Deficit Hyperactivity DisorderDocument11 pagesAttention Deficit Hyperactivity DisorderJosef PérezNo ratings yet
- Early Intervention of Autism: A Case For Floor Time ApproachDocument28 pagesEarly Intervention of Autism: A Case For Floor Time ApproachpsicosmosNo ratings yet
- Autism Treatment Tips: The Complete Guide to Taking Care of an Autistic Child (Autism Spectrum Disorder, Autism Symptoms, Autism Signs)From EverandAutism Treatment Tips: The Complete Guide to Taking Care of an Autistic Child (Autism Spectrum Disorder, Autism Symptoms, Autism Signs)Rating: 4 out of 5 stars4/5 (1)
- Text 01 What Is Autism Spectrum Disorder?: GenesDocument3 pagesText 01 What Is Autism Spectrum Disorder?: GenestayebNo ratings yet
- Autism Spectrum DisorderDocument32 pagesAutism Spectrum DisorderBastinNo ratings yet
- All About Autistic Spectrum DisordersDocument36 pagesAll About Autistic Spectrum DisordersFrank SmetsNo ratings yet
- ADHD Not Just Naughty: One mum's roadmap through the early challenges of ADHDFrom EverandADHD Not Just Naughty: One mum's roadmap through the early challenges of ADHDNo ratings yet
- Unit-4 CHILDHOOD MENTAL DISORDERSDocument22 pagesUnit-4 CHILDHOOD MENTAL DISORDERSNeha JainNo ratings yet
- The Parent?s Autism Sourcebook: A Comprehensive Guide to Screenings, Treatments, Services, and OrganizationsFrom EverandThe Parent?s Autism Sourcebook: A Comprehensive Guide to Screenings, Treatments, Services, and OrganizationsNo ratings yet
- Week 11 Ncm 109 Lecture PptxDocument49 pagesWeek 11 Ncm 109 Lecture PptxPolicarpio AprilNo ratings yet
- Child Autism BehaviorsDocument4 pagesChild Autism BehaviorsFlora PapastfNo ratings yet
- OPPOSITIONAL DEFIANT DISORDER: A Cutting-Edge Method for Recognizing and Guiding Your O.D.D Child Towards Success (2022 Guide for Beginners)From EverandOPPOSITIONAL DEFIANT DISORDER: A Cutting-Edge Method for Recognizing and Guiding Your O.D.D Child Towards Success (2022 Guide for Beginners)No ratings yet
- High-Functioning Autism Spectrum Disorder: Parent's Guide to Creating Routines, Diagnosis, Managing Sensory and Autism Awareness in Kids.From EverandHigh-Functioning Autism Spectrum Disorder: Parent's Guide to Creating Routines, Diagnosis, Managing Sensory and Autism Awareness in Kids.Rating: 5 out of 5 stars5/5 (1)
- Psy 411Document8 pagesPsy 411danoshkenNo ratings yet
- ADHD Raising an Explosive Child: Guidebook for Parents to Help Children Self-Regulate, Build Social Skills, Focus, Organise and Gain ConfidenceFrom EverandADHD Raising an Explosive Child: Guidebook for Parents to Help Children Self-Regulate, Build Social Skills, Focus, Organise and Gain ConfidenceNo ratings yet
- Understanding Autism Spectrum Disorder in Children and TeensDocument6 pagesUnderstanding Autism Spectrum Disorder in Children and TeenstayebNo ratings yet
- A Guide On ADHD Using Neural ConnectionsDocument13 pagesA Guide On ADHD Using Neural ConnectionsNehad BalochNo ratings yet
- The START of a JOURNEY: Understanding Autism Spectrum DisorderDocument28 pagesThe START of a JOURNEY: Understanding Autism Spectrum DisorderAnanya MishraNo ratings yet
- Autism Tips and Facts Sheet (Use This One)Document4 pagesAutism Tips and Facts Sheet (Use This One)api-284135781No ratings yet
- Autism Spectrum Disorder: Sensory IssuesDocument4 pagesAutism Spectrum Disorder: Sensory IssuesLove Aiza EscapalaoNo ratings yet
- ADHD Parenting Guide for Boys: Step-by-Step Strategies, Behavior Management, and Tools for Emotional Support, Academic Success, and Social Skills Development in Boys with ADHDFrom EverandADHD Parenting Guide for Boys: Step-by-Step Strategies, Behavior Management, and Tools for Emotional Support, Academic Success, and Social Skills Development in Boys with ADHDNo ratings yet
- Mentally Challenged ChildrenDocument4 pagesMentally Challenged ChildrenSanthosh.S.UNo ratings yet
- SENSORY PROCESSING DISORDER: Understanding, Managing, and Thriving with Sensory Processing Challenges (2024 Beginner Guide)From EverandSENSORY PROCESSING DISORDER: Understanding, Managing, and Thriving with Sensory Processing Challenges (2024 Beginner Guide)No ratings yet
- Reflective EssayDocument7 pagesReflective EssayJEA MARIE MENDOZANo ratings yet
- 06 Strategies To Help Children With AutismDocument4 pages06 Strategies To Help Children With Autismbeniki100% (1)
- 7 Vital Parenting Skills for Teaching Kids With ADHD: Proven ADHD Tips for Dealing With Attention Deficit Disorder and Hyperactive Kids: Secrets To Being A Good Parent And Good Parenting Skills That Every Parent Needs To Learn, #3From Everand7 Vital Parenting Skills for Teaching Kids With ADHD: Proven ADHD Tips for Dealing With Attention Deficit Disorder and Hyperactive Kids: Secrets To Being A Good Parent And Good Parenting Skills That Every Parent Needs To Learn, #3No ratings yet
- The Asperger's Syndrome Bible: Autism Spectrum Disorders & Managing relationships, social skills, therapy & parenting of aspergers from the inside out,for children, teens,boys and girls to adulthoodFrom EverandThe Asperger's Syndrome Bible: Autism Spectrum Disorders & Managing relationships, social skills, therapy & parenting of aspergers from the inside out,for children, teens,boys and girls to adulthoodNo ratings yet
- Behaviour Problems in Children and AdolescentsDocument4 pagesBehaviour Problems in Children and AdolescentsGillian WassmansdorfNo ratings yet
- ReportDocument6 pagesReportGab GonzalesNo ratings yet
- Parenting Children With Oppositional Defiant Disorder: Understand Your Child’s Behavior, Help Them Feel Better Emotionally, and Watch Them Grow Into a Cheerful AdultFrom EverandParenting Children With Oppositional Defiant Disorder: Understand Your Child’s Behavior, Help Them Feel Better Emotionally, and Watch Them Grow Into a Cheerful AdultNo ratings yet
- Unlocking The Spectrum: Navigating The Complexity Of Autism With Advanced Strategies And InsightsFrom EverandUnlocking The Spectrum: Navigating The Complexity Of Autism With Advanced Strategies And InsightsNo ratings yet
- How To Relieve Stress in WeldingDocument17 pagesHow To Relieve Stress in Weldingchubbymale33326No ratings yet
- How To Relieve Stress in WeldingDocument17 pagesHow To Relieve Stress in Weldingchubbymale33326No ratings yet
- How To Relieve Stress in WeldingDocument17 pagesHow To Relieve Stress in Weldingchubbymale33326No ratings yet
- CastirDocument2 pagesCastirchubbymale33326No ratings yet
- Distribución Preguntas API 1104 PDFDocument2 pagesDistribución Preguntas API 1104 PDFLora BoydNo ratings yet
- Home Science D 1204: Test Booklet No. Time: 1 Hours) (Maximum Marks: 100 Instructions For The CandidatesDocument24 pagesHome Science D 1204: Test Booklet No. Time: 1 Hours) (Maximum Marks: 100 Instructions For The CandidateskhanjkNo ratings yet
- Omnishelter - Shelter, Cabinets, Production & Installation - ADocument2 pagesOmnishelter - Shelter, Cabinets, Production & Installation - Achubbymale33326No ratings yet
- Artificial Intelligence PlanDocument1 pageArtificial Intelligence PlanAhmed Osama Al-SawahNo ratings yet
- Week 2 EIM 12 Q1 Indoyon Evaluated ESDocument8 pagesWeek 2 EIM 12 Q1 Indoyon Evaluated ESMarino L. SanoyNo ratings yet
- The Actor in You Teacher's GuideDocument9 pagesThe Actor in You Teacher's GuideIonut IvanovNo ratings yet
- Patient-Centered Care TrainingDocument10 pagesPatient-Centered Care Trainingradomir.boskovicNo ratings yet
- FAMILY TIES Lesson 2 ReadingDocument2 pagesFAMILY TIES Lesson 2 ReadingAtikah AmaranNo ratings yet
- Miss Jenelle M. de Vera: English TeacherDocument38 pagesMiss Jenelle M. de Vera: English Teacherromar brionesNo ratings yet
- Teacher Evaluation in NsuDocument23 pagesTeacher Evaluation in Nsumd shakilNo ratings yet
- W. Sellars - 'Science, Sense Impressions, and Sensa' (A Reply To Cornman)Document58 pagesW. Sellars - 'Science, Sense Impressions, and Sensa' (A Reply To Cornman)ahnp1986No ratings yet
- Semantics exam questions and answersDocument4 pagesSemantics exam questions and answersThiên Huy100% (1)
- Chapter 8 - Learning To Communicate ProfessionallyDocument4 pagesChapter 8 - Learning To Communicate ProfessionallyKTNo ratings yet
- First Grade Lesson Plan Counting by Ones and TensDocument2 pagesFirst Grade Lesson Plan Counting by Ones and TenskimNo ratings yet
- Kent State University Master of Library and Information Science Project Learning OutcomesDocument6 pagesKent State University Master of Library and Information Science Project Learning Outcomesapi-436675561No ratings yet
- Exercises: Functions of LanguageDocument34 pagesExercises: Functions of LanguageЯна ЯрохаNo ratings yet
- Papers Framework of Question Tag.Document15 pagesPapers Framework of Question Tag.YoonaNo ratings yet
- The Brown Bauhaus STUDIO ARCHITECTURE: Fundamental Course - Comprehensive Ale Review + Preparation ProgramDocument10 pagesThe Brown Bauhaus STUDIO ARCHITECTURE: Fundamental Course - Comprehensive Ale Review + Preparation ProgramClaro III TabuzoNo ratings yet
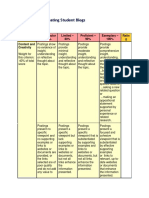
- A Rubric For Evaluating Student BlogsDocument5 pagesA Rubric For Evaluating Student Blogsmichelle garbinNo ratings yet
- GS PricelistDocument2 pagesGS PricelistKimberly OlaveNo ratings yet
- 1-Didactics vs. Pedagogy - Part 1Document14 pages1-Didactics vs. Pedagogy - Part 1ghadaNo ratings yet
- Edtpa Lesson 3Document4 pagesEdtpa Lesson 3api-511022719No ratings yet
- Socrates: Socratic Method and Entrepreneurial LearningDocument7 pagesSocrates: Socratic Method and Entrepreneurial Learningyuta nakamotoNo ratings yet
- Legal Research Process and StrategyDocument2 pagesLegal Research Process and StrategyAr-jay RomeroNo ratings yet
- Dissociative Identity DisorderDocument23 pagesDissociative Identity DisorderSania Khan0% (1)
- Equivalence in Translation TheoryDocument30 pagesEquivalence in Translation TheoryOksana KrychkivskaNo ratings yet
- American Sign Language Recognition Using Machine Learning and ComDocument57 pagesAmerican Sign Language Recognition Using Machine Learning and ComGurudev YankanchiNo ratings yet
- Basketball DribblingDocument3 pagesBasketball Dribblingapi-296964826No ratings yet
- Theoretical Model, Conceptual Model and QuestionnaireDocument7 pagesTheoretical Model, Conceptual Model and QuestionnaireRicardo Tablada0% (1)
- Post Lesson ReflectionDocument8 pagesPost Lesson Reflectionapi-430394514No ratings yet
- Solution of CASE STUDYDocument7 pagesSolution of CASE STUDYdamso recshNo ratings yet
- ACFrOgDbUDwBpyzaf-WscNRYnhXW02neLVMxDFiMXFlM1zH7egiz3BSqIhWJrwfXNkwl2TGeDj8zC 4mAtHzCj TA1otV1Wix0KiY n30tAJijbqE8g6 El4HTuUjvRIvWZOTf0RqmxUuVUErAmpDocument2 pagesACFrOgDbUDwBpyzaf-WscNRYnhXW02neLVMxDFiMXFlM1zH7egiz3BSqIhWJrwfXNkwl2TGeDj8zC 4mAtHzCj TA1otV1Wix0KiY n30tAJijbqE8g6 El4HTuUjvRIvWZOTf0RqmxUuVUErAmpEunice ArutaNo ratings yet
- Reading and Writing StrategiesDocument76 pagesReading and Writing StrategiesGerrylyn BalanagNo ratings yet