Professional Documents
Culture Documents
Hematopoiesis
Uploaded by
Cassandra Grace Labial PaynterOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hematopoiesis
Uploaded by
Cassandra Grace Labial PaynterCopyright:
Available Formats
Hematopoiesis: The production of all types of blood cells generated by a remarkable self-regulated system that is responsive to the demands
put upon it. The levels of the different types of the white blood cells in the granulocyte series (the neutrophils, eosinophils, and basophils) are normally maintained within preset normal ranges and prompt adjustments are made in response to demands such as infections, allergic reactions, etc. In much the same way, the levels of the other types of white cells (the monocytes and lymphocytes), the platelet, and red blood cell are regulated within normal ranges and respond rapidly to demands. The monocytes respond to infections, the lymphocytes respond to immune challenges, the platelets respond to hemorrhage or inflammation, and the red blood cells (erythrocytes) respond to hypoxia (low oxygen levels). When hematopoiesis is disturbed, the first cells to drop are usually the neutrophils (which have a life span in the blood of only 6 to 8 hours) followed by platelets (with a 10day life span). Anemia develops more slowly, over a much longer span of time (since the red blood cells have a 120-day lifespan). All types of blood cells are derived from primitive cells (stem cells) in the bone marrow. The production of blood cells is largely controlled by feedback. When the demand for production of cells of a particular type of cells increases or the levels of the cells fall in blood, stimulatory substances called cytokines are released. And the cytokines stimulate the stem cells to generate new mature blood cells. This occurs in the few days required for blood cell maturation. The production of lymphocytes is an exception to this neat scenario. Many more lymphocytes are generated daily than are needed in the blood. Most lymphocytes are destroyed during development. Thus, lymphopoiesis (the production of lymphocytes) is inefficient compared to all other hematopoiesis RBCs (Red Blood Cells)
The primary function of the red blood cells, or erythrocytes, is to carry oxygen from the lungs to body tissues and to transfer carbon dioxide from the tissues to the lungs. Oxygen transfer is accomplished via the hemoglobin contained in red blood cells. Hemoglobin combines readily with oxygen and carbon dioxide. Hemoglobin gives arterial blood its bright red color; because venous blood has a low oxygen content, it appears dark red. To enable the maximum amount of hemoglobin to be used, red cells are shaped like biconcave disks. This shape provides more surface area for the hemoglobin to combine with oxygen. Red blood cells are also able to change shape to permit passage through small capillaries that connect arteries with veins. The RBC is a count of the number of red blood cells per cubic millimeter of blood. In response to hypoxia, the hormone erthyropoietin, secreted by the kidneys, stimulates the bone marrow to produce red blood cells. The formation of red blood cells is known as erthyropoiesis. Normal red blood cell values at various ages are: Adults: (males): 4.6 - 5.9 million (Females): 4.2-5.4 million Pregnancy: slightly lower than normal adult values Newborns: 5.5 - 6 million Children: 4.6 - 4.8 million
Increase in Red Blood Cells An increase in red blood cell mass is known as polycythemia. Normal physiological increases in the RBC count occur at high altitudes or after strenuous physical training. At high altitudes, less atmospheric weight pushes air into the lungs, causing a decrease in the partial pressure of oxygen and hypoxia. With strenuous physical training, increased muscle mass demands more oxygen. The drugs gentamicin and methyldopa have been associated with increasing the number of red blood cells. Smokers also have a higher number of red blood cells than non-smokers. There are also pathological reasons for an increased number of red blood cells. Polycythemia vera is a disease of unknown origin that results in an abnormal increase in red blood cells. Polycythemia vera is referred to as a "primary polycythemia" because the overproduction of red blood cells does not result from hypoxia. The term "vera" means true; thus polycythemia vera refers specifically to overproduction of red blood cells in the bone marrow not caused by a physiologic need. Polycythemia vera is treated by radioactive phosphorus to slow down bone marrow overproduction of red blood cells. Patients with abnormally high red blood cell counts should have fluids withheld with caution, as a very high RBC mass may cause intravascular clotting. Examples of "secondary polycythemias," that occur in response to hypoxia, are chronic lung disease in adults and children with congenital heart defects characterized by cyanosis. Decrease in Red Blood Cells A lower than normal RBC can result from a number of causes, including: Massive RBC loss, such as acute hemorrhage Abnormal destruction of red blood cells Lack of substances needed for RBC production Bone marrow suppression The term "anemia" is a general term that refers to a decrease in red blood cells. Anemia can occur from either a decrease in the number of red blood cells, a decrease in the hemoglobin content, or both. Red blood cells live for approximately four months in the bloodstream. A reticulocyte count measures the numbers of reticulocytes, immature forms of erythrocytes, circulating in the bloodstream. Normal ranges for reticulocytes are 0.5% to 1.5% of the total numbers of red blood cells in men and 0.5% to 2.5% in women. A low reticulocyte count is seen with cirrhosis, folic acid deficiency, and bone marrow failure. A high reticulocyte count indicates that the bone marrow is responding to the need for increased red blood cell production. A person who has recently donated whole blood or who is responding to treatment for anemia would be expected to have a high reticulocyte count. Hematocrit The hematocrit, also known as the "Hct", "crit" or PVC (packed cell volume) determines the percentage of red blood cells in the plasma. The term hematocrit means "to separate blood." When the patient's blood sample is spun in a centrifuge, the white blood cells and platelets rise to the top in what is known as the "buffy coat." The heavier red blood cells sink to the bottom, where they can be calculated as a percentage of the total blood sample. Normal Hematocrit Values
Adults: (males): 45-52%, (females): 37-48% Pregnancy: decreased hematocrit, especially in the last trimester as plasma volume increases Newborn: up to 60% Children: varies with age If the RBC and the hemoglobin are both normal, it is possible to estimate the hematocrit as being approximately three times the hemoglobin. For example, a person whose hematocrit is 30% would have a hemoglobin of approximately 10 gm. Hemoglobin Hemoglobin is comprised of an iron containing pigment (heme) and a protein (globulin). Each gram of hemoglobin can carry 1.34 ml of oxygen. The oxygen-combining ability of the blood is in direct proportion to the hemoglobin concentration, rather than the numbers of red blood cells, because some cells contain more hemoglobin than others. Hemoglobin also serves as an important pH buffer in the extracellular fluid. Hemoglobin determination is used to screen for anemia, to identify the severity of anemia, and to assist in evaluating the patient's response to anemia therapy. Normal Hemoglobin Values Adult: (males): 13 - 18 gm (Females): 12 - 16 gm Pregnancy: 11 - 12 gm Newborn: 17 - 19 gm. 77% of this value is fetal hemoglobin, which drops to approximately 23% of the total at 4 months of age Children: 14-17 gm Decreased Hemoglobin Because hemoglobin is a component of all red blood cells, the conditions that cause a low RBC, such as blood loss and bone marrow suppression, also produce a low hemoglobin level. Hemoglobin levels are lowered in patients who have abnormal types of hemoglobin or hemoglobinopathies. Normal hemoglobin in adults is almost all adult hemoglobin, with a very small percentage of fetal hemoglobin (hgbF). Red blood cells with abnormal types of hemoglobin are often fragile and damaged or destroyed easily in the vascular system. Hemoglobin electrophoresis can distinguish among specific types of abnormal hemoglobin. In thalassemia major, the person has a high amount of fetal hemoglobin and abnormalities in hemoglobin synthesis. In sickle cell anemia, the patient has an abnormal type of hemoglobin known as sickle hemoglobin (hgbS). Some patients have a normal RBC count but a low hemoglobin level. This situation occurs with iron-deficiency anemia, in which red blood cells have less hemoglobin than normal. Iron deficiency anemia is also referred to as hypochromic anemia. Hypochromic is a term that means "less than normal color." In general, women need more iron in their diets than men, due to the regular loss of iron in the menstrual flow. During pregnancy a woman's need for iron to build more hemoglobin increases. If a woman becomes pregnant when she has low iron reserves, she is at risk of becoming severely anemic. Regular hemoglobin testing is an important part of prenatal care. During the last trimester of pregnancy, a condition known as "physiological anemia of pregnancy" occurs. This normal drop in hemoglobin values results from an increase in the plasma volume. Multiple blood draws in premature infants is a common cause of anemia. Red blood cells that have abnormal hemoglobin are damaged or destroyed more easily than cells with normal hemoglobin.
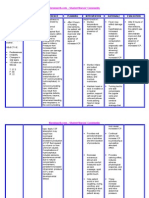
Critical Low and High Values of Hemoglobin A hemoglobin value under 5 gm may cause heart failure. A hemoglobin value over 20 gm may cause clogging of capillaries due to hemoconcentration. Increased levels of hemoglobin are found in any condition in which the number of circulating red blood cells rises above normal. Examples of conditions associated with increases in hemoglobin are polycythemia vera, severe burns, chronic obstructive pulmonary disease, and congestive heart failure. When a patient has a lower than normal hemoglobin, it is important to determine whether red blood cells are of normal size and if they have a normal concentration of hemoglobin. These measurements, known as erythrocyte or red blood cell indices, provide important information about various types of anemias. Red Cell Size, Red Cell Hemoglobin and Hemoglobin Concentration Mean corpuscular volume (MCV) measures the mean or average size of individual red blood cells. To obtain the MCV, the hematocrit is divided by the total RBC count. The MCV is an indicator of the size of red blood cells. If the MCV is low, the cells are microcytic or smaller than normal. Microcytic red blood cells are seen in iron deficiency anemia, lead poisoning and the genetic diseases thalassemia major and thalassemia minor. If the MCV is high, the cells are macrocytic, or larger than normal. Macrocytic red blood cells are associated with pernicious anemia and folic acid deficiencies. If the MCV is within the normal range, the cells are referred to as normocytic. A patient who has anemia from an acute hemorrhage would have a normocytic anemia. Mean corpuscular hemoglobin (MCH) measures the amount of hemoglobin present in one RBC. The weight of hemoglobin in an average cell is obtained by dividing the hemoglobin by the total RBC count. The result is reported by a very small weight called a picogram (pg). Mean corpuscular hemoglobin concentration (MCHC) measures the proportion of each cell taken up by hemoglobin. The results are reported in percentages, reflecting the proportion of hemoglobin in the RBC. The hemoglobin is divided by the hematocrit and multiplied by 100 to obtain the MCHC. The MCH and the MCHC are used to assess whether red blood cells are normochromic, hypochromic, or hyperchromic. An MCHC of less than 32% or an MCH under 17 pg. indicates that the red blood cells are deficient in hemoglobin concentration. This situation is most often seen with iron deficiency anemia. Normal Values for Erythrocyte Indices MCV: Men: 80-90 cubic microns Women: 82-98 cubic microns MCHC - 32-36% MCHC- 27-31 picomoles Classification of Anemias Using Erythrocyte Indices MCV, MCH and MCHC normal --- normocytic, normochromic anemia --- most often caused by acute blood loss Decreased MCV, MCH, and MCHC --- microcytic, hypochromic anemia --- most often
caused by iron deficiency Increased MCV, variable MCH and MCHC --- macrocytic anemia --- most often caused by Vitamin B12 deficiency (due to pernicious anemia) and folic acid deficiency Abnormal erthryocyte indices are helpful to classify types of anemia. However, diagnosis must be based on the patient's history, physical examination, and other diagnostic procedures.White blood cells, or leukocytes, are classified into two main groups: granulocytes and nongranulocytes (also known as agranulocytes).The granulocytes, which include neutrophils, eosinophils, and basophils, have granules in their cell cytoplasm. Neutrophils, eosinophils, and basophils also have a multilobed nucleus. As a result they are also called polymorphonuclear leukocytes or "polys." The nuclei of neutrophils also appear to be segmented, so they may also be called segmented neutrophils or "segs." The nongranuloctye white blood cells, lymphocytes and monocytes, do not have granules and have nonlobular nuclei. They are sometimes referred to as mononuclear leukocytes. WBCs (White Blood Cells) Eosinophils These cells have the purpose of giving large parasites such as helminths, a hard time. They attach via C3b receptors, the C3b having been produced during the course of alternative pathway complement activation by the helminth. The eosinophils release various substances from their eosinophilic granules. These include major basic protein (MBP), plus cationic proteins, peroxidase, arylsulphatase B, phospholipase D and histaminase. The granule contents are capable of damaging the parasite membrane. Polymorphonuclear Neutrophils (PMNs) Neutrophils, or neutrophil polymorphonuclear leucocytes, respond to chemotactic signals and leave capillaries by a complex process, involving margination (flowing nearer to the endothelial lining of blood vessels), rolling and then attaching (margination), following which they emigrate between the endothelial cells (extravasation, or diapedesis). Several mediators are involved. They include substances produced by micro-organisms, and by the cells participating in the inflammatory process. One such is a substance called interleukin-1 (IL-1), which is released by macrophages as a result of infection or tissue injury. Another is histamine, released by circulating basophils, tissue mast cells, and blood platelets. It causes capillary and venular dilatation. C3a and C5a produced during complement activation, are chemotactic for phagocytic cells. Another group of substances produced are the acute phase proteins. As a consequence of tissue damage, the liver produces a substance called C-reactive protein (CRP), which is so called on account of its ability to attach to the C-polysaccharide component of the cell wall of bacteria and fungi. This activates the complement system by the classical pathway, and as a result C3a is formed and coats the organism, facilitating its phagocytosis. Lymphocytes Lymphocytes are produced within bone marrow (a primary lymphoid organ). If they achieve immune-competence within the bone marrow, they are known as B cells, or if in the thymus (also a primary lymphoid organ), they are known as T cells. Organized lymphoid tissue elsewhere is known as secondary lymphoid tissue, and includes lymph nodes, adenoids, tonsils and mucosa associated tissue (MALT). MALT includes bronchus associated lymphoid tissue (BALT), gut associated lymphoid tissue (GALT), naso-phayngeal associated lymphoid tissue (NALT), and uro-genital associated lymphoid tissue. These lymphoid organs receive antigens from the tissues and mucosal
surfaces. Antigens that succeed in invading the blood stream are intercepted in the spleen. Lymphocytes respond to presented antigens by the production of antibodies (by B cells), to be described later, or lymphokines (by T and B cells). These have many actions, including control of the adaptive immune response by secondary action on the participating cells, and, in the case of cytolytic T cells, in killing virally-infected host cells. Lymphocytes possess receptors for these polypeptide antigens. The ability of a molecule or molecular configuration to induce an immune response is spoken of as immunogenicity, and the molecule as an immunogen. A molecule able to react with the ensuing antibody or T cell receptor is spoken of as an antigen. Some antigens, whilst able to react, are unable to induce, i.e. they lack immunogenicity and are known as haptens. Monocytes Monocytes circulate in the peripheral blood prior to emigration into the tissues. Within certain organs they have special names, e.g. in liver they are known as Kupfer cells, in brain as microglia, in kidney as mesangial cells, and in bone as osteoclasts. Elsewhere they are referred to as tissue macrophages. Basophils Basophils are non-phagocytic cells which, when activated, release numerous compounds from the basophilic granules within their cytoplasm. They play a major role in allergic responses, particularly type I hypersensitive reactions. The lifespan of white blood cells ranges from 13 to 20 days, after which time they are destroyed in the lymphatic system. When immature WBCs are first released from the bone marrow into the peripheral blood, they are called "bands" or "stabs." Leukocytes fight infection through a process known as phagocytosis. During phagocytosis, the leukocytes surround and destroy foreign organisms. White blood cells also produce, transport, and distribute antibodies as part of the body's immune response. The total number of white blood cells in a milliliter of blood, reported as an absolute number of "X" thousands of white blood cells, and the percentage of each of the five types of white blood cells. This test is known as a differential or "diff" and is reported in percentages. Normal values for total WBC and differential in adult males and females are: Total WBC: 5,000 - 10,000 Bands or Stabs: 3 - 5 % Granulocytes (or polymorphonuclears) Neutrophils (or segs): 50 - 70% relative value (3000-7000 absolute value) Eosinophils: 1 - 4% relative value (50-400 absolute value) Basophils: 0.5% - 1% relative value (25-100 absolute value) Agranulocytes (or Mononuclears) Lymphocytes: 25 - 40% relative value (1700-3400 absolute value) Moncytes: 2 - 8% relative value (200-600 absolute value) Each differential always adds up to 100%. To make an accurate assessment, consider
both relative and absolute values. For example a relative value of 70% neutrophils may seem within normal limits; however, if the total WBC is 20,000, the absolute value (70% x 20,000) would be an abnormally high count of 14,000. Neutrophils Neutrophils are so named because they are not well stained by either eosin, a red acidic stain, nor by methylene blue, a basic or alkaline stain. Neutrophils, are also known as "segs", "PMNs" or "polys" (polymorphonuclears). They are the body's primary defense against bacterial infection and physiologic stress. Normally, most of the neutrophils circulating in the bloodstream are in a mature form, with the nucleus of the cell being divided or segmented. Because of the segmented appearance of the nucleus, neutrophils are sometimes referred to as "segs." The nucleus of less mature neutrophils is not segmented, but has a band or rod-like shape. Less mature neutrophils - those that have recently been released from the bone marrow into the bloodstream - are known as "bands" or "stabs". Stab is a German term for rod. Increased Neutrophil Count An increased need for neutrophils, as with an acute bacterial infection, will cause an increase in both the total number of mature neutrophils and the less mature bands or stabs to respond to the infection. The term "shift to the left" is often used when determining if a patient has an inflammatory process such as acute appendicitis or cholecystitis. This term is a holdover from days in which lab reports were written by hand. Bands or stabs, the less mature neutrophil forms, were written first on the lefthand side of the laboratory report. Today, the term "shift to the left" means that the bands or stabs have increased, indicating an infection in progress. For example, a patient with acute appendicitis might have a "WBC count of 15,000 with 65% of the cells being mature neutrophils and an increase in stabs or band cells to 10%". This report is typical of a "shift to the left", and will be taken into consideration along with history and physical findings, to determine how the patient's appendicitis will be treated. In addition to bacterial infections, neutrophil counts are increased in many inflammatory processes, during physical stress, or with tissue necrosis that might occur after a severe burn or a myocardial infarction. Neutrophils are also increased in granulocytic leukemia. Decreased Neutrophil Count A decrease in neutrophils is known as neutropenia. Although most bacterial infections stimulate an increase in neutrophils, some bacterial infections such as typhoid fever and brucelosis and many viral diseases, including hepatitis, influenza, rubella, rubeola, and mumps, decrease the neutrophil count. An overwhelming infection can also deplete the bone marrow of neutrophils and produce neutropenia. Many antineoplastic drugs used to treat cancer produce bone marrow depression and can significantly lower the neutrophil count. Types of drugs that can produce neutropenia include some antibiotics, the psychotropic drug lithium, phenothiazines, and tricyclic antidepressants. Platelets Platelets are cell fragments formed in the bone marrow that circulate throughout the bloodstream. Platelets are a critical part of the body's ability to help blood clot. When blood vessels break, platelets form plugs that prevent further blood loss while healing takes place. Platelets live for approximately nine to 12 days in the bloodstream. A normal platelet count ranges between 150,000 and 450,000. Thrombocytopenia
occurs when the platelet count drops below 50,000. A thrombocytopenic patient is at high risk for bleeding if he or she has an injury or a complicating condition that affects blood coagulation, such as hemophilia or liver disease. When the platelet count drops below 20,000, the patient may have spontaneous bleeding that may result in death. A report of "adequate platelets" implies that there is at least one platelet for every 20 red blood cells. Critical low value for platelets - fewer than 50,000 platelets - places the patient at risk for bleeding episodes with even minor trauma; a platelet count under 20,000 can cause spontaneous bleeding. Thrombocytopenia occurs due to platelet destruction or impaired platelet production. In thrombotic thrombocytopenic purpura and disseminated intravascular coagulation, platelets are used up rapidly, and the platelet count falls significantly. Immune-related thrombocytopenic purpura, a condition that may occur early in HIV disease, may result in platelet destruction. In this situation, the HIV patient develops antibodies that attach to platelets as though they were an invading organism. When the damaged platelets circulate through the spleen, the attached antibody destroys them. When the bone marrow is suppressed due to radiation, chemotherapy, or other drugs that damage the bone marrow, production of new platelets is impaired. Malignancies of the bone marrow, such as leukemia, often cause the bone marrow to produce so many white blood cells that platelet production drops. A patient with a platelet count of less than 20,000 is at high risk for spontaneous bleeding. Signs of bleeding due to a low platelet count include: Easy bruising Unusual or heavy nosebleeds Hematuria Black, tar-like stools or frank bleeding with bowel movements Hematemesis Syncope or visual disturbances due to intracranial bleeding Gingival bleeding Heavy vaginal bleeding Treatment for thrombocytopenia involves treating the disease condition that is affecting platelet production or causing platelet destruction. Patients with thrombocytopenia may also receive platelet transfusions when the platelet count is dangerously low.
You might also like
- Paroxysmal Nocturnal Hemoglobinuria, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandParoxysmal Nocturnal Hemoglobinuria, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Types Of Hemolytic Anemia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandTypes Of Hemolytic Anemia, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- CBC InterpretationDocument8 pagesCBC InterpretationAna Marie Reyes BansaleNo ratings yet
- MK Hematology-AnemiasDocument86 pagesMK Hematology-AnemiasMoses Jr KazevuNo ratings yet
- Polycythemia ReportDocument18 pagesPolycythemia ReportCrisantaCasliNo ratings yet
- DR - Zahraa N. Alqaisy HematopathologistDocument23 pagesDR - Zahraa N. Alqaisy HematopathologistOmar MaanNo ratings yet
- Chapter TwoDocument7 pagesChapter TwoStanley AnadiNo ratings yet
- Problem Set 9: Hematopoeisis: Please Refer To The DiagramDocument3 pagesProblem Set 9: Hematopoeisis: Please Refer To The DiagramjohnjiaoNo ratings yet
- MEDSEM2LE4 Approach To AnemiaDocument19 pagesMEDSEM2LE4 Approach To AnemiaAndrea Ann MagpayoNo ratings yet
- Polycythemia Vera: What Are The Symptoms of Polycythemia?Document10 pagesPolycythemia Vera: What Are The Symptoms of Polycythemia?Dimpal ChoudharyNo ratings yet
- Case History: PBL 2 Failure To ThriveDocument9 pagesCase History: PBL 2 Failure To ThriveNazratun Choudhury BornyNo ratings yet
- Blood CellsDocument26 pagesBlood Cellsrussianbanana.hi.i.am.a.potatoNo ratings yet
- Anatomy and Physiology Summary Body Fluids and BloodDocument22 pagesAnatomy and Physiology Summary Body Fluids and BloodKelly Anne BrandNo ratings yet
- Blood: Physiology and Circulation (Edited by Kara Rogers) : ReferenceDocument3 pagesBlood: Physiology and Circulation (Edited by Kara Rogers) : ReferenceJossefa AlmanitaNo ratings yet
- 1 HaematologyDocument6 pages1 HaematologyEma FröhlichováNo ratings yet
- Blood Is A Body Fluid in Human and Other Animals That Delivers Necessary Substances Such AsDocument24 pagesBlood Is A Body Fluid in Human and Other Animals That Delivers Necessary Substances Such AsPaulo DanielNo ratings yet
- Red Blood Cells, Anemia, and Polycythemia: Lecturer DR Faraz Iqbal Tipu Indus UniversityDocument20 pagesRed Blood Cells, Anemia, and Polycythemia: Lecturer DR Faraz Iqbal Tipu Indus UniversityAreej TariqNo ratings yet
- 2019 Pathophysiology Textbook Part2 ZsmuDocument58 pages2019 Pathophysiology Textbook Part2 ZsmuSagar KhairwalNo ratings yet
- Blood Cells 2Document4 pagesBlood Cells 2Jo Louis CamiguingNo ratings yet
- Classification of Anemias: What Is Anemia, How Do You Diagnose Anemia, and How Are The Different Anemias Classified?Document78 pagesClassification of Anemias: What Is Anemia, How Do You Diagnose Anemia, and How Are The Different Anemias Classified?Kaushik BhuvaNo ratings yet
- PDF 20220223 180117 0000Document13 pagesPDF 20220223 180117 0000Ankit YadavNo ratings yet
- Anaphy Midterm Notes (The Blood Summary)Document4 pagesAnaphy Midterm Notes (The Blood Summary)Zosia Sage100% (1)
- Hematology 1Document64 pagesHematology 1Kervy Jay AgraviadorNo ratings yet
- EritropoesisDocument15 pagesEritropoesisFitriyani Dewi SuwandhiNo ratings yet
- JESUS Says: Take MY Hand and Let Us Walk Through This Day Together.Document63 pagesJESUS Says: Take MY Hand and Let Us Walk Through This Day Together.Jesus Mary JosephNo ratings yet
- Erythrocytosis: PolycythemiaDocument3 pagesErythrocytosis: PolycythemiaSaman HarsNo ratings yet
- Unit III AnemiaDocument58 pagesUnit III AnemiaTanishka SharmaNo ratings yet
- Anemia (: /Ə Ni Miə/ Also Spelled Greek Red Blood Cells HemoglobinDocument13 pagesAnemia (: /Ə Ni Miə/ Also Spelled Greek Red Blood Cells HemoglobinAryana BudiawanNo ratings yet
- Red Blood Cell Count (RBC)Document6 pagesRed Blood Cell Count (RBC)Sharmaine Grace FlorigNo ratings yet
- - تفسیر آزمایشات روتینDocument116 pages- تفسیر آزمایشات روتینrajabisamira8No ratings yet
- Hematology - A - RBCsDocument27 pagesHematology - A - RBCsAhmed Hassan KabarNo ratings yet
- CH 19 - The Blood - SV Complete (1) Kin 267 Module 7Document53 pagesCH 19 - The Blood - SV Complete (1) Kin 267 Module 7J aNo ratings yet
- Erythrocytosis PolycythemiaDocument2 pagesErythrocytosis PolycythemiaNeoMedica100% (2)
- Hereditary AnemiaDocument77 pagesHereditary AnemiaAravindh SivaNo ratings yet
- Physiology Lecture NoteDocument34 pagesPhysiology Lecture NoteAbdullahi YusuffNo ratings yet
- Complete Blood CountDocument18 pagesComplete Blood CountNazih MominNo ratings yet
- Red Cell DisordersDocument38 pagesRed Cell DisordersMARTINEZ JUSTINENo ratings yet
- Chapter 18 Anemia HematologyDocument30 pagesChapter 18 Anemia HematologyYelnats DatsimaNo ratings yet
- Pathophysiology of Anemia and Polycythemia Pathophysiology of Anemia and Polycythemia Pathophysiology of Anemia and PolycythemiaDocument48 pagesPathophysiology of Anemia and Polycythemia Pathophysiology of Anemia and Polycythemia Pathophysiology of Anemia and PolycythemiaSrishti GoenkaNo ratings yet
- Red Blood Cells Task 7Document3 pagesRed Blood Cells Task 7Sheharyar SandhuNo ratings yet
- BloodDocument39 pagesBloodAbdul HafeezNo ratings yet
- Anemia Anemia Describes The Condition in Which The Number of Red Blood Cells in The Blood Is Low. Probability & StatisticsDocument7 pagesAnemia Anemia Describes The Condition in Which The Number of Red Blood Cells in The Blood Is Low. Probability & StatisticsSahara GalayNo ratings yet
- AnemiaDocument11 pagesAnemiacentrino1780% (5)
- BloodDocument80 pagesBloodHem Chandra ShahNo ratings yet
- RBC DISORDERS StudentsDocument84 pagesRBC DISORDERS Studentskimberly abianNo ratings yet
- What Is Anemia?Document7 pagesWhat Is Anemia?Wajahat KazmiNo ratings yet
- Drowsiness Lethargy Tiredness Malaise Listlessness Weakness Muscular WeaknessDocument4 pagesDrowsiness Lethargy Tiredness Malaise Listlessness Weakness Muscular WeaknessCiariz CharisseNo ratings yet
- KitaDocument13 pagesKitaindah nur afifahNo ratings yet
- Hemoglobinopathies and Carbon Monoxide PoisoningDocument45 pagesHemoglobinopathies and Carbon Monoxide PoisoningBea SamonteNo ratings yet
- Circulation KDBDocument41 pagesCirculation KDBKiranNo ratings yet
- Haematological Tests: Jhanvi Ka Patel Rool No. 09Document21 pagesHaematological Tests: Jhanvi Ka Patel Rool No. 09Aditya PatelNo ratings yet
- Live Blood AnalysisDocument57 pagesLive Blood Analysisalliegator90% (10)
- Grade 7 Math ModuleDocument5 pagesGrade 7 Math ModuleAndre Labiste Aninon100% (2)
- AnemiaDocument2 pagesAnemiaSittie Salma RegaroNo ratings yet
- Tissue Engineering Red Blood Cells: MATSE 403Document10 pagesTissue Engineering Red Blood Cells: MATSE 403jtzug88No ratings yet
- Anemia.: Seminar OnDocument24 pagesAnemia.: Seminar OnAlma Susan100% (1)
- UPTODATE: Approach To The Adult With AnemiaDocument8 pagesUPTODATE: Approach To The Adult With AnemiakimberlynNo ratings yet
- Hemoglobin LevelsDocument13 pagesHemoglobin LevelsFebiola SafiraNo ratings yet
- Sickle Cell AnemiaDocument5 pagesSickle Cell Anemiaanne_obieNo ratings yet
- Anemia: Dr. Tanbira Alam MBBS, M.PhilDocument22 pagesAnemia: Dr. Tanbira Alam MBBS, M.Philsatvindar_muNo ratings yet
- Surgical InstrumentsDocument8 pagesSurgical InstrumentsCassandra Grace Labial PaynterNo ratings yet
- Operating Room ProceduresDocument13 pagesOperating Room ProceduresCassandra Grace Labial Paynter100% (1)
- Nursing Crib Com NURSING CARE PLAN HydrocephalusDocument3 pagesNursing Crib Com NURSING CARE PLAN HydrocephalusCassandra Grace Labial PaynterNo ratings yet
- Ketorolac (Drug Study)Document2 pagesKetorolac (Drug Study)Cassandra Grace Labial Paynter89% (18)
- Wa0005 PDFDocument75 pagesWa0005 PDFveniNo ratings yet
- Immunology ModuleDocument42 pagesImmunology ModuleAhmed KerAtyNo ratings yet
- Non Specific HostDocument46 pagesNon Specific HostAdrian BautistaNo ratings yet
- CT CellsDocument1 pageCT CellsTarlan SharifiNo ratings yet
- Immunology and Serology Lab IntroductionDocument10 pagesImmunology and Serology Lab IntroductionAldren Beliber100% (1)
- Ch2 InflamDocument49 pagesCh2 InflamleartaNo ratings yet
- Acute Inflammatory Response - : VPM 152 Winter 2006 Inflammation and Repair General Pathology 18Document19 pagesAcute Inflammatory Response - : VPM 152 Winter 2006 Inflammation and Repair General Pathology 18ANI REHMNo ratings yet
- Recommendations To Maintain Immune Health in Athletes Walsh 2018Document13 pagesRecommendations To Maintain Immune Health in Athletes Walsh 2018Felipe Ricardo Garavito PeñaNo ratings yet
- Interpretation of Peripheral SmearDocument34 pagesInterpretation of Peripheral Smearswathi bs100% (1)
- Immunology (Final) Laden SalehDocument193 pagesImmunology (Final) Laden SalehLaden SalehNo ratings yet
- 17 Human Health and Disease: SolutionsDocument14 pages17 Human Health and Disease: SolutionsEkta ManglaniNo ratings yet
- Chapter 2 (Questions 2008-2009 Compiled)Document89 pagesChapter 2 (Questions 2008-2009 Compiled)vetpathforum100% (1)
- (S.C. Rastogi) Essentials of Animal Physiology, 4t (BookSee - Org) 247Document1 page(S.C. Rastogi) Essentials of Animal Physiology, 4t (BookSee - Org) 247Indah Rizka AprilianiNo ratings yet
- Phagocytosis Block 5Document25 pagesPhagocytosis Block 5Mark Johnuel DuavisNo ratings yet
- Diagnostic Cytology: 10.1 Methods of Specimen AttainmentDocument54 pagesDiagnostic Cytology: 10.1 Methods of Specimen AttainmentSuraj_Subedi100% (3)
- Test Bank For Pathophysiology 8th Edition by MccanceDocument15 pagesTest Bank For Pathophysiology 8th Edition by Mccanceedwardfrostxpybgdctkr100% (25)
- CARDIO (PBL3) - Mohamad Arbian Karim - FMUI20Document10 pagesCARDIO (PBL3) - Mohamad Arbian Karim - FMUI20Mohamad Arbian KarimNo ratings yet
- 1 Semestr 1 LevelDocument9 pages1 Semestr 1 LevelHart ElettNo ratings yet
- Anti Inflammatory Prospective Study of Commiphora Mukul (Guggul) On Wistar Albino RatsDocument54 pagesAnti Inflammatory Prospective Study of Commiphora Mukul (Guggul) On Wistar Albino RatsKrish NalimelaNo ratings yet
- Infectious Diseases of The Dog and Cat, 3rd Edition: CHAPTER 90 Hepatobiliary InfectionsDocument47 pagesInfectious Diseases of The Dog and Cat, 3rd Edition: CHAPTER 90 Hepatobiliary InfectionssoledadDC329No ratings yet
- Leukocytes, Granulocytes, The Monocyte-Macrophage System, and InflammationDocument10 pagesLeukocytes, Granulocytes, The Monocyte-Macrophage System, and InflammationShi no MeNo ratings yet
- White Blood Cells (WBCS) : Total Leukocyte Count (TLC)Document7 pagesWhite Blood Cells (WBCS) : Total Leukocyte Count (TLC)Sharan MurugaboopathyNo ratings yet
- Oncologic NursingDocument132 pagesOncologic Nursingɹǝʍdןnos100% (10)
- Soalan Objektif Bab 10 & Bab 11Document16 pagesSoalan Objektif Bab 10 & Bab 11Sains Matematik PahangNo ratings yet
- Strategies of Neutrophil Diversification: Nature ImmunologyDocument10 pagesStrategies of Neutrophil Diversification: Nature ImmunologylfjuradozNo ratings yet
- Acute Myelogenous Leukemia - Patho, Anatomy, and Diagnostic TestDocument66 pagesAcute Myelogenous Leukemia - Patho, Anatomy, and Diagnostic TestCharles Kevin L. Bataga33% (3)
- Peripheral Blood Smear and HistologyDocument26 pagesPeripheral Blood Smear and Histologystudent2013No ratings yet
- Blood Histology Junqueira'sDocument22 pagesBlood Histology Junqueira'sDaira LizetNo ratings yet
- 1 - Cells and Tissues of The Immune SystemDocument32 pages1 - Cells and Tissues of The Immune SystemCaitríona BurkeNo ratings yet
- (Psychology of Emotions, Motivations and Actions) Leandro Cavalcanti (Ed.), Sofia Azevedo (Ed.) - Psychology of Stress - New Research-Nova Science Publishers (2013)Document214 pages(Psychology of Emotions, Motivations and Actions) Leandro Cavalcanti (Ed.), Sofia Azevedo (Ed.) - Psychology of Stress - New Research-Nova Science Publishers (2013)Jesus Jimenez100% (1)