Professional Documents
Culture Documents
208-The Versatility and Effectiveness
Uploaded by
ezfreshOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
208-The Versatility and Effectiveness
Uploaded by
ezfreshCopyright:
Available Formats
The Versatility and Ef f ectiv eness of the Multiloop Edg e wise Ar chwir e (MEAW) in T r eatment of Various Malocclusions
Young H. Kim, DDS, DMD, MS1/Unae K. Han, DMD, MPH, MS1
Aim: Treatment of anterior open bite is considered the most difficult task in the orthodontic specialty. These malocclusions are frequently subjected to orthognathic surgery, with questionable results. Multiloop edgewise archwire therapy, however, has been found to be effective in treating open bite malocclusions. Multiloop edgewise archwire therapy has been shown to be versatile and capable of correcting other malocclusions, such as Class II, Class III, deep overbite, and malocclusions with marked midline deviations. Methods: The biomechanics of multiloop edgewise archwire therapy and pertinent research findings are discussed, and three cases are presented. Conclusion: Orthognathic surgery was recommended for two of the three cases presented, but successful treatment without surgery was achieved with multiloop edgewise archwire therapy. World J Orthod 2001;2:208218.
OUT WRITTEN PERMISSION FROM THE PUBLISHER.
COPYRIGHT 2001 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITH-
he multiloop edgewise archwire (MEAW) was created in 1967 to treat severe anterior open bite malocclusions and it has been found to be effective in correcting such malocclusions. 1 It has since evolved to allow MEAW therapy of any malocclusion, especially during the final stage of treatment. In this article, the treatment modality of three cases will be discussed. The MEAW is constructed of a 15-inch 0.016 0.022-inch standard stainless steel rectangular wire (3M Unitek, Monrovia, CA, USA) and is shaped into an ideal arch form with L-shaped loops between the teeth from the distal of the lateral incisor to the posterior end of the dentition. Usually, there are five loops on each side in an arch that consists of 14 teeth (Fig 1). Since this wire is a relatively soft stainless steel wire, it should be heat-treated at about 1000F for approximately 5 minutes to increase the resiliency. Figure 2 shows examples of upper and lower MEAWs in the ideal arch forms. To upright mesially inclined premolars and molars, 3- to 5-
1Private
Practice of Orthodontics, Weston, Massachusetts, USA.
REPRINT REQUESTS/CORRESPONDENCE Dr Young H. Kim, 30 Colpitts Road, Weston, MA 02493, USA. E-mail: youngkimdmd@earthlink.net
degree tip-back bends are incorporated into the wire, from the first premolars to the second molars, according to the degree of uprighting required (Fig 3). For MEAW therapy, 0.018-inch slot brackets are used. Since the advent of the MEAW, its treatment modality has been used worldwide and numerous repor ts of successful results have been published.213 Some orthodontists have described the MEAW technique as magical or unbelievable, but it certainly is not. The diagnosis and treatment plan must be correct and construction of the MEAW must be precise to deliver the necessary forces to move the teeth to an optimal, stable relationship. Commonly, severe malocclusions such as open bite, Class III, or even Class II have been subjected to surgical intervention due to the inability to correct them with conventional orthodontic treatment. The MEAW technique can correct a majority of severe malocclusions when no disfiguring facial deformity exists. A variety of orthodontic techniques have come and gone, but most edgewise principles introduced by Edward H. Angle 75 years ago remain viable. Unfortunately, there are too many orthodontists who are not accustomed to bending wires and who instead depend on prefabricated straight archwires. Those who do not wish to bend wires cannot use this technique. Each patient is unique both
208
VOLUME 2, NUMBER 3, 2001
Kim/Han
OUT WRITTEN PERMISSION FROM THE PUBLISHER.
COPYRIGHT 2001 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITH-
Multiloop edgewise archwire Upper 89 mm 78 mm 56 mm 2.75 mm 7 6 5 4 3 2 1 .016 1.52 mm 78 mm 78 mm 5 mm 3 4 5 6 7
1 2 0.22 wire
0.5 mm
Multiloop edgewise archwire Lower 7 6 5 4 3 2 1 1 2 3 4 5
0.5 mm 6 7
89 mm
2.75 mm 67 mm 45 mm 67 mm .016 0.22 wire
78 mm
Fig 1
Diagrams of the upper and lower multiloop edgewise archwires (MEAWs).
Fig 2
Occlusal views of the MEAWs. (a) Upper. (b) Lower.
Fig 3
Lateral view of the MEAWs with tip-back activations. (a) Upper. (b) Lower.
209
Kim/Han
WORLD JOURNAL OF ORTHODONTICS
facially and dentally. The dental arch, therefore, must be individualized for that particular patient.
BIOMECHANICS
Vertical and horizontal tooth movement must be controlled in addition to achieving rotations and torque. The MEAW produces individualized movement of the posterior teeth and group movement of the incisors. The objectives of the loops can be characterized as follows: 1. The loops between the teeth significantly reduce the load deflection rate of the wire to as low as one-tenth of a 0.016 0.022-inch ideal archwire. 2. The vertical components (anterior and posterior legs) of the loops serve as a breaker between the teeth and allow the teeth to move independently. 3. The horizontal components of the loops allow control of the vertical relationship of each tooth. 4. The rectangular wire (0.016 0.022) provides torque control for each tooth, and the loops provide independent torquing tooth movement. 5. The tip-back activations in the posterior segment of the wire produce the uprighting movement of the posterior teeth. Fifteen degrees of molar uprighting produce as much as 4.5 mm of distalization. 6. Along with the tip-back activations, anterior vertical elastics correct the occlusal planes and, in turn, close the open bite. A photoelasticity study14 and a study on the Computer Aided Engineering Design System 15 have shown how the MEAW system can precisely distribute the force to an area where tooth movement is required. An experimental study on Rhesus monkeys shows that marked tooth movement, along with considerable bone remodeling cellular activity, was found in the monkey with MEAW therapy, while the control monkey without the MEAW showed signs of root resorption and insignificant cellular activity.16
bite) in the growing group was corrected to +1.58 mm of the average overbite, a net change of 3.85 mm. Similarly, it was found that 2.23 mm of the average anterior clearance in the nongrowing group was corrected to +1.78 mm of overbite, a net change of 4.01 mm. The posttreatment follow-up evaluation showed that there was an average decrease in overbite of 0.23 mm in the growing group and 0.35 in the nongrowing group. The relapses were not clinically or statistically significant.18
OUT WRITTEN PERMISSION FROM THE PUBLISHER.
COPYRIGHT 2001 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITH-
CEPHALOMETRIC ANALYSIS
Diagnostically, the cephalometric analysis is obtained by the overbite depth indicator (ODI) for an appraisal of the vertical component 19 and the anteroposterior dysplasia indicator (APDI) as a determinant of the horizontal component.20 The ODI is a combined measurement of two angles: the A-B plane to the mandibular plane and the palatal plane to the Frankfort horizontal (FH) plane. When the palatal plane slopes upward and forward in relation to the FH plane, it is read as a negative angle. When the palatal plane slopes downward and forward in relation to the FH plane, it is read as a positive angle. Should the palatal plane be a negative value, this value is subtracted from the A-B to the mandibular plane angle. Conversely, if the palatal plane angle is read as a positive value, the angle is added to the A-B to the mandibular plane angle. The normal mean of the ODI is 74.5 degrees. The ODI had the highest correlation coefficient value of 0.558 and the receiver operating characteristic (ROC) analysis21 showed that the ODI had the greatest validity in determining the open bite skeletal pattern. The analytic implications of the ODI are that when the figure is less than the mean, the greater chance there is of an open bite or a tendency toward it. On the other hand, if the measurement is greater than the mean, a greater depth of overbite or the tendency toward it is predicted. The APDI is obtained from three angles: the facial plane angle (Downs), plus or minus the A-B plane angle (Downs), and plus or minus the palatal plane angle in relation to the FH plane. The normal mean of the APDI is 81.4 degrees, with the highest correlation coefficient value of 0.643. The smaller the APDI value relative to the normal mean, the greater probability there is that a Class II malocclusion exists. Conversely, as the APDI value increases above the normal mean, the greater the chance of a Class III occlusal displacement. The ROC analyses on the APDI showed the highest validity in determining Class II and Class III malocclusions.22,23
210
CLINICAL STUDIES
In nongrowing patients, it has been found that the skeletal pattern does not change significantly after the treatment of open bite malocclusion. The open bites, however, were corrected, which indicated that the skeletal pattern does not have to be changed to correct an open bite malocclusion.17 In a posttreatment follow-up study on open bite malocclusions, 2.27 mm of the average anterior clearance (open
VOLUME 2, NUMBER 3, 2001
Kim/Han
The combination factor (CF) is used to determine the need for tooth extraction in the treatment of maloccusion.24 The CF is a combined figure of the ODI and the APDI. The mean value of the CF, therefore, is 155.9 degrees. In general, whenever the CF figure is higher than 155 degrees, extractions are not necessary to treat a malocclusion. Conversely, when the figure falls below 150 degrees, extractions are more likely indicated. To verify this, a study was conducted on 226 nonextraction cases and 246 extraction cases and it was found that the mean value of CF was 151 degrees. In other words, nearly all the cases in the nonextraction group showed CF values higher than 151 degrees and the cases in the extraction group fell below that level.25
DIAGNOSIS AND TREATMENT MODALITY
Case 1
Figure 4a shows the intraoral photographs of a female patient, 23 years of age, with a severe anterior open bite malocclusion. She had received treatment at an early age, but it markedly relapsed. She experienced temporomandibular joint pain and returned to her orthodontist, who equilibrated the molar cusps to close the bite, but this was not successful. He then recommended a surgical intervention, but the patient was hesitant to undergo surgery. Instead, she was successfully treated with MEAW therapy. The cephalometric analysis showed a skeletal pattern with an ODI of 69 degrees, an APDI of 79 degrees, and a CF of 148 degrees, indicating a Class II open bite pattern (Fig 5a). The mandibular dentition was mesially inclined. The maxillary occlusal plane sloped upward and forward, whereas the mandibular occlusal plane sloped downward and forward. The occlusal planes and the axial inclinations, therefore, had to be reconstructed to correct this malocclusion. The third molars, which were causing a wedging effect, had to be extracted. Subsequently, the maxillary and mandibular arches were aligned. After the mandibular second molars were uprighted, the joint symptoms subsided. Four months after the onset of treatment, upper and lower MEAW therapy with 3degree tip-back activation was applied, along with bilateral 3/16-inch 6-oz anterior vertical elastics from the upper first loop to the lower first loop (Fig 4b). Four months later, the open bite and the overjet were nearly corrected to a normal relationship, but the lower mandibular occlusal plane lacked a natural curve of Spee, which prevented a sufficient overbite.
211
The lower MEAW, therefore, was removed and a curve of Spee was incorporated. The wire was reinserted and bilateral 3/16-inch, 6-oz elastics were applied from the upper first loop to the lower first loop (Fig 4c). These elastics were worn full-time, except while eating, and were replaced with new ones at bedtime. After 6 months of MEAW therapy, a normal occlusion was obtained (Fig 4d). The patient was 24 years of age; the total active treatment time was 11 months. The posttreatment cephalogram and panoral radiograph showed favorable changes in the axial inclinations and the occlusion (Fig 5b). The pre- and posttreatment superimposition tracings showed that the mandible autorotated upward and forward about 4 degrees (Fig 5c). This result was essentially due to the elimination of the wedging effect achieved by removing the third molars. An examination at 37 months posttreatment revealed excellent stability clinically and radiographically (Figs 4e and 5d). The maxillary right lateral incisor was intruded slightly, which was attributed to a pencil-biting habit.
OUT WRITTEN PERMISSION FROM THE PUBLISHER.
COPYRIGHT 2001 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITH-
Case 2
Figure 6a shows the intraoral views of a patient, a boy 13 years of age, with a Class II, Division 1 deep overbite malocclusion. The cephalometric analysis revealed an ODI of 79 degrees and an APDI of 79 degrees, indicating a Class II deep overbite skeletal pattern (Fig 7a). Treatment to align the maxillary and mandibular dentitions was initiated with cervical headgear and a bite plate for 15 months. The Class II relationship, however, showed no signs of improvement. Poor compliance with the headgear may have been the reason for this lack of improvement. The Class II relationship remained the same and there was a bilateral buccal crossbite in the premolar region. At this time, the MEAW therapy was begun with 3-degree tip-back bends in the posterior segments of the maxillary dentition. A rectangular (0.016 0.022) ideal arch with gentle second-order tip-back bends was inserted on the mandibular dentition. The patient wore 5/16-inch, 6-oz Class II bilateral elastics from the mandibular second molar hook to the first loop of the upper MEAW (Fig 6b). Ten months of elastic therapy eliminated this marked Class II malocclusion (Fig 6c). The posttreatment cephalogram and panoral radiograph showed a normal dental relationship (Fig 7b). The posttreatment cephalometric superimposition tracings indicated more downward growth than forward growth of the maxilla and mandible (Fig 7c). These growth changes, in turn, decreased the ODI to 75 degrees and APDI to 78 degrees. A follow-up examination at
Kim/Han
WORLD JOURNAL OF ORTHODONTICS
OUT WRITTEN PERMISSION FROM THE PUBLISHER.
COPYRIGHT 2001 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITH-
Fig 4 Case 1. (a) Intraoral photographs showing the severe anterior open bite malocclusion of a 23-year-old female patient. She was treated at an early age, but her occlusion had markedly relapsed. Her orthodontist recommended surgical treatment, but she refused. (b) Intraoral photographs showing the MEAW mechanism in place. Bilateral elastics (3/16 inch, 6 oz) were engaged from the upper first loop to the lower first loop. (c) Four months later, the open bite was almost corrected. Then, a curve of Spee was incorporated into the lower MEAW to increase the overbite. Anterior vertical elastics (3/16 inch, 6 oz) were continued. (d) Posttreatment intraoral photographs, when the patient was 24 years of age, show the excellent result. The total treatment duration was 11 months. (e) Intraoral photographs at 37 months posttreatment, when the patient was 27.1 years of age, show an excellent occlusion and good stability.
212
VOLUME 2, NUMBER 3, 2001
Kim/Han
OUT WRITTEN PERMISSION FROM THE PUBLISHER.
COPYRIGHT 2001 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITH-
22y 11mo 24y 22y 11mo 24y
Fig 5 Case 1. (a) Pretreatment cephalogram and panoral radiograph. The ODI was 69 degrees and the APDI was 79 degrees. (b) Posttreatment cephalogram and panoral radiograph show a normal dental relationship. (c) Posttreatment cephalometric superimposition reveals that the molars were uprighted and the mandible autorotated counterclockwise about 4 degrees. (d) The 37-month follow-up cephalogram and panoral radiograph show excellent stability.
213
Kim/Han
WORLD JOURNAL OF ORTHODONTICS
OUT WRITTEN PERMISSION FROM THE PUBLISHER.
COPYRIGHT 2001 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITH-
Fig 6 Case 2. (a) Pretreatment intraoral photographs of a boy, 13 years of age, with a marked Class II, Division 1 malocclusion. (b) Fifteen months of cervical headgear and bite plate therapy did not correct the Class II relationship. The course of treatment, therefore, was changed to MEAW therapy. The upper MEAW and a lower 0.016 0.022inch ideal archwire with second-order tip-back bends were inserted, along with 5/16-inch, 6-oz Class II elastics. (c) Ten months after the Class II elastic therapy, the malocclusion was corrected. (d) Photographs at 27 months posttreatment show a slight deepening of the bite, but the occlusion stayed reasonably constant.
214
VOLUME 2, NUMBER 3, 2001
Kim/Han
OUT WRITTEN PERMISSION FROM THE PUBLISHER.
COPYRIGHT 2001 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITH-
13y 15y 1mo
13y 15y 1mo
Fig 7 Case 2. (a) Pretreatment cephalogram and panoral radiograph. The ODI was 79 degrees and APDI was 70 degrees, indicating a Class II deep overbite skeletal pattern. (b) Posttreatment cephalogram and panoral radiograph show a satisfactory result. (c) Posttreatment cephalometric superimposition reveals that the maxilla and the mandible grew downward. (d) Cephalogram and panoral radiograph, taken 27 months posttreatment, when the patient was 17.5 years of age.
215
Kim/Han
WORLD JOURNAL OF ORTHODONTICS
OUT WRITTEN PERMISSION FROM THE PUBLISHER.
COPYRIGHT 2001 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITH-
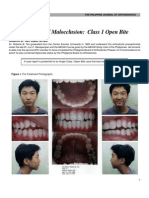
Fig 8 Case 3. (a) Pretreatment intraoral photographs of an Asian woman, 20 years 11 months of age, with a Class III malocclusion and a right unilateral posterior crossbite. (b) Seven months after the onset of treatment, an upper rectangular ideal arch and lower MEAW with 3-degree tip-back activation were inserted, and 5/16-inch, 6-oz Class III elastics were employed. (c) Ten months after the start of MEAW therapy, a normal occlusion was obtained. (d) The follow-up photographs at 28 months posttreatment show no changes in the occlusion.
27 months posttreatment showed that although the bite had deepened slightly, the occlusion remained stable (Figs 6d and 7d).
Case 3
An Asian woman, 20 years 11 months of age, had a Class III malocclusion with a slight anterior crossbite and a unilateral posterior crossbite on the right side
216
(Fig 8a). For 4 years, starting at 8 years of age, she underwent chin cap therapy for Class III malocclusion at a university clinic. However, her occlusion later relapsed. Between 13 and 15 years of age, the patient received full orthodontic treatment after extraction of the four first premolars. The occlusion, however, progressively worsened. At 20 years of age, orthognathic surgery was recommended, but she and her parents refused. Her family history was negative for the prognathic mandible.
VOLUME 2, NUMBER 3, 2001
Kim/Han
OUT WRITTEN PERMISSION FROM THE PUBLISHER.
COPYRIGHT 2001 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITH-
20y 11mo 22y 5mo 20y 11mo 22y 5mo
Fig 9 Case 3. (a) Pretreatment cephalogram and panoral radiograph. The ODI was 60 degrees and the APDI was 91 degrees. This indicated a Class III skeletal pattern with an open bite tendency. (b) Posttreatment cephalogram and panoral radiograph show an excellent dental relationship. (c) Posttreatment cephalometric superimposition reveals that there were no changes in the skeletal pattern, but the mandibular dentition was distalized and significantly uprighted.
The cephalometric analysis revealed that her ODI was 60 degrees and the APDI was 91 degrees, indicating a Class III skeletal pattern, with an open bite tendency (Fig 9a). The mandibular posterior dentition was mesially inclined. All four third molars were present but unerupted. To upright the posterior dentition, the third molars were removed, and the maxillar y and mandibular arches were aligned. Seven months after treatment onset, an upper rectangular ideal
217
arch (0.016 0.022) with second-order tip-back activations and a lower MEAW with 3-degree tipback activations were inserted, along with 5/16inch, 6-oz Class III elastics (Fig 8b). The elastics were engaged from the upper second molar hooks anteriorly to the first loops of the lower MEAW. Ten months after the onset of MEAW therapy, the malocclusion was satisfactorily corrected and the appliances were removed (Fig 8c). The duration of active treatment was 17 months.
Kim/Han
WORLD JOURNAL OF ORTHODONTICS
The posttreatment cephalogram and panoral radiograph showed a normal dental relationship and an uprighted posterior dentition (Fig 9b). The posttreatment cephalometric superimposition tracings revealed that the mandible had moved slightly downward and backward, while the mandibular dentition was considerably distalized (Fig 9c). The posttreatment ODI and APDI changed slightly, to 58.5 degrees and 87 degrees, respectively. Follow-up examination at 28 months posttreatment revealed an excellent occlusion and good stability of the dentition (Fig 8d).
CONCLUSION
The MEAW mechanism is both versatile and effective in correcting malocclusions such as open bite, deep overbite, Class II, Class III, and malocclusion with a midline deviation. Three cases were presented in this article, and in two of them another orthodontist had recommended orthognathic surgery, but all the patients were successfully treated with MEAW therapy. The treatment duration with the MEAW is usually short, particularly in cases of open bite malocclusions. It is, however, important to remember that mere insertion of the MEAW does not guarantee treatment success. MEAW therapy requires a keen sense of judgment in diagnosis and treatment planning. Since the MEAW mechanism moves the teeth rapidly, every minute detail of the wire bending must be precise to obtain the optimal result.
REFERENCES
1. Kim YH. Anterior openbite and its treatment with Multiloop Edgewise Arch-Wire. Angle Orthod 1987;57:290321. 2. Sato S. Application of Multiloop Edgewise Arch-Wire (MEAW) on the occlusal reconstruction of malocclusion. Japan Ortho Practice 1989;5:5773. 3. Kim YH. Common undesirable side effects of straight archwire technic. Int J MEAW 1994;1:85104. 4. Sato S. Case report: Developmental characterization of skeletal Class III malocclusion. Angle Orthod 1994;64:105111. 5. Mestre J. Reporte de un caso quirurgico. Rev Iberoam Ortod 1994;13:126134. 6. Protacio C, Sato S. The role of posterior discrepancy in the development of Class III malocclusion: Its clinical importance. Int J MEAW 1995;2:5168. 7. Oh SS. Non-surgical correction of a severe Class III malocclusion. Int J MEAW 1995;2:6983.
8. Kondo E. Two skeletal Class II cases with retrognathic mandible and temporo-mandibular joint disorder. Int J MEAW 1996;3:3850. 9. Kim YH. Nature of deep overbite and its treatment. Int J MEAW 1996;3:6786. 10. Park EW. Treatment of severe skeletal Class III malocclusion with MEAW therapy. Int J MEAW 1997;4:7594. 11. Kim YH. Aberrant growth of the mandible and its effect on the occlusion. Int J MEAW 1999;6:522. 12. Kim YH. Treatment of severe openbite malocclusions without surgical intervention. In: McNamara JA Jr (ed). Growth Modification: What Works, What Doesnt And Why. Monograph No. 35, Craniofacial Growth Series. Ann Arbor: Center for Human Growth and Development, The University of Michigan, 1999:193212. 13. Kim YH. Treatment of anterior openbite and deep overbite malocclusions with the Multiloop Edgewise Arch-Wire (MEAW) therapy. In: McNamara JA Jr (ed). The Enigma of the Vertical Dimension. Monograph No. 36, Craniofacial Growth Series. Ann Arbor: Center for Human Growth and Development, The University of Michigan, 2000:175202. 14. Matsui S, Caputo AA, Hayashi H, Katayama K, Kiyomura H. Effects of L-loops on the Multiloop Edgewise Arch-Wire with Class II elastics: A photoelasticity study. J Jpn Orthod Soc 1997;56:383390. 15. Nahm DS. Analysis of the biomechanical effects of MEAW. Int J MEAW 1994;1:105114. 16. Lee SY. Histologic changes in mandibular periodontium of the monkey following experimental extrusion of anterior teeth [PhD thesis]. Seoul: Seoul National University, 1995. 17. Chang YI, Moon SC. Cephalometric evaluation of the anterior open bite treatment. Am J Orthod Dentofacial Orthop 1999;115:2938. 18. Kim YH, Han UK, Lim DD, Serraon MLP. Stability of anterior openbite with Multiloop Edgewise Arch-Wire therapy. Am J Orthod Dentofacial Orthop 2000;118:4354. 19. Kim YH. Overbite depth indicator (ODI) with particular reference to anterior openbite. Am J Orthod 1974;65:586611. 20. Kim YH, Vietas JJ. Anteroposterior dysplasia indicator (APDI): An adjunct to cephalometric differential diagnosis. Am J Orthod 1978;113:619633. 21. Wardlaw DW, Smith RJ, Hertweck DW, Hildeboldt CF. Cephalometrics of anterior openbite: A receiver operating characteristic (ROC) analysis. Am J Orthod Dentofacial Orthop 1992;101: 234243. 22. Han UK, Kim YH. Determination of Class II and Class III skeletal patterns. Am J Orthod Dentofacial Orthop 1998;113: 538545. 23. Freudenthaler JW, Celer AG, Schneider B. Overbite depth and anteroposterior dysplasia indicators: The relationship between occlusal and skeletal patterns using the receiver operating characteristic (ROC) analysis. Eur J Orthod 2000;22:7583. 24. Kim YH, Caulfield Z, Chung WN, Chang YI. Overbite depth indicator, anteroposterior dysplasia indicator, combination factor and extraction index. Int J MEAW 1994;1:1132. 25. Chung WN, Kim YH. A comparative study of means and standard deviations of ODI, APDI, and combination factor in various malocclusions. Korean J Orthod 1992;22:779831.
OUT WRITTEN PERMISSION FROM THE PUBLISHER.
COPYRIGHT 2001 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITH-
218
You might also like
- Instructor's Manual For COUNSELING & PSYCHOTHERAPY THEORIES: IN CONTEXT AND PRACTICEDocument172 pagesInstructor's Manual For COUNSELING & PSYCHOTHERAPY THEORIES: IN CONTEXT AND PRACTICEherbalizer3392% (12)
- Pediatric Acute Lymphoblastic LeukemiaDocument9 pagesPediatric Acute Lymphoblastic LeukemiaAlvin PratamaNo ratings yet
- A Clinical Nurse Specialist-Led Interprofessional Quality Improvement Project To Reduce Hospital-Acquired Pressure Ulcers Clinical Nurse SpecialistDocument7 pagesA Clinical Nurse Specialist-Led Interprofessional Quality Improvement Project To Reduce Hospital-Acquired Pressure Ulcers Clinical Nurse SpecialistIhsan Nur MahmudiNo ratings yet
- Medication Calculation Practice Problems: Level Ii, Iii and IvDocument6 pagesMedication Calculation Practice Problems: Level Ii, Iii and IvQueennita100% (7)
- Essentials of Orthognathic Surgery, 3eDocument14 pagesEssentials of Orthognathic Surgery, 3epaolacsuarezaNo ratings yet
- Class II - DD and MX PDFDocument14 pagesClass II - DD and MX PDFserahNo ratings yet
- Holdaway SDocument64 pagesHoldaway SDryashpal Singh100% (1)
- Tranexamic AcidDocument3 pagesTranexamic AcidEchik Rodriguez100% (2)
- Class II Malocclusions Diagnostic and Clinical Considerations With and Without Treatment. Seminars in Orthodontics 12 (1) 11-24, Mar 2006. S. BisharaDocument14 pagesClass II Malocclusions Diagnostic and Clinical Considerations With and Without Treatment. Seminars in Orthodontics 12 (1) 11-24, Mar 2006. S. BisharaAhmad EgbariaNo ratings yet
- MRI TMJ TUTORIAL - PpsDocument22 pagesMRI TMJ TUTORIAL - Ppsguhander100% (1)
- Roth Versus MBTDocument23 pagesRoth Versus MBTJose Antonio Figuroa AbadoNo ratings yet
- Arabic TerminologiesDocument5 pagesArabic TerminologiesPearly Angelique Boco-MalateNo ratings yet
- DV y Plano OclusalDocument8 pagesDV y Plano OclusalDiego Andres Hincapie HerreraNo ratings yet
- Vethathiri - Holistic HealthDocument19 pagesVethathiri - Holistic HealthProf. Madhavan100% (2)
- The Story of The Master and Legend: 2015 American Association of Orthodontists Annual SessionDocument11 pagesThe Story of The Master and Legend: 2015 American Association of Orthodontists Annual SessionPaolaLNo ratings yet
- Cephalometrics in Clinical Practice: Beverly Hills, CalifDocument22 pagesCephalometrics in Clinical Practice: Beverly Hills, CalifDanilo Jose GomezNo ratings yet
- Andrews 1972 The Six Keys To Normal OcclusionDocument15 pagesAndrews 1972 The Six Keys To Normal OcclusionMiguelNo ratings yet
- Spradley1981 PDFDocument10 pagesSpradley1981 PDFFernando Ruiz BorsiniNo ratings yet
- Twin BlockDocument130 pagesTwin BlockRolando GamarraNo ratings yet
- Currie Et Al 2017 Angle Orthod PDFDocument14 pagesCurrie Et Al 2017 Angle Orthod PDFplayer osama100% (1)
- SATO Dental Asymmetry - TMDDocument5 pagesSATO Dental Asymmetry - TMDJorge Mori VelásquezNo ratings yet
- SEDATION and ANALGESIA in The PICU - Bijapur - Dr. Anand BhutadaDocument64 pagesSEDATION and ANALGESIA in The PICU - Bijapur - Dr. Anand BhutadacrplzNo ratings yet
- Self Care Deficit Nursing TheoryDocument30 pagesSelf Care Deficit Nursing TheoryDairyl Tagaro100% (1)
- RespiratoryDocument4 pagesRespiratoryDara Krishna Bantugan100% (1)
- 12 Diagnostic Aids For Functional AppliancesDocument240 pages12 Diagnostic Aids For Functional AppliancesDr Shivam VermaNo ratings yet
- Interceptive Orthodontics: A Practical Guide to Occlusal ManagementFrom EverandInterceptive Orthodontics: A Practical Guide to Occlusal ManagementNo ratings yet
- Nonvital Pulp Therapy On Primary TeethDocument15 pagesNonvital Pulp Therapy On Primary TeethJose RoldanNo ratings yet
- The Invisalign Appliance Today A Thinking Person S Orthodontic Appliance 2017 Seminars in OrthodonticsDocument53 pagesThe Invisalign Appliance Today A Thinking Person S Orthodontic Appliance 2017 Seminars in Orthodonticsdruzair007No ratings yet
- Understanding Masticatory Function in Unilateral CrossbitesFrom EverandUnderstanding Masticatory Function in Unilateral CrossbitesNo ratings yet
- MSE 10.1016@j.ajodo.2016.10.025Document11 pagesMSE 10.1016@j.ajodo.2016.10.025Neycer Catpo NuncevayNo ratings yet
- Orthodontically Driven Corticotomy: Tissue Engineering to Enhance Orthodontic and Multidisciplinary TreatmentFrom EverandOrthodontically Driven Corticotomy: Tissue Engineering to Enhance Orthodontic and Multidisciplinary TreatmentFederico BrugnamiNo ratings yet
- SS COCrDocument101 pagesSS COCrsoujanyaNo ratings yet
- Beggs HocevarDocument11 pagesBeggs HocevarAmanjot Bajwa100% (1)
- Growth Patterns in Subjects With Long and Short FacesDocument12 pagesGrowth Patterns in Subjects With Long and Short FacesMatt SanoudosNo ratings yet
- The Midline Diagnosis and Treatment ARTUROCAMACHODocument10 pagesThe Midline Diagnosis and Treatment ARTUROCAMACHOMiguel AngelNo ratings yet
- Topic - Maxillary Transverse DiscrepancyDocument42 pagesTopic - Maxillary Transverse Discrepancy王鈴鈞No ratings yet
- MBT Product CatalogDocument55 pagesMBT Product CatalogkirmaniNo ratings yet
- Cephalometrics Manual KrothDocument124 pagesCephalometrics Manual Krothimtiyazorthodontist100% (3)
- Late Expression of Class III MalocclusionDocument32 pagesLate Expression of Class III MalocclusionVikasini KondapakaNo ratings yet
- Severe Anterior Open Bite With Mandibular Retrusion Treated With Multiloop Edgewise Archwires and Microimplant Anchorage ComplementedDocument10 pagesSevere Anterior Open Bite With Mandibular Retrusion Treated With Multiloop Edgewise Archwires and Microimplant Anchorage ComplementedLedir Luciana Henley de AndradeNo ratings yet
- Diagnostic Imaginf of TMJ - A ReviewDocument4 pagesDiagnostic Imaginf of TMJ - A ReviewRhea RejiNo ratings yet
- The Role of Articulators in Orthodontics and Orthognatic SurgeryDocument5 pagesThe Role of Articulators in Orthodontics and Orthognatic SurgeryDr Shivam VermaNo ratings yet
- Eur J Orthod-2007-Björk-i82-8Document7 pagesEur J Orthod-2007-Björk-i82-8Tammy MuñozNo ratings yet
- Sunday, March 2, 2008: Important Orthodontic StudiesDocument6 pagesSunday, March 2, 2008: Important Orthodontic StudiesXnb HajiNo ratings yet
- American Journal QF Orthodontics: Facial Types Associated With Class II MalocclusionsDocument18 pagesAmerican Journal QF Orthodontics: Facial Types Associated With Class II MalocclusionsKhyati Gupta100% (1)
- The Retention Protocol 2017 Seminars in OrthodonticsDocument12 pagesThe Retention Protocol 2017 Seminars in Orthodonticsdruzair007No ratings yet
- Rotation of Jaws During Growth and Maturational and Aging ChangesDocument15 pagesRotation of Jaws During Growth and Maturational and Aging Changesshahzeb memon100% (1)
- Fudamentals of Biomechanics and Biomechanics of Levelling and Aligning Includes Biomechanics of Molar Control PDFDocument326 pagesFudamentals of Biomechanics and Biomechanics of Levelling and Aligning Includes Biomechanics of Molar Control PDFVioleta PajicNo ratings yet
- Miniscrew Assisted Rapid Palatal Expansion (Marpe) - ExpandingHorizons To Achieve An Optimum in Transverse Dimension A ReviewDocument15 pagesMiniscrew Assisted Rapid Palatal Expansion (Marpe) - ExpandingHorizons To Achieve An Optimum in Transverse Dimension A Reviewaa bbNo ratings yet
- Lillian B. MVSS, N.i) .S., XS.," kRORA, ILL: (1786) U-As OneDocument21 pagesLillian B. MVSS, N.i) .S., XS.," kRORA, ILL: (1786) U-As OneDiana Paola FontechaNo ratings yet
- 00 RWISO JOURNAL - Roth Williams International Society of PDFDocument61 pages00 RWISO JOURNAL - Roth Williams International Society of PDFanon_768201406No ratings yet
- Maintaining Clearly Defined Treatment Objectives:: Case StudyDocument5 pagesMaintaining Clearly Defined Treatment Objectives:: Case StudyAkylai IllanbekovaNo ratings yet
- Asymmetric Deep Bite With A Canted Occlusal Plane - A Case ReportDocument9 pagesAsymmetric Deep Bite With A Canted Occlusal Plane - A Case ReportIacominiGustavoNo ratings yet
- Class III and Fixed Functional ApplianceDocument51 pagesClass III and Fixed Functional ApplianceOsama GamilNo ratings yet
- Wjo 2 3 Kim1 PDFDocument11 pagesWjo 2 3 Kim1 PDFGoutam NookalaNo ratings yet
- Early Treatment of Class III Malocclusion With Modified Tandem Traction Bow Appliance and A Brief Literature Review 2247 2452.1000644Document5 pagesEarly Treatment of Class III Malocclusion With Modified Tandem Traction Bow Appliance and A Brief Literature Review 2247 2452.1000644kinayungNo ratings yet
- Biomechanics of Extra-Alveolar Mini-Implant Use in The Infrazygomatic Crest Area For Asymmetrical Correction of Class II Subdivision MalocclusionDocument9 pagesBiomechanics of Extra-Alveolar Mini-Implant Use in The Infrazygomatic Crest Area For Asymmetrical Correction of Class II Subdivision MalocclusionhabeebNo ratings yet
- Tweed1946 ARTICULO INGLES PDFDocument56 pagesTweed1946 ARTICULO INGLES PDFkNo ratings yet
- KimDocument12 pagesKimIvanna H. A.No ratings yet
- Growth QuesDocument8 pagesGrowth QuesShameer SFsNo ratings yet
- Facial Height Index: Case ReportDocument7 pagesFacial Height Index: Case ReportEstefania MontoyaNo ratings yet
- Manual Bio Art 4000sDocument22 pagesManual Bio Art 4000sArchitNo ratings yet
- JCO Roundtable Diagnosis and Treatment PlanningDocument23 pagesJCO Roundtable Diagnosis and Treatment PlanningRobert_Llamosa_9684100% (1)
- Retention and RelapseDocument59 pagesRetention and RelapseAshwin ThejaswiNo ratings yet
- Practical and Theoretical Seminar Of: Bioprogressive ScienceDocument5 pagesPractical and Theoretical Seminar Of: Bioprogressive SciencesaberNo ratings yet
- DR E. MenzelDocument4 pagesDR E. MenzelEtairia EogmeNo ratings yet
- Normal and Abnormal Growth of The Mandible. A Synthesis of Longitudinal Cephalometric Implant Studies Over A Period of 25 YearsDocument46 pagesNormal and Abnormal Growth of The Mandible. A Synthesis of Longitudinal Cephalometric Implant Studies Over A Period of 25 Yearsegray797No ratings yet
- Bomechancs in OrthodotnicsDocument74 pagesBomechancs in OrthodotnicsheycoolalexNo ratings yet
- Hydroxy Synthesis2010Document6 pagesHydroxy Synthesis2010ezfreshNo ratings yet
- HA Hydrogel 2013Document11 pagesHA Hydrogel 2013ezfreshNo ratings yet
- Interpreting TGA CurvesDocument20 pagesInterpreting TGA CurvesIoana MoldovanNo ratings yet
- CHAPTER (1) - Matter and ChangesDocument13 pagesCHAPTER (1) - Matter and ChangesezfreshNo ratings yet
- Open Bite CaseDocument10 pagesOpen Bite CaseezfreshNo ratings yet
- NUR341 - Assessment 2Document8 pagesNUR341 - Assessment 2KoechNo ratings yet
- Z-Tract Method of ImsDocument1 pageZ-Tract Method of Imsapi-242267470No ratings yet
- DextroseDocument1 pageDextroseamaliea234No ratings yet
- Head Lice: What Are Head Lice? Is Head Lice Contagious?Document2 pagesHead Lice: What Are Head Lice? Is Head Lice Contagious?Emmanuel WinfulNo ratings yet
- MK Sastry Nada Protocol The Grassroots TreatmentDocument12 pagesMK Sastry Nada Protocol The Grassroots Treatmentwilyanto yangNo ratings yet
- AS R A B A - W T C M C: Hort Eview of Cupuncture and Ronchial Sthma Estern AND Raditional Hinese Edicine OnceptsDocument11 pagesAS R A B A - W T C M C: Hort Eview of Cupuncture and Ronchial Sthma Estern AND Raditional Hinese Edicine Onceptsaprilia ciet cietNo ratings yet
- Pathology QuestionsDocument67 pagesPathology QuestionsRedentor MagdayaoNo ratings yet
- Medwatch 1Document26 pagesMedwatch 1Swaralipi GhoshNo ratings yet
- The Noble Foot Standing On A Firm Foundation: Shawneen SchmittDocument71 pagesThe Noble Foot Standing On A Firm Foundation: Shawneen SchmittCristina IuliaNo ratings yet
- Summary of Safety and Effectiveness Data: Her Option™ Uterine Cryoblation Therapy™ SystemDocument22 pagesSummary of Safety and Effectiveness Data: Her Option™ Uterine Cryoblation Therapy™ SystemIfeanyi UkachukwuNo ratings yet
- AcknowledgementDocument6 pagesAcknowledgementJustin VargheseNo ratings yet
- "Q" Umentation in Nursing: Recording For Quality Client CareDocument6 pages"Q" Umentation in Nursing: Recording For Quality Client CaresatmayaniNo ratings yet
- Bipolar Brochure English FINAL 150109 PDFDocument9 pagesBipolar Brochure English FINAL 150109 PDFIka M. HendrajayaNo ratings yet
- Hypnosis 0008 PDFDocument24 pagesHypnosis 0008 PDFalanNo ratings yet
- June, 2011Document24 pagesJune, 2011The Kohler VillagerNo ratings yet
- GASTROINSTINAL TRACT Robbins 8th EditionDocument4 pagesGASTROINSTINAL TRACT Robbins 8th EditionLim EricNo ratings yet
- Lymphedema TherapistDocument2 pagesLymphedema Therapistapi-78247176No ratings yet
- John Nash LifeDocument8 pagesJohn Nash Lifek_a1990No ratings yet
- Hyperurecimia and GoutDocument3 pagesHyperurecimia and GoutSunshine_Bacla_4275No ratings yet