Professional Documents
Culture Documents
Eastern Maine Healthcare Telemedicine
Uploaded by
tohcsOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Eastern Maine Healthcare Telemedicine
Uploaded by
tohcsCopyright:
Available Formats
TANDBERG CUSTOMER PROFILE ACCELERATING DECISION MAKING
EASTERN MAINE HEALTHCARE SYSTEMS
Rural patients across Maine now have access to critical care specialists, thanks to video communications from TANDBERG.
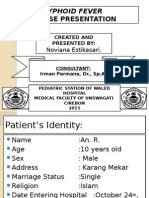
U.S. Commerce Secretary Gary Locke (left) and Eastern Maine Medical Center Dr. Rafael Grossman talk to Dr. Joe Babbitt (on screen) at the Blue Hill Hospital using the video conferencing technology which currently connects EMMC with 11 other hospitals. (Bangor Daily News/Bridget Brown)
CHALLENGE Serving nine counties in Maine, Eastern Maine Healthcare Systems (EMHS) is committed to ensuring that citizens in all areas of the state receive the same access to high-quality healthcare. However, with a shortage of medical professionals in the states rural areas, citizens must drive up to three hours one way to receive a full range of primary and specialty care services. In addition, emergency care often necessitates that patients be transferred by ambulance and/or helicopter from the seven EMHS affiliate hospitals to the Eastern Maine Medical Center (EMMC) in Bangor, where the majority of the states specialists practice. In 2006, EMHS received two telemedicine grants, followed by a third telemedicine grant in 2007. Having used video conferencing equipment from a variety of vendors since 1996 for education and meetings, EMHS chose TANDBERG equipment for the telemedicine initiative. Now, EMHS provides rural patients with access to critical care and other specialists, thus reducing helicopter and long-distance ambulance transports and delivering significant cost savings to medical facilities and patients alike.
P. 1/3
07 27 2010
TANDBERG CUSTOMER PROFILE ACCELERATING DECISION MAKING
SOLUTION According to Wanda Pacifici, Telemedicine Program Manager at EMMC, When we first started with video conferencing, it was used mostly for education and meetings. Over time it grew, and we started offering CME (continuing medical education) programs, which became quite popular, not only among our affiliated hospitals, but other hospitals as well. We put our first TANDBERG endpoint in our main hospital and the second one in our psychiatric hospital, and gradually we put endpoints in all our affiliate hospitals. And, once we received the telemedicine grants, it just exploded. Upon learning of the telemedicine grants, EMHS issued a request for proposal to purchase a new multipoint control unit (MCU). As Pacifici recalls, Five vendors presented, and TANDBERG just blew everybody out the door. In addition to the existing TANDBERG endpoints at each of our eight hospitals, we purchased the TANDBERG MCU, the TANDBERG Management Suite (TMS), the TANDBERG Content Server (TCS) and the TANDBERG Border Controller. We also put endpoints in the homes of three pediatric intensive care specialists and one psychiatrist. As a result, EMHS is well equipped to deliver telemedicine capabilities across a number of specialties, including: Emergency/Trauma Pediatrics Diabetes Endocrinology Oncology Psychiatry Rehabilitation In addition, says Pacifici, We are starting a Telestroke program, as well as another program that enables doctors to perform follow-up visits after surgeries. And, we have a psychiatrist who connects to our county jail. Our primary goal, she continues, is to reduce patient transfers by ambulance and helicopter by allowing rural patients to go to their local hospitals for specialty care. In our third year, we are seeing the number of telemedicine encounters increasing across all specialties.
We put our first TANDBERG endpoint in our main hospital and the second one in our psychiatric hospital, and gradually we put endpoints in all of our affiliate hospitals. And, once we received the telemedicine grants, it just exploded.
WANDA PACIFICI, TELEMEDICINE PROGRAM MANAGER AT EMMC
P. 2/3
07 27 2010
TANDBERG CUSTOMER PROFILE ACCELERATING DECISION MAKING
RESULTS Since the telemedicine program started in March 2007, there have been more than 5,330 telemedicine encounters across all specialties. Estimating a rate of 55 cents per mile, that translates into almost $163,000 of savings for patients alone. The savings realized from reducing air and ground patient transfers are much harder to quantify, as EMHS currently collects only the data for unnecessary and inappropriate modes of transfer for emergency cases. However, with each air transport costing approximately $4,800 and ground transport costing approximately $800, the savings to date in the emergency category arguably exceeds $110,000. And, as the telemedicine initiative continues to grow, so too will cost savings. Meanwhile, EMHS is seeing several additional benefits, from reduced staff travel for education and meetings (thus eliminating travel reimbursement) to faster time to-treatment for critically ill patients. The physicians really like video conferencing, Pacifici notes, and the patients all seem to like it, especially those who are further away. They dont want to drive three hours for an appointment its time away from work and family. When a patient does have to be transferred to the EMMC, she continues, the staff at the rural hospital is able to reconnect with us to follow the patients progress and learn from our specialists. Pacifici also provides a heart-warming example of how video conferencing can keep patients from missing important events. We had a patient in the ICU whose son was graduating. She was very upset that she was going to miss his graduation. We happened at that time to have a home healthcare unit in that area, so they took the video conferencing unit over to the school, we connected the patient from here, and she was able to see her son graduate. The biggest benefit of video conferencing, Pacifici concludes, is giving rural patients access to critical care specialists. Video conferencing also saves time for physicians who once had to drive 60 to 90 minutes to do clinics in other hospitals. And, oncologists can perform monthly follow-ups with their rural patients, saving time and addressing the shortage of those physicians in Maine. It all adds up to better patient care for less, she says.
The biggest benefit of video conferencing is giving rural patients access to critical care specialists.
WANDA PACIFICI
P. 3/3
07 27 2010
www.TANDBERG.com
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Tubigon Emergency Response Service and Support Unit (T.E.R.S.S.U)Document81 pagesTubigon Emergency Response Service and Support Unit (T.E.R.S.S.U)Gina BoligaoNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Drug Therapy ProblemDocument19 pagesDrug Therapy ProblemAulia NorfiantikaNo ratings yet
- Putney Rehab Centre TimetableDocument2 pagesPutney Rehab Centre Timetableapi-280584977No ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- DIGEST CIR Vs Philippine Healthcare ProvidersDocument14 pagesDIGEST CIR Vs Philippine Healthcare ProvidersEthel Joi Manalac MendozaNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- KSSHP Strategiakuva ENG - V01Document2 pagesKSSHP Strategiakuva ENG - V01Shahnaz NawazNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Salud Familiar - APS y Seguridad Social: Marco Aurelio Sosa GiraldoDocument17 pagesSalud Familiar - APS y Seguridad Social: Marco Aurelio Sosa GiraldoOsomolarNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Screening Epidemiology: Ansariadi, PHDDocument29 pagesScreening Epidemiology: Ansariadi, PHDjilyana adam0% (1)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Final Speech OutlineDocument3 pagesFinal Speech Outlineapi-300455857No ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- End of Term Assessment FormDocument6 pagesEnd of Term Assessment FormhappyhappylandNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Test Bank For Delivering Health Care in America 6th Ed Test BankDocument8 pagesTest Bank For Delivering Health Care in America 6th Ed Test Banktestbankloo0% (1)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Summer Internship ProjectDocument12 pagesSummer Internship ProjectBarun MalakarNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- ACC 2023 ResumenDocument7 pagesACC 2023 ResumenJuan Carlos FloresNo ratings yet
- Strategic Thinking and Hospital Performance Versi 2Document171 pagesStrategic Thinking and Hospital Performance Versi 2ismail aji100% (1)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Typhoid Case PresentationDocument17 pagesTyphoid Case PresentationAbdulMazidZabir0% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Nursing Ethics Paper 1Document13 pagesNursing Ethics Paper 1api-214213767No ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- DR Suman Thapa - Challenges of Glaucome Care in The HimalayasDocument54 pagesDR Suman Thapa - Challenges of Glaucome Care in The HimalayasAn Da100% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Toiletries/Cosmetics/ Personal Comfort or Convenience Items: SNO List of Expenses Excluded ("Non-Medical") SuggestionsDocument5 pagesToiletries/Cosmetics/ Personal Comfort or Convenience Items: SNO List of Expenses Excluded ("Non-Medical") SuggestionsnagarjunaNo ratings yet
- Designer DrugsDocument4 pagesDesigner DrugsShams KhalidNo ratings yet
- HSA 6004101-008-17-03 - 43 FSN - RedactedDocument16 pagesHSA 6004101-008-17-03 - 43 FSN - RedactedF CPNo ratings yet
- Health Psychology - Week 2 - Class 1Document12 pagesHealth Psychology - Week 2 - Class 1Behroze khalilNo ratings yet
- Hes 008 - Sas 22Document1 pageHes 008 - Sas 22Juliannah ColinaresNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Bioethics: Beneficence / Non-MaleficenceDocument35 pagesBioethics: Beneficence / Non-MaleficenceBheru LalNo ratings yet
- Topic: What Are Some of The Benefits of Modern Technology For Health Care Services?Document2 pagesTopic: What Are Some of The Benefits of Modern Technology For Health Care Services?asadNo ratings yet
- Li V Sps. SolimanDocument4 pagesLi V Sps. SolimanTriccie MangueraNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Gajanan Chame CV UpdatedDocument3 pagesGajanan Chame CV UpdatedShivanand MuleNo ratings yet
- Participate IN Various Programmes VasectomyDocument6 pagesParticipate IN Various Programmes Vasectomyvenkat krishnanNo ratings yet
- The Pharmaceutical Industry and The Future of Drug DevelopmentDocument42 pagesThe Pharmaceutical Industry and The Future of Drug Developmentgnk9No ratings yet
- Thesis On Health Care FinancingDocument5 pagesThesis On Health Care Financingchristinawestcharleston100% (2)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- NIP-MOP-Booklet 5Document22 pagesNIP-MOP-Booklet 5Kathryn Jan DomingoNo ratings yet
- Chief Executive Officer in Brentwood TN Resume Gary FergusonDocument3 pagesChief Executive Officer in Brentwood TN Resume Gary FergusonGaryFerguson1No ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)