Professional Documents
Culture Documents
Psychexam2 Cas
Uploaded by
Antonio Abreu Jr.Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
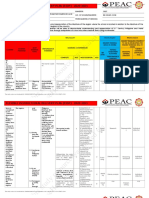
Psychexam2 Cas
Uploaded by
Antonio Abreu Jr.Copyright:
Available Formats
Psych Exam 2 Study Guide
Care and management of the Manic Patient:
(6) Mania: Alteration in mood expressed by feelings of elation, inflated self-esteem, grandiosity, hyperactivity, and accelerated thinking and speaking. 3 Manic Stages: hypomania, acute mania, & delirious mania: Hypomania: disturbance is not sufficiently severe to cause marked impairment MOOD: cheerful & expansive. irritability when wishes/desires are unmet. person is volatile & fluctuating. COGNITION & PERCEPTION: perceptions of self are exalted ( great worth & ability). person is easily distracted by irrelevant stimuli. ACTIVITY & BEHAVIOR: increased motor activity. extroverted & sociable. increased libido. anorexia & weight loss. engage in inappropriate behaviors. Acute Mania: impairment in functioning and require hospitalization. MOOD: euphoria & elation. "high". easily changes to irritability and anger. COGNITION & PERCEPTION: rapid thinking, flight of ideas. accelerated & pressured speech. hallucination & delusions. ACTIVITY & BEHAVIOR: sexual interest increased. poor impulse control. excessive spending. manipulate others to carry out their wishes. no need for sleep. Delirious Mania: severe clouding of consciousness & increased s/s of acute mania. MOOD: feelings of despair, changes to, ecstasy or irritability. panic anxiety. COGNITION & PERCEPTION: clouding of consciousness. confusion, disorientation, stupor. delusions & audible & visual hallucinations. easily distractible & incoherent. ACTIVITY & BEHAVIOR: agitated, purposeless movements. Signs & Symptoms: -Euphoric/expansive mood: Extremely happy, silly, or giddy. -Irritable mood: Hostility and rage, often over trivial matters. -Grandiosity: Believes abilities to be better than everyone elses. -Decreased need for sleep: May sleep for only 4 or 5 hours per night and wake up feeling rested. -Pressured speech: Loud, intrusive, difficult to interrupt. -Racing thoughts: Rapid change of topics -Distractibility: Unable to focus on school lessons -Increase in goal-directed activity/psychomotor agitation: Activities become obsessive. -Increased psychomotor agitation. -Excessive involvement in pleasurable or risky activities: Exhibits behavior that has an erotic, pleasure-seeking quality about it. -Psychosis: May experience hallucinations and delusions. -Suicidally: May exhibit suicidal behavior during a depressed or mixed episode or when psychotic. Treatment: Individual psychotherapy. Group therapy. Family therapy. Cognitive therapy. Electroconvulsive Therapy (ECT) Psychopharmacology: Lithium: Side Effects: drowsiness, dizziness, headache, dry mouth, thirst, GI upset, fine hand tremors, pulse irregularities, polyuria, weight gain. Lithium Toxicity: therapeutic levels: acute: 1.0-1.5. maintenance: 0.6-1.2. levels should be drawn weekly
during acute, monthly during maintenance. S/S: ataxia, blurred vision, diarrhea, N/V, tinnitus. Anticonvulsants: Side Effects: Tegretol: ataxia, blood dyscrasia, dependance/tolerance. Klonopin: ataxia, N/V, blood dyscrasia Depakote: (levels: 50-100) dizziness, weight gain, N/V, prolonged bleeding time. Lamictal: life-threatening skin rash, ataxia, photosensitivity, headache Neurontin: ataxia, nystagmus, tremor Trileptal: headache, ataxia, somnolence, N/V Topamax: dizziness, ataxia, impaired concentration, nervousness, vision changes, weight loss, decrease effectiveness of oral birth control. Antipsychotics: OLD: chlorpromazine. NEW (atypical): olanzapine, risperidone, aripiprazole, ziprasidone, quetipine. Nursing Interventions: Risk for violence: maintain low level of stimuli. Observes clients behavior frequently. Remove all dangerous objects from the client's environment. Intervene at first sign of increased anxiety. maintain a calm attitude toward the client. Use of mechanical restraints if necessary (check q15 min). Impaired Social Interaction: set limits on manipulative behaviors. Do not argue, bargain, or try to reason with the pt; merely state the limits & expectations (ppl with mania can be charming to fulfill their desires). Provide positive reinforcement for non-manipulative behaviors. help pt recognize that they are responsible for their own behaviors. help pt identify positive aspects about themselves.
Care and management of the Depressed Patient:(9)
Depression: alteration in mood with feelings of sadness, despair, pessimism, loss of interest in usual activities, and somatic symptoms. changes in sleep & eating patterns. Adolescence: harder to recognize in kids. S/S may be perceived as normal emotional stressors of growing up. S/S: anger, aggressiveness, running away, delinquency, social withdrawal, sexual acting out, substance abuse, restlessness, apathy, loss of self-esteem, sleep & eating problems, psychosomatic complaints. 4 Stages of Depression: EX: Transient, Mild, Moderate, Severe Transient: Life's everyday disappointments. sadness, having the "blues". some crying possible. tired & listless. Mild Depression: EX: Normal grieving response. denial of feelings, anger, anxiety, guilt, helplessness, sadness, tearfulness, agitation, withdrawal, preoccupation with loss, ambivalence, anorexia/over eating, & physical s/s r/t loss of significant other. Moderate Depression: EX: Dysthymic disorder. feelings of sadness, helplessness, gloomy, difficult to experience pleasure, slowed physical movements (psychomotor retardation), social isolation, self-destructive behavior, decreased personal hygiene, retarded thinking process, anorexia/over-eating, sleep disturbances, low energy levels, fatigue Severe Depression: intensified symptoms of moderate. EX: major depressive disorder & bipolar depression. feelings of total despair, hopelessness, flat affect, devoid of emotion, emptiness, sadness, loneliness. severe psychomotor retardation. non existent communication, delusional thinking & talking, no hygiene, confusion, indecisiveness, selfblame. thoughts of suicide (may not have energy to go through with it but strong thoughts are still present). general slow-down of entire body, decreased libido, weight & sleep problems.
Treatment: Individual psychotherapy. Group therapy. Family therapy. Cognitive therapy. Electroconvulsive Therapy (ECT). Transcranial Magnetic Stimulation: The introduction of short pulses of magnetic energy to stimulate nerve cells in the brain. Light Therapy: Used to treat seasonal affective disorder. Also used as an adjunct therapy in chronic major depressive disorder or dysthymia with seasonal exacerbations Psychopharm: all meds should be tapered gradually to prevent withdrawl symptoms. SSRIs: (inhibit CNS uptake of serotonin) 1st line, better than MAOIs & TCAs. Celexa, Lexapro, Prozac, Sarafem, Luvox, Zoloft. Side Effects: headache, insomnia, N/V, anorexia, diarrhea, dry mouth, sex dysfunction. Serotonin Syndrome: rare. can occur if taken with other meds that increase serotonin (MAOIs, etc). symptoms: confusion, agitation, tachy, HTN, abd pain, myoclonus, muscle rigidity, fever, sweating, tremor. treatment: stop other drugs, cooling blankets, meds. Heterocyclics: inhibit re-uptake of norepi & serotonin. Wellbutrin (also inhibits reuptake of dopamine). Side Effects: drowsiness, fatigue, dry mouth, headache, constipation, N/V. risk of seizures. SNRIs: inhibit serotonin & norepi reuptake. 2nd line. Effexor & Cymbalta. Side Effects: N/V, dizziness, insomnia, HTN, dry mouth, constipation, sex dysfunction. TCAs: 2nd or 3rd line. Anafranil, Norpramine, Sinequn, Tofranil, Aventyl, Pamelor, Vivactil, Surmontil. Side Effects: anticholinergic, cardiovascular, CNS, weight gain, photosensitivity, sex dysfunction. MAOIs: 3rd/last line, bad side-effect profile. Marplan, Nardil, Parnate, Emsam. Side Effects: dizziness, headache, insomnia, dry mouth, blurred vision, sex dysfunction, cardiac. Hypertensive crisis: r/t ingestion of foods/drugs with TYRAMINE. begins 2 hr after ingestion. S/S: occipital/temporal headache, photophobia, feeling of choking, palpitations, feeling of dread. Nursing Interventions: RIsk for Suicide: ask the pt directly about suicide (risk increased if pt has plan). create a safe environment (remove all potentially harmful objects). form a short-term contract with pt not to harm self during time period and that he/she will seek help if thoughts emerge. maintain close observation. special care in giving meds. make rounds at frequent, irregular intervals. encourage verbalization of honest feelings. express angry feelings. community resources. orient pt to reality. IMPORTANT: spend time with pt. Complicated Grieving: determine the grief stage pt is in. develop trusting relationship. encourage pt to express anger. physical activity to release anger. tell pt crying is ok. encourage pt to seek spiritual support and attend a support group. Low-self esteem/self care deficit: spend time with pt and be accepting. promote attendance in therapy groups. encourage pt to recognize ares of change and provide assistance toward this effort. teach assentiveness techniques. teach effective communication. encourage independence in the performance of ADLs. keep strict records of food/fluid intake. show pt how to person activities in which he/she is having problems with.
Care and management of the Suicidal Patient:
Risk Factors: AGE: older than 50. adolescents = high risk. GENDER: males succeed more, women try more
(6)
ETHNICITY: Caucasians MARITAL STATUS: single, divorces, widowed SOCIOECONOMIC STATUS: highest & lowest classes OCCUPATION: health care & business executives METHOD: firearms RELIGION: ppl with no religious group FAMILY HX: high risk = family hx of suicide. Predisposing disroders/factors & Symptoms: disorders: mood disorders (bipolar & major depression), substance use disorders, anxiety disorders, schizo, borderline & antisocial personality disorders, & ppl with terminal illness. factors: internalized anger, depression, desperation, guilt, hx of aggression, shame, developmental stressors, sociological influences, genetics, & neuro-chemical factors. Interventions (following discharge): person SHOULD NOT be left alone. establish nosuicide contract. have family & friends make sure home is safe and free of dangerous items. appts daily or weekly. establish rapport & promote trusting relationship. accept pt feelings in a nonjudgemental manner. discuss current crisis situation in pt's life (say: "you are incorrect in your belief that suicide is the only and best solution to your problem. There are alternative and they are good. What is more, you will be alive to test them"). antidepressants. -Be direct. Talk openly & matter-of-factly about suicide. Listen actively & encourage expression of feelings, including anger.
Care and management of the patient with an anxiety disorder
(15)
Panic Disorder: characterized by recurrent panic attacks, onset is unpredictable, and
manifested by intense apprehension, fear, terror, feelings of impending doom and physical discomfort. Symptoms come unexpectantly, not brought on by exposure (phobia). -At least four of the following symptoms must be present to identify the presence of a panic attack. When fewer than four symptoms are present, the individual is diagnosed as having limited symptom attack. Palpitations, pounding heart, or accelerated HR Sweating Trembling or shaking Sensations of SOB or smothering Feeling of choking Chest pain or discomfort Nausea or abd distress Feeling dizzy, unsteady, lightheaded, or faint Derealization (feelings of unreality) or depersonalization (being detached from oneself Feel of losing control or going crazy Fear of dying Paresthesias (numbness or tingling sensations) Chills or hot flashes Panic Disorder with Agoraphobia: a fear of being in places or situations from which escape might be difficult (or embarrassing) or in which help might not be available in the event that a panic attack should occur.
Phobias: fear cued by the presence of anticipation of a specific object or situation;
exposure provokes and immediate anxiety response or panic attack even though pt know that fear is excessive or unreasonable. Types of Phobias: animal-type. natural environment type. blood-injection type. situation type other type. Agoraphobia w/o panic disorder: fear of being in places or situation from which escape might be difficult or in which help might not be available. onset in 20-30s, equal to women & men. pt is unable to leave home without friend or family member. Social Phobia: excessive fear of situations in which a person might do something embarrassing or be evaluated negatively by others. pt has extreme concern about being exposed to possible scrutiny by others and fears social/performance situations. Exposure to the phobic situation usually results in feelings of panic anxiety, with sweating, tachy, and dyspnea. onset in childhood & adolescence. Specific Phobia: marked, persistent and excessive or unreasonable fear when in the presence of, or when anticipating an encounter with, a specific object or situation. Exposure to the phobic stimulus produces overwhelming symptoms of panic: palpitations, sweating, dizziness, difficulty breathing. Psychopharmacology for phobic disorders Anxiolytics: Benzodiazaepines have been successful in the tx of social phobia. Controlled studies have shown the efficacy of alprazolam and clonazepam in reducing symptoms of social anxiety. They are both well tolerated an have a rapid onset of action. However, because of their potential for abuse and dependence, they are not considered the first line choice of tx for social phobia. Antidepressants: The tricyclic imipramine and the MAOI phenelzine have been effective in diminishing symptoms of agoraphobia and social phobia. SSRIs have become the first drug of chouce for social phobia. Specific phobias are generally not txd with medication unless panic attacks accompany the phobia. Treatment modalities: Individual psychotherapy: most clients experience a marked lessening of anxiety when given the opportunity to discuss their difficulties with a concerned and sympathetic therapist. It focuses on helping patients understand the hypothesized unconscious meaning of the anxiety, the symbolism of the avoided situation, the need to repress impulses, and the secondary gains of the symptoms. The psychotherapist also can use logical and rational explanations to increase the clients understanding about various situations that create anxiety in his or her life. Psycho educational info may also be presented in individual psychotherapy. Cognitive therapy: the cognitive model relates how individuals respond in stressful situations to their subjective cognitive appraisal of the event. Anxiety is experienced when the cognitive appraisals one of danger with which the individual perceives that he or she is unable to cope. Impaired cognition can contribute to anxiety disorders when the individuals appraisals are chronically negative. Automatic negative appraisals provoke self-doubts, negative evals, and negative predictions. Anxiety is maintained by this dysfunctional appraisal of a situation. Behavior therapy: two common forms are systematic desensitization and implosion therapy *flooding). They are commonly used to treat clients with phobias and to modify stereotyped behavior of clients with PTSD. They have also been shown to be effective in a variety of other anxiety producing situations. Systematic desensitization: the client is gradually exposed to the phobic
stimulus, either in a real or imaginative situation. The concept is based on behavioral conditioning principles. Emphasis is placed on reciprocal inhibition or counterconditioning. Implosion therapy (flooding): therapeutic process in which the client must imagine situations or participate in real-life situations that he or she finds extremely frightening, for a prolonged period of time. Relaxation training is not part of this technique. Plenty of time must be allowed for these sessions b/c brief periods may be ineffective or even harmful. A session is terminated when the client responds with considerably less anxiety than at the beginning of the session.
Somatoform Disroders: Somatization Disorder:
(somatization disorder, pain disorder, hypochondriasis, conversion disorder, body dismorphic disorder) syndrome of multiple somatic symptoms that cannot be explained medically and are associated with psychological distress and long-term seeking of assistance from healthcare professionals. Periods of remission & exacerbation. -somatization: ( psychological needs are expressed in the form of physical symptoms). Signs & Symptoms: identified as pain (in @ least 4 areas), GI symptoms, sexual symptoms, & symptoms suggestive of neurological condition. Anxiety & depression. drug abuse is common complication. Nursing Interventions: -recognize and accept that the physical complain is real to the pt. -identify gains that the physical symptoms are providing for the pt. -initially, fulfill the pt's most urgent dependancy needs. -encourage the pt to verbalize fears and anxieties. -Help pt recognize that the physical symptoms occur & are exacerbated by specific stressors. -have pt keep a diary of appearance, duration, and intensity of physical pain. -help pt find ways to achieve recognition from others without resorting to the pain. -provide instruction in relaxation techniques and assertiveness skills. Treatment: -Antidepressants: TCAs, SNRIs -Anticonvulsants: Dilantin, Tegregol, Klonopin
Pain Disorder: severe and prolonged pain that causes clinically significant distress
or impairment in social, occupational, or other important areas of functioning. Pain is correlated with stressful event. Characteristic behaviors: frequent visits to DR office & excessive use of analgesics. symptoms of depression are common -primary gain: appearance of the pain enables the pt to avoid some unpleasant activity. -secondary gain: the pain promotes emotional support or attention that the pt might not otherwise receive otherwise.
Hypochondriasis: unrealistic or inaccurate interpretation of physical symptoms or
sensations leading to preoccupation and disabling fear of having serious disease. pt is totally aware with entire body and their response to small changes is unrealistic and exaggerated. "doctor shopping". anxiety & depression are common.
Conversion Disorder: loss of or change in body function resulting from a
psychological conflict, the physical symptoms of which cannot be explained in terms of
any known medical disorder or pathophysiological mechanism. Pt are unaware of the psychological basis and are therefore unable to control their symptoms. -S/S:must be explained by psychological factors and may be evidenced by primary & secondary gains. symptoms appear suddenly and pt has lack of concern (la bell indifference). Symptoms resolve spontaneously within a few weeks. The symptom usually occurs after a situation that produces extreme psychological stress for the individual. -Primary: enable the individual to avoid difficult situations or unpleasant activities about which he or she is anxious. -Secondary: obtain attention or support that might not otherwise be forthcoming. Nursing Interventions: -identify primary & secondary gains that the physical symptom is providing for the pt. -do not focus on the disability. -maintain nonjudgemental attitude. -do not allow the pt to use the disability as a manipulative tool to avoid participating in therapeutic activities. -encourage pt to verbalize fears. -help pt identify coping mechanisms. -give positive reinforcement.
Body Dismorphic Disorder:
exaggerated belief that the body is deformed or defective in some specific way. Social & occupational impairments. Symptoms of depression & OCD are present.
Dissociative Disorders:
(dissociative identity disorder, dissociative amnesia, depersonalization disorder, dissociative fugue)
Dissociative Identity Disorder: multiple personality disorder. characterized
by the existence of two or more personalities in a single individual. only one personality is evident at any given moment. Transition from 1 personality to another is usually sudden, dramatic, and precipitated by stress. Signs & Symptoms: before therapy, original personality does not know other personalities; the sub-personalities are usually aware of one another. Sub-personalities are usually opposite of original. Amnesia occurs when another personality is dominant but the personality dominant retains awareness and remembers past. Nursing Interventions: -nurse must develop trusting relationship with the original personality. -help the pt understand that existence of sub-personalities. -help pt identify stressful situations that precipitate transition from one personality to another. -Use nursing interventions to deal with maladaptive behaviors associated with individual sub-personalities (1 personality is suicidal = suicide precautions. if another is physically aggressive = precautions to protect person and HCP). -Possibly seek assistance from another personality (strong willed personality may help control behaviors of the "suicidal" personality). -help sub-personalities understand that their "being" will not be destroyed, but rather integrated into a unified identity within the individual. -provide support during disclosure of painful experiences. Treatment:
goal of therapy = optimize the pt's function and potential. goal of Integration (blending all personalities) = considered desirable. -Intensive long term psychotherapy. They must re-experience the abuse that caused their illness (abreaction). -During therapy each personality is explored and encouraged to become aware of the others across previous amnesic barriers.
Care and management of the patient undergoing ECT: presentation: (3)
ECT: induction of a grand mal (generalized) seizure through the application of electrical current to the brain. treatments last 10-15 seconds, administered every other day (3x/week). -treatment alternative for ppl with depression, mania, schizo and don't respond to other therapy. -contraindicated for ppl with ICP. CV disease = high risk for complications. -Side effects: memory loss, confusion. possible/rare: permanent memory loss, brain, damage, death. -During tx: meds given: short-acting anesthetic (Pentothal) & muscle relaxant (Anectine) given. -Anectine: paralyzes resp muscles, so pt is oxygenated with pure O2 during and after. Nursing Interventions: Before treatment: -Dr. must obtain informed consent & signed permission form is on chart. -most recent labs & ECG & xray are all available. -1 hr before: vital signs. have pt void, remove dentures, eyeglasses, contacts, jewelry, hairpins. -30 mins before: admin pretreatment meds (atropine sulfate or Robinul), given to decrease secretions (prevent aspiration) and counteract effects of vagal stimulation (bradycardia). -Stay with pt to help ease fears. During treatment: -place pt in supine position. -ensure patency of airway. suction is necessary. assist with oxygenation. -provide support to pt arm's & legs -observe and record types of movements. Post Treatment: -VS q 15mins for first hour, pt remains in bed. -position pt on side, to prevent aspiration -orient pt to time & place. describe what has occurred. -reassure that memory loss is only temporary and will come back. -stay with pt until they are fully awake. allow them to express fears -provide highly structured schedule for pt in order to reduce confusion.
Psychopharmacology (11) Anti-Anxiety:
Treatment for: anxiety disorders, acute alcohol withdrawal, muscle spams, convulsive disorders, status epilepticus, preoperative sedation.
Mechanism of action: CNS depression. **exception: BuSpar: does not depress CNS Side Effects & Nursing Interventions: -Drowsiness, confusion: do not drive or operate machinery -Tolerance, dependance: do not quit the drug abruptly. -ability to potentiate the effects of other CNS depressants: do not drink alcohol or take other meds that depress the CNS -Possibility of aggravating symptoms in depressed person. -Orthostatic hypotension: pt rise slowly. nurse take BP lysing and standing -Paradoxical excitement: (opposite symptoms) withhold drug and notify HCP -Dry mouth -N/V: take drug with food -Delayed onset (busprione only):ensure pt understands lag time of 10 days - 2 weeks. Not recommended for PRN.
Anti-Depressants:
Treatment for: dysrhythmic disorder, major depression (with psychotic symptoms), alcoholism, schizo, mental retardation, bipolar (depressive phase), depression from anxiety. Mechanism of action: increase concentration of norepi, serotonin, and/or dopamine in the body. Side Effects & Nursing Interventions: All chemical classes: -Dry mouth -Sedation: give drug at bedtime. pt not to drive or use machinery. -Nausea -Discontinuation syndrome: do not withdraw abruptly, meds should be tapered off. Tricyclics: -Blurred vision: pt not to drive -Constipation -Urinary retention: monitor I&O -Orthostatic hypotension: monitor BP lying and standing -Reduction of seizure threshold: seizure precautions. Wellbutrin: only 150mg doses. -Tachycardia, arrhythmia -Photosensitive -Weight gain SSRIs: -Insomnia, agitation: take dose in early morning. avoid caffeine. -headache -weight loss -sexual dysfunction -Serotonin Syndrome: (occur when multiple drugs increase serotonin) s/s: changes in mental status, restlessness, myoclonus, hyperrflexia, tachycardia, labile BP, diaphoresis, shivering, tremors. Interventions: discontinue other meds. monitor VS, provide safety measures, cooling blankets, monitor I&O. MAOIs: -Hypertensive Crisis: (when tyramine is consumed). S/S: occipital headache, palpitations, N/V, Fever, sweating, increased BP, chest pain, coma. Interventions: discontinue drug. monitor VS. antiHTN meds. external cooling measures. -Application site reactions: rash Miscellaneous: -Priapism (trazodone): prolonged/inappropriate penis erection. withhold med, &
notify HCP. -Hepatic failure (nefazodone): advise pt of s/s of liver dysfunction.
Mood-Stabilizers:
Lithium: Lithium Toxicity: therapeutic ranges: Acute: 1.0-1.5 Maintenance: 06.-1.2. Lithium levels should be monitored once or twice a week during maintenance and prior to administration during acute. if levels are above, hold med and notify HCP. S/S: blurred vision, tinnitus, N/V, diarrhea, increase dilute urine, tremors, muscle rigidity, confusion, seizures, coma, MI, cardiovascular collapse. -Education/Interventions: take med on regular basis. do not drive or operate machines. monitor Na & H2O (2500-3000mL) intake. use contraception. be aware of side effects Anticonvulsants: -Education/Interventions: don't abrutly stop meds. don't drive. avoid alcohol. report symptoms to HCP: skin rash, unusal bleeding, bruising, sore throat, fever, malaise, dark uine, yellow skin/eyes. Calcium Channel Blocker: -Education/Interventions: meds with meals. caution with driving. don't abruptly stop drug. rise slowly from sitting to standing position.
Anti-Psychotics:
Typical Meds: phenothiazines, haloperidol, loxapine, molindone, pimozide, thiothixene. Atypical Meds: aripiprazole, clozapine, olanzapine, quetiapine, risperidone, paliperidone, ziprasidone. Mechanism of Action: exact mechanism is unknown. blocks post-synaptic dopamine receptors. Side Effects/Interventions: -Anticholinergic effects: dry mouth, blurred vision, constipation, urinary retention. -Nausea/GI upset: take med with food. -Skin rash -Sedation: take drug at bedtime -Orthostatic hypotension -Photosensitivity: sunblock -Hormonal effects: decreased libido. amenorrhea (don't stop contraception bc ovulation still occurs). weight gain. -ECG changes. -Reduction of seizure threshold: (Clozaril) -Agranulocytosis: (typical) observe for symptoms of sore throat, fever, malaise. -Hyper-salivation (clozapine) -Extrapyramidal: pseudoparkinsonism, akinesia, akathisia, dystonia, oculogyric crisis. -Tardive dyskinesia: bizarre facial and tongue movements, stiff neck, & difficulty swallowing. withdrawal drug at first sign. possibly irreversible. -Neuroleptic malignant syndrome (NMS): discontinue med immediately. -Hyperglycemia & diabetes -Increased risk of mortality.
Benzodiapzepines:
Mechanism of action: (mimics GABA) bind to specific receptor sites and enhance the
inhibitory effect of GABA. Advantages: DOES NOT: suppress REM sleep
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Summary of 2018 Dental Exam Requirements: Required SectionsDocument13 pagesSummary of 2018 Dental Exam Requirements: Required Sectionsjentothesky100% (1)
- Ow Pakistan Offers Quota For Kashmiri Students Geelani S Resignation From HurriyatDocument21 pagesOw Pakistan Offers Quota For Kashmiri Students Geelani S Resignation From HurriyatABHINAV DEWALIYANo ratings yet
- Sing A Joyful Song - PREVIEWDocument5 pagesSing A Joyful Song - PREVIEWRonilo, Jr. CalunodNo ratings yet
- ALEXANDER, Jeffrey C. & SZTOMPKA, Piotr. Rethinking ProgressDocument281 pagesALEXANDER, Jeffrey C. & SZTOMPKA, Piotr. Rethinking ProgressJuan NiemesNo ratings yet
- Prel - Writing QP - Test 2Document3 pagesPrel - Writing QP - Test 2Rocio FernandezNo ratings yet
- Role of Teachers in Imparting Value EducationDocument3 pagesRole of Teachers in Imparting Value EducationMehebub AlamNo ratings yet
- Character Development Presentation PDFDocument16 pagesCharacter Development Presentation PDFapi-528422948No ratings yet
- Analyzing & Reporting Upon Workshop Evaluation Forms ResultsDocument3 pagesAnalyzing & Reporting Upon Workshop Evaluation Forms ResultsFebe NievaNo ratings yet
- Ten Health Benefits of Getting A Good Nights SleepDocument5 pagesTen Health Benefits of Getting A Good Nights SleepAngelica CiubalNo ratings yet
- Egyptian ArabicDocument2 pagesEgyptian ArabicIyesusgetanewNo ratings yet
- Learning Outcomes MathematicsDocument122 pagesLearning Outcomes MathematicsBHOLA MISHRANo ratings yet
- RBSK Resource MaterialDocument290 pagesRBSK Resource MaterialSachin ParmarNo ratings yet
- Lesson PlanDocument8 pagesLesson PlanMarvi Joyce Caballero100% (1)
- Degraded words in Fran Meneses' YouTube blog (Восстановлен)Document32 pagesDegraded words in Fran Meneses' YouTube blog (Восстановлен)10A opshNo ratings yet
- A Seminar Report On Hydrogen Cars by B.durga PrasadDocument4 pagesA Seminar Report On Hydrogen Cars by B.durga PrasadMi CkyNo ratings yet
- IBADocument11 pagesIBAMuhammad Noor AmerNo ratings yet
- Pedigree Analysis WorksheetDocument6 pagesPedigree Analysis WorksheetLloaana 12No ratings yet
- Question: 1. For The Heat Exchanger Shown in Fig. 1 With Water On Both TDocument3 pagesQuestion: 1. For The Heat Exchanger Shown in Fig. 1 With Water On Both TPrabhasha JayasundaraNo ratings yet
- Critical Reflective Techniques - Ilumin, Paula Joy DDocument2 pagesCritical Reflective Techniques - Ilumin, Paula Joy DPaula Joy IluminNo ratings yet
- Rosenberg SelfDocument5 pagesRosenberg SelfHanaeeyemanNo ratings yet
- Stress and Anxiety: Essay SampleDocument3 pagesStress and Anxiety: Essay SampleAshley Jane MacapayadNo ratings yet
- VWR Traceable 300-Memory StopwatchDocument1 pageVWR Traceable 300-Memory Stopwatchlusoegyi 1919No ratings yet
- Evolution of Traditional Media To New MediaDocument12 pagesEvolution of Traditional Media To New MediaCaroline AlvarezNo ratings yet
- Craap Test WorksheetDocument5 pagesCraap Test Worksheetapi-272946391No ratings yet
- This Study Resource Was Shared Via: Flexible Instructional Delivery Plan (Fidp) 2020-2021Document5 pagesThis Study Resource Was Shared Via: Flexible Instructional Delivery Plan (Fidp) 2020-2021Sa Le HaNo ratings yet
- The Implementation of Social Work Hybrid Program in Medical Mission Group College of General Santos City, Incorporated: Basis For Curriculum Development PlanDocument14 pagesThe Implementation of Social Work Hybrid Program in Medical Mission Group College of General Santos City, Incorporated: Basis For Curriculum Development PlanPsychology and Education: A Multidisciplinary JournalNo ratings yet
- How Many Hours Should One Study To Crack The Civil Services Exam?Document27 pagesHow Many Hours Should One Study To Crack The Civil Services Exam?654321No ratings yet
- Hypothesis Test - Difference in MeansDocument4 pagesHypothesis Test - Difference in Meansr01852009paNo ratings yet
- Capstone IdeasDocument9 pagesCapstone IdeastijunkNo ratings yet
- List of TextbooksDocument5 pagesList of TextbooksESPORTS GAMING ZONENo ratings yet