Professional Documents
Culture Documents
California Edition: AIDS Mortality Plummets in California
Uploaded by
PayersandProvidersOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
California Edition: AIDS Mortality Plummets in California
Uploaded by
PayersandProvidersCopyright:
Available Formats
1 December 2011
California Edition
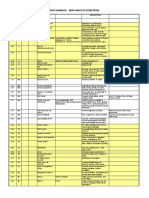
Calendar
December 1
!>885.6!L15=7"&8!;.63@1&83.!;KM!N1&5$B! ;.63@1&83.!<841D$"8=(!:1/!>89"6"/B!>! 611J!.=!=&"84/!.84!%"/=!O&.#=3#"/!38! 7".6=7#.&"!="#781619,B!EP*HE'*GB
AIDS Mortality Plummets In California
Deaths a Fraction of Past Rate; Disparities Persist
Hospitalization data on Californias HIV and AIDS patients released by the Ofce of Statewide Health Planning and Development show a steadily dropping mortality rate, but cases continue to rise and minority populations are affected by the disease disproportionately. The report, released on the eve of World AIDS Day, shows that the number of Californians living with AIDS or the HIV virus has nearly tripled between 1988 and 2008, to 107,000 from 37,000. However, far fewer Californians are dying from the disease. The mortality rate in 1988 stood at about 230 per 1,000. But by 2008, it stood at around 20 per 100,000. Ofcials with OSHPD and the California Department of Public Health, which held a joint press conference on Wednesday to announce the ndings, credited the drop to the use of antiretroviral drugs beginning in the mid-1990s. There was a time when men were basically returning home from the hospital to die, said CDPH director Mark Chapman, M.D., who saw the onset of the epidemic rsthand while practicing at a Northern California hospital in the 1980s. Weve come a long way since that time. There have been miraculous advances in treatment. Hospitalizations for treatment of the disease also dropped, from 400 per 1,000 at its peak to less than 200 per 1,000 in 2008. The mortality rate of those who are hospitalized for HIV/AIDS-related conditions dropped from 12.7% in 1988 to 5% in 2008. Although the news was encouraging, stark differences in how the disease affect certain minority groups persist. The percentage of those living with HIV/AIDS in California has more doubled among Latinos, which represent 30% of its total population in 2008, compared to 14% in 1988. African-Americans comprised 19% of the HIV/AIDS population in 2008, compared to 12% in 1988. Among African-Americans, the disease affected about 90 individuals per 10,000 population, more than quadruple the rate from the 1980s. African-Americans also die from AIDS at higher rates than all other minority groups other than Native Americans. Asian-Americans had the lowest rate of the disease as a group, at around 10 cases per 10,000 population. Latinos are also being diagnosed with HIV/AIDS far later than other groups, putting them at greater risk of dying from the disease. Chapman suggested such disparities could be addressed in part by ne-tuning outreach programs to address how specic minority groups address the disease. Weve gotten progressive in certain areas of public health, but we still have a long way to go, he said.
;63#J!?"&"!@1&!C1&"!K8@1&$.=318
December 5-6
<397=7!.885.6!>$"&3#.8!?".6=7!;.&"! ;18@"&"8#"!.84!<A73%3=318B!>8.7"3$! C.&&31==B!>8!"A.$38.=318!1@!8"D!4"632"&,! $14"6/!.84!38="9&.=318!/=&.="93"/B!E'()FGH E'(IF*B ! ;63#J!?"&"!@1&!C1&"!K8@1&$.=318
January 12-14
;.63@1&83.!;7.O="&!1@!=7"!;166"9"!1@! <$"&9"8#,!-7,/3#3.8/!PG=7!.885.6! <$"&9"8#,!C"43#38"!38!Q1/"$3="! #18@"&"8#"B!>7D.8""!?1="6(!Q1/"$3="! R.=318.6!-.&JB!>!43/#5//318!1@!=&"84/!.84! =&".=$"8=/!.@@"#=389!<!!#.&"B!EPSGHEST*B ! ;63#J!?"&"!@1&!C1&"!K8@1&$.=318
E-Mail info@payersandproviders.com with the details of your event, or call (877) 248-2360, ext. 3. It will be published in the Calendar section, space permitting.
!"#"$%"&!'(!)*''!+!)*''!%,!-.,"&/!0!-&1234"&/!-5%63/7389(!::;
Payers & Providers
Top Placement... Bottomless Potential
NEWS
Page 2
Patient Breaches Continue To Grow
Little is Done to Address Portable Device Security
As Sacramento-based hospital system Sutter Health faces litigation over a breach of patient data involving 4.2 million patients it disclosed last month, a new study of hospital systems indicates that the situation involving compromised medical data is getting worse, not better. The study of 75 healthcare systems by the Michigan-based Ponemon Institute concluded that healthcare data breaches increased 32% in 2011 compared to 2010. The average cost of such a breach is more than $2.2 million up around 9% from a year ago. It also damages the brand of the healthcare institution where the breach occurs and leads to lost patients. In California, 19 healthcare organizations reported breaches to the U.S. Department of Health and Human Services in 2010, compared to 12 so far in 2011. Of such breaches, 49% involved a lost or stolen computing device, as was the case with the Sutter incident. Thats up from 41% in 2010. Ponemon Institute Chairman Larry Ponemom indicated that safeguarding such devices particularly smart phones will be one of the biggest challenges facing healthcare organizations in 2012. Folks in the study have conceded that (portable devices) are not secure, said Ponemon. Another challenge is safeguarding data as its transferred from paper to electronic format. Sutter disclosed the breach last month, which occurred as the result of the theft of a desktop computer. The device was passwordprotected but not encrypted. Law rms in Los Angeles and Sacramento led class-action suits last week against Sutter. One of the suits seeks more than $4 billion in damages.
Advertise Here
(877) 248-2360, ext. 2
In Brief
Primes Billing For Heart Failure Examined
Chino Valley Hospital has allegedly been billing Medicare to treat patients for heart failure at rates far higher than the national average, according to a recent report by California Watch. According to analysis of billing data for Chino Valley, nearly onethird of its Medicare patients in recent years suffered from acute heart failure--a rate nearly six times the average for California. The facility is owned by Ontario-based Prime Healthcare Services. California Watch, a non-prot investigative journalism organization, noted the hospital billed Medicare for virtually no heart failure patients in 2006, just prior to Medicare initiating a rule change that allowed a bonus for treating such cases. Between 2008 and 2010, the hospital treated nearly 2,000 patients for the ailment. Eighteight percent of the time, the diagnoses was billed in a way that would trigger the extra payments. Prime ofcials disputed the report by California Watch, which has been scrutinizing Prime's billing practices. Anthony Glassman, a Prime attorney, told the organization its analysis was "faulty, unfair and biased." He added that Chino Valley treated such a large number of heart failure patients because many are admitted from nearby nursing homes and through the hospital's emergency department.
CHA Tries To Enjoin Medi-Cal Cuts
Motion on Matter Will Be Heard Later This Month
The California Hospital Association is seeking a federal court injunction against pending reductions in Medi-Cal payments it believes will seriously damage its constituents. The motion for an injunction, which will be heard in Los Angeles on Dec. 19, comes as trade groups representing physicians, dentists and pharmacists led their own suits against the Department of Health and Human Services and the California Department of Health Care Services for cuts in Medi-Cal reimbursement expected to affect their practices. The reductions, which range from 10% to more than 20%, are retroactive to June 1 and were recently approved by the federal government. If enacted, they would save the Medi-Cal program about $623 million per year. During months of conversations with state and federal ofcials, hospitals across
Continued on Next Page
Thursday, Dec. 15, 2011
Blue Shield Sends Out Policholder Credits
San Francisco-based health plan Blue Shield of California has begun distributing credits to its policyholders that range from 18% to 54% of a monthly premium.
10 A.M. PST
California Healthcare: A 2012 Business Forecast
Please join Steven T. Valentine, President of The Camden Group, Henry R. Loubet, Chief Strategy Officer for Keenan, and Jim Lott, Executive Vice President of the Hospital Association of Southern California, to discuss the trends that will shape California!s healthcare business environment in 2012:
http://www.healthwebsummit.com/ppcalifornia121511.htm
a HealthcareWebSummit Event
co-sponsored by
Continued on Page 3
PAYERS & PROVIDERS
!"#"$%"&!'(!)*''!+!)*''!%,!-.,"&/!0!-&1234"&/!-5%63/7389(!::;
Payers & Providers
Longer ALOS!*
NEWS
CHA (Continued from Page One)
California provided compelling evidence about the impact these cuts will have on access to care for our most vulnerable patients, said CHA President C. Duane Dauner. We believe that the cuts are in violation of federal Medicaid law and without regard for the welfare of thousands of patients with complex medical needs. The CHA, which led suit against the state and federal government last month, wants to block rate cuts for skilled nursing
Page 3
Advertise Here
(877) 248-2360, ext. 2
*For our ads, not your hospital
In Brief
Blue Shield announced the credits earlier this year as part of a pledge to limit its net income to 2% of its annual revenue. Blue Shield is a not-for-prot organization. As a mission-based, not-forprot health plan, we made this commitment to help keep coverage affordable for our members. While these credits will help our customers, every player in the healthcare industry must do more to reduce the cost of care, said Blue Shield Chief Executive Ofcer Bruce Bodaken. The average credit for an individual plan enrollee is $135, with a family of four receiving about $420. Large and mid-sized group customers will receive credits ranging from $195 to $235 per enrollee, with small groups receiving an average of $220.
facilities operating within hospitals. According to a recent survey of its membership, half would close their skilled nursing facilities, while more than a third are pondering reducing beds or closing such services to Medi-Cal enrollees. In addition to the CHA suit, the California Medical Association, California Dental Association, California Pharmacists Association and the National Association of Chain Drug Stores sued late last month.
Kaiser Enters Breast-Feeding Pact
Initiative Expected to Fight Childhood Obesity
Healthcare system Kaiser Permanente has entered into a pact with the Partnership for a Healthier America to signicantly ramp up the number of children born at its facilities who breastfeed. The initiatives aim is to reduce the skyrocketing rates of childhood obesity. Nearly 20% of American children are considered obese, a rate that has tripled over the past 30 years. Although breast-feeding a child during the rst year of life is linked by some research to lower rates of obesity, only 13% of children are still being breast-fed within six months of birth, according to the U.S. Surgeon Generals ofce, which blamed the trend in part on poor planning by hospitals. Barriers to breastfeeding are widespread during labor, delivery, and postpartum care, as well as in hospital discharge planning, read a Surgeon Generals report issued in January. Under the agreement, Kaiser said by early 2013, all of its hospitals that offer maternal services would either be designated as baby-friendly based on criteria provided by the Baby Friendly Hospital Initiative, or participate in the Joint Commissions perinatal core measures program. That requires each hospital to report breastfeeding rates at discharge. Those rates will also be included in Kaisers quarterly quality scorecard. Fewer than half of Kaisers hospitals now have the baby-friendly designation. Kaiser could not provide specic data on what percentage of children born at its facilities leave breastfeeding. California has one of the higher rates of breastfeeding children in the U.S. "Kaiser Permanente's commitment to make breastfeeding a priority for each child born in one of their hospitals has potential to make a very big impact, said Lawrence A. Soler, chief executive ofcer of Partnership for a Healthier America. We're pleased they are such a strong partner in ghting childhood obesity."
UCLA Nursing School Intervention Program Gets Federal Funding
The U.S. Department of Health and Human Services has chosen for funding a program started by the UCLA School of Nursing that targets minority teenagers who have given birth or are pregnant. The Public Health Nursing Early Intervention Program for Adolescent Mothers provides education for expecting Latina and AfricanAmerican teen mothers regarding prenatal healthcare, childbirth and preparation for motherhood. The intent is to cut down on healthcare costs for their newborns, many of which have low birth weights and other problems often requiring hospitalization. The costs to the U.S. healthcare system are substantial about $9 billion each year so it is in the interest of the states to enhance the health outcomes for those teens who do become pregnant and for their babies, said Deborah Koniak-Grifn, a UCLA nursing professor and director of the universitys Center for Vulnerable Populations Research.
HEALTHCARES BEST ADVERTISING VALUE
]
PAYERS & PROVIDERS reaches 5,000 hospital, health plan and nonprot executives statewide. There is no better venue for marketing your organization or conference, or recruiting new staff.
CALL (877) 248-2360, ext. 2 OR CLICK HERE
!"#"$%"&!'(!)*''!+!)*''!%,!-.,"&/!0!-&1234"&/!-5%63/7389(!::;
Payers & Providers
OPINION
Page 4
<165$"!=(!>//5"!??
-.,"&/!0!-&1234"&/!3/! @5%63/7"4!"2"&,!A75&/4.,!%,! -.,"&/!0!-&1234"&/!-5%63/7389(! ::;B!C8!.885.6!38432345.6! /5%/#&3@D318!3/!EFF!.!,".&! GE'?F!38!%56H!5@!D1!'*! /5%/#&3%"&/IB!>D!3/!4"632"&"4!%,! "J$.36!./!.!-!K!.DD.#7$"8D(! 1&!./!.8!"6"#D&183#!8"L/6"DD"&B
C66!.42"&D3/389(!/5%/#&3%"&!.84! "43D1&3.6!38M53&3"/N
GOPPI!)?OJ)=Q* 38R1S@.,"&/.84@&1234"&/B#1$
Employers As Tough Benefit Managers
Little Attention is Paid to Making Coverage Perform
Healthcare is like no other U.S. industry. years, employers often tell me that less than Employers do not manage their health costs 10% or even 20% of their targeted population like they do every other supplier or vendor; is engaged in these programs. youd be hard pressed to nd another example Translated to common purchases, bananas where companies pay millions of dollars for are sold at about $1 a pound and there are services without requiring quality or even typically four bananas in a pound. If you pay results, for that matter. As one of the largest $1, you expect four bananas. What if you only purchasers of healthcare, employers must take received one banana? Would you want a responsibility to combat rising costs and poor refund? Would you want the grocer to go at quality by demanding and measuring quality risk to guarantee you get the bananas? Why is and value for every dollar spent with their this not the case for healthcare? vendors (i.e. health plans and providers). Even acknowledging that some folks will According to recent research released by never engage, you might expect 75% the non-prot Center for Health engagement in the programs. Perhaps Value Innovation (CHVI), we could be comfortable with three healthcare benets are underof the four bananas. But today managed. A focus on outcomes employers are often settling for a missing from most benet programs return of only one or two bananas. -- could produce better results. This lack of oversight leads to CHVIs efforts over the past ve signicant waste. Employers are years have conrmed that worn down from the past several engagement and accountability are years of economic turmoil, the fear sorely lacking across all of the of changing insurance plans or stakeholders in the health supply benets advisers during the health chain, including consumers, reform ramp up, and the employers, providers and health downsizing of benets staff at many plans. Payment reform has been companies. promoted to manage the rising costs Employers must begin to take a By of inpatient and outpatient services, more active and disciplined risk Cyndy Nayer management approach for health and outcomes-based contracting (aligning incentives across all benets. Employee health screenings stakeholders) has taken a major step should be their rst step. After that, forward to align payment with metrics that employers should offer guidance to employees matter (adherence to safety and clinical on the goal-setting and tracking of prescribed guidelines, for example). Outcomes-based treatment; build accountability through contracting puts a part of a service agreement outcomes-based contracting by creating a at risk and then uses benet design incentives prototype contract for services, data and to drive patients to the higher-performing measures; and identify and implement best service providers, improving engagement and practices that improve accountability for accountability. outcomes. Many employers spend millions of dollars We must treat employee benets and on healthcare without understanding their healthcare expenses like any other business engagement and outcomes patterns. In these practice. We need to align responsibilities to all-too-common scenarios, healthcare services control healthcare and absence costs in a way are purchased on a rate per employee. For that encourages good performance and good instance, medication coaching may be health. purchased for $10 per diagnosed employee for management of diabetes. (Numbers here are Cyndy Nayer is president and chief executive used only for illustration and not related to of the Center for Health Value Innovation. actual costs.) If there are 100 diagnosed diabetics in the population, then the employers pay 100 times $10, or $1,000. Op-ed submissions of up to 600 words are Yet who is managing the deliverables? In welcomed. Please e-mail proposals to surveys and seminars I have led for over 15
editor@payersandproviders.com
T.36389!.44&"//N
O'O!UB!V166,L114!W.,(!X53D"!Y Y5&%.8H(!;C!F'Z*Z
W"%/3D"
LLLB@.,"&/.84@&1234"&/B#1$
K.#"%11H
LLLBR.#"%11HB#1$[@.,"&/@&1234"&/
AL3DD"&
LLLBDL3DD"&B#1$[@.,"&/@&1234"&/
\43D1&3.6!Y1.&4
XD"2"8!AB!<.6"8D38"(!-&"/34"8D(! A7"!;.$4"8!]&15@ ^1//!]164%"&9(!>$$"43.D"!-./D! -&"/34"8D(!:1/!^1%6"/!V1/@3D.6! .84!T"43#.6!;"8D"& T.&H!K385#.8"(!T.8.9389! !3&"#D1&(!C62.&"_!0!T.&/.6 V"8&,!:15%"D(!;73"R!XD&.D"9,! `RR3#"&(!a""8.8 C8D718,!W&397D(!\b"#5D32"! !3&"#D1&(!V".6D7!C##"//!;.63R1&83.
-5%63/7"&[\43D1&
^18!X738H$.8
@5%63/7"&S@.,"&/.84@&1234"&/B#1$ >R!,15!41!81D!&"#"32"!,15&!3//5"!1R! -.,"&/!0!-&1234"&/!%,!'!-BTB!18! A75&/4.,(!@6"./"!#.66!GOPPI)?OJ)=Q*B
!"#"$%"&!'(!)*''!+!)*''!%,!-.,"&/!0!-&1234"&/!-5%63/7389(!::;
Payers & Providers
MARKETPLACE/EMPLOYMENT
Page 5
SENIOR NETWORK CONTRACT MANAGER
UnitedHealthcare Employer & Individual is actively seeking a Senior Network Contract Manager to join our team. The Senior Network Contract Manager develops the provider network (physician groups and hospitals) yielding a geographically competitive, broad access, stable network that achieves objectives for unit cost performance and trend management, and produces an affordable and predictable product for customers and business partners. Senior Network Contract Managers evaluate and negotiate contracts in compliance with company contract templates, reimbursement structure standards, and other key process controls. Specifically the Senior Network Contract Manager will: Formulate and execute contracting plans using financial models to meet or exceed established targets. Negotiate financial terms and contract language for capitated and fee-for-service medical group and hospital agreements. Provide contract language interpretation as needed for related departments. Identify solutions to challenging issues, working with other departments to bring matters to resolution.
CHIEF MEDICAL OFFICER
Inter Valley Health Plan, a regional Medicare Advantage Plan headquartered in Pomona, has an opening for a Chief Medical Officer. Reporting to the President and Chief Executive Officer with dotted line reporting to the Vice President, Health and Member Services, the Chief Medical Officer is responsible for the design and implementation of clinical systems, strategies and initiatives to continuously improve the quality of patient care provided to members by medical staff. As a key member of the executive team, the Chief Medical Officer will oversee clinical business strategies for the health plan while establishing the highest standards of best practices. Responsibilities also include providing leadership and direction in clinical integration, education and medical staff development as well as overseeing the development, implementation and monitoring of Health Plan quality and Utilization Management programs. Requirements Include: M.D. or D.O license in California with Board Certification in Internal Medicine; Masters degree in Public Health or related area a plus; Experience in Managed Care with an emphasis on Medicare and IPA Management Provider systems; demonstrated successful experience with managing UM, QM, and Credentialing areas; demonstrated strong leadership and management skills with ability to employ sound reasoning and resourcefulness to accomplish company objectives. To Apply: Please submit resume with cover letter to: jobs@ivhp.com; fax: 909-622-9634.
Qualified candidates please apply online at http://careers.unitedhealthgroup.com, Job number: 360202
It costs up to $27,000 to fill a healthcare job*
will do it for a lot less.
Employment listings begin at just $1.65 a word Call (877) 248-2360, ext. 2 Or e-mail: advertise@payersandproviders.com Or visit: www.payersandproviders.com
*New England Journal of Medicine, 2004.
!"#"$%"&!'(!)*''!+!)*''!%,!-.,"&/!0!-&1234"&/!-5%63/7389(!::;
Payers & Providers
MARKETPLACE/EMPLOYMENT
Page 6
CLINICAL PHARMACIST (Long Beach, CA) JOB SUMMARY: Work in collaboration with the pharmacy staff to update and maintain the formulary used by SCAN. Spearhead and oversee the implementation of key clinical pharmacy programs. Work with appropriate departments to produce pharmacy related marketing materials in accordance with CMS guidelines. ESSENTIAL JOB RESULTS: Produce marketing materials within internally determined timeframes with accuracy and in accordance with the CMS marketing guidelines. Utilize CMS model templates to populate pharmacy specific information per CMS guidelines; partner with Marketing, Compliance and Member Education as needed. Work in collaboration with other pharmacy staff to support the annual formulary/ prior authorization (PA) criteria submission to CMS. Prepare monographs & prior authorization/ non-formulary exception criteria and present clinical data on new drug therapies and clinical programs at Pharmacy and Therapeutics Committee meetings. Review new drugs with the Pharmacy & Therapeutics Committee within 90-180 days of being marketed. Decisions related to the drug formulary and utilization management restrictions will reflect compliance with CMS guidelines. Develop and update Prior authorization criteria by using appropriate clinical references when new clinical information becomes available. Coordinate the implementation of new and revised PA/non-formulary exception criteria with the PBM company. Develop and/or implement clinical pharmacy programs in-house or in collaboration with the Pharmacy Benefit Management (PBM) company as needed. Daily interactions with SCAN employees and/or PBM representatives may be required. In-depth knowledge of CMS guidelines related to the Clinical Pharmacists job and the ability to ensure compliance with the CMS requirements is essential. Maintain professional and technical knowledge by attending educational workshops; reviewing and contributing to professional publications; establishing personal networks; participating in professional societies. Contribute to team effort by accomplishing related results as needed. QUALIFICATIONS: Pharm.D. Degree with a residency program in Drug Information or Geriatric Pharmacy preferred. Pharmacy Licensure in California required. Part D experience preferred. Managed care experience at a PBM, health plan or medical group preferred. Excellent verbal and writing skills required. Proficient in MS Office. FT position, M-F 8 AM to 5 PM, occasional extended work hours as needed. Telecommute up to 25%. Apply to www.scanhealthplan.com - Job Opportunities - Req # 11-285
DIRECTOR, PHARMACY CLINICAL SERVICES (Long Beach, CA) JOB SUMMARY: Reporting to VP of Pharmacy Services, this position will play a central role in pharmacy management for a senior-focused Medicare Advantage Plan with over $140 million in annual drug expenditure. Director will be accountable for providing leadership support to department, managing change, improving efficiencies and managing and ensuring strong clinical programs aligned with organizational direction. In addition, Director will service as Part D pharmacy expert for the department and organization. ESSENTIAL JOB RESULTS: Serve as a clinical/subject matter expert on pharmacy benefit management. Coordinate the work product of clinical operation team members (clinical pharmacists and pharmacy benefits administrators). Oversee PBM operations to ensure high service level to SCAN and our members. Oversee clinical and technical initiatives (eg. MTM, e-prescribing, provider/member web based tools). Monitor, evaluate, develop and implement quality initiatives (i.e. DUR programs) and drug cost management strategies. Serve to oversee clinical operations of pharmacy department to ensure proper accuracy and efficiency. Serve as backup of clinical operations when necessary (Grievances, appeals, medication therapy management reviews, formulary management). Participate in business and budget planning process. Oversee pharmacy operations for Employer Group Retiree Plans. Lead department initiatives. Foster strong relations with internal departments and external providers. Serve as pharmacy expert on a variety of committees and workgroups. Maintain current knowledge of Medicare Part D regulations by participating in CMS calls and reading released guidance. QUALIFICATIONS: California State Board of Pharmacy, Registered Pharmacy license required. Doctor of Pharmacy (Pharm. D.), with residency in clinical pharmacy practice preferred. Five (5) years or more of managed care pharmacy experience as a Director; or equivalent experience in a managed care setting, strongly preferred. Demonstrated knowledge of Medicare Part D required. Medicaid knowledge preferred. Excellent written, oral and interpersonal communication skills required. Strong computer skills using MS Word, Excel and PowerPoint required. Strong leadership & supervisory skills required. Strong analytical, problem-solving, negotiation, and decision-making skills required. FT position, M-F 8 AM to 5 PM, occasional extended work hours as needed. Apply to www.scanhealthplan.com - Job Opportunities Req # 11-375
!"#"$%"&!'(!)*''!+!)*''!%,!-.,"&/!0!-&1234"&/!-5%63/7389(!::;
Payers & Providers
MARKETPLACE/EMPLOYMENT
Alameda Alliance for Health is a public, not-for-profit managed care health plan for lower income people in Alameda County. TheAlliance provides healthcare coverage to over 130,000children and adults through four programs: Medi-Cal, Healthy Families, Alliance Group Care, and Alliance CompleteCare.
Page 7
Health care you can count on. Service you can trust.
DIRECTOR, MEDICARE
This position is responsible for the oversight and management of the Medicare Special Needs Plan and will work cross-functionally within the organization and externally on all issues related to Medicare. The position will also provide leadership on Medicare staffing and functions, organizational structure, and operational standards. The position requires an individual with Medicare operations and oversight experience, preferably who also has experience with dual eligibles or Medi-Cal. A Masters degree in Business Administration, Public Health, Public Policy, or related field is preferred, plus 2 years experience and/or training. A minimum of 2 years of recent Medicare Advantage Part D plan experience is required.
DIRECTOR, COMPLIANCE
This position is responsible for developing, implementing, and providing oversight of all compliance activities related to the Alliances adherence to laws, regulations, and contracts that govern its business. The position will assess areas of risk, develop the annual audit plan and internal audit tools, conduct internal audits, and implement plans to reduce risk and maintain compliance. The position is also responsible for compliance training, and managing the intake, investigation/ reporting of fraud, waste and abuse incidents. A Bachelors degree is required and a minimum of 5 years compliance experience in a managed care plan or a community clinic is required. A Masters degree and certification in Healthcare Compliance (CHC) is preferred.
MANAGER, HEALTHCARE ANALYTICS
This position is responsible for the oversight and management of analytical staff and the implementation of systems and techniques for analysis and reporting. The position requires an understanding of business needs, informational systems, healthcare data inputs and operations to ensure data quality and completeness in support of analysis and reports that improve the quality and efficiency of clinical and business processes and performance. The position will work with key internal staff and outside business users to develop the functional and architectural design of data systems and data warehouses and to select reporting tools that will enable easier end user access to data. A Bachelors degree or equivalent training in a health-related, scientific, or public policy/business discipline is required. 10 or more years experience in healthcare with Medicare risk adjustment, reconciliation, and reporting experience preferred. A minimum of 2 years supervisory experience is required.
MANAGER, MEDICARE COMPLIANCE
This position will implement a compliance assessment, auditing and monitoring program for the health plans Medicare Advantage Plan. Responsibilities include coordinating external audits and conducting internal compliance audits to ensure compliance with contractual and regulatory requirements. Other responsibilities include creating reports, educating and following up with business areas to ensure that processes exist to demonstrate compliance.The position will also support the entire organization with compliance related training. The position investigates, summarizes findings, and reports suspected fraud, abuse, and non-compliance to the Compliance Officer, regulatory agencies, Medicare Director, and others. A Bachelors degree in a related field is required, a Masters degree is preferred. Knowledge of managed care contractual and regulatory requirements for Medicare and Medicaid is required.
We offer an excellent compensation & benefits package. Please visit our website at www.alamedaalliance.org and click on the Careers button for more specific job information and to apply for these positions. EEO.
SEEKING A NEW POSITION?
CAN HELP.
We publish advertisements for those seeking new career opportunities for just $1.25 a word. If you prefer discretion, well handle all responses to your ad. Call (877) 248-2360, ext. 2, or e-mail advertise@payersandproviders.com.
!"#"$%"&!'(!)*''!+!)*''!%,!-.,"&/!0!-&1234"&/!-5%63/7389(!::;
Payers & Providers
MARKETPLACE/EMPLOYMENT
Page 8
DIRECTOR, QUALITY IMPROVEMENT
JOB SUMMARY: The Director, Quality Improvement is responsible for coordinating assigned regulatory, accreditation, clinical quality and/or service improvement programs. Functions as a leader for assigned health services initiatives handling multiple large-scale complex initiatives. May collaborate on national, regional and multi-plan initiatives. Develops programs in compliance with accreditation and regulatory requirements/standards and monitors ongoing program performance to maintain compliance. Acts as a resource for training, policy and regulatory/ accreditation interpretation. DUTIES AND RESPONSIBILITIES: Leads and manages multiple complex initiatives that impact the quality or effectiveness of health care delivery and/or health care services provided to members, ensuring compliance with accreditation and regulatory requirements. Provides an assessment of programs, initiatives and interventions to determine the effectiveness of activities and makes recommendations to improve outcomes. Develops targeted activities to improve HEDIS, CAHPS, provider satisfaction and other identified performance measures. Completes project-related communication, including member/physician mailings, business plans, graphics, minutes and agendas. Monitors and analyzes outcomes to ensure goals, objectives, outcomes, accreditation and regulatory requirements are met. Identifies areas of improvement within the company and works collaboratively with other departments to develop clinical and non-clinical performance improvement projects. Researches best practices, national and regional benchmarks, and industry standards. Ensures that clinical and service quality improvement standards are compliant with accreditation, state and federal requirements. Interfaces with contracted providers or provider groups to promote participation in quality improvement collaborative to improve clinical care outcomes, health care service utilization and costs. In conjunction with medical director, communicates quality improvement initiatives, results, and/or performance data to participating physician groups. Assess current industry trends and regulations for enterprise-wide adoption to assure quality and effectiveness of health care delivery and/or healthcare services provided to members. Supports the function of the Quality Improvement Committee. QUALIFICATIONS: Bachelors Degree with Registered Nurse License or Masters Degree in a related health field (i.e. MPH or MPA) or field of experience. Minimum 2 years experience in clinical/health care environment with related degree program. 5 years managed care experience. Experience in compliance, accreditation, service or and quality improvement. Complex project management experience. Experience with Medicare and/or NCQA preferred.
PROJECT MANAGER-HEDIS (Long Beach, CA) JOB SUMMARY: Position supports the Quality Initiatives Team and Healthcare Informatics in activities related to quality improvement, measurement, reporting and analysis. ESSENTIAL JOB RESULTS: Manage all aspects of the HEDIS project, including, but not limited to, data collection, abstraction, and the compliance audit. Hire, train and supervise temporary HEDIS staff. Identify data sources and ensure accuracy and completeness of the HEDIS data repository. Collaborate with other departments on project implementation. Provide weekly status update to management. Conduct analyses to identify barriers, gaps, and opportunities for improvement. Educate network providers on evidence based clinical guidelines and best practices to improve quality of care and service for members through webinars, on-site meetings, mail and electronic correspondence. Conduct targeted member and provider outreach and education via electronic data exchange, phone calls/IVR, mailings, etc. Utilize HEDIS/HOS/CAHPS metrics to monitor and improve clinical outcomes. Maintain professional and technical knowledge by attending educational and technological workshops. QUALIFICATIONS: Bachelors or Masters degree in health care or related area with emphasis in quantitative data analysis. Experience in quality improvement and HEDIS project management. Moderate to strong knowledge in processing of claims, encounters, and pharmacy data. Proficient in SAS/SQL programming. Proficient in Microsoft Office applications. Strong verbal and written communication skills with the ability to express ideas in a clear and organized manner. Strong organizational and time management skills to efficiently handle multiple projects with changing priorities. FT position, M-F 8 AM to 5PM, with extended working hours and occasional travel as needed. Apply to www.scanhealthplan.com Job Opportunities Req. # 11-415
Competitive salary, plus excellent benefits. If you meet the requirements of this job opportunity, please send your resume to HR@goldchp.org. NO THIRD PARTY AGENCY OR SEARCH FIRMS.
!"#"$%"&!'(!)*''!+!)*''!%,!-.,"&/!0!-&1234"&/!-5%63/7389(!::;
You might also like
- Quality Assurance Plan For Building ConstructionDocument18 pagesQuality Assurance Plan For Building ConstructionANup GhiMire100% (3)
- Final Health Care Policy Analysis PaperDocument12 pagesFinal Health Care Policy Analysis Paperapi-242943882100% (2)
- Audit Universe and Risk Assessment ToolDocument10 pagesAudit Universe and Risk Assessment ToolAsis KoiralaNo ratings yet
- Midwest Edition: Missouri Throws Out Med-Mal CapDocument5 pagesMidwest Edition: Missouri Throws Out Med-Mal CapPayersandProvidersNo ratings yet
- California Edition: Providers Facing Big Medi-Cal CutsDocument5 pagesCalifornia Edition: Providers Facing Big Medi-Cal CutsPayersandProvidersNo ratings yet
- California Edition: L.A. Care Will Absorb Medi-Cal CutsDocument6 pagesCalifornia Edition: L.A. Care Will Absorb Medi-Cal CutsPayersandProvidersNo ratings yet
- California Edition: L.A. Care Will Absorb Medi-Cal CutsDocument6 pagesCalifornia Edition: L.A. Care Will Absorb Medi-Cal CutsPayersandProvidersNo ratings yet
- California Edition: Medi-Cal Caregivers Are in A PinchDocument7 pagesCalifornia Edition: Medi-Cal Caregivers Are in A PinchPayersandProvidersNo ratings yet
- California Edition: Healthcare Is Hit Hard by New CutsDocument6 pagesCalifornia Edition: Healthcare Is Hit Hard by New CutsPayersandProvidersNo ratings yet
- California Edition: Health Net, DHCS Settle Rate LawsuitDocument5 pagesCalifornia Edition: Health Net, DHCS Settle Rate LawsuitPayersandProviders100% (1)
- Midwest Edition: Wellpoint at Bottom of Hospitals' ListDocument5 pagesMidwest Edition: Wellpoint at Bottom of Hospitals' ListPayersandProvidersNo ratings yet
- Covid19 Updates ArticlesDocument7 pagesCovid19 Updates ArticlesCindy P. PagaNo ratings yet
- California Edition: Millions Awarded For Medical HomesDocument6 pagesCalifornia Edition: Millions Awarded For Medical HomesPayersandProvidersNo ratings yet
- California Edition: Eisenhower Seeing Tougher BattlesDocument7 pagesCalifornia Edition: Eisenhower Seeing Tougher BattlesPayersandProvidersNo ratings yet
- California Edition: Millions Awarded For Medical HomesDocument6 pagesCalifornia Edition: Millions Awarded For Medical HomesPayersandProvidersNo ratings yet
- 50 Signs That The UDocument12 pages50 Signs That The Ubigwill35No ratings yet
- 11 Himmelstein, David U., SteffieWoolhandler, Mark Almberg, and Clare Fauke 2017 - The U.S. Health Care Crisis Continues A Data SnapshotDocument14 pages11 Himmelstein, David U., SteffieWoolhandler, Mark Almberg, and Clare Fauke 2017 - The U.S. Health Care Crisis Continues A Data SnapshotMiguel AgustínNo ratings yet
- California Edition: 140,000 Booted From Medicare PlansDocument5 pagesCalifornia Edition: 140,000 Booted From Medicare PlansPayersandProvidersNo ratings yet
- Midwest Edition: Wisconsin Targets Quality UpgradeDocument5 pagesMidwest Edition: Wisconsin Targets Quality UpgradePayersandProvidersNo ratings yet
- California Edition: California Blues Launch New AcosDocument8 pagesCalifornia Edition: California Blues Launch New AcosPayersandProvidersNo ratings yet
- Five Myths About Medical NegligenceDocument12 pagesFive Myths About Medical NegligenceLateNightRomeNo ratings yet
- Southwest Hospital Center Case1Document9 pagesSouthwest Hospital Center Case1api-233761215No ratings yet
- Payers & Providers California Edition - Issue of January 5, 2012Document6 pagesPayers & Providers California Edition - Issue of January 5, 2012PayersandProvidersNo ratings yet
- Midwest Edition: Two Rural Hospital Funds May Dry UpDocument5 pagesMidwest Edition: Two Rural Hospital Funds May Dry UpPayersandProvidersNo ratings yet
- California Edition: Blue Shield, Hospitals CollaborateDocument7 pagesCalifornia Edition: Blue Shield, Hospitals CollaboratePayersandProvidersNo ratings yet
- Payers & Providers Midwest Edition - Issue of June 5, 2012Document6 pagesPayers & Providers Midwest Edition - Issue of June 5, 2012PayersandProvidersNo ratings yet
- Payers & Providers California Edition - Issue of May 3, 2012Document6 pagesPayers & Providers California Edition - Issue of May 3, 2012PayersandProvidersNo ratings yet
- 1 Million Daily Covid 19 Cases Could Hit The U by The End of The Year Report FindsDocument5 pages1 Million Daily Covid 19 Cases Could Hit The U by The End of The Year Report Findskim haroldNo ratings yet
- California Edition: Providers Line Up Against InitiativeDocument7 pagesCalifornia Edition: Providers Line Up Against InitiativePayersandProvidersNo ratings yet
- Healthcare Fraud in CanadaDocument28 pagesHealthcare Fraud in CanadaMartin McTaggartNo ratings yet
- Federal Judge Blocks Vaccine Mandate For Health Workers - The New York TimesDocument2 pagesFederal Judge Blocks Vaccine Mandate For Health Workers - The New York TimesGampa TurnerNo ratings yet
- The US government is suspending 暂停 its program of free home tests for CovidDocument2 pagesThe US government is suspending 暂停 its program of free home tests for Covid吴吴勉No ratings yet
- Rationing Health Care More FairlyDocument3 pagesRationing Health Care More FairlyicantbelievethisNo ratings yet
- Midwest Edition: States Taking Their Own ACA TackDocument6 pagesMidwest Edition: States Taking Their Own ACA TackPayersandProvidersNo ratings yet
- California Edition: Much of ACA Survives A SqueakerDocument7 pagesCalifornia Edition: Much of ACA Survives A SqueakerPayersandProvidersNo ratings yet
- California Edition: Blue Cross Backs Off Some IncreasesDocument6 pagesCalifornia Edition: Blue Cross Backs Off Some IncreasesPayersandProvidersNo ratings yet
- California Edition: The Long, Mysterious Appeals RoadDocument6 pagesCalifornia Edition: The Long, Mysterious Appeals RoadPayersandProvidersNo ratings yet
- California Edition: IHA Cites Medical Groups For QualityDocument6 pagesCalifornia Edition: IHA Cites Medical Groups For QualityPayersandProvidersNo ratings yet
- Health CareDocument5 pagesHealth Care6xmarkNo ratings yet
- California Edition: Rural Seniors in Healthcare BindDocument6 pagesCalifornia Edition: Rural Seniors in Healthcare BindPayersandProvidersNo ratings yet
- Payers & Providers Midwest Edition - Issue of May 8, 2012Document5 pagesPayers & Providers Midwest Edition - Issue of May 8, 2012PayersandProvidersNo ratings yet
- California Edition: Dual-Eligible Project Is LaunchedDocument7 pagesCalifornia Edition: Dual-Eligible Project Is LaunchedPayersandProvidersNo ratings yet
- Smart HospitalsDocument4 pagesSmart HospitalsCory WilsonNo ratings yet
- 59-4 HansenDocument3 pages59-4 Hansenvoruganty_vvsNo ratings yet
- Clinics Brace For CutsDocument4 pagesClinics Brace For Cutsapi-84383303No ratings yet
- Lake Forest Student Letters Final Draft - Arsh ShahDocument6 pagesLake Forest Student Letters Final Draft - Arsh ShahArsh Axis ShahNo ratings yet
- Hca 300 County ProfileDocument12 pagesHca 300 County Profileapi-487927401No ratings yet
- Midwest Edition: Illinois Swings Machete at Safety NetDocument6 pagesMidwest Edition: Illinois Swings Machete at Safety NetPayersandProvidersNo ratings yet
- Midwest Edition: Michigan Has A $1 Billion QuestionDocument5 pagesMidwest Edition: Michigan Has A $1 Billion QuestionPayersandProvidersNo ratings yet
- Americans' Medical Debts Are Bigger Than Was Known, Totaling $140 Billion - The New York TimesDocument3 pagesAmericans' Medical Debts Are Bigger Than Was Known, Totaling $140 Billion - The New York TimesMinh MinhNo ratings yet
- Updatelitreview AndrewsDocument5 pagesUpdatelitreview Andrewsapi-583764833No ratings yet
- Midwest Edition: AHA Examines Community ServicesDocument5 pagesMidwest Edition: AHA Examines Community ServicesPayersandProvidersNo ratings yet
- Peer Reviewed Second DraftDocument8 pagesPeer Reviewed Second DraftZnaLeGrandNo ratings yet
- Midwest Edition: From Cars To Catheters in MichiganDocument5 pagesMidwest Edition: From Cars To Catheters in MichiganPayersandProvidersNo ratings yet
- Midwest Edition: Cost-Cutting Measures in MissouriDocument5 pagesMidwest Edition: Cost-Cutting Measures in MissouriPayersandProvidersNo ratings yet
- Medical Coding and Compliance NIHDocument18 pagesMedical Coding and Compliance NIHBrandi TadlockNo ratings yet
- Essay 3 - Daivon BrownDocument6 pagesEssay 3 - Daivon Brownapi-644111810No ratings yet
- Midwest Edition: in Twin Cities, Improvement, GapsDocument6 pagesMidwest Edition: in Twin Cities, Improvement, GapsPayersandProvidersNo ratings yet
- US Department of Justice Official Release - 01502-05 Civ 489Document3 pagesUS Department of Justice Official Release - 01502-05 Civ 489legalmattersNo ratings yet
- Fact and OpinionDocument4 pagesFact and OpinionEstu MbaitaNo ratings yet
- Supervisor Janet Nguyen's Presentation On Orange County Grand Jury Report.Document20 pagesSupervisor Janet Nguyen's Presentation On Orange County Grand Jury Report.PayersandProvidersNo ratings yet
- Payers & Providers National Edition - Issue of October 2012Document8 pagesPayers & Providers National Edition - Issue of October 2012PayersandProvidersNo ratings yet
- Midwest Edition: Ford Merger Likely To DisappointDocument5 pagesMidwest Edition: Ford Merger Likely To DisappointPayersandProvidersNo ratings yet
- California Edition: Health Net, DHCS Settle Rate LawsuitDocument5 pagesCalifornia Edition: Health Net, DHCS Settle Rate LawsuitPayersandProviders100% (1)
- Midwest Edition: Sequester May Hit Health ResearchDocument5 pagesMidwest Edition: Sequester May Hit Health ResearchPayersandProvidersNo ratings yet
- Payers & Providers California Edition - Issue of October 25, 2012Document5 pagesPayers & Providers California Edition - Issue of October 25, 2012PayersandProvidersNo ratings yet
- Payers & Providers Midwest Edition - Issue of November 6, 2012Document5 pagesPayers & Providers Midwest Edition - Issue of November 6, 2012PayersandProvidersNo ratings yet
- Payers & Providers California Edition - Issue of November 1, 2012Document5 pagesPayers & Providers California Edition - Issue of November 1, 2012PayersandProvidersNo ratings yet
- California Edition: Dignity Health Facing ChallengesDocument5 pagesCalifornia Edition: Dignity Health Facing ChallengesPayersandProvidersNo ratings yet
- Midwest Edition: Vouchers Could Spike PremiumsDocument5 pagesMidwest Edition: Vouchers Could Spike PremiumsPayersandProvidersNo ratings yet
- Payers & Providers California Edition - Issue of October 18, 2012Document5 pagesPayers & Providers California Edition - Issue of October 18, 2012PayersandProvidersNo ratings yet
- Midwest Edition: Michigan Has A $1 Billion QuestionDocument5 pagesMidwest Edition: Michigan Has A $1 Billion QuestionPayersandProvidersNo ratings yet
- California Edition: Dignity Health Facing ChallengesDocument5 pagesCalifornia Edition: Dignity Health Facing ChallengesPayersandProvidersNo ratings yet
- California Edition: Dignity Health Facing ChallengesDocument5 pagesCalifornia Edition: Dignity Health Facing ChallengesPayersandProvidersNo ratings yet
- Payers & Providers Midwest Edition - Issue of September 25. 2012Document5 pagesPayers & Providers Midwest Edition - Issue of September 25. 2012PayersandProvidersNo ratings yet
- Payers & Providers National Edition - Issue of September 2012Document8 pagesPayers & Providers National Edition - Issue of September 2012PayersandProvidersNo ratings yet
- Payers & Providers Midwest Edition - Issue of October 2, 2012Document5 pagesPayers & Providers Midwest Edition - Issue of October 2, 2012PayersandProvidersNo ratings yet
- Payers & Providers Midwest Edition - Issue of October 9, 2012Document5 pagesPayers & Providers Midwest Edition - Issue of October 9, 2012PayersandProvidersNo ratings yet
- Payers & Providers California Edition - Issue of October 4, 2012Document5 pagesPayers & Providers California Edition - Issue of October 4, 2012PayersandProvidersNo ratings yet
- California Edition: IHA Cites Medical Groups For QualityDocument6 pagesCalifornia Edition: IHA Cites Medical Groups For QualityPayersandProvidersNo ratings yet
- Midwest Edition: Healthpartners, Park Nicollet MergeDocument5 pagesMidwest Edition: Healthpartners, Park Nicollet MergePayersandProvidersNo ratings yet
- California Edition: State's Hospitals Make Quality GainsDocument6 pagesCalifornia Edition: State's Hospitals Make Quality GainsPayersandProvidersNo ratings yet
- Midwest Edition: UM Docs Slash Dual-Eligible CostsDocument5 pagesMidwest Edition: UM Docs Slash Dual-Eligible CostsPayersandProvidersNo ratings yet
- Payers & Providers California Edition - Issue of September 6, 2012Document6 pagesPayers & Providers California Edition - Issue of September 6, 2012PayersandProvidersNo ratings yet
- Payers & Providers National Edition - Issue of August 2012Document8 pagesPayers & Providers National Edition - Issue of August 2012PayersandProvidersNo ratings yet
- Payers & Providers California Edition - Issue of September 13, 2012Document6 pagesPayers & Providers California Edition - Issue of September 13, 2012PayersandProvidersNo ratings yet
- Payers & Providers Midwest Edition - Issue of August 28, 2012Document5 pagesPayers & Providers Midwest Edition - Issue of August 28, 2012PayersandProvidersNo ratings yet
- Payers & Providers California Edition - Issue of August 30, 2012Document6 pagesPayers & Providers California Edition - Issue of August 30, 2012PayersandProvidersNo ratings yet
- California Edition: The Long, Mysterious Appeals RoadDocument6 pagesCalifornia Edition: The Long, Mysterious Appeals RoadPayersandProvidersNo ratings yet
- Midwest Edition: Wellpoint at Bottom of Hospitals' ListDocument5 pagesMidwest Edition: Wellpoint at Bottom of Hospitals' ListPayersandProvidersNo ratings yet
- Rules For Planning and Conducting Audits: Rainforest AllianceDocument41 pagesRules For Planning and Conducting Audits: Rainforest AlliancenisbabaNo ratings yet
- Management System Audit Report Executive SummaryDocument31 pagesManagement System Audit Report Executive Summarybabu541No ratings yet
- Akg Exim Limited Akg Exim Limited Akg Exim Limited: Annual Report Annual Report 2019-2020Document80 pagesAkg Exim Limited Akg Exim Limited Akg Exim Limited: Annual Report Annual Report 2019-2020Nihit SandNo ratings yet
- Butterfly Marketing LimitedDocument66 pagesButterfly Marketing LimitedSadia PressNo ratings yet
- At Quizzer 3 - (Profl Responsibilities) FEU MakatiDocument15 pagesAt Quizzer 3 - (Profl Responsibilities) FEU Makatiiyah100% (1)
- F08120000220104012F0812 P12 Behavioural Research in AccountingDocument34 pagesF08120000220104012F0812 P12 Behavioural Research in AccountingHasim kunNo ratings yet
- Warranty Manaul PDFDocument88 pagesWarranty Manaul PDFjfcr1234No ratings yet
- Specification 201 Quality ManagementDocument74 pagesSpecification 201 Quality Managementstuart lowdenNo ratings yet
- Review #14-019 Bayfront Park VIP Complimentary Tickets - FINALDocument17 pagesReview #14-019 Bayfront Park VIP Complimentary Tickets - FINALal_crespoNo ratings yet
- The Indonesia Corporate Governance Manual First EditionDocument533 pagesThe Indonesia Corporate Governance Manual First EditionRyan Hegar SuryadinathaNo ratings yet
- SMETA Guidance Workflow AuditorsDocument1 pageSMETA Guidance Workflow AuditorsSam SmithNo ratings yet
- Practice Questions Psa 210 Amp 300Document10 pagesPractice Questions Psa 210 Amp 300Trixie Pearl TompongNo ratings yet
- SMPFC Final Prospectus 8 Feb 20111Document263 pagesSMPFC Final Prospectus 8 Feb 20111mon samboNo ratings yet
- Guide To Completing A SMETA CAPR 6.1Document29 pagesGuide To Completing A SMETA CAPR 6.1Alexchandar AnbalaganNo ratings yet
- Quality and ReliabilityDocument9 pagesQuality and ReliabilityForger ForgerNo ratings yet
- Arens14e Ch06 PPT GeDocument38 pagesArens14e Ch06 PPT GeYogeswari RavindranNo ratings yet
- Financial Statement Audit ProcessDocument3 pagesFinancial Statement Audit ProcesssajiahNo ratings yet
- Key Changes AS9100:2016Document67 pagesKey Changes AS9100:2016Armand LiviuNo ratings yet
- OTHM Level 6 Occupational Health and Safety Spec 2021 01Document49 pagesOTHM Level 6 Occupational Health and Safety Spec 2021 01Waqas Akram MuhammadNo ratings yet
- Yalla Group May 2021 Swan Street ResearchDocument31 pagesYalla Group May 2021 Swan Street Researchnone foundNo ratings yet
- PA00TVKPDocument49 pagesPA00TVKPAkm EngidaNo ratings yet
- AIB Standards of InspectionDocument62 pagesAIB Standards of InspectionRekta DEPNo ratings yet
- COA Sec2 DigestsDocument3 pagesCOA Sec2 DigestsAmberChanNo ratings yet
- Brochure Certification Final VersionDocument2 pagesBrochure Certification Final Versionudiptya_papai2007No ratings yet
- Fixed AssetsDocument10 pagesFixed AssetsMikka JoyNo ratings yet
- The Marketing Audit and Business PerformanceDocument11 pagesThe Marketing Audit and Business PerformanceWassim SebtiNo ratings yet
- 5 6318691500020466224-1Document5 pages5 6318691500020466224-1shuchim guptaNo ratings yet
- Duties and Responsibilities of A DDODocument5 pagesDuties and Responsibilities of A DDOAamir GhaziNo ratings yet