Professional Documents
Culture Documents
Peritonitis
Uploaded by
Diane ArgoteOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Peritonitis
Uploaded by
Diane ArgoteCopyright:
Available Formats
Student Nurses Community
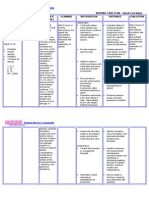
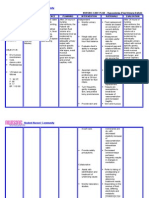
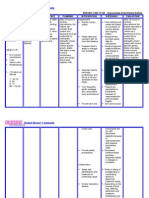
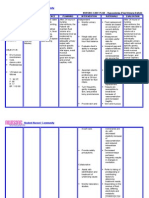
NURSING CARE PLAN Peritonitis ASSESSMENT SUBJECTIVE: Sumasakit ang tiyan ko at nasusuko ako (I've been
experiencing abdominal pain and I feel nauseous) as
DIAGNOSIS Deficient (mixed) fluid volume may be related to fluid shifts from extracellular, intravascular, and interstitial compartments into intestines and/or peritoneal space; vomiting; medically restricted intake; nasogastric or intestinal aspiration; fever; hypermetabolic state.
INFERENCE Peritonitis is an acute inflammation of the visceral/parietal peritoneum and endothelial lining of the abdominal cavity, or peritoneum. Peritonitis can be classified as primary or secondary, localized or generalized. When the peritoneal cavity is contaminated by bacteria, the body initially produces an inflammatory reaction that walls off a localized area to fight the infection. If this walling off process fails, the inflammation spreads and contamination becomes massive, resulting in diffuse peritonitis.
PLANNING After 8 hours of nursing interventions, the Patient will demonstrate improved fluid balance as evidenced by adequate urinary output with normal specific gravity, stable vital signs, moist mucous membranes, good skin turgor, prompt capillary refill, and weight within acceptable range.
INTERVENTION Independent Monitor vital signs, noting presence of hypotension (including postural changes), tachycardia, and fever. Measure central venous pressure (CVP) if available. Maintain accurate intake and output and correlate with daily weights. Include measured and estimated losses, such as with gastric suction, drains, dressing, hemovacs, diaphoresis, and abdominal girth for third spacing fluid. Measure urine specific gravity.
RATIONALE Aids in evaluating degree of fluid deficit, effectiveness of fluid replacement therapy, and response to medications. Reflects over all hydration status.
EVALUATION After 8 hours of nursing interventions, the Patient was able to demonstrate improved fluid balance as evidenced by adequate urinary output with normal specific gravity, stable vital signs, moist mucous membranes, good skin turgor, prompt capillary refill, and weight within acceptable range.
verbalized by the patient.
OBJECTIVE: Dry mucous membranes Poor skin turgor Weak peripheral pulses V/S taken as follows T: 36.5C P: 49 R: 14 BP: 110/ 80
Reflects hydration
status and changes in renal function, which may warn of developing acute renal failure in response to hypovolemia and effect of toxins. Hypovolemia, fluid shifts, and
Observe skin and mucous membrane dryness and turgor.
Student Nurses Community
nutritional deficits contribute to skin turgor and taut edematous tissues. Reduces gastric stimulation and vomiting response. Edematous tissue with compromised circulation is prone to breakdown. Provides information about hydration and organ function. Reduces vomiting caused by hyperactivity of bowel; manages stomach and intestinal fluids.
Eliminate noxious sights or smells from environment. Change position frequently, provide frequent skin care, and maintain, dry wrinkle-free bedding.
Collaborative Monitor laboratory studies.
Maintain NPO status with NG or intestinal aspiration.
Student Nurses Community
Student Nurses Community
Student Nurses Community
Student Nurses Community
You might also like
- Case No 45: of Intermittent Abdominal Pain Abdominal Bloating and Nausea and Vomiting (NVDocument17 pagesCase No 45: of Intermittent Abdominal Pain Abdominal Bloating and Nausea and Vomiting (NVPremiums of the RoseNo ratings yet
- Nursing Care PlanDocument14 pagesNursing Care PlanVin Landicho100% (1)
- Acute Renal Failure Nursing Care PlanDocument15 pagesAcute Renal Failure Nursing Care PlanRanusha AnushaNo ratings yet
- Plan of Care For:: Nursing Diagnosis: Excess Fluid VolumeDocument3 pagesPlan of Care For:: Nursing Diagnosis: Excess Fluid VolumeKenji CadizNo ratings yet
- Antepartum HemorrhageDocument3 pagesAntepartum Hemorrhagenur1146No ratings yet
- Managing COPD ExacerbationDocument17 pagesManaging COPD ExacerbationSean Menard Flores100% (1)
- Nursing Students Peritonitis Care PlanDocument2 pagesNursing Students Peritonitis Care PlanJide Manuel100% (1)
- Nursing Care Plan For LYING inDocument4 pagesNursing Care Plan For LYING inKarissa CiprianoNo ratings yet
- NCP PainDocument2 pagesNCP PainApril_Ivy_Raga_3835No ratings yet
- Nutrition diagnosis: Imbalanced nutrition less than requirementsDocument3 pagesNutrition diagnosis: Imbalanced nutrition less than requirementsIlisa ParilNo ratings yet
- Activity IntoleranceDocument6 pagesActivity IntoleranceRaidis PangilinanNo ratings yet
- CNN Practice QuestionsDocument5 pagesCNN Practice QuestionsUri Perez MontedeRamosNo ratings yet
- Scribd 020922 Case Study-Oncology A&kDocument2 pagesScribd 020922 Case Study-Oncology A&kKellie DNo ratings yet
- Acute TonsillopharyngitisDocument17 pagesAcute TonsillopharyngitisRachel Haide NaravalNo ratings yet
- NCPDocument15 pagesNCPCamille PinedaNo ratings yet
- LCPDDocument7 pagesLCPDakoismeNo ratings yet
- NCP FVDDocument1 pageNCP FVDsisjing88510No ratings yet
- Thoracentesis Reflective EssayDocument2 pagesThoracentesis Reflective EssayAnjae GariandoNo ratings yet
- NCPDocument2 pagesNCPNaidin Catherine De Guzman-AlcalaNo ratings yet
- Healthcare - Nursing Care Plan - Excess Fluid VolumeDocument4 pagesHealthcare - Nursing Care Plan - Excess Fluid VolumeBenjamin CañalitaNo ratings yet
- Nursing Care Plan Impaired Gas ExchangeDocument1 pageNursing Care Plan Impaired Gas ExchangeKarylle PetilNo ratings yet
- Peritoneal Dialysis WK 6Document3 pagesPeritoneal Dialysis WK 6Reem NurNo ratings yet
- Nursing Care Plan for Client with Major BurnDocument2 pagesNursing Care Plan for Client with Major BurnMaricel R. ManabatNo ratings yet
- Which It Is A Process Whereby Pancreatic Enzymes Destroy Its Own Tissue Leading ToDocument8 pagesWhich It Is A Process Whereby Pancreatic Enzymes Destroy Its Own Tissue Leading ToAriane-Gay Cristobal DuranNo ratings yet
- Impaired Tissue Integrity - CellulitisDocument3 pagesImpaired Tissue Integrity - CellulitisKelvin Kurt B. AgwilangNo ratings yet
- Hyperosmolar Hyperglycemic State (HHS)Document21 pagesHyperosmolar Hyperglycemic State (HHS)Malueth AnguiNo ratings yet
- Ostomy Nursing Care and ManagementDocument5 pagesOstomy Nursing Care and ManagementLara GatbontonNo ratings yet
- 11 Digestion and Bowel Elimination 2019 (Nursing) Geriatric NursingDocument44 pages11 Digestion and Bowel Elimination 2019 (Nursing) Geriatric NursingDarla SaulerNo ratings yet
- Managing Upper GI Bleeding in a Male PatientDocument19 pagesManaging Upper GI Bleeding in a Male PatientMary Ann Garcia100% (1)
- Nursing Care Plan for Spinal Cord InjuryDocument3 pagesNursing Care Plan for Spinal Cord InjuryDan Leo UnicoNo ratings yet
- NCP BronchopneumoniaDocument8 pagesNCP BronchopneumoniaCrisantaCasliNo ratings yet
- Nursing Interventions CHFDocument3 pagesNursing Interventions CHFbanyenye25100% (1)
- Nursing Care Plan: Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Risk For ConstipationDocument4 pagesNursing Care Plan: Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Risk For Constipationkenneth_bambaNo ratings yet
- How to treat and prevent breast engorgementDocument1 pageHow to treat and prevent breast engorgementkurniaNo ratings yet
- NCP Micu Hascvd Cad - RioDocument5 pagesNCP Micu Hascvd Cad - RioRio BonifacioNo ratings yet
- Client Assessment BasicsDocument56 pagesClient Assessment Basicsdanny_ng080% (1)
- Osteomalacia Care Plan/OthersDocument11 pagesOsteomalacia Care Plan/OthersJill Jackson, RNNo ratings yet
- Asthma Nanda Diagnoses Goals InterventionsDocument4 pagesAsthma Nanda Diagnoses Goals InterventionsZinya RobinsonNo ratings yet
- Fluid VolumeDocument2 pagesFluid Volumecoldfire28No ratings yet
- ANTENATAL CARE Translate GooglingDocument26 pagesANTENATAL CARE Translate GooglingLutfi ari206100% (2)
- Decreased Cardiac OutputDocument4 pagesDecreased Cardiac OutputAdnan Khan100% (1)
- 51 100Document18 pages51 100Jaessa Feliciano100% (1)
- NCPDocument10 pagesNCPCristina L. JaysonNo ratings yet
- DM & DI ExamsDocument11 pagesDM & DI ExamsTomzki CornelioNo ratings yet
- Nursing Care Plan EportfolioDocument14 pagesNursing Care Plan Eportfolioapi-279212367No ratings yet
- Hypertension NclexDocument5 pagesHypertension Nclexハニファ バランギNo ratings yet
- Diverticular DiseaseDocument8 pagesDiverticular Diseasenurse_enzo100% (1)
- Nursing Care Plan: IndependentDocument1 pageNursing Care Plan: IndependentJay Mar BabateNo ratings yet
- Nursing Care Plan Renal FailureDocument18 pagesNursing Care Plan Renal FailureKundan KumarNo ratings yet
- Digestive System 2Document32 pagesDigestive System 2Johnmer AvelinoNo ratings yet
- Perforated PeritonitisDocument5 pagesPerforated PeritonitisDeepak singh ratheeNo ratings yet
- Nursing Diagnosis For AppendicitisDocument1 pageNursing Diagnosis For AppendicitisTweenie DalumpinesNo ratings yet
- Liver Cirrhosis Care PlanDocument3 pagesLiver Cirrhosis Care PlanWendy EscalanteNo ratings yet
- Assessment Diagnosis Planning Nursing Intervention Rationale EvaluationDocument2 pagesAssessment Diagnosis Planning Nursing Intervention Rationale Evaluationjennelyn losantaNo ratings yet
- Care of Patients with Chest Drainage SystemsDocument29 pagesCare of Patients with Chest Drainage SystemsMSc. PreviousNo ratings yet
- Impaired Physical Mobility R/T Neuromuscular ImpairmentDocument3 pagesImpaired Physical Mobility R/T Neuromuscular ImpairmentjisooNo ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- PERITONITISDocument27 pagesPERITONITISTiffany Adrias100% (1)
- Hypovolemia Nursing Care PlanDocument2 pagesHypovolemia Nursing Care PlanLyn Reyes100% (1)
- Deficit)Document2 pagesDeficit)goldenboyjNo ratings yet
- Deficit)Document2 pagesDeficit)Lee DeeNo ratings yet
- CTDocument1 pageCTDiane ArgoteNo ratings yet
- CommonDocument1 pageCommonDiane ArgoteNo ratings yet
- DDDD DDDD DDDDDocument1 pageDDDD DDDD DDDDDiane ArgoteNo ratings yet
- HolesDocument1 pageHolesDiane ArgoteNo ratings yet
- MaximsDocument1 pageMaximsDiane ArgoteNo ratings yet
- CPR: Lifesaving Technique for Cardiac & Respiratory EmergenciesDocument5 pagesCPR: Lifesaving Technique for Cardiac & Respiratory EmergenciesMukesh KumarNo ratings yet
- Biomedical Admissions Test - Past Paper 2009 Section 1: Answer KeyDocument2 pagesBiomedical Admissions Test - Past Paper 2009 Section 1: Answer Keyhirajavaid246No ratings yet
- Procedures in O&GDocument7 pagesProcedures in O&GAbdulrahman NajiNo ratings yet
- Ards Prone PositionDocument9 pagesArds Prone PositionAnonymous XHK6FgHUNo ratings yet
- Quality Issu in Midwifery ICM PDFDocument9 pagesQuality Issu in Midwifery ICM PDFFarhatiNo ratings yet
- The Acute Scrotum: DR - Dwimantoro Iman P, SpuDocument24 pagesThe Acute Scrotum: DR - Dwimantoro Iman P, SpuAanisah Ikbaar SayyidahNo ratings yet
- Headache PDFDocument92 pagesHeadache PDFRohamonangan TheresiaNo ratings yet
- Addis Ababa Sciece and Technology University Collage of Biological and Chemical Engineering Department of BiotechnologyDocument14 pagesAddis Ababa Sciece and Technology University Collage of Biological and Chemical Engineering Department of BiotechnologyEshetu ShemetNo ratings yet
- Knowledge Attitude and Practices of Oral Hygiene ADocument5 pagesKnowledge Attitude and Practices of Oral Hygiene APatrycia Solavide SijabatNo ratings yet
- Best Dentists in Delhi. ToDocument9 pagesBest Dentists in Delhi. Torohit22221No ratings yet
- Duty Report 02-09-2023 MFDDocument20 pagesDuty Report 02-09-2023 MFDDede KurniawanNo ratings yet
- Latch ScoreDocument1 pageLatch ScoreAnnie LijinNo ratings yet
- The Health Bank (THB) Connected Care Program A Pilot Study of Remote Monitoring For The Management of Chronic Conditions Focusing On DiabetesDocument5 pagesThe Health Bank (THB) Connected Care Program A Pilot Study of Remote Monitoring For The Management of Chronic Conditions Focusing On DiabetesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- mmc1 PDFDocument48 pagesmmc1 PDFAnthony LachNo ratings yet
- Symptoms of A Stomach Ulcer - Ulcers of The StomachDocument3 pagesSymptoms of A Stomach Ulcer - Ulcers of The StomachmeoluoinhacNo ratings yet
- NMJ Special OncologyDocument24 pagesNMJ Special OncologyMalcolm LeeNo ratings yet
- Sample Legal Letter of Notice To Principles and School NursesDocument2 pagesSample Legal Letter of Notice To Principles and School NursesJimUKNo ratings yet
- 2 The Baby Friendly Hospital Initiative Final 2Document31 pages2 The Baby Friendly Hospital Initiative Final 2v_vijayakanth7656No ratings yet
- 4.3.1 Triage in Light of Four Hour TargetDocument16 pages4.3.1 Triage in Light of Four Hour TargetWilliam Wagner Müller XavierNo ratings yet
- LIS 141 Report - Medical TermsDocument14 pagesLIS 141 Report - Medical TermsR.B. DavilaNo ratings yet
- Unsafe Abortion PDFDocument66 pagesUnsafe Abortion PDFIntan Wahyu CahyaniNo ratings yet
- Crown 1Document1 pageCrown 1محمدعبده راشد الشاهريNo ratings yet
- SAM Management - Community & Facility Based CareDocument14 pagesSAM Management - Community & Facility Based CareArkadeb Kar100% (1)
- Jasim CVDocument3 pagesJasim CVjasimvet1985No ratings yet
- Risk Factors of Anastomotic Leak in Intestinal Surgery AuthorDocument2 pagesRisk Factors of Anastomotic Leak in Intestinal Surgery AuthorluisNo ratings yet
- 1.structure of The TeethDocument5 pages1.structure of The TeethCălin PavelNo ratings yet
- Vesalio Announces The Completion of Enrollment in Its FDA IDE Clinical Study For Acute Ischemic StrokeDocument3 pagesVesalio Announces The Completion of Enrollment in Its FDA IDE Clinical Study For Acute Ischemic StrokePR.comNo ratings yet
- Layout 2Document12 pagesLayout 2saddam ud dinNo ratings yet
- Syphilis in Pregnancy: Clinical Expert SeriesDocument15 pagesSyphilis in Pregnancy: Clinical Expert SeriesWindy MuldianiNo ratings yet