Professional Documents
Culture Documents
Angina Pectoris
Uploaded by
Blessy BreganzaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Angina Pectoris
Uploaded by
Blessy BreganzaCopyright:
Available Formats
Angina Pectoris Angina, or angina pectoris, is the medical term used to describe the temporary chest discomfort that
occurs when the heart is not getting enough blood.
The heart is a muscle (myocardium) and gets its blood supply from the coronary arteries. Blood carries the oxygen and nutrients the heart muscle needs to keep pumping. When the heart does not get enough blood, it can no longer function at its full capacity.
When physical exertion, strong emotions, extreme temperatures, or eating increase the demand on the heart, a person with angina feels temporary pain, pressure, fullness, or squeezing in the center of the chest or in the neck, shoulder, jaw, upper arm, or upper back. This is angina, especially if the discomfort is relieved by removing the stressor and/or taking sublingual (under the tongue) nitroglycerin.
The discomfort of angina is temporary, meaning a few seconds or minutes, not lasting hours or all day.
An episode of angina is not a heart attack. Having angina means you have an increased risk of having a heart attack.
A heart attack is when the blood supply to part of the heart is cut off and that part of the muscle dies (infarction). Angina can be a helpful warning sign if it makes the patient seek timely medical help and avoid a heart attack.
Prolonged or unchecked angina can lead to a heart attack or increase the risk of having a heart rhythm abnormality. Either of those could lead to sudden death. Time is very important in angina.
The more time the heart is deprived of adequate blood flow (ischemia), and thus oxygen, the more the heart muscle is at risk of heart attack or heart rhythm abnormalities. The longer the patient experiences chest pain from angina, the more the heart muscle is at risk of dying or malfunctioning. Not all chest pain is angina. Pain in the chest can come from a number of causes, which range from not serious to very serious.
o o o o
For example, chest pain can be caused by: acid reflux (gastroesophageal reflux disease, GERD), upper respiratory infection, asthma, or sore muscles and ligaments in the chest (chest wall pain) If chest pain is severe and/or recurrent, the patient should see a healthcare provider. Go to a hospital emergency department if the patient has any of the following with chest pain:
o o o
Other symptoms such as: sweating, weakness, faintness, numbness or tingling, or nausea Pain that does not go away after a few minutes Pain that is of concern in any way
Angina Pectoris Causes
Angina is classified as one of the following two types:
Stable angina Unstable angina
Stable Angina Stable angina is the most common angina, and the type most people mean when they refer to angina.
People with stable angina usually have angina symptoms on a regular basis. The episodes occur in a pattern and are predictable. For most people, angina symptoms occur after short bursts of exertion. Stable angina symptoms usually last less than five minutes. They are usually relieved by rest or medication, such as nitroglycerin under the tongue.
Unstable Angina Unstable angina is less common. Angina symptoms are unpredictable and often occur at rest.
This may indicate a worsening of stable angina, but sometimes the first time a person has angina it is already unstable.
The symptoms are worse in unstable angina - the pains are more frequent, more severe, last longer, occur at rest, and are not relieved by nitroglycerin under the tongue. Unstable angina is not the same as a heart attack, but it warrants an immediate visit to the healthcare provider or a hospital emergency department. The patient may need to be hospitalized to prevent a heart attack. If the patient has stable angina, any of the following may indicate worsening of the condition:
An angina episode that is different from the regular pattern Being awakened at night by angina symptoms More severe symptoms than usual Having angina symptoms more often than usual Angina symptoms lasting longer than usual
Coronary Heart Disease The most common cause for the heart not getting enough blood is coronary heart disease, also called coronary artery disease.
In this disease, the coronary arteries become blocked, narrowed, or otherwise damaged. They can no longer supply the heart with all of the blood it needs.
Most cases of coronary heart disease are caused by atherosclerosis (hardening of the arteries).
Atherosclerosis is a condition in which a fatty substance/cholesterol builds up inside the blood vessels.
These buildups are called plaques, and they can block blood flow through the vessels partially or completely. Multiple risk factors, particularly:
o o o o o
diabetes, high blood pressure, smoking, high cholesterol, and genetic predisposition may accelerate this build up.
Coronary Artery Spasm Another cause of unstable angina is coronary artery spasm.
Spasm of the muscles surrounding the coronary arteries causes them to narrow or close off temporarily. This blocks the flow of blood to the heart muscle for a brief time, causing angina symptoms. This is called variant angina or Prinzmetal angina. This is not the same as atherosclerosis, although some people have both conditions. The symptoms often come on at rest (or during sleep) and without apparent cause. Cocaine use/abuse can cause significant spasm of the coronary arteries and lead to a heart attack.
Other Causes
Other causes of angina symptoms include the following:
Blockage of a coronary artery by a blood clot or by compression from something outside the artery Inflammation or infection of the coronary arteries Injury to one or more coronary arteries Poor functioning of the tiny blood vessels of the heart (microvascular angina)
When a person has underlying atherosclerosis, spasm, or damage to the coronary arteries, angina symptoms usually are set off by one of the following triggers:
Physical exertion or exercise Emotional stress Exposure to cold Decreased oxygen content in the air you breathe (for example flying in an airplane or at high altitudes) Using a stimulant such as caffeine or smoking cigarettes (which lowers the amount of oxygen in the blood)
Risk Factors for Atherosclerosis and Angina Risk factors for atherosclerosis and angina include the following. Some of these are reversible.
High blood pressure (hypertension) High levels of cholesterol and other fats in the blood Diabetes Smoking Male gender Inactive (sedentary) lifestyle Family history of coronary heart disease Aging
Regular use of stimulants, especially nicotine, cocaine, or amphetamines: Other stimulants include theophyllines, inhaled beta-agonists, caffeine, diet pills, and decongesta
Angina Pectoris Symptoms
Angina itself is a symptom (or set of symptoms), not a disease. Any of the following may signal angina:
An uncomfortable pressure, fullness, squeezing, or pain in the center of the chest It may also feel like tightness, burning, or a heavy weight. The pain may spread to the shoulders, neck, or arms. It may be located in the upper abdomen, back, or jaw. The pain may be of any intensity from mild to severe.
Other symptoms may occur with an angina attack, as follows:
Shortness of breath Lightheadedness Fainting Anxiety or nervousness Sweating or cold, sweaty skin Nausea Rapid or irregular heart beat Pallor (pale skin) Feeling of impending doom
These symptoms are identical to the signs of an impending heart attack described by the American Heart Association. It is not always easy to tell the difference between angina and a heart attack, except angina only lasts a few minutes and heart attack pain does not go away.
If you have never had symptoms like this before, sit down. If you are able, call your healthcare provider, call 911, or go to the closest hospital emergency department. If you have had angina attacks before and this attack is similar to those, rest for a few minutes. Take your sublingual nitroglycerin. Your angina should be totally relieved in five minutes. If not, you may repeat the nitroglycerin dose and wait another five minutes. A third dose may be tried but if you still have no relief, call 911 or go to the nearest hospital emergency department.
When to Seek Medical Care
If the patient has never had these symptoms, can call the healthcare provider, especially if the patient is uncertain of the symptoms or what action to should take.
Do not delay calling 911. Do not wait for a call back from the doctor. Do not "wait it out." To wait is to risk your life. Emergency personnel are trained to recognize angina and to treat it rapidly and safely.
If the patient has had angina before, they may not need to seek medical care if the symptoms are the same as they always are.
If the patient has already been evaluated by a healthcare provider and received advice about how to react to these symptoms, follow that advice. This usually involves rest, removing the stressor, and taking sublingual nitroglycerin.
If the patient has had angina before, go to the nearest hospital emergency department if any of the following situations occur:
If the usual pattern of angina symptoms changes in any way If the symptoms are different than usual or more severe If the symptoms occur at rest or with less activity than usual If the symptoms do not get better with rest or sublingual nitroglycerin If the patient is not certain about what to do
Any of these situations may be a medical emergency and requires a visit to a hospital emergency department.
Don't delay or try to "wait it out." Do not drive yourself to the hospital. Call 911 for emergency medical transport.
If a person believes they have risk factors for angina, but no symptoms, they should call a healthcare provider to arrange for an evaluation in the office. Don't wait for symptoms to occur.
Exams and Tests
Upon hearing about the patient's symptoms, the primary healthcare provider or the provider in the emergency department will immediately think of angina and other heart problems. Time is of the essence - treatment will probably begin as the evaluation continues. An electrocardiogram (ECG) will be done.
This painless test checks for abnormalities in the beating of the heart.
Electrodes are attached to the chest and other points on the body. The electrodes read the electrical impulses linked to the beating of the heart. The ECG looks for signs of a heart attack or of impaired blood flow to the heart. For many patients with angina, the ECG result is normal.
The patient may have a chest x-ray. This will show any fluid buildup in the lungs. It can also rule out some other causes of chest pain. There is no blood lab test that can tell with certainty that someone is having angina. There are certain blood tests that suggest that a person may be having a heart attack. These tests may be done if a heart attack is suspected.
While these tests are going on, the healthcare provider will be asking questions to help with the diagnosis.
o o o o
The questions will be about the symptoms and about the patient's medical history: previous operations, medications, allergies, and habits and lifestyle. The physical exam will include listening to the heart and lungs and feeling the heart through the chest.
If, after these tests, the healthcare provider suspects the patient may have coronary heart disease, additional tests will be performed to confirm the possibility.
Exercise stress test: An ECG is taken before, during, and after exercise (usually walking on a treadmill) to detect inadequate blood flow to the heart muscle indirectly by changes on the ECG. This usually is done only for stable angina. Thallium stress test: This is a more complex and expensive test that injects a radioisotope into the circulation and indirectly detects parts of the heart that may not be getting enough blood during "stress" (usually walking on a treadmill, or after administration of a drug that mimics exercise in those unable to walk on the treadmill). This information indicates more accurately whether any of the coronary arteries may be narrowed, causing inadequate blood flow to the heart muscle or ventricle. Again, this is usually done only for stable angina.
Dobutamine echocardiogram stress test: This is done for people who cannot walk on a treadmill. A drug called dobutamine stimulates and speeds up the heart, creating an increased demand or need for blood flow tot he left ventricle or muscle. If the muscle shows a slowing of function on the ultrasound image of the heart muscle, then it indirectly indicates inadequate blood flow to the muscle.
Coronary angiogram (or arteriogram): This test of the coronary arteries is the most accurate but also the most invasive. It is a type of x-ray. A thin, plastic tube called a catheter is threaded through an artery in the arm or groin to one of the main coronary arteries. A contrast, or harmless dye is injected into the arteries. The dye depicts the arteries directly and shows any blockage more accurately than the above or more noninvasive procedures. The healthcare provider will make the decision about whether these tests or any treatment need to be done on an urgent basis. If so, the patient will be admitted to the hospital. If not, the tests will be scheduled for the next few days, and the patient may be allowed to go home.
Self-Care at Home
Stop doing whatever it is that causes the symptoms and call 911. Immediate help and intervention is the best chance for survival if someone is having a heart attack or other serious problem.
Lie down in a comfortable position with the head up.
Chew a regular adult aspirin or its equivalent (as long as the patient is not allergic to aspirin). Chewing more than one will not do any good and may cause unwanted side effects. If the patient has had angina before and been evaluated by a healthcare provider, follow his or her recommendations.
This may mean rest and the immediate use of sublingual nitroglycerin.
It may include a visit to the hospital emergency department.
Medical Treatment
If the patient has come to the hospital emergency department, they may be sent to another care area for further testing, treatment, or observation. On the basis of the provider's preliminary diagnosis, the patient may be sent to the following units:
An observation unit pending test results or further testing A cardiac care unit A cardiac catheterization unit
Regardless of where the patient is sent, several basic treatments may be started. Which ones are given depends on the severity of the symptoms and the underlying disease.
At least one IV line will be started. This line is used to give medication or fluids. Aspirin will probably be administered (unless the patient has already taken one)
Oxygen will be administered through a face mask or a tube in the nose. This will help if the patient is having trouble breathing or feeling uncomfortably short of breath. The direct administration of oxygen raises the oxygen content of the blood. Treatment will depend on the severity of the symptoms, severity of the underlying disease, and extent of damage to the heart muscle, if any.
Simple rest and observation, an aspirin, breathing oxygen, and sublingual nitroglycerin may be all that the patient needs, if it is only angina. Medication may be administered to reduce anxiety. Medication may be administered to lower blood pressure or heart rate. Medication may be administered to reduce the risk of having a blood clot or to prevent further clotting.
If the healthcare provider believes the chest pain actually represents a heart attack, the patient may be given a fibrinolytic (apowerful clot-buster medication). After reviewing the patient's immediate test results, the hospital healthcare provider will make a decision about where the patient should be for the next hours and days.
If the diagnosis of angina is made, and the patient is feeling better and their condition is stable they may be allowed to go home. The patient may be given medications to take. Follow-up with a primary healthcare provider within the next day or two will be recommended.
The patient will be admitted o the hospital if the they are unstable with continuing symptoms. Further testing will be ordered, and if the arteries are critically blocked, the patient may undergo coronary angiography, coronary artery angioplasty, or even coronary artery bypass surgery. Angioplasty is a treatment used for people whose angina does not get better with medication and/or who are at high risk of having a heart attack.
Before angioplasty can be done, the area(s) of coronary artery narrowing is located with coronary arteriography.
A thin plastic tube called a catheter is inserted into an artery in the arm or groin with local sedation. The catheter has a tiny balloon attached to the end. The catheter is threaded through the arteries and into the artery where the narrowing is. The balloon on the catheter is inflated, opening up the narrowing.
Following ballon treatment, many patients require placement of a "stent," a small metal sleeve that is placed in the narrowed artery. The stent holds the artery open. If the patient has had angina symptoms and is visiting their primary healthcare provider for evaluation, he or she will make a decision about how to proceed with the evaluation. The choices include going ahead with the evaluation on an outpatient basis, referring the patient to a specialist in heart disorders (cardiologist), or admitting the patient to the hospital for further workup. Nitroglycerin is a sublingual (under the tongue) medication relieves angina symptoms by expanding blood vessels and decreasing the muscle's need for oxygen. This allows more blood to flow through the coronary arteries. Nitroglycerin is taken only when the patient actually has symptoms or expect to have them. Slow - or long-acting nitroglycerin can be used as a preventative treatment for angina but not until beta blockers are tried first. Beta blockers: Beta blockers lessen the heart's workload. They slow the heart rate, decrease blood pressure, and lessen the force of contraction of the heart muscle. This decreases the heart's need for oxygen and thus decreases angina symptoms. Beta blockers are taken every day, regardless of whether the patient is having symptoms, because they are proven to prevent heart attacks and sudden death. Calcium channel blockers (CCBs): Calcium channel blockers are used primarily when beta blockers cannot be used and/or the patient is still having angina with beta blockers. Calcium channel blockers also lower blood pressure and certain ones slow heart rate. Calcium channel blockers have to be taken every day. Aspirin: Daily aspirin therapy is mandatory to decrease the possibility of sticky platelets in the blood starting a blood clot. Statins: Statins lower cholesterol and have been shown to stabilize the fatty plaque on the inner lining of the coronary artery, even when the blood cholesterol is normal or minimally increased. Low density lipoprotein (LDL) or "bad cholesterol" levels should be less than 70 mg/dL for those at high risk of heart disease. Every person with angina needs to know exactly what his or her blood lipids/fats are. Miscellaneous anti-anginal drugs: New drugs are being studied to treat angina. In 2006, the FDA approved ranolazine (Ranexa). Because of its side effects (potential to cause abnormal heart rhythm), ranolazine is indicated only after other conventional drug treatments are found to be ineffective.
Surgery
Like angioplasty, surgery is an option for people whose angina does not improve with medications and others who are at high risk of having a heart attack. Surgery is usually reserved for people with very severe narrowing or blockage in several coronary arteries. In almost all cases, the operation used for severely narrowed coronary arteries is coronary artery bypass grafting. Coronary Artery Bypass Surgery
The chest and rib cage are opened up (open heart surgery)
The narrowed part of the artery is bypassed by a piece of vein removed from the leg, or with a piece of artery behind the sternum (internal mammary artery), or a portion of the radial artery taken from the lower arm or forearm. Several arteries can be bypassed in one operation.
This is a very safe operation, with a mortality rate of less than 1%, in people whose heart muscle is not severely damaged irreversibly and who have normal lungs, kidneys, liver, and other organs. Because the chest is opened, the recovery time can be quite long, especially if the patient is older and has multiple other health problems. Transmyocardial Revascularization Transmyocardial revascularization is a procedure for people who cannot undergo angioplasty or surgery.
A simple incision is made in the chest, and a laser is used to "drill" small holes through the outside wall of the heart into the left ventricle. About 20-40 holes are made. Bleeding from these holes is minimal and usually stops after a few minutes of pressure.
It is not clear why this helps relieve angina. One theory is that it stimulates growth of new blood vessels that improve blood flow to the heart. Other investigators believe it is a placebo effect. Current research is focusing on trying to find growth factors that could be injected into coronary arteries or directly into the left ventricle to encourage growth of new blood vessels.
Next Steps Follow-up
If a patient has stable angina, they will need to visit their healthcare provider on a regular basis to monitor angina episodes and assess if risk factors are being reduced. The patient's healthcare provider will probably test their heart function periodically and assess the underlying disease. These tests will probably include the following:
ECG Exercise tolerance tests Thallium stress test
Repeat cardiac catheterization to see if the dilated artery or stent is still open and/or a surgical bypass graft is still open or closed. This is the key downside of both angioplasty and surgery: arteries, stents, and grafts restenose (occlude) with the same disease process of atherosclerosis. None of these procedures are a permanent cure. The patient has to be very compulsive in correcting potential risk factors, or they will return with the same blockages they started with.
Prevention
The best action is to reduce risk factors early in life. The goal is to not have angina, a heart attack, or sudden death in the first place. Although no one can escape aging, inherited risk, or gender, certain risk factors are in your control.
Stop smoking and using nicotine in any form. Control high blood pressure.
Lower blood fats (through diet, exercise, and medications). Maintain a healthy weight. Control diabetes and blood sugar Do not use stimulants such as cocaine or amphetamines.
If a person already has atherosclerosis and angina, they can learn to take precautions to avoid having symptoms. Avoiding the "triggers" will help keep the person comfortable and free of symptoms.
Quit smoking Do not use caffeine, cocaine, amphetamines, or other stimulants Drink alcohol moderately (no more than 1-2 drinks daily) Avoid large and heavy meals that leave you feeling "stuffed" Decrease stress Establish a regular exercise routine (discuss the plan with your healthcare provider)
The question of exercise for a person with angina is important. Exercise is recommended.
If the patient has been exercising strenuously, they may need to cut back to avoid symptoms.
If the patient has not been exercising, or has been exercising moderately, talk to a healthcare provider first about physical activity that will be safe and comfortable. Sometimes a structured cardiac rehabilitation program is a beneficial way to begin an exercise program. The healthcare provider may recommend taking an aspirin daily.
Aspirin has been shown to reduce the risk of a second heart attack in people who have already had one, and may reduce the risk of a first heart attack. Taking aspirin is not without risks, especially in elderly people, people with digestive diseases or blood clotting disorders, and people who take certain types of medications. Allergy to aspirin is not uncommon. Tell your healthcare provider if you are allergic to aspirin or have a reaction to aspirin.
Outlook
The most common and serious complications of coronary heart disease are heart attack and sudden death from cardiac arrest. A person's future depends on the severity of their condition, any heart muscle injury they have incurred, and their risk of heart rhythm abnormalities.
The outlook is good if there is no prior heart muscle injury and angina is relieved by rest. Reversing risk factors will increase the long-term chances of avoiding a heart attack.
Many authorities believe that some people can actually reverse plaque buildup through diet and exercise and reversing other risk factors for heart disease.
You might also like
- Bachelor of Laws Pre-Entry ExaminationDocument150 pagesBachelor of Laws Pre-Entry ExaminationKavuma Ernest100% (21)
- Angina Pectoris Diagnosis and TreatmentDocument23 pagesAngina Pectoris Diagnosis and TreatmentIllakiya Venkatesh67% (9)
- Heart DiseaseDocument38 pagesHeart DiseaseDr.Sunil KumarNo ratings yet
- Coronary AngiogramDocument58 pagesCoronary AngiogramEllaine Jennel100% (3)
- Overview On Peripheral Artery Disease - FinalDocument78 pagesOverview On Peripheral Artery Disease - FinalMITHANo ratings yet
- Atrial FibrillationDocument19 pagesAtrial FibrillationAnwari MuhammadNo ratings yet
- Outsmarting The Number One KillerDocument52 pagesOutsmarting The Number One Killerhusankar2103100% (1)
- Pathophysiology: Cardiovascular Diseases Coronary Artery Disease (CAD)Document5 pagesPathophysiology: Cardiovascular Diseases Coronary Artery Disease (CAD)Grace Bernadine H. Ramos100% (1)
- Coronary Heart DiseaseDocument11 pagesCoronary Heart DiseaseZaryna TohNo ratings yet
- Demystifying Interventional Radiology A Guide For Medical StudentsDocument195 pagesDemystifying Interventional Radiology A Guide For Medical StudentsMo Haroon100% (1)
- Lesson 13 - Diabetes, Cancer and Heart DiseaseDocument28 pagesLesson 13 - Diabetes, Cancer and Heart DiseaseAlejandro GuerreroNo ratings yet
- Unstable Angina, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandUnstable Angina, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Angina Pectoris, (Heart Chest Pain) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandAngina Pectoris, (Heart Chest Pain) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- Test Bank CardioDocument16 pagesTest Bank CardioLudwigJayBarayuga86% (7)
- CPG Management of Ischaemic Stroke (2nd Edition)Document64 pagesCPG Management of Ischaemic Stroke (2nd Edition)umiraihana1100% (1)
- Angina PectorisDocument29 pagesAngina Pectoriszabrynah100% (1)
- Respiratory SystemDocument15 pagesRespiratory SystemMonicaNo ratings yet
- Notes On History Taking in The Cardiovascular SystemDocument9 pagesNotes On History Taking in The Cardiovascular Systemmdjohar72100% (1)
- Medical AbbreviationsDocument21 pagesMedical AbbreviationsReachel Ann RonquilloNo ratings yet
- Heart CareDocument14 pagesHeart CareArman CareNo ratings yet
- Medical Surgical Nursing - Responses To Altered Tissue PerfusionDocument23 pagesMedical Surgical Nursing - Responses To Altered Tissue PerfusionLouise NicoleNo ratings yet
- Angina Pectoris OverviewDocument7 pagesAngina Pectoris OverviewamiemichieevNo ratings yet
- Heart Disease (Vargas)Document26 pagesHeart Disease (Vargas)Jhon Brian VargasNo ratings yet
- Angina Pectoris OverviewDocument6 pagesAngina Pectoris OverviewClarisse GomosNo ratings yet
- AnginaDocument8 pagesAnginaiyah_18No ratings yet
- Lecture 1 Medicine 1Document28 pagesLecture 1 Medicine 1Dr.Jamal ShahNo ratings yet
- Angina Symptoms, Causes, Tests and TreatmentDocument33 pagesAngina Symptoms, Causes, Tests and TreatmentAnonymous mIw67bMXNo ratings yet
- Angina PectorisDocument3 pagesAngina PectorisKhalid Mahmud Arifin100% (2)
- Unstable Angina: CausesDocument5 pagesUnstable Angina: CausesMahnoorNo ratings yet
- Heart Attack: by Chris MclarenDocument16 pagesHeart Attack: by Chris MclarenBheru LalNo ratings yet
- Differential Diagnosis of Cardiovascular SystemDocument50 pagesDifferential Diagnosis of Cardiovascular Systemkashmala afzalNo ratings yet
- Cad - AcsDocument40 pagesCad - Acssmart reyNo ratings yet
- Angina Chest Pain CausesDocument8 pagesAngina Chest Pain CausesDarryl SpencerNo ratings yet
- AnginaDocument8 pagesAnginaahmed02_99No ratings yet
- Angina 2Document3 pagesAngina 2Afdol Triatmojo SikumbangNo ratings yet
- Patient/Family Information Sheet What Is Angina?Document2 pagesPatient/Family Information Sheet What Is Angina?iri_balNo ratings yet
- Angina Pectoris Symptoms: NitroglycerinDocument4 pagesAngina Pectoris Symptoms: NitroglycerinCatherine Jane SarmientoNo ratings yet
- Heart AttackDocument13 pagesHeart AttackSaadNo ratings yet
- AnginaDocument42 pagesAnginaDarius DsouzaNo ratings yet
- Coronary Artery Disease Symptoms: CholesterolDocument21 pagesCoronary Artery Disease Symptoms: CholesterolLau AngelNo ratings yet
- Unstable Angina PectorisDocument24 pagesUnstable Angina PectorisAkbar IskandarNo ratings yet
- CRS CSS: Atherosclerosis, Angina, and Acute Coronary SyndromesDocument58 pagesCRS CSS: Atherosclerosis, Angina, and Acute Coronary Syndromesre septian IlhamsyahNo ratings yet
- Emergency Department - AnginaDocument23 pagesEmergency Department - Anginahaya waqrNo ratings yet
- Myocardial Infarction: Alternative NamesDocument5 pagesMyocardial Infarction: Alternative NamesKhalid Mahmud ArifinNo ratings yet
- Chest PainDocument39 pagesChest Painni husNo ratings yet
- Heart Attack AnnaDocument7 pagesHeart Attack Annaannamuhamad81No ratings yet
- Angina PectorisDocument19 pagesAngina PectorisRenas SalayNo ratings yet
- 5+2 Chest PainDocument27 pages5+2 Chest PainMazen HossamNo ratings yet
- Angina Diagnosis and TreatmentDocument23 pagesAngina Diagnosis and TreatmentIllakiya Venkatesh100% (1)
- Heart Attack: Book: Mayo Clinic Healthy Heart For Life!Document3 pagesHeart Attack: Book: Mayo Clinic Healthy Heart For Life!Anonymous JOOQkGbwoRNo ratings yet
- Case 2Document105 pagesCase 2Ritz CelsoNo ratings yet
- Coronary Artery Disease Nclex, Peripheral Vascular DiseaseDocument88 pagesCoronary Artery Disease Nclex, Peripheral Vascular DiseaseKrishna SapkotaNo ratings yet
- Angina pectoris symptoms, causes, treatmentDocument2 pagesAngina pectoris symptoms, causes, treatmentannisa yunita raniNo ratings yet
- HLTAID003 - Provide First Aid Slideshow 4 Chest PainDocument9 pagesHLTAID003 - Provide First Aid Slideshow 4 Chest Painiftekhar islamNo ratings yet
- MedTech Heart DiseasesDocument10 pagesMedTech Heart DiseasesGina MarieNo ratings yet
- 2 - Ischemic Heart DiseaseDocument42 pages2 - Ischemic Heart Diseasesamar yousif mohamedNo ratings yet
- Coronary Heart DiseaseDocument7 pagesCoronary Heart DiseaseAusaf AhmedNo ratings yet
- Pharmacotherapeutics AssignmentDocument14 pagesPharmacotherapeutics AssignmentKaneez ZehraNo ratings yet
- Notes On History Taking in The Cardiovascular SystemDocument10 pagesNotes On History Taking in The Cardiovascular Systemmdjohar72No ratings yet
- Angina Chest Pain Causes TypesDocument5 pagesAngina Chest Pain Causes TypesjackcharlieNo ratings yet
- Angina Pectoris PDFDocument5 pagesAngina Pectoris PDFolueabukola147No ratings yet
- Chest Pain Causes GuideDocument4 pagesChest Pain Causes Guidertishaii18No ratings yet
- Heart AttackDocument2 pagesHeart AttackًNo ratings yet
- Heart AtackDocument6 pagesHeart AtackUSMP FN ARCHIVOSNo ratings yet
- Angina Pectoris (Stable Angina) : Coronary Heart Disease IschemiaDocument2 pagesAngina Pectoris (Stable Angina) : Coronary Heart Disease IschemiaiamSiEnnNo ratings yet
- Coronary Artery Disease Education for PatientsDocument26 pagesCoronary Artery Disease Education for PatientsPaz Aymar Escarcena EscobarNo ratings yet
- Lec 4 باطنيهDocument12 pagesLec 4 باطنيهmaraymalani9090No ratings yet
- Heart Attack: Most Common SymptomsDocument2 pagesHeart Attack: Most Common SymptomsVinceNo ratings yet
- Angina PectorisDocument17 pagesAngina PectorisRacel HernandezNo ratings yet
- Angina: (an-JI-nuh or AN-juh-nuh)Document9 pagesAngina: (an-JI-nuh or AN-juh-nuh)yeohstNo ratings yet
- Symptoms: Heart Failure Blood Clots AneurysmDocument7 pagesSymptoms: Heart Failure Blood Clots Aneurysmjohn mendozaNo ratings yet
- 111 Case Study 4Document3 pages111 Case Study 4jabyleynesNo ratings yet
- Transplatation and Ethics: Editors' SummaryDocument10 pagesTransplatation and Ethics: Editors' SummaryBlessy BreganzaNo ratings yet
- Abortion and Maternal Ethical IssueDocument10 pagesAbortion and Maternal Ethical IssueBlessy BreganzaNo ratings yet
- ChemistryDocument1 pageChemistryBlessy BreganzaNo ratings yet
- Ancylostoma DuodenaleDocument2 pagesAncylostoma DuodenaleBlessy BreganzaNo ratings yet
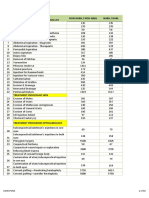
- Superspecialty Procedures Under DR YSR Aarogyasri - PC - 13.08.2019 - 001finalDocument18 pagesSuperspecialty Procedures Under DR YSR Aarogyasri - PC - 13.08.2019 - 001finalLokesh KuppiliNo ratings yet
- Chapter 12Document28 pagesChapter 12Muhammad AmirNo ratings yet
- Cathet Cardio Intervent - 2021 - Rocha Singh - Directional Atherectomy Before Paclitaxel Coated Balloon Angioplasty inDocument10 pagesCathet Cardio Intervent - 2021 - Rocha Singh - Directional Atherectomy Before Paclitaxel Coated Balloon Angioplasty inEnrique San NorbertoNo ratings yet
- PHYS 3616E Chap91Document15 pagesPHYS 3616E Chap91johnNo ratings yet
- Sample Patient ProfileDocument7 pagesSample Patient ProfileElisabeth CampbellNo ratings yet
- CARDIODocument10 pagesCARDIOkristineNo ratings yet
- Chapter 9 KeyDocument17 pagesChapter 9 KeySrinu WestNo ratings yet
- IGCSE BioDocument5 pagesIGCSE BioMajid DardasNo ratings yet
- Test Bank For Health Economics and Policy 5th Edition James W Henderson DownloadDocument24 pagesTest Bank For Health Economics and Policy 5th Edition James W Henderson DownloadCoryDuncancmyd100% (49)
- Ultrasound Guided Compression of Femoral PseudoaneurysmDocument2 pagesUltrasound Guided Compression of Femoral PseudoaneurysmIOSRjournalNo ratings yet
- List of 37 Critical IllnessDocument13 pagesList of 37 Critical IllnessdexterNo ratings yet
- Schedule D: List of Life Saveing or Life Sustaining Medical DevicesDocument5 pagesSchedule D: List of Life Saveing or Life Sustaining Medical DevicesAasma RehmanNo ratings yet
- CGHS Rates - PuneDocument46 pagesCGHS Rates - PunePrachi KhandelwalNo ratings yet
- Critical Limb IschemicDocument27 pagesCritical Limb IschemicErik Judika2No ratings yet
- Anatomy Intervention: AND OF Cerebral VasculatureDocument123 pagesAnatomy Intervention: AND OF Cerebral Vasculaturemira ariantiNo ratings yet
- Cardiac Catheterization - 4Document2 pagesCardiac Catheterization - 4Indranil SinhaNo ratings yet
- Mrs. Maria Eloisa Lim Chu Gungon: When You Reach Age 75 When You Reach Age 75 If The Insured Passes Away at Age 75Document11 pagesMrs. Maria Eloisa Lim Chu Gungon: When You Reach Age 75 When You Reach Age 75 If The Insured Passes Away at Age 75John Philip TiongcoNo ratings yet
- ICICI Pru Iprotect SmartDocument16 pagesICICI Pru Iprotect SmartVipul KumarNo ratings yet