Professional Documents
Culture Documents
Valvular Heart Dse
Uploaded by
Jaillah Reigne Cura0 ratings0% found this document useful (0 votes)
124 views8 pagesVALVULAR heart DISEASE Stenosed valve Insufficient (incompetent) Incidence Decreasing steadily 5% of the population is affected women > men I. MITRAL valve DISEASE Etiology and Risk Factors Rheumatic heart disease infectious endocarditis connective Tissue abnormality.
Original Description:
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentVALVULAR heart DISEASE Stenosed valve Insufficient (incompetent) Incidence Decreasing steadily 5% of the population is affected women > men I. MITRAL valve DISEASE Etiology and Risk Factors Rheumatic heart disease infectious endocarditis connective Tissue abnormality.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
124 views8 pagesValvular Heart Dse
Uploaded by
Jaillah Reigne CuraVALVULAR heart DISEASE Stenosed valve Insufficient (incompetent) Incidence Decreasing steadily 5% of the population is affected women > men I. MITRAL valve DISEASE Etiology and Risk Factors Rheumatic heart disease infectious endocarditis connective Tissue abnormality.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 8
Curu, Lorelyn June P.
BSN III-1 Page 1
ANGELES UNIVERSITY FOUNDATION
Angeles City
College of Nursing
Nursing Care Management 103
Handout for Management of Clients with Structural Cardiac Disorders
VALVULAR HEART DISEASE
Stenosed valve
Insufficient (incompetent)
Incidence
Decreasing steadily
One of the most common cardiac abnormalities mitral valve prolapsed
5% of the population is affected
Women > men
I. MITRAL VALVE DISEASE
Etiology and Risk Factors
Rheumatic Heart Disease
Infectious Endocarditis
Connective Tissue Abnormality
Myocardial Ischemia - blood flow in the heart
A. Mitral Stenosis
- Valve becomes calcified and immobile
- Valvular orifice narrows (normally 4 6 cm
2
)
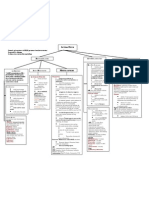
Pathophysiology:
Blood is not adequately pumped
from LA to LV during diastole
Inadequate filling of LV
(preload)
Pressure in LA elevates
Cardiac Output
Back pressure elevates Pulmonary
Venous & Pulmonary Capillary
Pressures
Pulmonary HTN
RV hypertrophy as it needs to pump
blood harder
MITRAL STENOSIS
Right-Side Heart Failure
RV failure can result
Hypertrophy
Curu, Lorelyn June P. BSN III-1 Page 2
Manifestations
Dyspnea, orthopnea, exercise tolerance, PND
Hemoptysis
Diastolic murmur
Systemic congestion
Opening snap is heard (apex) diaphragm
Atrial fibrillation common in mitral stenosis
Mural thrombi
Irregular pulse
Diet
Na restricted diet
Surgical Management
Percutaneous Balloon Valvuloplasty
Temporarily redues backflow by enhancing forward blood flow into the aorta
Note:
Mechanical mostly prescribed for children
- after 10 years it becomes 30% inefficient
- need anti-coagulant therapy
Tissue for adults
- less durable
- for clients with bleeding tendency
- for pregnant women
- no anti-coagulant therapy needed
B. Mitral Regurgitation
Pathophysiology
Backflow of blood from
LV to LA
Reduced amount of
blood flow to LV
Large amount of blood received
by the LA during systole
LV must pump harder
to pressure CO
LA hypertrophy/
LA pressure LV hypertrophy
Pulomonary
congestion
LV failure
RV hypertrophy since it has to pump
against a higher resistance
CO pulmonary
congestion
Right-side Heart
Failure
Systemic congestion
Curu, Lorelyn June P. BSN III-1 Page 3
Manifestation
Symptoms of CO
Fatigue, dyspnea, orthopnea, PND
Systolic murmur: blowing & high pitched, heard immediately after S
1
Changes in the mean capillary pressure
S
3
gallop: rapid in flow rate across mitral orifice
Manifestations of right-sided heart failure
Atrial fibrillation: irregular heart beat
Management
Pharmacologic Management
Diuretic
To decrease cardiac workload
Digitalis
Nitrates tx of angina
ACE inhibitors
Diet
Na restricted diet
Activity
Restriction of physical activities that produce fatigue and dyspnea
C. Mitral Valve Prolapse
Barlow Syndrome
Systolic Click Murmur Syndrome
Floppy Valve Syndrome
Pathophysiology
Manifestations
Asymptomatic
Regurgitant murmur with med systolic click
Tachycardia, palpitation r/t dysrhythmias
Lightheadedness, syncope, fatigue, weakness, dyspnea
Anxiety
Dyspnea & chest discomfort
Anterior & posterior cusps of mitral valve billow
upward into the atrium during systolic contraction
Chordae tendineae lengthen allowing the valve cusps
to stretch upward
Cusps enlarges & thickens
Regurgitation
Curu, Lorelyn June P. BSN III-1 Page 4
Management
Beta blockers
Aspirin
Antibiotics
Diet
Eliminate caffeine & alcohol from the diet
Surgical Mgt
Mitral valve replacement
II. AORTIC VALVE DISEASE
In aortic stenosis the orifice of the aortic valve becomes narrowed
Aortic regurgitation (insuffient) allows blood to leak back from the aorta to the
left ventricle
Both aortic stenosis and regurgitation overwork the left ventricle ventricle
hypertrophy
Etiology and Risk Factors
Congenital defects of the aortic valve
Calcification of the valve
Rheumatic Fever
A. Aortic Stenosis
Pathophysiology
Note:
Systole contraction
Diastole relaxation
Narrowed aortic valve
Blood not adequately pumped
from LV to aorta
Pressure in LV elevates during
systole
LV hypertrophy/Dilation
Elevated End-Diastolic Pressure
Decreased CO/LV Failure
Left-Side Heart Failure/
Pulmonary Congestion
Curu, Lorelyn June P. BSN III-1 Page 5
Manifestation
Gradually and late in the course of the disease
Angina pectoris in 66% (similar with CAD), dysrhythmias
Syncope during exertion due to fixed CO during periods of increased demand
Symptoms of left-sided heart failure
In severe AS: palpitation, fatigue, and visual disturbances
Systolic murmur
Early ejection click & systolic thrill
Management
Pharmacologic Mgt
Antibiotics
Diuretics
Digitalis
Activity
Avoid vigorous activity
Surgical Mgt
Aortic Valve Replacement
Percutaneous Balloon Valvuloplasty
B. Aortic Regurgitation
Pathophysiology
Manifestation
Even with severe AR, pts may be asymptomatic for a long time
Palpitation, fatigue
Prominent carotid artery pulsation and head-bobbing with each heartbeat (de
Musset sign)
Widening Pulse Pressure: high systolic in LV and low diastolic pressure in aorta
Diastolic murmur
Corrigans or water hammer pulse (sharp pulse then sudden collapse in diastolic
pressure)
Blood in the aorta flows back in the
LV through an incompetent valve
Volume overload in the LV
Increased left ventricular end
diastolic volume
Hypertrophy & dilation of left ventricle
Progression of condition leads to decline in contractility
Curu, Lorelyn June P. BSN III-1 Page 6
Management
Antibiotics
Diuretics
Digitalis
Beta blockers
Diet
Na restricted diet
Surgical Mgt
Aortic Valve replacement
III. TRICUSPID VALVE DISEASE
Tricuspid stenosis & regurgitation
Usually develops from rheumatic fever or in combination with other structural
disorders of the heart
right atrial pressure
A. Tricuspid Stenosis
Pathophysiology
Manifestation
Dyspnea, fatigue, jugular vein distention, peripheral edema & weight loss
Pulsation in the neck with prominent waves
Diastolic murmur is heard best along the left lower sterna border
Management
Diuretics
Digitalis
Beta blockers
B. Tricuspid Regurgitation
Pathophysiology
Inability of RA to propel blood
across the stenosed valve
RA
Pressure/Systemic Venous
Congestion
Cardiac Output
Backflow of blood from the RV back into the RA during systole
RA pressure
Systemic venous congestion
Curu, Lorelyn June P. BSN III-1 Page 7
Manifestation
Decreased CO
Right-side Heart Failure
- hepatic congestion
- peripheral edema
Atrial Fibrillation
Systolic murmur/S
3
gallop
Management
Anti-dysrythmic drugs
Digitalis
IV. PULMONIC VALVE DISEASE
Usually a congenital defiect
May be caused by RHD
Caused by mitral stenosis, pulmonary emboli & chronic lung disease
Pulmonic stenosis and regurgitation lead to in CO
A. Pulmonary Stenosis
Pathophysiology
Manifestation
Murmur
Right sided heart failure
B. Pulmonic Regurgitation
Allows blood to flow back from the PA to the RV during diastole
Most common cause: dilatation of the pulmonic valve ring due to pulmonary
hypertension
Charac. Murmur: GRAHAM STEELL MURMUR: begins after S
2
and the sound is
accentuated with inspiration
Tap is heard & palpable systolic pulsation on the left parasternal area
Manifestation
SOB, fatigue, cyanosis, fainting
Chest pain
Poor weight gain & failure to thrive in infants
Heart murmur
Management
Diuretics
Digitalis
ACE inhibitors
Vasodilators
Narrowing of the entrance of the pulmonary artery
Interferring with the blood flow out of the right side of the
heart
CO
Curu, Lorelyn June P. BSN III-1 Page 8
Nursing Diagnosis
1. Decreased Cardiac Output (Valvular Dse) r/t reduced ventricular filling and/or emptying
Assess VS
Monitor I & O
Restrict fluids as ordered
Elevate the head of the bed
Provide physical, emotional & mental rest
Administer prescribed medications to reduce cardiac workload
2. Activity Intolerance r/t imbalance between O
2
supply and demand
Monitor VS before, during and after exercise
Encourage adequate rest
Encourage self care
activity levels gradually
Assist with ADLs as needed
Formulate a schedule with alternating rest and activities
3. Risk for Infetion r/t Inadequate primary defense
Assess wounds and catheter sites for signs of infection
Use antiseptic techniques for all invasive procedures
Provide proper wound care
4. Risk for Fluid Volume Excess r/t Na and fluid retention
5. Anxiety r/t change in health status
6. Knowledge deficit regarding preventive measures against endocarditis
7. Risk for Non-compliance
You might also like
- Creatin. Creatin. Creatin. Creatin. Creatin. CreatinDocument2 pagesCreatin. Creatin. Creatin. Creatin. Creatin. CreatinEna PaparićNo ratings yet
- Uworld EndocrineDocument211 pagesUworld Endocrineهنادي رازمNo ratings yet
- Increased ICP: A) HeadacheDocument5 pagesIncreased ICP: A) Headachemohamed nagyNo ratings yet
- Pathogens of The Vagina-Annie Espinosa - This Is The Revised VersionDocument1 pagePathogens of The Vagina-Annie Espinosa - This Is The Revised VersionMicroposterNo ratings yet
- Respiratory Tract InfectionsDocument1 pageRespiratory Tract InfectionsShannon RamsumairNo ratings yet
- Abnormal LFTsDocument2 pagesAbnormal LFTsRenu RosyNo ratings yet
- PnemoniaDocument4 pagesPnemoniadhavalNo ratings yet
- Essentials of Respiratory SystemDocument138 pagesEssentials of Respiratory SystemMuhammad Ahmad bin makruf syammakuNo ratings yet
- Hyperthyroidism Deranged PhysiologyDocument11 pagesHyperthyroidism Deranged PhysiologyManisha Sekaran Muniandy100% (1)
- 7sgdfgf PDFDocument438 pages7sgdfgf PDFPratik JadhavNo ratings yet
- ECG Demographics Rate: 300/# Large Box in RR IntervalDocument11 pagesECG Demographics Rate: 300/# Large Box in RR IntervalJonathan DavisNo ratings yet
- Pain 2. Pallor Poikylothermia Parasthesia Pulselessness Factor V Leiden (Activated Protein C Resistance)Document3 pagesPain 2. Pallor Poikylothermia Parasthesia Pulselessness Factor V Leiden (Activated Protein C Resistance)Ryan TurnerNo ratings yet
- Week 7. Renal Pathology Continued.Document9 pagesWeek 7. Renal Pathology Continued.Amber LeJeuneNo ratings yet
- Hem-Onc: AnswerDocument3 pagesHem-Onc: AnswerAman Raj KNo ratings yet
- Vasculitis: Disorder Vessels Pathology Presentation Test TX OtherDocument3 pagesVasculitis: Disorder Vessels Pathology Presentation Test TX OthermcwnotesNo ratings yet
- IKD9 - Radiological Evaluation of Renal CystsDocument26 pagesIKD9 - Radiological Evaluation of Renal CystsRenal Association MauritiusNo ratings yet
- ENDOCRINE PATHOLOGY WebpathDocument35 pagesENDOCRINE PATHOLOGY Webpathapi-3766657No ratings yet
- Accordion Sign-Appearance (C. Difficile)Document41 pagesAccordion Sign-Appearance (C. Difficile)Andra HijratulNo ratings yet
- 3-Major Veins of The BodyDocument26 pages3-Major Veins of The BodyTJPlayz100% (1)
- CardiomyopathyDocument8 pagesCardiomyopathyKarisaNo ratings yet
- LeukemiaDocument2 pagesLeukemiaAyeshaArifNo ratings yet
- Approach To Pleura LeffusionDocument91 pagesApproach To Pleura Leffusionrodie1050% (1)
- Pleural Effusion: Dr.S.Sesha Sai (MD), Pulmonary MedicineDocument52 pagesPleural Effusion: Dr.S.Sesha Sai (MD), Pulmonary MedicinevaishnaviNo ratings yet
- Rheumatic Fever and Rheumatic Heart DiseaseDocument132 pagesRheumatic Fever and Rheumatic Heart DiseaseDamie FernandezNo ratings yet
- First Aid PharmacoDocument61 pagesFirst Aid PharmacogirNo ratings yet
- Neuro General Neuro: Proptosis/ Exophthalmos ChemosisDocument4 pagesNeuro General Neuro: Proptosis/ Exophthalmos ChemosisShakina FareedNo ratings yet
- NEPHROTIC SYNDROME - HamidDocument20 pagesNEPHROTIC SYNDROME - HamidAbdul Hamid OmarNo ratings yet
- Pathology of The Lung: Djumadi AchmadDocument26 pagesPathology of The Lung: Djumadi AchmadVivi DeviyanaNo ratings yet
- Mitral Valve ProlapseDocument5 pagesMitral Valve ProlapseDerofiez Hana RuhyadinNo ratings yet
- (MED II) 1.05 Emergencies in Cancer PatientsDocument17 pages(MED II) 1.05 Emergencies in Cancer PatientsJearwin AngelesNo ratings yet
- Cardio Block 3Document62 pagesCardio Block 3Maya LaPradeNo ratings yet
- VQ - O2 GradientDocument27 pagesVQ - O2 GradientIkbal NurNo ratings yet
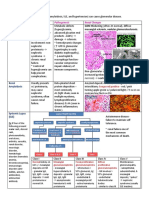
- Acute Myeloproliferative Acute Lymphoproliferative Chronic Myeloproliferative Chronic Lymphoproliferative Plasma Cell NeoplasmDocument1 pageAcute Myeloproliferative Acute Lymphoproliferative Chronic Myeloproliferative Chronic Lymphoproliferative Plasma Cell NeoplasmAudreySlitNo ratings yet
- 4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangDocument4 pages4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangMiel Raphael AranillaNo ratings yet
- Electrolyte DisordersDocument10 pagesElectrolyte DisordersSlavicaNo ratings yet
- Systolic Dysfunction:: Types of Heart FailureDocument13 pagesSystolic Dysfunction:: Types of Heart FailureElisabeth F. OjhaNo ratings yet
- Urological History TakingDocument6 pagesUrological History TakingayuniNo ratings yet
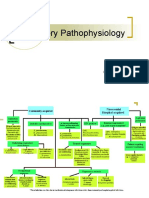
- Respiratory Pathophysiology: B. Pimentel, M.D. University of Makati College of NursingDocument12 pagesRespiratory Pathophysiology: B. Pimentel, M.D. University of Makati College of NursingDoc JacqueNo ratings yet
- Renal SyndromeDocument13 pagesRenal SyndromeAndreas KristianNo ratings yet
- Tumor Markers: Blood Group AntigenDocument5 pagesTumor Markers: Blood Group AntigenAngela ReyesNo ratings yet
- Pathogens of The Female Reproductive System - Leah NechamkinDocument1 pagePathogens of The Female Reproductive System - Leah NechamkinMicroposterNo ratings yet
- WBC Lymph Node SpleenDocument12 pagesWBC Lymph Node Spleendr brijesh TiwariNo ratings yet
- Genetic Disorders-Www - Qworld.co - inDocument13 pagesGenetic Disorders-Www - Qworld.co - inQworld100% (1)
- Medicine OSCE - Common Diseases Ver2Document4 pagesMedicine OSCE - Common Diseases Ver2TrisNo ratings yet
- Cvs (Diuretics)Document2 pagesCvs (Diuretics)CatNo ratings yet
- Week 10 - Hypertension, Atherosclerosis, ArrhythmiaDocument14 pagesWeek 10 - Hypertension, Atherosclerosis, Arrhythmiashivani patel100% (1)
- Overview of AnaemiaDocument2 pagesOverview of AnaemiaGerardLumNo ratings yet
- Red Vascular: Polygonal Cells Growing in Nests or Cords Lamellae of Dense CollagenDocument3 pagesRed Vascular: Polygonal Cells Growing in Nests or Cords Lamellae of Dense CollagenMaryam FadahNo ratings yet
- PleuraDocument6 pagesPleuraameerabest100% (1)
- Medical Boards Step 2 Made Ridiculously Simple (Medicalstudyzone - Com)Document377 pagesMedical Boards Step 2 Made Ridiculously Simple (Medicalstudyzone - Com)Benyamin KhalevNo ratings yet
- Internal Medicine Quick TablesDocument276 pagesInternal Medicine Quick Tablesjoey plouffeNo ratings yet
- Respiratory Notes (Chris Andersen, ICUPrimaryPrep - Com)Document14 pagesRespiratory Notes (Chris Andersen, ICUPrimaryPrep - Com)PkernNo ratings yet
- Arterial Blood Gas Workshop Dr. Lanzona 12.06.07: Lala 3C-Med-09 1Document4 pagesArterial Blood Gas Workshop Dr. Lanzona 12.06.07: Lala 3C-Med-09 1pramastutiNo ratings yet
- Cardiovascular Nursing: Study Online atDocument7 pagesCardiovascular Nursing: Study Online atLilly DayeNo ratings yet
- Source NotesDocument30 pagesSource NotesChris Jardine Li100% (1)
- Asthma DrugsDocument1 pageAsthma DrugskakuNo ratings yet
- Cont of Lesson 2Document1 pageCont of Lesson 2Jane Pineda CuraNo ratings yet
- Try ThisDocument1 pageTry ThisJane Pineda CuraNo ratings yet
- Congestive Heart FailureDocument8 pagesCongestive Heart FailureJane Pineda CuraNo ratings yet
- Case Report Hirschsprung's DseDocument10 pagesCase Report Hirschsprung's DseJane Pineda CuraNo ratings yet
- Case Report Hirschsprung's DseDocument10 pagesCase Report Hirschsprung's DseJane Pineda CuraNo ratings yet
- About The Open Source InitiativeDocument6 pagesAbout The Open Source InitiativeJane Pineda CuraNo ratings yet
- Movie AnalysisDocument2 pagesMovie AnalysisJane Pineda CuraNo ratings yet
- Imci 2Document4 pagesImci 2Jane Pineda CuraNo ratings yet
- DeanDocument5 pagesDeanJane Pineda CuraNo ratings yet
- Micu Case Study d1Document28 pagesMicu Case Study d1jmarc_2180% (5)
- Cardiac CycleDocument30 pagesCardiac CycleCarrine Liew100% (2)
- Endocrine Pharmacology Ppt-MergedDocument169 pagesEndocrine Pharmacology Ppt-MergedLordgin OpenianoNo ratings yet
- Board Desember 2015 Fix Answer - BALIDocument67 pagesBoard Desember 2015 Fix Answer - BALIrahageng wida kusuma100% (1)
- Heart Failure With Normal Ejection Fraction (HFNEF)Document64 pagesHeart Failure With Normal Ejection Fraction (HFNEF)medpedshospitalist100% (1)
- 1 كتب دكتور علام باطنه General & Cardio.whiteKnightLoveDocument111 pages1 كتب دكتور علام باطنه General & Cardio.whiteKnightLoveNour ShăbanNo ratings yet
- Pathophysiology of MI, COPD and BPHDocument10 pagesPathophysiology of MI, COPD and BPHSarah Lim100% (1)
- Rheumatic Fever and Rheumatic Heart DiseaseDocument54 pagesRheumatic Fever and Rheumatic Heart DiseaseFian AldyNo ratings yet
- Cardiac Asthma - Causes, Symptoms, Diagnosis and Treatment - Tips Curing DiseaseDocument5 pagesCardiac Asthma - Causes, Symptoms, Diagnosis and Treatment - Tips Curing DiseaseBharat JamodNo ratings yet
- NSG 3000 Exam 2 GuideDocument19 pagesNSG 3000 Exam 2 GuideJoy MathewsNo ratings yet
- Original Research Abstract AFCC ASMIHA 2019Document82 pagesOriginal Research Abstract AFCC ASMIHA 2019Program Studi Kardiologi100% (1)
- Echo Go HFDocument15 pagesEcho Go HFGaxi BofNo ratings yet
- Forensic4 MDTRMSDocument15 pagesForensic4 MDTRMSsteffymyrhNo ratings yet
- January 2022 (IAL) QPDocument28 pagesJanuary 2022 (IAL) QPMaria Shabbir PanjiwalaNo ratings yet
- ATPL Human PerformanceDocument583 pagesATPL Human PerformanceAmilton Morillas100% (1)
- Step by Step Pediatric Echocardiography PDFDocument141 pagesStep by Step Pediatric Echocardiography PDFDiana_anca6100% (1)
- Congestive Cardiac FailureDocument61 pagesCongestive Cardiac FailureYAMINIPRIYANNo ratings yet
- Microsoft PowerPoint - Left and Right Heart CathDocument43 pagesMicrosoft PowerPoint - Left and Right Heart CathIr Soebagoes100% (2)
- Mi Case StudyDocument27 pagesMi Case StudyMary Hope BacutaNo ratings yet
- Funda ExamDocument18 pagesFunda Examronnax100% (2)
- Pre and Post Operative Care For Patient After Cardiac SurgeryDocument20 pagesPre and Post Operative Care For Patient After Cardiac SurgeryGayathri RNo ratings yet
- Anatomy and Physiology AnswersDocument11 pagesAnatomy and Physiology AnswersKojo Yeboah EnchillNo ratings yet
- Pathophysiology of Congenital Heart Disease in The Adult: Special ReportDocument10 pagesPathophysiology of Congenital Heart Disease in The Adult: Special ReportLwin ThantNo ratings yet
- Names and Functions of The Human AnatomiesDocument92 pagesNames and Functions of The Human AnatomiesShania Kate Ledesma ManabatNo ratings yet
- Essay On Cardiac Cycle (With Diagram) - Heart - Human - BiologyDocument28 pagesEssay On Cardiac Cycle (With Diagram) - Heart - Human - Biologydr_swaralipiNo ratings yet
- A Practical Approach To Cardiac Anesthesia-Lippincot - Wolters Kluwer (2012)Document1,677 pagesA Practical Approach To Cardiac Anesthesia-Lippincot - Wolters Kluwer (2012)ElenaCondratscribdNo ratings yet
- Ebook Egans Fundamentals of Respiratory Care 11Th Edition Kacmarek Test Bank Full Chapter PDFDocument40 pagesEbook Egans Fundamentals of Respiratory Care 11Th Edition Kacmarek Test Bank Full Chapter PDFalexandercampbelldkcnzafgtw100% (11)
- Congestive Heart FailureDocument13 pagesCongestive Heart Failureali alrashediNo ratings yet
- Hap - Multiple Choice QuestionsDocument11 pagesHap - Multiple Choice QuestionsAnitha Mary DambaleNo ratings yet
- Congestive Heart FailureDocument43 pagesCongestive Heart Failure568563100% (1)