Professional Documents
Culture Documents
1st Line Medication of An e Cart
Uploaded by
Colette Marie PerezOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1st Line Medication of An e Cart
Uploaded by
Colette Marie PerezCopyright:
Available Formats
DRUG NAME
EPINEPHRINE
ADULT DOSE
1mg IV or 2-5 mg IV via ETT 40 units IV For VF or pulseless VT: 300mg IV push 1-1.5 push mg/kg IV
PEDIATRIC DOSE
0.01mg/kg IV or IO or 0.1mg/kg via ETT Not indicated For VF or pulseless VT: 5mg/kg IV push Same 25-50mg/kg IV slow push 15 mg/kg IV load;3-6 mg/kg over 5min,not to exceed 100mg/kg 0.02mg/kg;mini mum dose of 0.1 mg
INDICATI ON
Any pulseless arrhythms VF, PulselessVT VF, pulseless VT,VT with a pulse,SVT VF, pulseless VT,VT with a pulse Torsde de pointes, known hypomagnese mia VT with a pulse
FREQUENCY
Every 3-5 min
VASOPRESSIN AMIODARONE
Single dose,may be followed at 10 min by epinephrine May use 2nddose of 150mg for recurrent VF/VT.In children may be repeated in 5mg/kg doses to a total of 15mg/kg 2nd & subsequent doses of 0.75mg/kg every 5 min to a total dose of 3 mg/kg Single dose
LIDOCAINE MAGNESIUM
1-2g IV slow push
PROCAINAMI DE
17 mg/kg IV slow bolus at maximum rate of 50mg/min PerfusingPatients: 0.5mg Iv push5min, to maximum of 3mg. Pulseless patients: 1mg IV push q 5 min, to maximum of 3mg 6 mg rapid IV push through proximal peripheral line; central line dose is one-half 0.25mg/kg to a maximum dose of 20mg IV push over 2min 500Mcg/kg over 1 min bolus
Continue infusion(4mg/min) until QRS widening>50%,dysrhythmia terminated, onset of hypotension; or 17 mg/kg infused. May be repeated once upto maximum dose of 3mg
ATROPINE
Bradycardia, asystole.
ADENOSINE
0.1mg/kg rapid IV push;maximum dose,6mg Same
SVT
If needed,2nd dose of 12 mg(pediatric,doble initial dose up to 12 mg);3rd dose of 12-18 mg 2nd dose of 0.35mg/kg,maximum dose of 25mg, at 15min;after conversion, start dilitiazem drip at 5-15 mg/H
DILITIAZEM
SVT
ESMOLOL
100-500 Mcg/kg bolus over 1min Not indicated Not indicated
SVT
May give another bolus if desired effect is not achieved; start drip 50Mcg/kg/min Repeat in 10 min, then give 50mg oral load Repeat twice at 5min intervals, then give 50 mg oral load
ATENOLOL METOPROLOL
5mg IV over 5min 5 mg IV push
SVT,MI SVT,MI
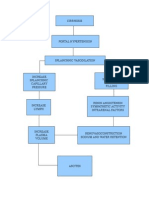
EPINEPHRINE (Beta2 Adrenergic Agonists)
Action Stimulates beta receptors in lung. Relaxes bronchial smooth muscle. Increases vital capacity Increases BP, HR, PR Decreases airway resistance. Indication Asthma Bronchitis Emphysema All cardiac arrest, anaphylaxis Used for symptomatic bradycardia. Relief of bronchospasm occurring during anesthesia Exercised-induced bronchospasm
Nursing Management Monitor V/S. and check for cardiac dysrrhythmias Drug increases rigidity and tremor in patients with Parkinsons disease Epinephrine therapy interferes with tests for urinary catecholamine Avoid IM use of parenteral suspension into buttocks. Gas gangrene may occur Massage site after IM injection to counteract possible vasoconstriction. Observe patient closely for adverse reactions. Notify doctor ifadverse reaction develop If blood pressure increases sharply, rapid-acting vasodilators such as nitrates or alphablockers can be given to counteract Medication Classification, Mechanism of action, uses, contraindication, side effects and nursingconsiderations
VASOPRESSIN (Antidiuretic)
Action Increases cyclic adenosine monophosphate (cAMP) which increases water permeabilityat the renal tubuleresulting in decreased urine volume and increased osmolality; causesperistalsis bydirectly stimulating the smooth muscle in the GI tract; directvasoconstrictor without inotropic or chronotropic effects Indications Adjunct in the treatment of GI hemorrhage and esophageal varices; pulseless arrest(ventricular tachycardia [VT]/ventricular fibrillation [VF], asystole/pulseless electricalactivity [PEA]); vasodilatory shock ; donor management in brain-dead patients Nursing consideration Evaluate patient history closely for use cautions. Assess potential for interactions with other pharmacological agents patient may betaking (eg, concurrent use that will block or enhance anti diuretic response). Note: Dosing and administration vary according to purpose for use. I.V. requires use of infusion pump and close monitoring to prevent extravasation (may cause severe necrosis and gangrene). Assess results of laboratory tests, therapeutic effectiveness, and adverse response (eg,cardiac status, blood pressure, CNS status, fluid balance, signs or symptoms of water intoxication, intra nasal irritation) on a regular basis during therapy. Teach patient possible side effects/appropriate interventions and adverse symptoms to report Diltiazem (Cardizem) (50mg/10mL) Classification Anti-anginals Antiarrhythmics Antihypertensive Ca channel blocker Action Inhibits calcium transport into myocardial smooth muscle cells Systemic and coronary vasodilation Indication Hypertension Angina Pectoris SupraventricularArrhythmia Atrial flutter/fibrillation Nursing Management Monitor BP and pulse before therapy, during titration and therapy Monitor I&O and weight
Assess for CHF Routine serum Digoxin monitoring
Adenosine (Adenocard) (6mg/2mL) Classification Nucleoside Indication To convert paroxysmal supraventicular tachycardia (PSVT) to sinus rhythm Action A naturally occurring nucleoside that acts on the AV node to slow conduction and inhibit re entry pathways. Also useful in treating PSVTs, including those with accessory by pass tracts (Wolff-Parkinson-White syndrome) Nursing Management ALERT: by decreasing conduction through the AV node, drug may produce first-, secondor third-degree heart block. Patients who develop high-level heart block after a single dose shouldnt receive additional doses. ALERT: new arrhythmias, including heart block and transient a systole, may develop;monitor cardiac rhythm and treat as indicated. If solution is cold, crystals may form; gently warm solution to room temperature. Dont use solutions that arent clear. Drug lacks preservatives. Discard unused portion Magnesium sulfate (50%(500mg/mL)) Classification Anticonvulsant Indication Treatment of hypomagnesaemia accompanied by signs of tetany Control of HTN Encephalopathy & convulsions Prevention & control of convulsions in patients w/ preeclampsia or eclampsia Prevention of hypomagnesaemia in patients receiving TPN Action May decrease acetylcholine released by nerve impulses, but its anticonvulsant mechanism is unknown Nursing Management Monitor the following: I.V.: Rapid administration: ECG monitoring, vital signs, deep tendon reflexes; magnesium, calcium, and potassium levels; renal function during administration. Obstetrics: Patient status including vital signs, oxygen saturation, deep tendon reflexes,level of consciousness, fetal heart rate, maternal uterine activity. Oral: Renal function; magnesium levels;bowel movements Amiodarone Classification: Cardiac Drugs Indication: Ventricular and supraventricular arrhythmias.
Action: Blocks potassium chloride leading to prolongation of action potential duration
Nursing Measures: Monitor cardiac rhythm continuously. Monitor for an extended period when dosage adjustments are made. Monitor for safe and effective serum levels (0.52.5 mcg/mL). Doses of digoxin, quinidine, procainamide, phenytoin, and warfarin may need to bereduced one-third to one-half when amiodarone is started. Give drug with meals to decrease GI problems. Arrange for ophthalmologic exams; reevaluate at any sign of optic neuropathy. Arrange for regular periodic blood tests for liver enzymes, thyroid hormone levels. Drug dosage will be changed in relation to response of arrhythmias; you will need to be hospitalized during initiation of drug therapy; you will be closely monitored when dosageis changed. Have regular medical follow-up, monitoring of cardiac rhythm, chest x-ray, eye exam,blood tests Procainamide (Pronestyl)1 gm Classification Antiarrhythmics Action Blocks open Na channels and prolong the cardiac action potential. This results in slowed conduction and ultimately the decreased rate of rise of the action potential may result on the widening of QRS on ECG Indication Supraventricular and ventricular arrhythmias. Treatment ofWolf-Parkinson-White Syndrome Nursing Management Assess cardiovascular status before therapy . Assess pulmonary, hepatic and thyroid. function before and during therapy. Monitor fluid and electrolytes, I&O, K, Na and Cl. Monitor ECG, BP. Assess vision Lidocaine (Xylocaine) 100 mg bolus 1 gm Classification CV drugs: Antiarrhythmics Anesthetic Action Increases electrical stimulation of ventricle and His-Purkinje system by direct action ontissues, resulting to decrease depolarization, automaticity and excitability in ventriclesduring diastolic phase Indication Anesthesia Arrhythmias Control of Status Epilepticus refractory to other treatments Nursing Management Assess pt before and after therapy Pts infusion must be on cardiac monitor Monitor ECG, if QT or QRS increases by 50% or more, withhold the drug
Monitor BP, check for rebound HPN after 1-2 hrs Assess respiratory status, oxygenation and pulse deficits Assess renal and liver function Monitor CNS symptoms Monitor blood levels Atropine Sulfate (4mg/mL) Classification Anticholinergic Indication Pre-op meds/pre-anesthetic meds To restore cardiac rate and arterial pressure during anesthesia when vagal To lessen the degree of A-V heart block To overcome severe carotid sinus reflex Antidote for cholinergic toxicity Nursing Management Monitor VS. Report increase HR Monitor for constipation, oliguria. Instruct to take 30 minutes before meals Eat foods high in fiber and drink plenty fluids. Can cause photophobia Instruct client not to drive a motor vehicle or participate in activities requiring alertness.
You might also like
- Pharmacology Checklist - Rationale 02Document30 pagesPharmacology Checklist - Rationale 02Tisha DeiparineNo ratings yet
- Emergency DrugsDocument47 pagesEmergency DrugsBesimanNo ratings yet
- NCP EsrfDocument9 pagesNCP EsrfKen RegalaNo ratings yet
- Fluids and Electrolytes ConceptDocument31 pagesFluids and Electrolytes ConceptDarwin AndalNo ratings yet
- Case 1Document9 pagesCase 1Joselyn M. LachicaNo ratings yet
- IVTDocument11 pagesIVTNoorwashilaNo ratings yet
- COPD Therapeutics CaseDocument34 pagesCOPD Therapeutics CaseCindy NoufalNo ratings yet
- Reteplase (MIRel)Document23 pagesReteplase (MIRel)Jhoann JamanilaNo ratings yet
- Changing An IV SolutionDocument2 pagesChanging An IV SolutionNoel100% (9)
- Angiotensin Converting Enzyme (ACE) InhibitorsDocument4 pagesAngiotensin Converting Enzyme (ACE) InhibitorsPutri Mulia HasibuanNo ratings yet
- Drug Study On DigoxinDocument8 pagesDrug Study On DigoxinDonald BidenNo ratings yet
- "Emergency Drugs": Pictures/ Generic Name Brand Name/ Classification/ Stock Dose/ Indication Nursing ResponsibilitiesDocument7 pages"Emergency Drugs": Pictures/ Generic Name Brand Name/ Classification/ Stock Dose/ Indication Nursing ResponsibilitiesJohn Balgoa100% (2)
- High Alert Medications 2018Document30 pagesHigh Alert Medications 2018Eman MohamedNo ratings yet
- Er Drug StudyDocument29 pagesEr Drug StudyMa Karenina DualanNo ratings yet
- Steps To Perform A Blood TransfusionDocument1 pageSteps To Perform A Blood Transfusionzepoli_zepoly6232No ratings yet
- Medical Management To ConclusionDocument88 pagesMedical Management To ConclusionRomelle Jane M. VelascoNo ratings yet
- Case StudyDocument34 pagesCase StudyBSNNursing101No ratings yet
- Term 3 Rationale Pharmacology and MCNDocument35 pagesTerm 3 Rationale Pharmacology and MCNKing KongNo ratings yet
- Nursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveDocument2 pagesNursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveFreisanChenMandumotanNo ratings yet
- NCM 112 MidtermDocument25 pagesNCM 112 MidtermJan Charlie Sophia100% (1)
- Endorsement SheetDocument1 pageEndorsement SheetLucelle MarieNo ratings yet
- Hypovolemic ShockDocument12 pagesHypovolemic ShockHassanal DimaporoNo ratings yet
- Blood Transfusion Purpose: 9. Check Blood For Presence of BubblesDocument2 pagesBlood Transfusion Purpose: 9. Check Blood For Presence of BubblesMabes100% (1)
- Emergency Medicine ListDocument1 pageEmergency Medicine ListmomnaNo ratings yet
- Nursing OrganizationsDocument2 pagesNursing Organizationsemman leonardo100% (1)
- IV Insertion ProcedureDocument11 pagesIV Insertion ProcedureEdelweiss Marie Cayetano100% (1)
- Emergency Drugs - NMMC ECARTDocument1 pageEmergency Drugs - NMMC ECARTKaloy KamaoNo ratings yet
- Nursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Document9 pagesNursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Gayu Patel0% (1)
- Drug StudyDocument12 pagesDrug StudyFiela De VillaNo ratings yet
- Ecart DrugsDocument3 pagesEcart Drugsgreen_archerNo ratings yet
- Mosegor Vita Is A Vitamin SupplementDocument1 pageMosegor Vita Is A Vitamin SupplementlolabayNo ratings yet
- CyclosporineDocument2 pagesCyclosporineMuhammad ArsalanNo ratings yet
- NVS Written ReportDocument20 pagesNVS Written ReportbabiNo ratings yet
- Neuro - Sir Chavez - AS OF 12PMDocument5 pagesNeuro - Sir Chavez - AS OF 12PMCarl JustineNo ratings yet
- Clinical Features and Diagnosis of Hemophagocytic Lymphohistiocytosis - UpToDateDocument27 pagesClinical Features and Diagnosis of Hemophagocytic Lymphohistiocytosis - UpToDateSalvatore ScutoNo ratings yet
- 220 Nursing Bullets Fundamentals of Nursing Reviewer 1Document23 pages220 Nursing Bullets Fundamentals of Nursing Reviewer 1Kyles JumaritoNo ratings yet
- Case StudyDocument3 pagesCase StudyDanae Kristina Natasia BangkanNo ratings yet
- Head Nursing - StudentDocument26 pagesHead Nursing - Studentstepcoy123100% (1)
- Written Report:: Transitional Human ShelterDocument7 pagesWritten Report:: Transitional Human ShelterKasandra Dawn Moquia BerisoNo ratings yet
- AdenosineDocument2 pagesAdenosinejdmedicNo ratings yet
- NCP Proper CholecystectomyDocument2 pagesNCP Proper CholecystectomyGail Lian SantosNo ratings yet
- Calcium AcetateDocument3 pagesCalcium AcetateKIM NAMJOON'S PEACHES & CREAM100% (1)
- Echo 01.20.15Document5 pagesEcho 01.20.15Soad ShedeedNo ratings yet
- Transcultural Perspective in The Nursing Care of Adults Physiologic Development During AdulthoodDocument5 pagesTranscultural Perspective in The Nursing Care of Adults Physiologic Development During AdulthoodeuLa-mayzellNo ratings yet
- Ecart Medications and EquipmentDocument9 pagesEcart Medications and EquipmentJan Philippe BelandoNo ratings yet
- Levemir Product Insert PDFDocument11 pagesLevemir Product Insert PDFDegee O. GonzalesNo ratings yet
- The Ethico Legal Aspects of Intravenous Therapy BasicDocument38 pagesThe Ethico Legal Aspects of Intravenous Therapy BasicRoan Nepomuceno - Joaquin100% (2)
- NCM 103.1 FINAL - OkDocument99 pagesNCM 103.1 FINAL - OkElizalde HusbandNo ratings yet
- 16 ARDS - Nursing Care ManagementDocument2 pages16 ARDS - Nursing Care ManagementTisha CarretteNo ratings yet
- ACS AMI FacilitatorDocument21 pagesACS AMI FacilitatorPaul Zantua57% (7)
- Case 1 - Pneumonia (Final)Document4 pagesCase 1 - Pneumonia (Final)Joegie ArioNo ratings yet
- CarePlan #2Document3 pagesCarePlan #2Monika StasiakNo ratings yet
- Impaired Gas ExchangeDocument1 pageImpaired Gas Exchangeruggero07No ratings yet
- Devices Used in ICU: Critical Care NursingDocument95 pagesDevices Used in ICU: Critical Care NursinghendranatjNo ratings yet
- Drug StudyDocument7 pagesDrug StudydivineNo ratings yet
- NCM 118B Emergency MedicationsDocument110 pagesNCM 118B Emergency MedicationsJan Crizza Dale R. FrancoNo ratings yet
- Drug StudyDocument9 pagesDrug StudyChristine PunsalanNo ratings yet
- Drug Study On Emergency DrugsDocument16 pagesDrug Study On Emergency DrugsJosepNo ratings yet
- Emergency DrugsDocument15 pagesEmergency Drugsjheverly123100% (1)
- Drug Study On Emergency DrugsDocument15 pagesDrug Study On Emergency DrugsJAy TootNo ratings yet
- A Case Study On Company CasesDocument8 pagesA Case Study On Company CasesColette Marie PerezNo ratings yet
- Project Proposal KALINISANDocument4 pagesProject Proposal KALINISANColette Marie Perez0% (1)
- Non Modifiable FactorsDocument2 pagesNon Modifiable FactorsColette Marie PerezNo ratings yet
- Drug Study Child FeverDocument2 pagesDrug Study Child FeverColette Marie PerezNo ratings yet
- Ma. Georgina Belen A. Guevara 27 San Mateo St. Kapitolyo, Pasig City 576-4687 / 0927-317-8221Document4 pagesMa. Georgina Belen A. Guevara 27 San Mateo St. Kapitolyo, Pasig City 576-4687 / 0927-317-8221Colette Marie PerezNo ratings yet
- Dap and Dar Week1Document7 pagesDap and Dar Week1Colette Marie PerezNo ratings yet
- NCP - Impaired Skin IntegrityDocument4 pagesNCP - Impaired Skin IntegrityColette Marie PerezNo ratings yet
- Staffing PatternDocument2 pagesStaffing PatternColette Marie PerezNo ratings yet
- Action of Plan: Date: Week and Day: 1 I. Area of ConcernDocument4 pagesAction of Plan: Date: Week and Day: 1 I. Area of ConcernColette Marie PerezNo ratings yet
- Patho AscitesDocument1 pagePatho AscitesColette Marie PerezNo ratings yet
- A. System Reviews I. Health Perception and Health Management PatternDocument4 pagesA. System Reviews I. Health Perception and Health Management PatternColette Marie PerezNo ratings yet
- NCP - Impaired Skin IntegrityDocument4 pagesNCP - Impaired Skin IntegrityColette Marie PerezNo ratings yet
- Theoretical FrameworkDocument24 pagesTheoretical FrameworkColette Marie PerezNo ratings yet
- Elec DSDocument5 pagesElec DSColette Marie PerezNo ratings yet
- Drug StudyDocument7 pagesDrug StudyRam Van MunsterNo ratings yet
- Family History and DevelopmentalDocument4 pagesFamily History and DevelopmentalColette Marie PerezNo ratings yet
- Predisposing Factors For TB Infection Include The FollowingDocument1 pagePredisposing Factors For TB Infection Include The FollowingColette Marie PerezNo ratings yet
- Predisposing Factors For TB Infection Include The FollowingDocument1 pagePredisposing Factors For TB Infection Include The FollowingColette Marie PerezNo ratings yet
- Core Competencies in Nursing-1Document11 pagesCore Competencies in Nursing-1yakapmNo ratings yet
- 1st Line Medication of An e CartDocument5 pages1st Line Medication of An e CartColette Marie PerezNo ratings yet
- Fire Prevention Month (Program)Document1 pageFire Prevention Month (Program)Colette Marie Perez100% (1)
- Developmental History ICUDocument3 pagesDevelopmental History ICUColette Marie PerezNo ratings yet
- Patho AscitesDocument1 pagePatho AscitesColette Marie PerezNo ratings yet
- Action of Plan: Date: Week and Day: 1 I. Area of ConcernDocument4 pagesAction of Plan: Date: Week and Day: 1 I. Area of ConcernColette Marie PerezNo ratings yet
- First AidDocument1 pageFirst AidColette Marie PerezNo ratings yet
- Family History and DevelopmentalDocument4 pagesFamily History and DevelopmentalColette Marie PerezNo ratings yet
- Fire Prevention.Document3 pagesFire Prevention.Colette Marie PerezNo ratings yet
- First AidDocument1 pageFirst AidColette Marie PerezNo ratings yet
- First AidDocument1 pageFirst AidColette Marie PerezNo ratings yet
- 1 s2.0 S1110016815000563 Main PDFDocument13 pages1 s2.0 S1110016815000563 Main PDFvale1299No ratings yet
- 01-20 Optical Multiplexer and Demultiplexer BoardDocument57 pages01-20 Optical Multiplexer and Demultiplexer BoardDaler ShorahmonovNo ratings yet
- Notes Transfer of Thermal EnergyDocument12 pagesNotes Transfer of Thermal Energymahrosh mamoon100% (2)
- Paper-Czechowski-Slow-strain-rate Stress Corrosion Testing of Welded Joints of Al-Mg AlloysDocument4 pagesPaper-Czechowski-Slow-strain-rate Stress Corrosion Testing of Welded Joints of Al-Mg Alloysjavo0128No ratings yet
- English Class Vii PDFDocument101 pagesEnglish Class Vii PDFpannapurohitNo ratings yet
- GB GW01 14 04 02Document2 pagesGB GW01 14 04 02Muhammad LukmanNo ratings yet
- Etoricoxib - Martindale 39thDocument2 pagesEtoricoxib - Martindale 39thCachimbo PrintNo ratings yet
- The History of AstrologyDocument36 pagesThe History of AstrologyDharani Dharendra DasNo ratings yet
- LinkageDocument9 pagesLinkageHarshu JunghareNo ratings yet
- Exam 3 DynamicsDocument7 pagesExam 3 DynamicsJulioNo ratings yet
- 23001864Document15 pages23001864vinodsrawat33.asiNo ratings yet
- Statics: Vector Mechanics For EngineersDocument39 pagesStatics: Vector Mechanics For EngineersVijay KumarNo ratings yet
- Line Differential Protection Red670Document8 pagesLine Differential Protection Red670igorsfaceNo ratings yet
- Optical Scattering of Gold NanosphereDocument24 pagesOptical Scattering of Gold NanosphereParas KumarNo ratings yet
- MMW ReviewerDocument3 pagesMMW ReviewerMarcSaloj NeryNo ratings yet
- Surface Finish Measurement NotesDocument32 pagesSurface Finish Measurement NotesAneez ShresthaNo ratings yet
- Mega StructuresDocument2 pagesMega StructuresSanthosh KumarNo ratings yet
- Danika Cristoal 18aDocument4 pagesDanika Cristoal 18aapi-462148990No ratings yet
- Karl MarxDocument4 pagesKarl Marxeirvine noah isidroNo ratings yet
- Asco Series 238 ASCO Pilot Operated Solenoid Valves (Floating Diaphragm)Document2 pagesAsco Series 238 ASCO Pilot Operated Solenoid Valves (Floating Diaphragm)Khyle Laurenz DuroNo ratings yet
- Isulat Lamang Ang Titik NG Tamang Sagot Sa Inyong Papel. (Ilagay Ang Pangalan, Section atDocument1 pageIsulat Lamang Ang Titik NG Tamang Sagot Sa Inyong Papel. (Ilagay Ang Pangalan, Section atMysterious StudentNo ratings yet
- Bulk Material/Part Ppap Process Checklist / Approval: Required?Document32 pagesBulk Material/Part Ppap Process Checklist / Approval: Required?krds chidNo ratings yet
- Reynold A. Nicholson - The Mystics of IslamDocument65 pagesReynold A. Nicholson - The Mystics of IslamLuminon SamanNo ratings yet
- Optik: Original Research ArticleDocument6 pagesOptik: Original Research ArticlesimarpreetNo ratings yet
- CulvertsDocument18 pagesCulvertsAmmar A. Ali100% (1)
- Underground Equipment SelectionDocument44 pagesUnderground Equipment SelectionCherotich Silas cheboseiNo ratings yet
- Iec60227-3 (Ed2.1) en DDocument6 pagesIec60227-3 (Ed2.1) en Duntuk donlod aaaNo ratings yet
- Gujral FCMDocument102 pagesGujral FCMcandiddreamsNo ratings yet
- Usp Description and SolubilityDocument1 pageUsp Description and SolubilityvafaashkNo ratings yet
- Us Navy To Evaluate Anti Submarine Warfare Training SystemDocument2 pagesUs Navy To Evaluate Anti Submarine Warfare Training SystemVictor PileggiNo ratings yet
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (5)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (24)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- Self-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!From EverandSelf-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!Rating: 5 out of 5 stars5/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)From EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Rating: 4 out of 5 stars4/5 (378)
- To Explain the World: The Discovery of Modern ScienceFrom EverandTo Explain the World: The Discovery of Modern ScienceRating: 3.5 out of 5 stars3.5/5 (51)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (58)