Professional Documents
Culture Documents
Advances in Feline Neurology
Uploaded by
kimyounggiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Advances in Feline Neurology
Uploaded by
kimyounggiCopyright:
Available Formats
Advances in Feline Neurology
Philip A. March, DVM, MS Diplomate ACVIM (Neurology) Assistant Professor Department of Veterinary Clinical Sciences College of Veterinary Medicine The Ohio State University Columbus, Ohio 43210 KEY WORDS neurologic examination meningoencephalomyelitis myasthenia gravis epilepsy meningioma Neurologic disorders in the cat are a diagnostic and therapeutic challenge. The inherent difficulties in performing a thorough neurologic examination in cats and the atypical signs sometimes exhibited by cats make neurolocalization of lesions difficult. Cats also are not susceptible to the same types of diseases as dogs. Specifically, idiopathic inflammatory disorders, such as granulomatous meningoencephalomyelitis (GME), idiopathic meningitis disorders, polyradiculoneuritis, and polymyositis, are rare in the cat. Infectious, neoplastic, and vascular diseases are common in cats and can affect the nervous system focally or multifocally. Because underlying diseases are common, it is advisable to approach both the diagnosis and treatment of feline neurologic disorders aggressively. This paper addresses some important differences in the diagnosis and treatment of neurologic problems in the cat compared to the dog. Selected disorders that preferentially affect different areas of the nervous system are discussed from the standpoint of their usual presentation, tests now being used for definitive diagnosis, and therapeutic modalities currently available for each condition. DIAGNOSTIC AIDS The Neurologic Examination Stress and the sympathetic overdrive that many cats experience during the neurologic examination mask certain deficits, create new ones, and generally complicate the practitioners ability to neurolocalize the lesion. It is rare to be able to perform a thorough examination on cats unless the patient is extremely cooperative or is dull or obtunded because of the underlying disease. Certain reflex and response tests in cats are more reliable and not as subject to environmental stress. Even these tests may be difficult to per88
form in an excited, apprehensive cat unless the examiner maintains some patience and minimizes restraint during the examination. Certain neurologic examination tests in alert, nonobtunded cats are frequently unreliable. These include the knuckling tests for conscious proprioception and myotactic limb reflexes. Hopping, hemihopping, and tactile placing are more reliable tests of postural control in cats. The flexor withdrawal reflex is the most reliable limb reflex in cats, and close attention to the strength of the withdrawal and the participation of all muscle groups in this reflex can be very helpful in determining whether a peripheral or a lower motor neuron (LMN) disorder is present. Observing for a crossed extensor (abnormal extension of the opposite limb) during the flexor reflex is important as well. Presence of a crossed extensor is indicative of an upper motor neuron (UMN) lesion (brain or spinal cord). Gait analysis is also difficult in cats that refuse to move because of either fright or imbalance. Placing the cat in an empty, quiet room or observing ambulation in a cage may be helpful techniques. Wheelbarrowing, hopping, placing tests, and gently coaxing the patient to jump from an elevated surface to the floor are used to assess strength and coordination. Because some cats do not menace because of fear and increased sympathetic tone, dropping cotton balls or using the visual placing test may be a better test of vision. The dolls eye reflex in cats is best accomplished by holding the cat in the examiners hands and rotating the cat around the examiner. In the final analysis, there is no substitute for a detailed description of neurologic signs that were evident to the owner in the home environment. Questions concerning abnormal behavior, seizurelike activity, sleep-wake cycles, circling tendencies, stumbling, falling, incoordination, reluctance to jump, bumping into objects, etc., should be asked. The speed of onset and progression of clinical signs are likewise critical pieces of information. A videotape of episodic events can provide extremely valuable information. Approach to Diagnostic Testing As discussed in the previous section, an aggressive diagnostic approach to a cat with neurologic signs is often warranted. Infectious, neoplastic, and vascular disorders can affect multiple body systems, so a complete blood count, chemistry profile, urinalysis, feline immunodeficiency virus (FIV) and feline leukemia virus (FeLV) testing, and thoracic radiographs are recommended if neurologic signs are present. Hepatic
ADVANCES IN FELINE NEUROLOGY
89
alanine aminotransferase (ALT) elevations may be found in cats with feline infectious peritonitis (FIP dry form), toxoplasmosis, and hyperthyroidism, all diseases with potential nervous system involvement. Central nervous system (CNS) lymphosarcoma is strongly associated with nonregenerative anemia and positive FeLV status.1 In older cats, a T4 level and blood pressure measurements are indicated, especially if forebrain signs are present. A complete ophthalmic examination is recommended in feline patients with nervous system disease. Cryptococcosis, toxoplasmosis, and FIP are common causes of anterior and posterior uveitis. Systemic hypertension may lead to spontaneous hemorrhage in both the retina and the CNS. Papilledema may be observed in cats with brain tumors and elevated intracranial pressure. Horners syndrome is relatively more common in cats than in dogs and pharmacologic testing may be indicated to determine whether the lesion is postganglionic (common cause is a middle/inner ear disease) or preganglionic (common cause is a cranial mediastinal mass). Serology is a critical component of the diagnostic workup. This is especially important in cats with any outdoor history or exposure to multiple cats in a household (catteries, etc.). There are, however, reported cases of cryptococcosis in strictly indoor cats with no exposure to other cats. The latex agglutination antigen test is the current test of choice for diagnosis of Cryptococcus neoformans.24 Paired serum titers (23 weeks apart) are strongly recommended for diagnosis of toxoplasmosis. Coronavirus titers are recommended by this author if signs of FIP are present. False-negative and false-positive results are possible,57 but a very high titer in conjunction with typical clinical signs (fever, uveitis, central vestibular signs/seizures) is highly suggestive of infection. Cerebrospinal fluid (CSF) cytology and titers are indicated in certain circumstances. Multifocal signs or focal signs present in conjunction with a high suspicion of infectious diseases are indications for CSF analysis. CSF cytology should be performed within 1 hour of collection by a laboratory that has cell counting abilities and a cytocentrifuge. Local human hospital laboratories may be willing to perform this service and have been very approachable in this authors experience. The usual delay in processing that occurs with most veterinary courier services results in cell lysis and a nondiagnostic sample. Colorado State University Veterinary Diagnostic Laboratory performs a variety of antigen and antibody tests on CSF (including tests for cryptococcosis and toxoplasmosis). If serum is also submitted in conjunction with CSF, this
laboratory will also determine whether intrathecal antibody is present (a definitive test for CNS infection). In some cases, serum titers may not reflect what is occurring in the CNS. Furthermore, cases of CNS cryptococcosis with negative serum titers have been reported.8 Imaging is usually indicated if a focal lesion is suspected. Examples include focal lesions of the forebrain, brain stem, or spinal cord. Skull radiographs may be useful in cases of craniocerebral trauma or if a meningioma is suspected (look for areas of focal hyperostosis or lysis/thinning of the calvarium). Bulla radiographs are indicated in cases of middle/inner ear disease (otitis, neoplasia). Computed tomography (CT) is a sensitive imaging modality for middle/inner ear disease in the cat. Plain spinal radiographs and myelography are sometimes useful, but high-quality magnetic resonance imaging (MRI) of the spinal cord is the most sensitive means of detecting intramedullary lesions in cats. MRI is also the diagnostic test of choice for imaging of intracranial neoplastic masses in cats. Because of the expense of MRI, it is usually performed if owners are interested in surgery and/or radiation therapy for their pet. Electrodiagnostic testing is used most frequently in cases of motor unit (peripheral nervous system) disease. Electromyography (EMG), nerve conduction tests, and repetitive nerve stimulation are commonly used in the cat to help localize a lesion to nerve, muscle, or neuromuscular junction. Muscle and/or nerve biopsies are indicated if EMG and nerve conduction tests are abnormal. SELECTED DISORDERS Diseases of the Forebrain Lesions of the forebrain in cats typically cause signs of behavior change, seizures, circling or body turn toward the side of the lesion, contralateral visual deficits, and contralateral postural deficits (slow hopping reactions). Any or all these signs may be present. Head trauma, infectious agents (FIP, toxoplasmosis, cryptococcosis), feline ischemic encephalopathy (FIE) and other vascular disorders, and neoplastic diseases may cause forebrain signs in cats. FIE refers to a condition of unilateral cerebrocortical infarction due to vasospasm and/or occlusion of the middle cerebral artery. Typical signs of FIE include a peracute onset of circling, behavior change, visual deficits, and seizures. In some cases, seizures may be the only sign observed.9,10 Recently, FIE has been associated with aberrant migration of Cuterebra spp. larvae in the cat brain.10 This finding may relate to the high incidence of FIE in the late summer and
90
PROCEEDINGS OF THE 23rd WALTHAM/OSU SYMPOSIUM
early fall, times of the year when Cuterebra spp. are most prevalent in the environment. The most common cause of forebrain signs in older cats is neoplasia. Among primary brain tumors, feline meningiomas are by far the most common tumors found and are also a frequent cause of seizures in this age group. The signs, diagnosis, and treatment of feline meningiomas are discussed next. Meningiomas Feline meningiomas may arise from meninges (the arachnoid layer) covering the cerebral cortex, brain stem, falx and tentorium, or tela choroidea of the third ventricle. The most common site of involvement is the external surface of the cerebral cortex.11,12 As the tumor grows and expands, adjacent brain tissue is slowly compressed but rarely invaded directly by neoplastic cells. The brain has an enormous capacity to compensate for slowly compressive lesions, which is why signs may be so insidious in onset. In many cases, the signs reported by owners are subtle and include mild lethargy, decreased appetite, decreased responsiveness, and pacing. Seizures (partial or generalized) may be the only sign observed. A thorough neurologic examination may uncover contralateral postural and visual field deficits. It is not uncommon for large, space-occupying meningiomas to cause positional nystagmus. This is probably due to elevated intracranial pressure and early forebrain herniation with brain stem compression.11,12 MRI is the diagnostic test of choice to image the tumor and also can be used to plan an eventual surgical approach. Signs are initially prednisone responsive for many weeks, until the tumor reaches a critical volume. If signs of early herniation are present, mannitol therapy (1 g/kg IV over 20 minutes) may be required to stabilize the patient. The treatment of choice is surgical resection. The tumor often shells out because it is so well encapsulated. Recurrence may or may not occur in months to years. In one study, 6 out of 10 cats that underwent surgical meningioma resection lived for longer than 2 years postsurgery.13 Antiepileptic drug (AED) therapy is often required postoperatively to control seizures. Idiopathic Epilepsy Primary or inherited epilepsy, as found in many canine breeds, is not commonly recognized in cats. Some feline patients with epilepsy are classified as idiopathic when no obvious lesions are found through antemortem diagnostic tests (including CSF analysis, MRI, etc.). It is important to realize that previous insults (traumatic, inflammatory, vascular) to
the brain often leave little evidence of a lesion, even on MRI. The insult, however, may leave an area of hyperexcitable brain tissue (a seizure focus) that leads to a condition of epilepsy (recurrent seizure activity of neural origin). Treatment of epilepsy in the cat is similar to treatment of epilepsy in the dog, but there are some important differences. Phenobarbital is considered the first drug of choice for feline epilepsy. Phenobarbital is metabolized at a slower rate in the cat than in the dog, and cats are generally more susceptible to the sedative effects of the drug. The recommended starting dose is 2.5 mg/kg daily.14 This dose may need to be increased, depending on serum concentrations actually achieved and response to therapy. The therapeutic blood concentration in cats is 10 to 30 g/ml, which differs from the 15 to 40 g/ml therapeutic range in dogs. Steady-state phenobarbital concentrations are attained in about 9 days.14 Concurrent administration of drugs that are highly protein bound, such as sulfonamides and aspirin, should be avoided. Potential side effects of phenobarbital in the cat are excessive sedation, behavior change, dermatitis, and blood dyscrasias. 15 Hepatotoxicity has been reported with phenobarbital therapy in cats, but this author has not observed this side effect. The pharmacokinetics of potassium bromide (KBr) has recently been examined in the cat.16 The dose required to achieve blood concentrations in the 100 to 150 mg/dl range is similar to that used in dogs (30 mg/kg daily). The half-life of KBr in cats is 10 days, which is considerably shorter than that in dogs (2128 days). This means that steady-state drug concentrations of bromide in cats are achieved in 7 to 8 weeks. Efficacy of KBr in feline epilepsy is still not documented, although early reports claim that successful seizure control has been achieved in some patients. The best way to administer KBr in cats (because of their sensitivity to liquid preparations) is as capsules containing 50 to 100 mg of active compound per capsule.15 Diazepam is an effective oral AED in cats. The recommended dose is quite variable in the literature. This author usually starts at 0.5 mg/kg every 8 to 12 hours and increases the dose in increments if satisfactory seizure control is not achieved. A recent report of fulminant hepatotoxicity in a small number of cats has caused diazepam to fall out of favor as a first-line AED.17 Careful monitoring of ALT after 1 week and again after 1 month of therapy usually detects this idiosyncratic drug reaction. Clorazepate has been used by the Neurology Service at The Ohio State University Veterinary Hospital
ADVANCES IN FELINE NEUROLOGY
91
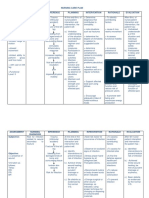
Table 1 Commonly Used Antiepileptic Drugs in Cats
Antiepileptic Drug Phenobarbital Dose and Dose Interval 2.5 mg/kg PO every 1224 hours Approximate Half-Life IV: 3643 hours PO: 58 hours PO: 1520 hours (diazepam and metabolites) 10 days Time to Steady State 9 days Therapeutic Range 1030 g/ml
Diazepam
0.52 mg/kg PO every 812 hours
45 days (calculated)
0.50.7 g/ml (?)
Potassium bromide
30 mg/kg PO every 24 hours or divided every 12 hours 3.757 mg PO per cat every 1224 hours
78 weeks
Not established
Clorazepate
3.6 hours (?) (N-desmethyl-diazepam)
Unknown
Unknown
IV = intravenously; PO = per os.
as a long-term AED in several epileptic cats. This AED is especially useful for persistent partial seizures in cats.14 The recommended dose is 3.75 to 7 mg per cat daily. Rarely, this may need to be increased to a twice daily dosing interval. Excellent seizure control in this small population of cats suggests that clorazepate may be a very effective AED in the feline. See Table 1 for a list of the most commonly used AEDs in cats. Diseases of the Brain Stem The cat brain stem is highly susceptible to a variety of disorders. C. neoformans, FIP virus, and Toxoplasma gondii commonly affect brain stem structures. The primary sign of brain stem involvement from any cause is a central vestibular syndrome. Head tilt, vestibular ataxia, and nystagmus are common features of this syndrome. Specific diagnostic and therapeutic recommendations for cryptococcosis, toxoplasmosis, and FIP are discussed in the next sections. Cryptococcosis C. neoformans can cause signs of nasal, ocular, and nervous system disease in cats. A chronic mucoid nasal discharge in conjunction with central vestibular signs (ataxia, nystagmus) or seizures should immediately raise ones suspicions for this disease. Clinical signs of CNS involvement are due to the inflammatory response to the organism (granulomatous meningoencephalomyelitis) or to a coalescence of large aggregates of encapsulated organisms, resulting in a mass lesion. Signs may be multifocal or focal. Some cats may also exhibit weight loss, coughing, subcutaneous granulomas around the face and nose, and lymphadenopathy. Serum and/or CSF antigen titers, as previously discussed, are highly sensitive and specific.2,9,11 CSF analysis usually shows a mixed pleocytosis and a mild to moderate elevation in protein. Occasion-
ally, organisms can be seen in CSF, especially if India ink staining is used. Cytology of nasal exudates often reveals the organism (512 m in diameter budding yeasts with a thick capsule). The treatment of choice is currently fluconazole 50 mg/cat every 12 hours for a minimum of 2 to 4 months, although long-term studies of efficacy for CNS disease have not been performed on a large population of cats.24 Itraconazole therapy 10 to 25 mg/kg every 24 hours for 4 to 16 months is useful for treatment of extraneural signs, but its efficacy for CNS infection has not been adequately studied.3 Traditionally, cats with CNS cryptococcosis have been given poor prognoses for recovery. As newer antifungal pharmaceutical agents become available, this outlook may change (Table 2). In studies of cats infected with Cryptococcus but not showing CNS signs, serum antigen titers have been followed over time during and after treatment. In one study, titers generally decreased during therapy and this tended to coincide with clinical improvement.3 However, positive titers were seen in some recovered cats in another study.4 Although the results of the two studies on this subject differ somewhat, it appears that some cats retain a positive titer after treatment and do not show clinical signs of infection. Current recommendations for therapy are to treat 2 to 3 months beyond resolution of clinical signs. If titers become negative, two negative antigen titers 1 month apart are recommended before therapy is discontinued.3,4 Toxoplasmosis Toxoplasmosis is a very interesting and still not fully understood infection of the CNS of cats. Many cats previously infected with T. gondii have bradyzoite organisms encysted in various tissues, including brain and muscle. In most cats, these encysted organisms
92
PROCEEDINGS OF THE 23rd WALTHAM/OSU SYMPOSIUM
Table 2 Antimicrobial Drugs for Central Nervous System Infections in Cats
Drug Amphotericin B Ampicillin Cefotaxime Ceftriaxone Cephalexin Chloramphenicol Clavamox Clindamycin Doxycycline Enrofloxacin Fluconazole Flucytosine Gentamicin Itraconazole Ketoconazole Metronidazole Penicillin G Pyrimethamine Tetracycline Trimethoprimsulfadiazine Target Pathogen(s) Cryptococcus spp./other fungi Bacteria Bacteria Bacteria Bacteria Bacteria/Rickettsia spp. Bacteria Toxoplasma spp. Bacteria/Rickettsia spp. Bacteria/Rickettsia spp. Cryptococcus spp./other fungi Cryptococcus spp./other fungi Bacteria Cryptococcus spp./other fungi Cryptococcus spp./other fungi Bacteria (anaerobic) Bacteria Toxoplasma spp. Bacteria/Rickettsia spp. Toxoplasma spp./bacteria BBB Penetration Poor Intermediate Good Good Poor Good Poor Poor Intermediate Intermediate Good Good Poor Poor Poor Good Intermediate Good Poor Good Bactericidal vs Bacteriostatic Static Cidal Cidal Cidal Cidal Static Cidal Static Static Cidal Static Static Cidal Static Static Cidal Cidal Cidal Static Cidal Dose (mg/kg) 0.150.5 (in 5% dextrose in water) 1020 2550 20 1030 1525 1020 12.525 2.55.0 2.55.0 510 2550 2.04.0 5 510 25 20,00040,000 units/kg 0.51.0 1520 1530 Route IV IV IV or IM IV PO PO PO PO PO PO PO PO IV or IM PO PO PO IV PO PO PO Frequency (hours) 48 6 8 12 8 12 812 12 12 12 12 68 8 1224 812 1224 6 24 8 12
BBB = blood-brain barrier; IM = intramuscularly; IV = intravenously; PO = per os.
remain in this latent phase, may produce some chronic antigenic stimulation, but are usually incidental. Immunocompromising factors (steroid therapy, viral infection [FIV or FeLV], stress, neoplasia) appear to initiate the recrudescence of these organisms. During recrudescence, organisms enter a proliferative phase and incite an inflammatory response. The inflammatory response can be exuberant, with formation of microscopic and macroscopic granulomas. Typical signs of multifocal or focal CNS injury include seizures (often partial seizures), central vestibular signs, cerebellar signs, and, occasionally, cord signs.6,9,18 As discussed previously, paired serum titers or combination serum/CSF titers are very useful in diagnosing CNS toxoplasmosis. This author prefers to use CSF titers and the IgG index to estimate intrathecal antibody production. This information combined with compatible clinical signs is usually adequate to make a tentative diagnosis of toxoplasmosis. CSF cytology may show a mixed pleocytosis (usually nonsuppurative, although neutrophils may be present also). Protein in CSF may be normal to moderately elevated. The treatment of choice for toxoplasmosis is either clindamycin or trimethoprim-sulfadiazine with pyrimethamine (Table 2). Although clindamycin is
usually better tolerated by cats, its penetration of the intact blood-brain and blood-CSF barriers is marginal at best. In human studies, clindamycin did not cross the blood-brain barrier even if meningitis was present. Despite this finding, clindamycin is advocated for use in feline CNS toxoplasmosis at 25 mg/kg every 12 hours for 4 to 6 weeks.18 The author has recently used clindamycin in an infected cat (positive CSF titers) with CNS signs. Clinical signs disappeared while the cat was treated with the drug. When the drug was discontinued, the cats clinical signs returned in 4 to 8 weeks. Trimethoprimsulfadiazine at 15 to 30 mg/kg every 12 hours for 3 to 4 weeks with or without pyrimethamine (0.51.0 mg/kg/day orally for 710 days) may also be effective. This drug combination may cause signs of nausea and salivation in cats and also has the potential of producing bone marrow suppression. Folic acid supplementation (1 mg/kg orally every 24 hours) is recommended for cats on long-term sulfadiazine/ pyrimethamine therapy.18,19 Feline Infectious Peritonitis The FIP virus (dry form) can cause a granulomatous to pyogranulomatous inflammation of the meninges, ependyma (ventricular linings) and subependymal tis-
ADVANCES IN FELINE NEUROLOGY
93
sues, and choroid plexus. Central vestibular signs are the most common neurologic signs seen with FIP virus infection of the CNS. Feline infectious peritonitis virus is also a common cause of seizures in cats less than 1 year of age. Hyperesthesia and caudal paresis may be seen with spinal cord involvement. A secondary hydrocephalus (with dullness, blindness, etc.) can occur because of obstruction of the fourth ventricle by fibrinous exudate and pyogranulomatous tissue. A cavernous sinus syndrome with a unilateral fixed pupil, ophthalmoplegia, and absent ocular sensation has recently been seen with FIP infection of the forebrain in cats.9 FIP is primarily found in very young cats, and clinical signs are more likely to occur after repeated exposure to the virus. Ocular signs, fever, weight loss, and anorexia often accompany CNS signs. A definitive diagnosis of FIP can be made only by finding pyogranulomatous inflammation in multiple tissues at necropsy.57 A tentative diagnosis is supported by high coronavirus titers and a CSF tap that shows a neutrophilic pleocytosis (some mononuclear inflammation also may be seen) and a very elevated protein content (often greater than 200 mg/dl). Coronavirus titers may be negative in some affected cats.57 Recently, molecular techniques (probes generated against FIV RNA in leukocytes and probes generated by polymerase chain reaction against smaller viral nucleotides) are showing some promise for definitive diagnosis of virulent FIP strains. There is no effective treatment for CNS FIP. Prednisone and other immunosuppressive/immunomodulatory therapy may help in the short term, but the disease is invariably progressive and ultimately fatal. Some vaccines have shown some efficacy in protection against experimental FIP challenge in cats, but efficacy against natural exposure requires further study. Peripheral Vestibular Disease Causes of peripheral vestibular problems in cats include idiopathic vestibular syndrome, inflammatory polyps, otitis (mites/bacteria), and middle and inner ear neoplasia (ceruminous gland adenocarcinoma and squamous cell carcinoma are the most common). Infections or mass lesions of the middle and inner ear may produce vestibular signs (head tilt, ataxia with or without nystagmus), cranial nerve VII signs (facial paralysis), and Horners syndrome. Idiopathic feline vestibular syndrome is the most common cause of peripheral vestibular signs in cats. Only vestibular signs are present and these signs may be severe (pronounced head tilt, rolling, falling, rotary or horizontal nystagmus with fast phase away from the side of the lesion). This disorder is usually seen in
the late summer or early fall and, like FIE, coincides with the time of year when Cuterebra larvae are abundant. Peracute signs are usually self-limiting over 3 to 7 days with no treatment. Supportive care (nutritional support, intravenous or subcutaneous fluids, etc.) may be necessary if anorexia, vomiting, or both accompany the vestibular signs. Spinal Cord Diseases Spinal cord diseases in cats are relatively uncommon compared to the dog. Intervertebral disk herniation can occur in cats, but clinical disease is extremely rare. More common causes of spinal cord injury include trauma, infectious meningomyelitis (as from toxoplasmosis, cryptococcosis, FIP), lymphosarcoma, and other neoplastic processes. Recently, vaccineassociated fibrosarcomas have been identified that have invaded the spinal canal and spinal cord following surgical excision from subcutaneous and muscular tissues. Spinal radiographs, CSF analysis, serum and CSF titers, and sometimes myelography or MRI are indicated in a cat with spinal cord signs. This author recommends myelography if CSF analysis is normal and an extradural lesion is suspected. MRI is preferred if an intramedullary lesion is suspected. Intramedullary lesions in cats include infectious myelitis (inflammation of the cord parenchyma itself), intradural lymphosarcoma, and intramedullary glial tumors (gliomas). Treatment guidelines depend on the underlying cause. Spinal cord lymphosarcoma carries a poor prognosis, but temporary remission of clinical signs can sometimes be achieved with chemotherapy. 20 Cobalt 60 teletherapy may also provide some benefit if used in conjunction with chemotherapy. Combined therapy may provide remission of clinical signs in many cats, but relapses often occur within 6 months of onset of treatment.20 FeLV status should be checked because prognosis and response to therapy tend to be poorer in FeLV-positive cats. If trauma (vertebral fracture/luxation or a traumatic disk) is the source of injury, medical therapy is indicated and surgical decompression and stabilization may be necessary. The cat served as one of the major animal models of spinal cord injury in the mid to late 1980s, and methylprednisolone sodium succinate (MPSS, or Solu-Medrol [Pharmacia & Upjohn]) therapy trials were attempted in cats during this time. Solu-Medrol was shown to be effective for spinal trauma if administered at 30 mg/kg within several hours of the trauma.21 Subsequent doses of 15 mg/kg at 2 hours and 6 hours followed by a constant rate infusion at 2.5 mg/kg/hour for 24 to 48 hours also im-
94
PROCEEDINGS OF THE 23rd WALTHAM/OSU SYMPOSIUM
proved outcome. The primary mechanism of action of MPSS is its ability to scavenge free radicals and prevent lipid peroxidation of cell membranes.21 The limiting factor is that this drug is effective only if administered within hours of injury. Its use beyond 6 to 8 hours of injury probably provides little benefit. Motor Unit Disorders Motor unit diseases in cats are uncommon. Myopathies and neuropathies may occur but are often secondary to metabolic or endocrine disorders. Acquired myasthenia gravis (MG) is found sporadically in cats, especially in purebred or mixed Abyssinian and Somali breeds. This is an immune-mediated junctionopathy characterized by the presence of autoantibodies directed against the acetylcholine receptor on the muscle membrane. The typical clinical signs are development of a stiff, choppy gait with exercise, severe weakness and/or collapse, ventral neck flexion due to cervical muscle weakness, and weak palpebral reflexes.22,23 One cat described in the literature had signs of focal MG (dropped jaw and dysphagia due to focal cranial nerve involvement).24 Megaesophagus is also a common finding. The definitive test for acquired MG is the serum acetylcholine receptor antibody test, but because serum has to be sent to special laboratories that perform this test, there is often a significant time delay before results are known. Intravenous injection of edrophonium chloride, a short-acting anticholinesterase drug, will alleviate clinical signs for a few minutes and is a provocative diagnostic test for MG. According to one author, the response of cats to Tensilon (ICN) is not as predictable as it is in dogs.19 Repetitive nerve stimulation is quite reliable, although other neuromuscular junction disorders (botulism, chronic organophosphate toxicity) can also cause a decremental response during stimulation. Treatment is directed at treating the immune-mediated disorder with prednisone and/or other immunosuppressive agents. Concurrent treatment with long-acting anticholinesterase agents (pyridostigmine bromide at 0.53.0 mg/kg orally every 8 to 12 hours) is also helpful in alleviating the tetraparetic state. Cats have a greater sensitivity to pyridostigmine bromide than do dogs, so starting at 0.5 mg/kg and slowly titrating upward until a clinical response is seen is the most rational approach.19,24 Myasthenia gravis in the cat is often self-limiting, but signs can persist for months before clinical remission is achieved. Monitoring the serum acetylcholine receptor antibody titer is used as a gauge to decide when to start tapering immunosuppressive therapy. Feline Hyperesthetic Syndrome Feline hyperesthetic syndrome is a poorly under-
stood disorder characterized by episodes of agitation, rippling of the thoracolumbar muscles, swishing of the tail, biting of the pelvic limbs and lumbosacral region, vocalization, and often running frantically as if startled. Various explanations for this behavior have been proposed, including a psychic behavioral disturbance, allergic skin disease, partial complex seizure, and true hyperesthesia due to focal spinal cord or nerve root disease. This author has attempted hypoallergenic diets, serotonin reuptake inhibitor therapy (fluoxetine, tricyclic antidepressants, etc.), antiepileptic drug therapy, and corticosteroid drug therapy with little success. Recently, the Neurology Service at The Ohio State University Veterinary Teaching Hospital has identified EMG changes and pathologic alterations in epaxial muscles of affected cats. Abnormalities in muscle include the presence of inclusion bodies that resemble those found in inclusion body myopathies of humans. Although the significance of these inclusions is as yet unknown, they may provide a clue to the etiology of this syndrome. CONCLUSIONS Cats with signs of neurologic disease may be difficult to diagnose because of problems inherent in performing a thorough neurologic examination and because of the great number of acquired disorders that can affect cats. Localization of the lesion(s) to specific compartments of the nervous system helps to narrow down the list of differential diagnoses, but, ultimately, extensive ancillary diagnostic testing is required to determine the etiologic basis of the clinical signs. Considerable progress has been made recently in the diagnosis and therapy of CNS cryptococcosis and toxoplasmosis. Clearly, understanding the long-term efficacy of many antimicrobial agents in the treatment of CNS infections is an area of weakness. On the other hand, therapy for other disorders (epilepsy, spinal trauma, neoplasia, myasthenia gravis, etc.) has expanded dramatically in the last decade and many treatment options are available. Greater knowledge of the dynamic interplay between the CNS and the systemic response to injury is critical for the development of rational therapeutic strategies for feline nervous system disease in the future. REFERENCES
1. Spodnick GJ, Berg J, Moore FM, Cotter SM: Spinal lymphoma in cats: 21 cases (19761989). JAVMA 3:373376, 1992. 2. Malik R, Wigney DI, Muir DB, et al: Cryptococcosis in cats: Clinical and mycological assessment of 29 cases and evaluation of treatment using orally administered fluconazole. J Med Vet Mycol 30:133144, 1992. 3. Jacobs GJ, Medleau L, Calvert C, Brown J: Cryptococcal infection in cats: Factors influencing treatment outcome, and results of sequential serum antigen titers in 35 cats. J Vet Intern Med 11:14, 1997. 4. Flatland B, Greene RT, Lappin MR: Clinical and serologic evaluation of cats
ADVANCES IN FELINE NEUROLOGY
95
with cryptococcosis. JAVMA 209:11101113, 1996. 5. Baroni M, Heinhold Y: A review of the clinical diagnosis of feline infectious peritonitis viral meningoencephalomyelitis. Prog Vet Neurol 6:8894, 1995. 6. Munana KR: Encephalitis and meningitis. Vet Clin North Am Small Anim Pract 26:857873, 1996. 7. Weiss RC: Feline infectious peritonitis and other coronaviruses, in Sherding RG (ed): The Cat: Diseases and Clinical Management, ed 2. New York, Churchill Livingstone, 1994, pp 449477. 8. Glass E, de Lahunta A, Kent M, et al: A cryptococcal granuloma in the brain of a cat causing focal signs. Prog Vet Neurol 7:141144, 1996. 9. Fenner WR: Diseases of the brain, spinal cord, and peripheral nerves, in Sherding RG (ed): The Cat: Diseases and Clinical Management, ed 2. New York, Churchill Livingstone, 1994, pp 15071567. 10. Glass E, Cornetta AM, de Lahunta A, et al: Clinical and clinicopathologic features in 11 cats with Cuterebra larvae myiasis of the central nervous system. J Vet Intern Med 12:365368, 1998. 11. Nafe LA: Meningiomas in cats: A retrospective clinical study of 36 cases. JAVMA 174:12241227, 1979. 12. Schrader SC: Neurosurgery, in Sherding RG (ed): The Cat: Diseases and Clinical Management, ed 2. New York, Churchill Livingstone, 1994, pp 15771598. 13. Lawson DC, Burk RL, Prata RG: Cerebral meningioma in the cat: Diagnosis and surgical treatment of ten cases. JAAHA 20:333342, 1984. 14. Podell M: Antiepileptic drug therapy. Clin Tech Small Anim Pract 13:185192, 1998.
15. Boothe DM: Anticonvulsant therapy in small animals. Vet Clin North Am Small Anim Pract 28:411448, 1998. 16. George K, Boothe DM, Nguyen J, Legrange S: Disposition of bromide in cats following oral administration of the potassium salt. San Antonio, Proc 14th ACVIM Forum, 1996, p 757. 17. Hughes D, Moreau RE, Overall KL, Van Winkle TJ: Acute hepatic necrosis and liver failure associated with benzodiazepine therapy in six cats, 19861995. J Vet Emergency Crit Care 6(1):1320, 1996. 18. Lappin MR: CVT update: Feline toxoplasmosis, in Bonagura JD (ed): Kirks Current Veterinary Therapy XII: Small Animal Practice. Philadelphia, WB Saunders, 1995, pp 309314. 19. Cuddon PA: Feline neuromuscular diseases, in Kirk RW, Bonagura JD (eds): Current Veterinary Therapy XI: Small Animal Practice. Philadelphia, WB Saunders, 1992, pp 10241031. 20. Couto CG, Hammer AS: Oncology, in Sherding RG (ed): The Cat: Diseases and Clinical Management, ed 2. New York, Churchill Livingstone, 1994, pp 755818. 21. Hall ED: Review Article: The neuroprotective pharmacology of methylprednisolone. J Neurosurg 76:1322, 1992. 22. Joseph RJ, Carrillo JM, Lennon VA: Myasthenia gravis in the cat. J Vet Intern Med 2:7579, 1988. 23. Indrieri RJ, Creighton SR, Lambert EH, Lennon VA: Myasthenia gravis in two cats. JAVMA 182:5760, 1983. 24. Shelton GD: Disorders of neuromuscular transmission. Semin Vet Med Surg Small Anim 4:126132, 1989.
You might also like
- Convulsiones Gatos 2Document13 pagesConvulsiones Gatos 2Aleja Torres GaviriaNo ratings yet
- Neurological Manifestations of Common Inflammatory DiseasesDocument17 pagesNeurological Manifestations of Common Inflammatory DiseasesvetthamilNo ratings yet
- Acutelowermotorneuron Tetraparesis: Sònia AñorDocument22 pagesAcutelowermotorneuron Tetraparesis: Sònia AñorWira KusumaNo ratings yet
- Equine Protozoal MyeloencephalitisDocument4 pagesEquine Protozoal Myeloencephalitisfreak009No ratings yet
- Toxoplasmosis y NeosporaDocument12 pagesToxoplasmosis y NeosporaAntonio ReaNo ratings yet
- 1 s2.0 S0749073922000219 MainDocument15 pages1 s2.0 S0749073922000219 Mainbdjxk95cyhNo ratings yet
- Tetanus in Dogs Clinical Signs and ManagementDocument10 pagesTetanus in Dogs Clinical Signs and ManagementLonely WolfNo ratings yet
- Neurological Examination and Diagnostic Testing in Birds and ReptilesDocument18 pagesNeurological Examination and Diagnostic Testing in Birds and ReptilesAnnie Ariza Palacio100% (1)
- Veterinary Internal Medicne - 2023 - Liatis - Idiopathic and Structural Episodic Nonintentional Head Tremor in Dogs 100Document9 pagesVeterinary Internal Medicne - 2023 - Liatis - Idiopathic and Structural Episodic Nonintentional Head Tremor in Dogs 100Jairo OrtegaNo ratings yet
- Neurological Examination in Small AnimalsDocument11 pagesNeurological Examination in Small AnimalsAriana ZegarraNo ratings yet
- Neur CL in Pract 2013005694Document10 pagesNeur CL in Pract 2013005694Haha RowlingNo ratings yet
- Clinical Approach andDocument21 pagesClinical Approach andtavooppNo ratings yet
- Canine Distemper: Morbillivirus. Despite Vaccination, It Remains An Important Cause of Encephalitis in DogsDocument2 pagesCanine Distemper: Morbillivirus. Despite Vaccination, It Remains An Important Cause of Encephalitis in DogsNabin NeupaneNo ratings yet
- Practical Neurology (Cerebellar Ataxia)Document11 pagesPractical Neurology (Cerebellar Ataxia)idno1008No ratings yet
- Cat Blood NeutrophilsDocument12 pagesCat Blood Neutrophilsnora ivanovaNo ratings yet
- Cerebral Palsy Sumber AaprmDocument6 pagesCerebral Palsy Sumber AaprmBiandaNo ratings yet
- CVJ 10 1091Document3 pagesCVJ 10 1091Rayza LubisNo ratings yet
- Clinical Cases in Pediatric Peripheral NeuropathyDocument23 pagesClinical Cases in Pediatric Peripheral NeuropathyMateen ShukriNo ratings yet
- Peripheral Neuropathy Diff Diagnosis and Management AafpDocument6 pagesPeripheral Neuropathy Diff Diagnosis and Management Aafpgus_lions100% (1)
- Neurologic Diseases of RuminantsDocument6 pagesNeurologic Diseases of Ruminantsh8tcsfmmndNo ratings yet
- An Algorithm For The Evaluation of Peripheral Neuropathy - American Family PhysicianDocument9 pagesAn Algorithm For The Evaluation of Peripheral Neuropathy - American Family PhysicianAnonymous vnv6QFNo ratings yet
- 17 The Peripheral Nervous SystemDocument12 pages17 The Peripheral Nervous Systemkarar AhmedNo ratings yet
- Paraneoplastic Neurologic Syndromes Are Defined and Characterized by An Inappropriate Immune Response Targeting Native Nervous System Antigens That Are Ectopically Expressed by A Systemic TumorDocument11 pagesParaneoplastic Neurologic Syndromes Are Defined and Characterized by An Inappropriate Immune Response Targeting Native Nervous System Antigens That Are Ectopically Expressed by A Systemic TumorAnonymous ZUaUz1wwNo ratings yet
- Meningoencephaltis of Unknown Origin (MUO) : Client FactsheetDocument3 pagesMeningoencephaltis of Unknown Origin (MUO) : Client FactsheetCoote Castro RetamalNo ratings yet
- VEM5384 Clincial Neurology DisordersDocument62 pagesVEM5384 Clincial Neurology DisordersdeadnarwhalNo ratings yet
- Desordenes Musculares GatosDocument13 pagesDesordenes Musculares GatosDulce BorbollaNo ratings yet
- tmpD6CD TMPDocument8 pagestmpD6CD TMPFrontiersNo ratings yet
- TachdjianDocument25 pagesTachdjianduracell54No ratings yet
- A Cohort Study To Assess The New WHO Japanese Encephalitis Surveillance StandardsDocument9 pagesA Cohort Study To Assess The New WHO Japanese Encephalitis Surveillance StandardsarmankoassracunNo ratings yet
- Jvim 15681Document39 pagesJvim 15681daniruizcasNo ratings yet
- 4 5827873873068033714Document1,947 pages4 5827873873068033714s.oana90No ratings yet
- Differential Diagnoses of SeizuresDocument6 pagesDifferential Diagnoses of SeizureslinevetNo ratings yet
- Longterm Outcome Neonatal MeningitisDocument7 pagesLongterm Outcome Neonatal MeningitisElizabeth Joan SalimNo ratings yet
- Enfermedad GlomerularDocument7 pagesEnfermedad GlomerularKatty ZanabriaNo ratings yet
- G. Rees Cosgrove, M.D., F.R.C.S. (C) and Andrew J. Cole M.D., FRCP (C)Document11 pagesG. Rees Cosgrove, M.D., F.R.C.S. (C) and Andrew J. Cole M.D., FRCP (C)Jean Costan RNNo ratings yet
- Cerebrospinal Fluid and Blood Biomarkers of Status Epilepticus - 2020Document40 pagesCerebrospinal Fluid and Blood Biomarkers of Status Epilepticus - 2020Reny Wane Vieira dos SantosNo ratings yet
- Necrotizing Cerebellitis Neospora JVIM 2010Document8 pagesNecrotizing Cerebellitis Neospora JVIM 2010Rafael Porto GoncalvesNo ratings yet
- CANINE-CAnine Systemic Lupus Erythematosus - Part IDocument7 pagesCANINE-CAnine Systemic Lupus Erythematosus - Part Itaner_soysurenNo ratings yet
- Critical Care in NeurologyDocument65 pagesCritical Care in NeurologydrbhawnavermaNo ratings yet
- Encephalitozoon CuniculiDocument5 pagesEncephalitozoon CuniculiSebastián Ordóñez RamírezNo ratings yet
- Meningoencephalitis of Unknown Origin in Dogs CR - 881Document6 pagesMeningoencephalitis of Unknown Origin in Dogs CR - 881Ezequiel Davi Dos SantosNo ratings yet
- Javma-Javma 20 12 0706Document11 pagesJavma-Javma 20 12 0706Bright DerlacuzENo ratings yet
- Discoveries 08 110Document19 pagesDiscoveries 08 110Riki AntoNo ratings yet
- Neuropsychology in EpilepsyDocument47 pagesNeuropsychology in EpilepsydasilvaseamaNo ratings yet
- Immune Mediated Pediatric Encephalitis - Need For Comprehensive Evaluation and Consensus GuidelinesDocument8 pagesImmune Mediated Pediatric Encephalitis - Need For Comprehensive Evaluation and Consensus GuidelinesJudit SzamosujvariNo ratings yet
- Recognition and Management of Pediatric Seizures: Steven M. Wolf, MD and Patricia Engel Mcgoldrick, NPDocument12 pagesRecognition and Management of Pediatric Seizures: Steven M. Wolf, MD and Patricia Engel Mcgoldrick, NPAbdullah Shidqul AzmiNo ratings yet
- Translate Fira IngDocument6 pagesTranslate Fira IngRio Taruna JatiNo ratings yet
- Seizure Disorder CaseStudyDocument29 pagesSeizure Disorder CaseStudyAnn50% (2)
- A Child With Myoclonus-Dystonia (DYT11) Misdiagnosed As Atypical Opsoclonus Myoclonus SyndromeDocument3 pagesA Child With Myoclonus-Dystonia (DYT11) Misdiagnosed As Atypical Opsoclonus Myoclonus SyndromeStephen AttardNo ratings yet
- Approach To The Seizure PatientDocument9 pagesApproach To The Seizure PatientOzkar JaraNo ratings yet
- 2022 Masingue P.Latour Rev Neurol Genetic Analysis in HereditaryDocument20 pages2022 Masingue P.Latour Rev Neurol Genetic Analysis in HereditaryLéo VidoniNo ratings yet
- Initial Evaluation VertigoDocument8 pagesInitial Evaluation VertigoTanri Hadinata WiranegaraNo ratings yet
- Convulsion Febril PediatricsDocument11 pagesConvulsion Febril PediatricsOrlando HernandezNo ratings yet
- Neuropathology Simplified: A Guide for Clinicians and NeuroscientistsFrom EverandNeuropathology Simplified: A Guide for Clinicians and NeuroscientistsNo ratings yet
- Pedsinreview 2021005096supplementarydataDocument52 pagesPedsinreview 2021005096supplementarydataFelipe VergaraNo ratings yet
- Seizure Disorders in Goats and SheepDocument6 pagesSeizure Disorders in Goats and SheepYaserAbbasiNo ratings yet
- Ataxia AcutaDocument17 pagesAtaxia AcutaAlina AndreiNo ratings yet
- Straight Back SyndromeDocument1 pageStraight Back SyndromemisbahNo ratings yet
- Massive Transfusion ProtocolDocument2 pagesMassive Transfusion ProtocolmukriNo ratings yet
- Material ManagementDocument27 pagesMaterial ManagementGuna Ramya71% (7)
- Generic TPN Final Version 15sep13Document3 pagesGeneric TPN Final Version 15sep13AsriNo ratings yet
- Report DeglutologiaDocument28 pagesReport DeglutologiaDavide Capone100% (1)
- VISION 2020 Priority Eye DiseasesDocument7 pagesVISION 2020 Priority Eye DiseaseschandradwtrNo ratings yet
- EpispadiasDocument9 pagesEpispadiassheranadhilaNo ratings yet
- Acteon Surgery Clinical BookletDocument56 pagesActeon Surgery Clinical BookletJTDentalGroupNo ratings yet
- Nursing Care Plan Assessment Nursing Diagnosis Inference Planning Intervention Rationale Evaluation SubjectiveDocument2 pagesNursing Care Plan Assessment Nursing Diagnosis Inference Planning Intervention Rationale Evaluation SubjectiveDat boiNo ratings yet
- Proximal Stripping PDFDocument11 pagesProximal Stripping PDFsmilecarekkmNo ratings yet
- Pharma Ko VigilanceDocument20 pagesPharma Ko VigilanceIndah LindianaNo ratings yet
- APPA Protocol PDFDocument2 pagesAPPA Protocol PDFMarcos MartiniNo ratings yet
- Functional Results of Cataract Surgery in The Treatment of Phacomorphic GlaucomaDocument5 pagesFunctional Results of Cataract Surgery in The Treatment of Phacomorphic Glaucomachindy sulistyNo ratings yet
- BLS Healthcare Provider AlgorithmDocument7 pagesBLS Healthcare Provider AlgorithmyuniNo ratings yet
- Support Services SOPDocument18 pagesSupport Services SOPdamarwuNo ratings yet
- Fulminant Hepatic FailureDocument33 pagesFulminant Hepatic FailureRojan CardinalNo ratings yet
- Definition of Osteoporosis: Symptoms of OsteoporosisDocument3 pagesDefinition of Osteoporosis: Symptoms of OsteoporosisYing Flavia100% (2)
- Tools Used in Community DiagnosisDocument23 pagesTools Used in Community DiagnosisMaureen A. Bawang33% (3)
- Oral & Craniofascial PainDocument36 pagesOral & Craniofascial PainMaria Fudji hastutiNo ratings yet
- HCVDocument33 pagesHCVsherif555No ratings yet
- Health Teching Pak Tri GastritisDocument3 pagesHealth Teching Pak Tri GastritisCitra MahendraNo ratings yet
- WHO MC - Manual - 2018 PDFDocument403 pagesWHO MC - Manual - 2018 PDFchimbimbNo ratings yet
- September 2015 Ophthalmic PearlsDocument3 pagesSeptember 2015 Ophthalmic PearlsLouis WakumNo ratings yet
- Icon Strategies and Quality PracticeDocument4 pagesIcon Strategies and Quality PracticeSammy ChegeNo ratings yet
- Complex RestorationDocument59 pagesComplex Restorationsamar yousif mohamed100% (1)
- Incontinence 1Document2 pagesIncontinence 1lalitrajindoliaNo ratings yet
- Rectal SuppositoriesDocument2 pagesRectal SuppositoriesAngel Leo M. ZuñigaNo ratings yet
- Apollo Hospitals - Presentation (ETOP)Document24 pagesApollo Hospitals - Presentation (ETOP)p_sonera0% (1)
- CPR PDFDocument37 pagesCPR PDFArdhi AgustjikNo ratings yet
- CKAPS - Specialist ClinicsDocument11 pagesCKAPS - Specialist ClinicsGohdsNo ratings yet