Professional Documents
Culture Documents
Erros Com ESBL
Uploaded by
Daniela PécoraOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Erros Com ESBL
Uploaded by
Daniela PécoraCopyright:
Available Formats
ORIGINAL INVESTIGATION
Impact of Inadequate Initial Antimicrobial Therapy on Mortality in Infections Due to Extended-Spectrum -LactamaseProducing Enterobacteriaceae
Variability by Site of Infection
Emily P. Hyle, BS; Adam D. Lipworth, BS; Theoklis E. Zaoutis, MD; Irving Nachamkin, DrPH, MPH; Warren B. Bilker, PhD; Ebbing Lautenbach, MD, MPH, MSCE
Background: Infections due to extended-spectrum -lactamaseproducing Escherichia coli and Klebsiella species (ESBL-EK) have increased markedly in recent years. Risk factors for mortality among ESBL-EK infections have not been studied. Methods: This retrospective cohort study was conducted in a 625-bed tertiary care medical center and a 344-bed urban community hospital to determine whether inadequate initial antimicrobial therapy (IIAT) ( 48 hours between the time a culture was obtained and initiation of an agent to which the infecting organism was susceptible) is associated with mortality in ESBL-EK infections. All hospitalized patients with an ESBL-EK infection between June 1, 1997, and December 31, 2002, were eligible for inclusion. Subsequently, we conducted a nested case-control study to identify risk factors for IIAT. Results: Of 187 subjects, 32 (17.1%) died while in the
hospital. Clinical site of infection was a significant effect modifier in the association between IIAT and mortality. The presence of IIAT was an independent risk factor for mortality, but only for nonurinary ESBL-EK infections (adjusted odds ratio [95% confidence interval], 10.04 [1.90-52.96]). Independent risk factors for IIAT were (1) infection with a multidrug-resistant ESBL-EK (ie, resistant to sulfamethoxazole-trimethoprim, aminoglycosides, and quinolones) (14.58 [1.91-111.36]) and (2) health careacquired ESBL-EK infection (4.32 [1.4912.54]).
Conclusions: Inadequate initial antimicrobial therapy is an independent risk factor for mortality in ESBL-EK infections, but only among nonurinary infections. Multidrug resistance was a strong risk factor for IIAT.
Arch Intern Med. 2005;165:1375-1380 ings might also be applicable to ESBL-EK infections has not, to our knowledge, been studied. To investigate the association between inadequate initial antimicrobial therapy (IIAT) and mortality among patients with ESBL-EK infections, we conducted a retrospective cohort study. Furthermore, we investigated whether the relationship between IIAT and mortality varied across different clinical sites of infection (ie, urinary tract vs nonurinary). Finally, we conducted a nested casecontrol study to identify risk factors for IIAT among ESBL-EK infections.
METHODS This study was conducted at 2 hospitals in the University of Pennsylvania Health System located in Philadelphia: the Hospital of the University of Pennsylvania, a 625-bed academic tertiary care medical center, and Presbyterian Medical Center, a 344-bed urban community hospital. Eligible patients were identified
Author Affiliations are listed at the end of this article. Financial Disclosure: Dr Lautenbach previously received a research grant from Merck & Co and is currently a consultant for Elan Pharmaceuticals and Bayer Pharmaceuticals Corp.
of extended-spectrum -lactamaseproducing Escherichia coli and Klebsiella species (ESBL-EK) in the 1980s, their prevalence has increased steadily.1,2 Infections with ESBL-EK have been associated with increased morbidity, mortality, hospital length of stay, and hospital cost.3 These infections are particularly problematic because choices for antimicrobial therapy, both empirical and definitive, may be severely restricted given that these organisms are often resistant to multiple antibiotics and antibiotic classes.4,5 The possible reasons for worse outcomes among patients infected with ESBL-EK have not been elucidated. Recent studies of general bloodstream infections suggest that a delay in effective antimicrobial therapy may result in poorer outcomes and that inadequate antimicrobial therapy is more likely to occur in resistant infections.6-8 Whether these find-
INCE THE INITIAL EMERGENCE
(REPRINTED) ARCH INTERN MED/ VOL 165, JUNE 27, 2005 1375
WWW.ARCHINTERNMED.COM
Downloaded from www.archinternmed.com at ROYAL PERTH HOSPITAL, on June 30, 2005 2005 American Medical Association. All rights reserved.
through records of the clinical microbiological laboratory at the Hospital of the University of Pennsylvania, which processes and performs cultures of all clinical specimens obtained at these institutions. All inpatients who had an ESBL-EK infection between June 1, 1997, and December 31, 2002, were eligible for inclusion. Infection was defined on the basis of criteria of the Centers for Disease Control and Prevention.9 Subjects were included if documentation existed for both the antibiotic therapy administered and the patients in-hospital outcome (ie, survived or died). Patients could be included more than once if they had multiple positive ESBL-EK cultures during the study period. For a given patient, the first ESBL-EK infection was included, and subsequent infections were included only if they occurred more than 30 days after the initial infection. A retrospective cohort study was performed to investigate the association between IIAT and crude in-hospital mortality. Inadequate initial antimicrobial therapy was defined as greater than 48 hours elapsing between the time a culture was obtained and initiation of treatment with an antimicrobial agent to which the infecting organism was ultimately shown to be susceptible. Data were ascertained with regard to potential confounders and other risk factors for mortality. Data obtained included age, sex, race, hospital location at the time of infection, number of hospital days before infection, and severity of illness at the time of infection, as calculated by the Acute Physiology and Chronic Health Evaluation (APACHE) II score.10 The presence of a central venous catheter, urinary catheter, or mechanical ventilation was documented, as was the primary site of infection and the species of infecting organism. Health careacquired infection was defined as either (1) infection that occurred more than 48 hours after hospital admission or (2) infection that occurred 48 hours or less after admission to the hospital if that patient had been hospitalized within the 30 days before admission, or if the patient had been transferred from an outside hospital or long-term care facility.3,11 Of note, this definition is similar to recent recommendations for defining health careassociated infections.12 The following comorbid conditions were documented: hepatic dysfunction, malignancy, diabetes mellitus, renal insufficiency (indicated by a serum creatinine level 2.0 mg/dL [ 177 mol/L] or the requirement of dialysis), human immunodeficiency virus infection, neutropenia, previous organ transplantation, use of an immunosuppressive agent (including corticosteroids) in the 30 days before infection, and surgical procedure or trauma in the 30 days before infection.
MICROBIOLOGICAL TESTING
Susceptibilities to all antimicrobial agents were performed and interpreted according to criteria of the National Committee for Clinical Laboratory Standards by means of either a semiautomated system (MicroScan [Dade Behring, Deerfield, Ill] or Vitek [Bio Mrieux, Charbonnires les Bains, France]) or disk diffusion susceptibility testing. From 1997 to April 2000, we used previously described methods for detecting ESBL-EK.4 After that time, we used guidelines published by the National Committee for Clinical Laboratory Standards for detecting and confirming ESBL-EK.13-15
Fisher exact test. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated to evaluate the strength of any association. We calculated ORs rather than relative risks to facilitate comparison of unadjusted and adjusted ORs in the final multivariable model. Continuous variables were compared by 2-tailed t test or the Wilcoxon rank sum test, depending on the validity of the normality assumption.16 Stratified analyses were then conducted to help identify where data were sparse and to elucidate where confounding and interaction (effect modification) were likely to exist in the multivariable analysis. We were primarily interested in investigating the effect of stratification by site of infection (ie, urinary tract vs nonurinary) on the primary association of interest (ie, between IIAT and mortality). The Mantel-Haenszel test for summary statistics was used to evaluate for possible confounding,17 which was considered to be present if the crude and adjusted ORs differed by 15% or more. Interaction was assumed to be present when the test for heterogeneity between the ORs for different strata was significant (P .05). Multivariable analysis was performed by means of multiple logistic regression.18 Building of the multivariable model began with inclusion of the exposure of interest (ie, IIAT). All variables with P .20 on bivariable analysis were also considered for inclusion in a multivariable explanatory model.19 Finally, variables were considered for inclusion in the model if they were noted to be involved in confounding on stratified analysis. The interaction between risk factor variables was also investigated. After these primary analyses, we sought to identify risk factors for IIAT among ESBL-EK infections. For this analysis, we conducted a case-control study nested within the primary cohort study described above. We compared cases (ie, patients who received IIAT) with controls (ie, patients who received adequate therapy) to identify risk factors for IIAT. We were particularly interested in exploring the role of multidrugresistant (MDR) ESBL-EK isolates. We defined as MDR an ESBL-EK that also demonstrated resistance to the following antibiotics or antibiotic classes: (1) sulfamethoxazoletrimethoprim, (2) aminoglycosides (ie, amikacin, netilmicin, gentamicin, and tobramycin), and (3) fluoroquinolones (ie, ciprofloxacin, ofloxacin, and levofloxacin). Of note, if an ESBL-EK isolate was susceptible to any one of the drugs within a class (eg, aminoglycosides), the isolate was considered susceptible to the class. Bivariable, stratified, and multivariable analyses proceeded as already described. A 2-tailed P .05 was considered significant. All statistical calculations were performed by means of standard programs in Stata version 8.0 software (Stata Corp, College Station, Tex). RESULTS
STATISTICAL ANALYSIS
We first compared the incidence of mortality in subjects with inadequate and adequate initial antimicrobial therapy. Bivariable analyses were then conducted to determine the association between other potential risk factors or confounders and mortality. Categorical variables were compared by means of the
During the 5-year study period, 288 patients with ESBL-EK infections met eligibility criteria. Of these, 187 (64.9%) had complete medical records available for review. Of note, there were no significant differences when available data (ie, age, sex, race, species of infecting organism, susceptibility profile of infecting pathogen, location in the hospital, duration of hospitalization before infection, and disposition at discharge) were compared for patients who were and were not included. Of the 187 subjects included in the cohort, 97 (51.9%) were male. The median age of subjects was 65 years (95% CI, 61-68 years). Fifty-five patients (29.9%) were identified as white, 85 (45.5%) were African American, and 47 (25.1%) were of another or unknown race. At the time
WWW.ARCHINTERNMED.COM
(REPRINTED) ARCH INTERN MED/ VOL 165, JUNE 27, 2005 1376
Downloaded from www.archinternmed.com at ROYAL PERTH HOSPITAL, on June 30, 2005 2005 American Medical Association. All rights reserved.
120 100
Klebsiella Species Escherichia coli
18 16 14
P < .001 (2, Trend)
Mortality, %
80
12 10 8 6 4
Total No.
60 40 20 0
2 0 Urinary Respiratory Blood Wound Abdominal Skin/ Soft Tissue Other <24 <48 <72 <96 <120 120
Time to Institution of Effective Antimicrobial Therapy, h
Site of Infection
Figure 2. Delay in initial antimicrobial therapy and mortality. Figure 1. Sites of infection with extended-spectrum -lactamaseproducing Escherichia coli and Klebsiella species.
of infection, 54 subjects (28.9%) were located at Presbyterian Medical Center and 133 (71.1%) at the Hospital of the University of Pennsylvania. Thirty-two patients (17.1%) died while hospitalized. Microbiological analysis of the infecting ESBL-EK isolates disclosed that 83 (44.4%) were E coli, 88 (47.1%) were Klebsiella pneumoniae, and 11 (5.9%) were Klebsiella oxytoca. One patient was infected with both K pneumoniae and K oxytoca. The ESBL-EK organisms were isolated from a variety of anatomic sites (Figure 1). Of the 187 subjects, 112 (59.9%) received IIAT. Among these 112 patients, 24 (21.4%) died. In comparison, 8 (10.7%) of 75 patients who received adequate therapy died (OR [95% CI], 2.28 [0.92-6.24]; P= .06). Furthermore, there was a significant association between increasing time to initiation of adequate antimicrobial therapy and increased mortality (P .001, trend) (Figure 2). A number of other variables were associated with mortality on bivariable analyses (Table 1). Of note, patients with a nonurinary ESBL-EK infection had a significantly elevated risk of death, as did patients with a higher APACHE II score or a longer duration of hospitalization before ESBL-EK infection. On stratified analysis, the clinical site of infection was a significant effect modifier in the association between IIAT and mortality (P = .02). Specifically, among patients with urinary tract infections, there was no significant association between IIAT and mortality (OR [95% CI], 0.71 [0.17-2.88]). In contrast, for patients with nonurinary infections, a highly significant association existed (OR [95% CI], 7.54 [1.57-70.73]). Given these results, we included an interaction term in multivariable analyses reflecting the interaction between site of infection (ie, urinary tract vs nonurinary) and IIAT. On multivariable analyses, IIAT was a significant risk factor for mortality only for patients with nonurinary infection (adjusted OR [95% CI], 10.04 [1.9152.96]; P=.007) (Table 2). No significant association between IIAT and mortality existed for patients with urinary tract infection (adjusted OR [95% CI], 0.69 [0.192.53]; P=.58). Our primary analysis allowed a subject to be included more than once (ie, if a patient had ESBL-EK in-
fections more than 30 days apart). We subsequently performed a secondary analysis in which each subject was included only once (ie, for the first ESBL-EK infection). The final multivariable model was not substantively different from the primary model; IIAT remained a significant risk factor for mortality, but only for infections from a nonurinary site. We subsequently conducted a nested case-control study to investigate risk factors for IIAT. Among the 112 patients who received IIAT, 21 (18.8%) were infected with an MDR ESBL-EK isolate (ie, an ESBL-EK also resistant to sulfamethoxazole-trimethoprim, aminoglycosides, and fluoroquinolones), while only 1 (1.3%) of the 75 patients who were treated with adequate antimicrobials had an MDR ESBL-EK isolate (OR [95% CI], 17.1 [2.84- ]; P=.001). Two variables were independent risk factors for IIAT on multivariable analysis: (1) infection with an MDR ESBL-EK (adjusted OR [95% CI], 14.58 [1.91-111.36]; P=.01), and (2) health care acquisition of the ESBL-EK infection (adjusted OR [95% CI], 4.32 [1.49-12.54]; P=.007).
COMMENT
In our cohort of 187 hospitalized patients with ESBL-EK infection, approximately 17% died while in the hospital. The presence of IIAT was significantly associated with mortality, but only for ESBL-EK infections of nonurinary origin. Other independent risk factors for mortality included higher APACHE II score, location in an intensive care unit at the time of infection, and presence of malignancy. Finally, infection with an MDR ESBL-EK (ie, resistant to sulfamethoxazole-trimethoprim, aminoglycosides, and fluoroquinolones) was an independent risk factor for receiving IIAT. Given the increasing prevalence of ESBL-EK, risk factors for mortality in these infections must be clearly elucidated. Such data are essential in designing effective interventions targeted not only to improve outcomes but also to optimize judicious use of antimicrobial agents in an effort to curtail further emergence of resistance.20 We found a significant association between IIAT and mortality, but only for nonurinary ESBL-EK infections. Other studies that have demonstrated an association between delayed antimicrobial therapy and mortality have often
WWW.ARCHINTERNMED.COM
(REPRINTED) ARCH INTERN MED/ VOL 165, JUNE 27, 2005 1377
Downloaded from www.archinternmed.com at ROYAL PERTH HOSPITAL, on June 30, 2005 2005 American Medical Association. All rights reserved.
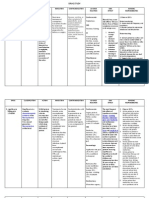
Table 1. Risk Factors for Mortality (Bivariable Analysis)
Variable Inadequate antimicrobial therapy Yes No Race (African American) Yes No Nursing home residence Yes No Health care acquisition of infection Yes No APACHE II score, median (range) Among deceased Among survivors ICU location at time of infection Yes No Duration of hospitalization, median (range) Among deceased Among survivors Site of infection Nonurinary Urinary tract Malignancy Yes No Central venous catheter Yes No Urinary catheter Yes No Mechanical ventilation Yes No Mortality, No./ Total No. (%) 24/112 (21.4) 8/75 (10.7) 9/85 (10.6) 13/61 (21.3) 5/50 (10.0) 27/137 (19.7) 32/166 (19.3) 0/20 13 (6-29) 10 (0-26) 24/68 (35.3) 8/116 (6.9) 12 (0-239) 3.5 (0-150) 20/88 (22.7) 12/99 (12.1) 12/31 (38.7) 20/155 (12.9) 23/91 (25.3) 8/91 (8.8) 26/136 (19.1) 5/49 (10.2) 22/47 (46.8) 10/139 (7.2) 2.13 (0.91-5.12) 7.36 (2.89-20.23) OR (95%CI) 2.28 (0.92-6.24) P Value* .06
0.44 (0.15-1.21)
.07
0.45 (0.13-1.30)
.12
...
.03
.001
.001
.009
.05
4.26 (1.61-10.87)
.001
3.51 (1.40-9.61)
.003
2.08 (0.72-7.36)
.15
11.35 (4.45-29.86)
.001
Abbreviations: APACHE II, Acute Physiology and Chronic Health Evaluation II; CI, confidence interval; ICU, intensive care unit; OR, odds ratio; ellipses, not calculable. *Fisher exact test (categorical variables); Wilcoxon rank sum test (continuous variables). Only variables for which bivariable P .20 are shown. No treatment was given with an antibiotic to which the infecting organism was susceptible within 48 hours of the culture being sent. Days from hospital admission until infection with extended-spectrum -lactamaseproducing Escherichia coli and Klebsiella species.
Table 2. Independent Risk Factors for Mortality (Multivariable Analysis)
Variable Inadequate antimicrobial therapy* APACHE II score Malignancy Nonurinary infection Interaction between inadequate antimicrobial therapy and nonurinary infection Regression Coefficient (SE) 0.36 (0.66) 0.13 (0.04) 1.60 (0.50) 1.30 (0.91) 2.67 (1.08) Adjusted OR (95% CI) 0.69 (0.19-2.53) 1.14 (1.05-1.24) 4.96 (1.85-13.30) 0.27 (0.05-1.64) P Value .58 .002 .001 .16
Abbreviations: APACHE II, Acute Physiology and Chronic Health Evaluation II; CI, confidence interval; OR, odds ratio. *No treatment was given with an antibiotic to which the infecting organism was susceptible within 48 hours of the culture being sent. The OR is for subjects with urinary tract infections. The association between inadequate antimicrobial therapy and mortality for nonurinary infections was as follows: adjusted OR, 10.04; 95% CI, 1.90-52.96; P = .007. The OR reflects the odds associated with each 1-point increase in APACHE II score. The OR is for subjects with adequate microbial therapy.
included only 1 type of infection (eg, bacteremia, pneumonia) and thus could not comment on possible effect modification by site of infection.7,8 Our results are con-
sistent with recent conclusions drawn by Paterson et al21 that the specific source of Klebsiella bacteremia was predictive of mortality; bacteremias that originated from
WWW.ARCHINTERNMED.COM
(REPRINTED) ARCH INTERN MED/ VOL 165, JUNE 27, 2005 1378
Downloaded from www.archinternmed.com at ROYAL PERTH HOSPITAL, on June 30, 2005 2005 American Medical Association. All rights reserved.
blood-borne or respiratory infections had the highest mortality rate, whereas bacteremias that originated from a urinary tract infection had the lowest mortality rate. Our results suggest that earlier implementation of effective therapy may result in improved outcomes. However, blanket use of broad antimicrobial regimens is likely to result in further emergence of resistance. Thus, efforts to optimize initial therapy must be balanced with efforts to promote judicious use of antimicrobial agents.20 To this end, our results suggest that efforts to optimize initial therapy should be primarily targeted only to suspected nonurinary ESBL-EK infections. Determination of whether clinical site of infection is an effect modifier in the relationship between IIAT and outcomes in infections due to other resistant organisms should be pursued in future studies. In investigating possible reasons why adequate initial antimicrobial therapy might be delayed, we found that the susceptibility profile of the infecting ESBL-EK pathogen plays an important role. The ESBL-EK isolates often demonstrate resistance to multiple antimicrobial classes.4 Besides the carbapenems, ESBL-EK infections may be effectively treated with sulfamethoxazole-trimethoprim, aminoglycosides, and fluoroquinolones. We hypothesized that ESBL-EK isolates demonstrating resistance to these agents would be more likely to go untreated with initial empirical therapy. Indeed, we found that MDR ESBL-EK infection (ie, ESBL-EK resistant to sulfamethoxazole-trimethoprim, aminoglycosides, and fluoroquinolones) was an independent risk factor for IIAT. In the future, it will be important to elucidate the epidemiology of MDR ESBL-EK, both to understand their prevalence and to inform possible intervention strategies based on earlier identification of patients with such isolates, and to tailor initial antimicrobial therapy accordingly. Several potential limitations exist in our study. Selection bias can be introduced because of lost or missing charts; complete medical records were available for 65% of eligible subjects in this study. However, when available data were compared, no significant differences existed between the patients included in the study and those who were not included because of missing charts. Although the potential for bias exists, this comparison argues against substantial selection bias. Selection bias may also have been introduced by allowing subjects to be included more than once (ie, if they had ESBL-EK infections greater than 30 days apart). However, no substantive difference was evident in the secondary analysis in which subjects were included only once. We defined our outcome of interest as in-hospital mortality. Although this defined end point is unambiguous, it does not differentiate according to the cause of death, so that some deaths may not have been directly attributable to the ESBL-EK infection. However, efforts to designate outcomes as attributable to a specific infection are often very subjective and inconsistently applied.22 Finally, our study was conducted in a large academic tertiary care medical center and a smaller urban community hospital; the results may not be generalizable to other institutions.
In conclusion, we found the mortality rate among patients with ESBL-EK infections to be high, approaching 20% in this cohort study. Inadequate initial antimicrobial therapy was an independent risk factor for mortality in these infections, but only among nonurinary infections. Recognizing the importance of maintaining judicious antibiotic use, these results suggest that empirical antimicrobial therapy interventions targeted to improve outcomes should be directed primarily at patients with suspected nonurinary infections. In addition, since MDR among ESBL-EK was a strong risk factor for inadequate therapy, efforts to elucidate the emergence and epidemiology of MDR ESBL-EK should be emphasized. Accepted for Publication: February 21, 2005. Author Affiliations: Center for Clinical Epidemiology and Biostatistics (Ms Hyle, Mr Lipworth, and Drs Zaoutis, Bilker, and Lautenbach), Center for Education and Research on Therapeutics (Ms Hyle, Mr Lipworth, and Drs Zaoutis, Bilker, and Lautenbach), Departments of Pathology and Laboratory Medicine (Dr Nachamkin) and Biostatistics and Epidemiology (Drs Bilker and Lautenbach), and Division of Infectious Diseases, Department of Medicine (Dr Lautenbach), University of Pennsylvania School of Medicine, Philadelphia; and Division of Infectious Diseases, Department of Medicine, The Childrens Hospital of Philadelphia (Dr Zaoutis). Correspondence: Ebbing Lautenbach, MD, MPH, MSCE, Center for Clinical Epidemiology and Biostatistics, University of Pennsylvania School of Medicine, 825 Blockley Hall, 423 Guardian Dr, Philadelphia, PA 191046021 (elautenb@mail.med.upenn.edu). Funding/Support: This study was supported by Public Health Service grant DK-02987-01 from the National Institutes of Health, Bethesda, Md (Dr Lautenbach). This study was also supported in part by Centers for Education and Research on Therapeutics grant U18-HS10399 from the Agency for Healthcare Research and Quality, Rockville, Md.
REFERENCES
1. Burwen DR, Banerjee SN, Gaynes RP; National Nosocomial Infections Surveillance System. Ceftazidime resistance among selected nosocomial gramnegative bacilli in the United States. J Infect Dis. 1994;170:1622-1625. 2. Itokazu GS, Quinn JP, Bell-Dixon C, Kahan FM, Weinstein RA. Antimicrobial resistance rates among aerobic gram-negative bacilli recovered from patients in intensive care units: evaluation of a national postmarketing surveillance program. Clin Infect Dis. 1996;23:779-784. 3. Lautenbach E, Patel JB, Bilker WB, Edelstein PH, Fishman NO. Extendedspectrum -lactamaseproducing Escherichia coli and Klebsiella pneumoniae: risk factors for infection and impact of resistance on outcomes. Clin Infect Dis. 2001;32:1162-1171. 4. Lautenbach E, Strom BL, Bilker WB, Patel JB, Edelstein PH, Fishman NO. Epidemiological investigation of fluoroquinolone resistance in infections due to extended-spectrum -lactamaseproducing Escherichia coli and Klebsiella pneumoniae. Clin Infect Dis. 2001;33:1288-1294. 5. Jacoby GA. Extended-spectrum -lactamases and other enzymes providing resistance to oxyimino- -lactams. Infect Dis Clin North Am. 1997;11:875-887. 6. Kollef MH, Ward S, Sherman G, et al. Inadequate treatment of nosocomial infections is associated with certain empiric antibiotic choices. Crit Care Med. 2000; 28:3456-3464. 7. Lodise TP, McKinnon PS, Swiderski L, Rybak MJ. Outcomes analysis of delayed antibiotic treatment for hospital-acquired Staphylococcus aureus bacteremia. Clin Infect Dis. 2003;36:1418-1423. 8. Harbarth S, Garbino J, Pugin J, Romand JA, Lew D, Pittet D. Inappropriate initial
(REPRINTED) ARCH INTERN MED/ VOL 165, JUNE 27, 2005 1379
WWW.ARCHINTERNMED.COM
Downloaded from www.archinternmed.com at ROYAL PERTH HOSPITAL, on June 30, 2005 2005 American Medical Association. All rights reserved.
9. 10. 11.
12.
13.
14.
15.
antimicrobial therapy and its effect on survival in a clinical trial of immunomodulating therapy for severe sepsis. Am J Med. 2003;115:529-535. Garner JS, Jarvis WR, Emori TG, Horau TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988;16:128-140. Knaus WA, Drapier EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818-829. Lautenbach E, Fishman NO, Bilker WB, et al. Risk factors for fluoroquinolone resistance in nosocomial Escherichia coli and Klebsiella pneumoniae infections. Arch Intern Med. 2002;162:2469-2477. Friedman ND, Kaye KS, Stout JE, et al. Health careassociated bloodstream infections in adults: a reason to change the accepted definition of communityacquired infections. Ann Intern Med. 2002;137:791-797. National Committee for Clinical Laboratory Standards. NCCLS Performance Standards for Antimicrobial Disk Susceptibility Testing: Approved Standard. 10th ed. Wayne, Pa: NCCLS; 2000. NCCLS Informational Supplemental Document M100S10. National Committee for Clinical Laboratory Standards. NCCLS Performance Standards for Antimicrobial Susceptibility Testing. 11th ed. Wayne, Pa: NCCLS; 2001. NCCLS Informational Supplemental Document M100-S11. National Committee for Clinical Laboratory Standards. NCCLS Performance Stan-
16. 17. 18. 19.
20.
21.
22.
dards for Antimicrobial Susceptibility Testing. 12th ed. Wayne, Pa: NCCLS; 2002. NCCLS Informational Supplemental Document M100-S12. Kleinbaum DG, Kupper LL, Morgenstern H. Epidemiologic Research: Principles and Quantitative Methods. New York, NY: Van Nostrand Reinhold; 1982. Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719-748. Hosmer DO, Lemeshow SL. Applied Logistic Regression. New York, NY: John Wiley & Sons; 1989. Sun GW, Shook TL, Kay GL. Inappropriate use of bivariable analysis to screen risk factors for use in multivariable analysis. J Clin Epidemiol. 1996;49:907916. Paterson DL, Rice LB. Empirical antibiotic choice for the seriously ill patient: are minimization of selection of resistant organisms and maximization of individual outcome mutually exclusive? Clin Infect Dis. 2003;36:1006-1012. Paterson DL, Ko WC, Von Gottberg A, et al. International prospective study of Klebsiella pneumoniae bacteremia: implications of extended-spectrum -lactamase production in nosocomial infections. Ann Intern Med. 2004;140:26-32. Cosgrove SE, Carmeli Y. The impact of antimicrobial resistance on health and economic outcomes. Clin Infect Dis. 2003;36:1433-1437.
(REPRINTED) ARCH INTERN MED/ VOL 165, JUNE 27, 2005 1380
WWW.ARCHINTERNMED.COM
Downloaded from www.archinternmed.com at ROYAL PERTH HOSPITAL, on June 30, 2005 2005 American Medical Association. All rights reserved.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Levofloksasin Hemihidrat MsdsDocument6 pagesLevofloksasin Hemihidrat MsdsEsin KahramanNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- CASENGHI, Buruli Ulcer FINAL - WatermarkedDocument1 pageCASENGHI, Buruli Ulcer FINAL - WatermarkedjackstewartbriggsNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Prescribing Antibiotics and Analgesics in ChildrenDocument4 pagesPrescribing Antibiotics and Analgesics in ChildrenPreetam PatnalaNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Identifying 5Document6 pagesIdentifying 5Nidia MaradiagaNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Pharmacology MCQDocument36 pagesPharmacology MCQNack Tie100% (2)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Vademecum English 2010Document70 pagesVademecum English 2010Gonzalo Mejía VásquezNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Present Advancement in The Diagnosis and Treatment of Typhoid FeverDocument7 pagesPresent Advancement in The Diagnosis and Treatment of Typhoid Feverelsa_imamNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- What Is CelecoxibDocument3 pagesWhat Is CelecoxibKevin LabbeikNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- 31Document4 pages31Noman AliNo ratings yet
- Adverse Effects of FluoroquinolonesDocument10 pagesAdverse Effects of FluoroquinolonesAvelox FloxNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Antibiotics in DentistryDocument25 pagesAntibiotics in Dentistryimmortalneo100% (1)
- CEPP National Audit - Focus On Antibiotic PrescribingDocument33 pagesCEPP National Audit - Focus On Antibiotic PrescribingmedicembuNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- (A. Garrido Frenich ... Et Al.) Veterinary Drugs A PDFDocument158 pages(A. Garrido Frenich ... Et Al.) Veterinary Drugs A PDFrajeevunnaoNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Pharmacology of PneumoniaDocument7 pagesPharmacology of PneumoniaGomedi WuNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Paracetamol and Levofloxacin Drug StudyDocument9 pagesParacetamol and Levofloxacin Drug StudyKevin Sam AguirreNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Urinary and Male GenitalDocument116 pagesUrinary and Male GenitalMultazam ZamNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Gereige 2013 PneumoniaDocument21 pagesGereige 2013 PneumoniaLuis Carlos OlguínNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- ENDOMETRITISDocument6 pagesENDOMETRITISKhrisna ParamaarthaNo ratings yet
- WSC Abstracts - 2011Document667 pagesWSC Abstracts - 2011cyber_zac52No ratings yet
- Pharmacology II OutlineDocument52 pagesPharmacology II Outlinerjones53No ratings yet
- Drug StudyDocument6 pagesDrug StudyRyan BancoloNo ratings yet
- 2014-01-06 Gulf War Illness Tied To Cipro AntibioticsDocument10 pages2014-01-06 Gulf War Illness Tied To Cipro AntibioticsAvelox FloxNo ratings yet
- Drugs Study For PneumoniaDocument5 pagesDrugs Study For PneumoniaLucelle ArellanoNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Urinary Tract Infection and QuinolonesDocument49 pagesUrinary Tract Infection and QuinolonesKhanzada ShahzebNo ratings yet
- Kirti Soni 2012Document11 pagesKirti Soni 2012Karyna de WolffNo ratings yet
- Enrofloxacin: Therapeutic ReviewDocument4 pagesEnrofloxacin: Therapeutic ReviewAndi Dytha Pramitha SamNo ratings yet
- Fapas Food Chemistry Programme 2016Document48 pagesFapas Food Chemistry Programme 2016Vishal SharmaNo ratings yet
- 30131Document38 pages30131Virda MaharaniNo ratings yet
- Fluoroquinolones Versus - Lactam Based Regimens For The Treatment of OsteomyelitisDocument8 pagesFluoroquinolones Versus - Lactam Based Regimens For The Treatment of OsteomyelitisFrank Barreiro SanchezNo ratings yet
- Medical Uses: Ciprofloxacin (Document10 pagesMedical Uses: Ciprofloxacin (Fahad Bin Saeed RabbaniNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)